A Systematic Review on Spinal Asymmetries in Case Studies of Unilateral Nephroptosis from a Viscerosomatic Point of View
Abstract
1. Introduction
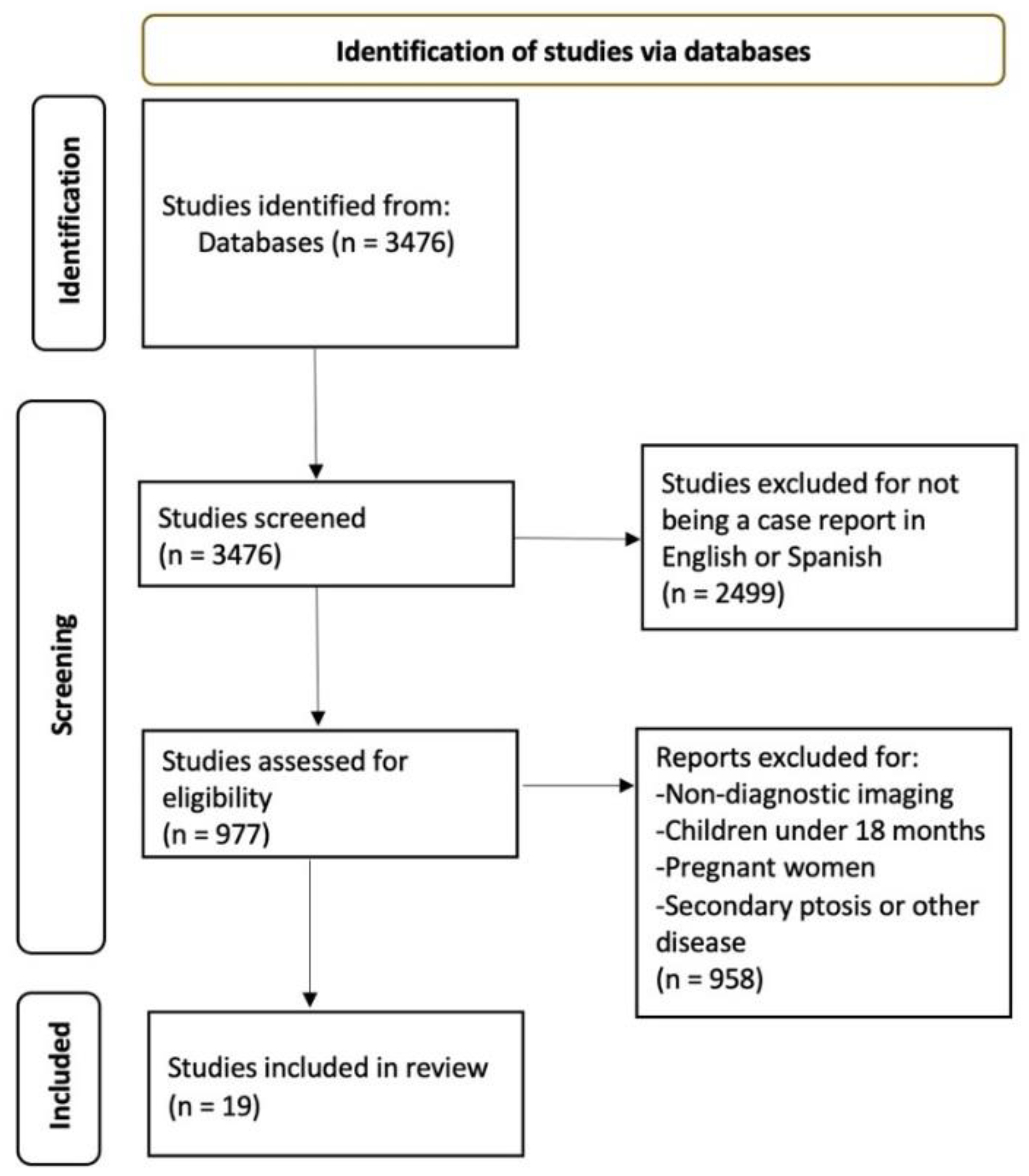
2. Materials and Methods
2.1. Data Sources and Search Strategy
2.2. Study Selection
2.3. Methodological Quality
2.4. Data Extraction
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. CARE Checklist Results
| TOPIC | ITEM | STUDIES | |||||
| Khan et al. [27] | Machado Bairo et al. [28] | Lezrek et al. [29] | O’Reilly et al. [30] | Marcovich et al. [31] | Leong et al. [32] | ||
| TITLE | 1 | NO | NO | NO | NO | NO | NO |
| KEYWORDS | 2 | YES | YES | YES | NO | NO | NO |
| ABSTRACT | 3a | YES | YES | YES | YES | YES | NO |
| 3b | NO | NO | NO | YES | YES | NO | |
| 3c | YES | YES | YES | NO | YES | NO | |
| 3d | YES | YES | YES | NO | YES | NO | |
| INTRODUCTION | 4 | YES | YES | YES | YES | NO | YES |
| PATIENT INFORMATION | 5a | YES | YES | YES | YES | YES | YES |
| 5b | YES | YES | YES | YES | YES | YES | |
| 5c | NO | NO | NO | NO | NO | NO | |
| 5d | YES | YES | NO | YES | YES | NO | |
| CLINICAL FINDINGS | 6 | YES | NO | YES | YES | YES | YES |
| TIMELINE | 7 | NO | NO | NO | NO | NO | NO |
| DIAGNOSTIC ASSESSMENT | 8a | YES | YES | YES | YES | YES | YES |
| 8b | NO | NO | NO | NO | NO | NO | |
| 8c | NO | NO | NO | NO | NO | NO | |
| 8d | NO | NO | NO | NO | NO | NO | |
| THERAPEUTIC INTERVENTION | 9a | YES | YES | YES | YES | YES | YES |
| 9b | YES | YES | YES | NO | YES | NO | |
| 9c | NO | NO | NO | NO | NO | NO | |
| FOLLOW-UP AND OUTCOMES | 10a | YES | YES | YES | YES | YES | NO |
| 10b | YES | YES | YES | YES | YES | YES | |
| 10c | NO | NO | NO | NO | NO | NO | |
| 10d | NO | NO | NO | NO | NO | NO | |
| DISCUSSION | 11a | YES | YES | YES | NO | YES | NO |
| 11b | YES | YES | YES | YES | YES | NO | |
| 11c | YES | YES | YES | YES | YES | NO | |
| 11d | YES | YES | YES | YES | YES | NO | |
| PATIENT PERSPECTIVE | 12 | NO | NO | NO | NO | NO | NO |
| INFORMED CONSENT | 13 | NO | NO | NO | NO | NO | NO |
| TOTAL | 18/30 | 17/30 | 17/30 | 14/30 | 17/30 | 7/30 | |
| TOPIC | ITEM | STUDIES | ||||||
| Jungling et al. 1º [33] | Jungling et al. 2º [33] | Tunc et al. [34] | Boylu et al. [35] | Baldassarre et al. [36] | Sood et al. [37] | Wroclawski et al. [38] | ||
| TITLE | 1 | NO | NO | NO | NO | NO | NO | NO |
| KEYWORDS | 2 | NO | NO | YES | NO | YES | NO | NO |
| ABSTRACT | 3a | NO | NO | YES | YES | YES | NO | YES |
| 3b | NO | NO | NO | YES | YES | NO | YES | |
| 3c | NO | NO | YES | YES | YES | NO | YES | |
| 3d | NO | NO | YES | YES | YES | NO | YES | |
| INTRODUCTION | 4 | YES | YES | YES | NO | YES | YES | NO |
| PATIENT INFORMATION | 5a | YES | YES | YES | YES | YES | YES | NO |
| 5b | YES | YES | YES | YES | YES | YES | NO | |
| 5c | YES | NO | NO | NO | NO | NO | NO | |
| 5d | YES | NO | NO | NO | YES | NO | NO | |
| CLINICAL FINDINGS | 6 | YES | YES | YES | YES | YES | YES | NO |
| TIMELINE | 7 | NO | YES | NO | NO | NO | NO | NO |
| DIAGNOSTIC ASSESSMENT | 8a | YES | NO | YES | YES | YES | YES | YES |
| 8b | NO | NO | NO | NO | NO | NO | NO | |
| 8c | NO | NO | NO | NO | NO | NO | NO | |
| 8d | NO | NO | NO | NO | NO | NO | NO | |
| THERAPEUTIC INTERVENTION | 9a | YES | YES | YES | YES | YES | YES | NO |
| 9b | NO | NO | YES | YES | YES | NO | NO | |
| 9c | NO | NO | NO | NO | NO | NO | NO | |
| FOLLOW-UP AND OUTCOMES | 10a | YES | YES | YES | YES | YES | YES | NO |
| 10b | YES | YES | YES | YES | YES | NO | NO | |
| 10c | NO | NO | NO | NO | NO | NO | NO | |
| 10d | NO | NO | NO | NO | NO | NO | NO | |
| DISCUSSION | 11a | NO | NO | YES | YES | NO | NO | NO |
| 11b | YES | YES | YES | YES | NO | NO | NO | |
| 11c | YES | YES | YES | YES | YES | NO | NO | |
| 11d | YES | YES | YES | YES | YES | NO | NO | |
| PATIENT PERSPECTIVE | 12 | NO | NO | NO | NO | NO | NO | NO |
| INFORMED CONSENT | 13 | NO | NO | NO | NO | NO | NO | NO |
| TOTAL | 13/30 | 11/30 | 17/30 | 16/30 | 17/30 | 7/30 | 5/30 | |
| TOPIC | ITEM | STUDIES | ||||||
| Hua Chan et al. [39] | Yoshida et al. [40] | Carola et al. [41] | Matsuda et al. [42] | Clark et al. [43] | Nanayakkara et al. [44] | Lim et al. [45] | ||
| TITLE | 1 | NO | NO | NO | YES | NO | NO | NO |
| KEYWORDS | 2 | NO | YES | YES | YES | NO | NO | NO |
| ABSTRACT | 3a | NO | NO | NO | NO | YES | NO | NO |
| 3b | NO | YES | NO | NO | YES | NO | NO | |
| 3c | NO | YES | NO | NO | YES | NO | NO | |
| 3d | NO | YES | NO | NO | YES | NO | NO | |
| INTRODUCTION | 4 | NO | YES | NO | YES | YES | NO | NO |
| PATIENT INFORMATION | 5a | YES | YES | YES | YES | YES | YES | YES |
| 5b | YES | YES | YES | YES | YES | YES | YES | |
| 5c | YES | YES | NO | NO | NO | NO | NO | |
| 5d | NO | NO | NO | NO | YES | NO | NO | |
| CLINICAL FINDINGS | 6 | YES | YES | NO | NO | YES | YES | YES |
| TIMELINE | 7 | NO | YES | YES | NO | NO | NO | NO |
| DIAGNOSTIC ASSESSMENT | 8a | YES | YES | YES | YES | YES | YES | YES |
| 8b | NO | NO | NO | NO | YES | YES | NO | |
| 8c | YES | YES | NO | NO | NO | NO | YES | |
| 8d | NO | NO | NO | NO | NO | NO | NO | |
| THERAPEUTIC INTERVENTION | 9a | YES | NO | NO | YES | YES | YES | YES |
| 9b | NO | NO | NO | YES | YES | NO | NO | |
| 9c | NO | NO | NO | NO | NO | NO | NO | |
| FOLLOW-UP AND OUTCOMES | 10a | NO | NO | NO | YES | YES | YES | NO |
| 10b | NO | NO | NO | YES | YES | YES | NO | |
| 10c | NO | NO | NO | NO | NO | NO | NO | |
| 10d | NO | NO | NO | NO | NO | NO | NO | |
| DISCUSSION | 11a | NO | NO | NO | YES | NO | NO | NO |
| 11b | NO | YES | NO | YES | NO | NO | NO | |
| 11c | NO | YES | NO | YES | YES | NO | NO | |
| 11d | NO | YES | NO | YES | YES | NO | NO | |
| PATIENT PERSPECTIVE | 12 | NO | NO | NO | NO | NO | NO | NO |
| INFORMED CONSENT | 13 | NO | YES | NO | NO | NO | NO | NO |
| TOTAL | 7/30 | 16/30 | 5/30 | 14/30 | 17/30 | 8/30 | 6/30 | |
References
- Greenman, P.E. Principios y Práctica de la Medicina Manual, 3rd ed.; Médica Panamericana: Buenos Aires, Argentina, 2005. [Google Scholar]
- Santos, T.S.; Oliveira, K.K.B.; Martins, L.V.; Vidal, A.P.C. Effects of manual therapy on body posture: Systematic review and meta-analysis. Gait Posture 2022, 96, 280–294. [Google Scholar] [CrossRef]
- Srinivas, M.; Jain, M.; Bawane, P.; Jayanthi, V. Normative values for esophageal motility assessed in the physiological seated position for 16-channel water perfused high-resolution esophageal manometry system and postural variations in healthy volunteers. J. Neurogastroenterol. Motil. 2020, 26, 61–66. [Google Scholar] [CrossRef]
- Chuang, T.Y.; Chiu, Y.C.; Fan, Y.H.; Hung, S.C.; Cheng, W.M. Better sleep quality could reinforce the relationship between sleep posture and kidney stone laterality in obstructive sleep apnea patients. Urolithiasis 2020, 48, 245–249. [Google Scholar] [CrossRef]
- Faure, A.; Dicrocco, E.; Hery, G.; Boissier, R.; Bienvenu, L.; Thirakul, S.; Maffei, P.; Panait, N.; Karsenty, G.; Merrot, T.; et al. Postural therapy for renal stones in children. J. Pediatr. Urol. 2016, 12, 252.e1–252.e6. [Google Scholar] [CrossRef]
- Krzanowski, M.; Partyka, L.; Drelicharz, L.; Mielnik, M.; Frolow, M.; Malinowski, K.P.; Sliwka, A.; Marciniak, K.; Aleksiejew-Kleszczynski, T. Posture commonly and considerably modifies stenosis of left common iliac and left renal veins in women diagnosed with pelvic venous disorder. J. Vasc. Surg. Ven. Lymphatic Disord. 2019, 7, 845–852.e2. [Google Scholar] [CrossRef]
- Ziaee, S.A.; Moradi, A.; Fateh, M.; Moghaddam, S.M.H. Sleep posture and unilateral renal stone formation. Scand. J. Urol. Nephrol. 2008, 42, 551–554. [Google Scholar] [CrossRef]
- Milani, G.P.; Mazzoni, M.B.M.; Burdick, L.; Bianchetti, M.G.; Fossali, E.F. Postural proteinuria associated with left renal vein entrapment: A follow-up evaluation. Am. J. Kidney Dis. 2010, 55, e29–e31. [Google Scholar] [CrossRef]
- Peng, L.; Wen, J.; Zhong, W.; Zeng, G. Is physical therapy effective following extracorporeal shockwave lithotripsy and retrograde intrarenal surgery: A meta-analysis and systematic review. BMC Urol. 2020, 20, 93. [Google Scholar] [CrossRef]
- Cao, L.; Wang, Y.Q.; Yu, T.; Sun, Y.; He, J.; Zhong, Y.; Li, X.; Sun, X. The effectiveness and safety of extracorporeal shock wave lithotripsy for the management of kidney stones. A protocol of systematic review and meta-analysis. Medicine 2020, 99, e21910. [Google Scholar] [CrossRef]
- Zanotto, T.; Gobbo, S.; Bullo, V.; Vendramin, B.; Roma, E.; Duregon, F.; Bocalini, D.S.; Di Blasio, A.; Cugusi, L.; Furian, L.; et al. Postural balance, muscle strength, and history of falls in end-stage renal disease patients living with a kidney transplant: A cross-sectional study. Gait Posture 2020, 76, 358–363. [Google Scholar] [CrossRef]
- Young, H.H.; Davis, D.M. Malformations and abnormalities of the urogenital tract. In Young’s Practice of Urology; Young, H.H., Ed.; W.B. Saunders: Philadelphia, PA, USA, 1926; pp. 1–36. [Google Scholar]
- Hoenig, D.M.; Ashok, K.H.; Shalhav, A.L.; Clayman, R.V. Nephroptosis: A “disparaged” condition revisited. Urology 1999, 54, 590–596. [Google Scholar] [CrossRef] [PubMed]
- Plas, E.; Daha, K.; Riedl, C.R.; Hünber, W.A.; Pflüger, H. Long-term follow-up after laparoscopic nephropexy for symptomatic nephroptosis. J. Urol. 2001, 166, 449–452. [Google Scholar] [CrossRef] [PubMed]
- Bratt, D.G.; Jaffer, A.; Chandra, L.; Patel, C.; Biyani, C.S. Nephroptosis: Is body mass index (BMI) the key? Scand. J. Urol. 2018, 52, 309–311. [Google Scholar] [CrossRef] [PubMed]
- Barber, N.J.; Thomspson, P.M. Nephroptosis and nephropexy—Hung up on the past? Eur. Urol. 2004, 46, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Westbrook, A.; Tambe, A.; Subramanian, K.; Monk, J.; Calthorpe, D. The mannequin sign. Spine 2005, 30, E115–E117. [Google Scholar] [CrossRef]
- Giamberardino, M.A. Referred muscle pain/hyperalgesia and central sensitisation. J. Rehabil. Med. 2003, 41, 85–88. [Google Scholar] [CrossRef]
- Jaberzadeh, S.; Zoghi, M. Mechanosensitivity of the median nerve in patients with chronic carpal tunnel syndrome. J. Bodyw. Mov. Ther. 2013, 17, 157–164. [Google Scholar] [CrossRef]
- Jaberzadeh, S.; Scutter, S.; Nazeran, H. Mechanosensitivity of the median nerve and mechanically produced motor responses during upper limb neurodynamic test 1. Physiotherapy 2005, 91, 94–100. [Google Scholar] [CrossRef]
- Balster, S.; Jull, G. Upper trapezius muscle activity during the brachial plexus tension test in asymptomatic subjects. Man. Ther. 1997, 2, 144–149. [Google Scholar] [CrossRef]
- Edgar, D.; Jull, G.; Sutton, S. The relationship between upper trapezius muscle length and upper quadrant neural tissue extensibility. Aust. J. Physiother. 1994, 40, 99–103. [Google Scholar] [CrossRef][Green Version]
- Elvey, R.L. Physical evaluation of the peripheral nervous system in disorders of pain and dysfunction. J. Hand Ther. 1997, 10, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Giamberardino, M.A.; Affaitati, G.; Lerza, R.; Fanò, G.; Fulle, S.; Belia, S.; Lapenna, D.; Vecchiet, L. Evaluation of índices of skeletal muscle contraction in áreas of referred hyperalgesia from an artificial ureteric Stone in rats. Neurosci. Lett. 2003, 338, 213–216. [Google Scholar] [CrossRef] [PubMed]
- Rakowska, M.; Królikowska, K.; Jobs, K.; Placzynska, M.; Kalicki, B. Pathophysiology and symptoms of renal colic in children—a case report. Dev. Period Med. 2018, 22, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Riley, D.S.; Barber, M.S.; Kienle, G.S.; Aronson, J.K.; von Schoen-Angerer, T.; Tugwell, P.; Kiene, H.; Helfand, M.; Altman, D.G.; Sox, H.; et al. CARE guidelines for case reports: Explanation and elaboration document. J. Clin. Epidemiol. 2017, 89, 218–235. [Google Scholar] [CrossRef]
- Khan, A.M.; Holman, E.; Tóth, C. Percutaneous nephropexy. Scand. J. Urol. Nephrol. 2000, 34, 157–161. [Google Scholar] [CrossRef] [PubMed]
- Machado Bairo, M.; Decia Mendizabal, R.; Suarez Besio, R. Nefropexia percutánea. Arch. Esp. Urol. 2001, 54, 151–155. [Google Scholar]
- Lezrek, M.; El Harrech, Y.; Bazine, K.; Sossa, J.; Assebane, M.; Alami, M.; Kasmaoui, E.; Beddouch, A.; Ameur, A. Percutaneous endoscopic nephropexy with a percutaneous suture passed through the kidney. Arab J. Urol. 2013, 11, 68–73. [Google Scholar] [CrossRef]
- O’Reilly, P.H.; Pollard, A.J. Nephroptosis: A cause of renal pain and a potential cause of inaccurate split renal function determination. Br. J. Urol. 1988, 61, 284–288. [Google Scholar] [CrossRef]
- Marcovich, R.; Wolf, J.S., Jr. Laparoscopy for the treatment of positional renal pain. Urology 1998, 52, 38–43. [Google Scholar] [CrossRef]
- Leong, J.Y.; Teplitsky, S.; Shenot, P.J. Medial renal ptosis: First radiographic documentation with computed tomography. Urology 2019, 126, e1–e2. [Google Scholar] [CrossRef]
- Jungling, M.L. Nephroptosis as the cause of lower abdominal pain. J. Iowa Med. Soc. 1979, 69, 16–18. [Google Scholar] [PubMed]
- Tunc, L.; Yesil, S.; Guneri, C.; Biri, H.; Ure, I.; Bozkirli, I. The use of polymer clips in transperitoneal laparoscopic nephropexy. Surg. Laparosc. Endosc. Percutan Tech. 2008, 18, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Boylu, U.; Lee, B.R.; Thomas, R. Robotic-assisted laparoscopic pyeloplasty and nephropexy for ureteropelvic junction obstruction and nephroptosis. J. Laparoendosc. Adv. Surg. Tech. A 2009, 19, 379–382. [Google Scholar] [CrossRef] [PubMed]
- Baldassarre, E.; Marcangeli, P.; Vigano, M.; Vittoria, I.; Pone, D.; Gillo, A.; Pierini, P. Robotic nephropexy in case of symptomatic nephroptosis. Arch. Ital. Urol. Androl. 2011, 83, 160–162. [Google Scholar]
- Sood, A.; Rogers, C. Floating kidney. BMJ Case Rep. 2018, 2018, bcr2018224921. [Google Scholar] [CrossRef]
- Wroclawski, M.L.; Peixoto, G.A.; Moschovas, M.C.; Carneiro, A.; Borrelli, M., Jr.; Colombo, J.R., Jr. Robot-assisted nephropexy. Int. Braz. J. Urol. 2018, 44, 1047–1048. [Google Scholar] [CrossRef]
- Hua Chan, V.S.; Wing Lam, T.P.; Man Lam, W.W. Nephroptosis: The wandering kidney. Kidney Res. Clin. Pract. 2018, 37, 306–307. [Google Scholar] [CrossRef]
- Yoshida, S.; Matsumura, M.; Maekawa, K.; Minaga, K.; Kamata, K.; Nozawa, M.; Watanabe, T.; Kudo, M. Recurrent abdominal pain caused by nephroptosis. Clin. J. Gastroenterol. 2020, 13, 621–625. [Google Scholar] [CrossRef]
- Carola, F. Renal ptosis and change of glomerular filtration values in the upright and supine positions. Clin. Nucl. Med. 2003, 28, 150–153. [Google Scholar] [CrossRef]
- Matsuda, T.; Uchida, J.; Ashida, M.; Mikami, O. Laparoscopic nephropexy: A case report. Int. J. Urol. 1996, 3, 397–400. [Google Scholar] [CrossRef]
- Clark, B.A.; Sekhon, A. Nephroptosis in a young woman with joint laxity. Nat. Rev. Nephrol. 2009, 5, 722–725. [Google Scholar] [CrossRef] [PubMed]
- Nanayakkara, P.W.; Van Bunderen, C.C.; Santerse, B. A bumpy ride to a discarded diagnosis. Lancet 2007, 369, 436. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.-H.; Chang, Y.-H. Tennis ball kidney of nephroptosis. BMJ Case Rep. 2011, 2011, bcr0720103174. [Google Scholar] [CrossRef] [PubMed]
- Srirangam, S.J.; Pollard, A.J.; Adeyoju, A.B.; O’Reilly, P.H. Nephroptosis: Seriously misunderstood? BJU Int. 2009, 103, 296–300. [Google Scholar] [CrossRef] [PubMed]
- Isbir, C.A.; Duger, C.; Gursoy, S.; Kayusuz KKol, I.O.; Bozdag, A.; Mimaroglu, C. A puzzling and rare cause of chest and shoulder pain: Migrated foreign body to the spleen. Pain Med. 2012, 13, 1660–1661. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saad, A.; Rex, D.K. Colonoscopy-induced splenic injury: Reporto f 3 cases and literatura review. Dig. Dis. Sci. 2008, 53, 892–898. [Google Scholar] [CrossRef]
- Luong, C.; Starovoytov, A.; Heydari, M.; Sedlak, T.; Aymong, E.; Saw, J. Clinical presentation of patients with spontaneous coronary artery dissection. Catheter Cardiovasc. Interv. 2017, 89, 1149–1154. [Google Scholar] [CrossRef]
- Ghanem, A.N. “Disparaged” nephroptosis. Urology 2000, 56, 183–184. [Google Scholar] [CrossRef]
- Moss, S.W. Floating kidneys: A century of nephroptosis and nephropexy. J. Urol. 1997, 158, 699–702. [Google Scholar] [CrossRef]
- Tutusaus, R.; Potau, J.M. Sistema Fascial: Anatomía, Valoración y Tratamiento; Médica Panamericana: Madrid, Spain, 2015. [Google Scholar]
- Lalonde, F. The runner’s kidney: A case report. Int. J. Osteopath Med. 2014, 17, 206–210. [Google Scholar] [CrossRef]
- Mogorovich, A.; Selli, C.; De Maria, M.; Manassero, F.; Durante, J.; Urbani, L. Clinical reappraisal and state of the art of nephropexy. Urología 2018, 85, 135–144. [Google Scholar] [CrossRef]
- Reinstein, E.; Pimentel, M.; Pariani, M.; Nemec, S.; Sokol, T.; Rimoin, D.L. Visceroptosis of the bowel in the hypermobility type of Ehlers-Danlos syndrome: Presentation of a rare manifestation and review of the literature. Eur. J. Med. Genet. 2012, 55, 548–551. [Google Scholar] [CrossRef]
- Truc, E.; Tesniéres, B. L’élement péritonéo conjonctif de la statique rénale. J. d’Urol. 1954, 60, 23–37. [Google Scholar]
- González Viejo, M.E.; Cohí, O.; Salinas, F. Escoliosis. Realidad Tridimensional; Masson: Barcelona, Spain, 2001. [Google Scholar]
- Morrissy, R.T.; Weinstein, S.L. Lovell and Winter’s Pediatric Orthopaedics, 6th ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2006; pp. 693–762. [Google Scholar]
- Groiso, J.A. Patología ortopédica. In Atención Integral de Adolescentes y Jóvenes. Criterios de Diagnóstico y Tratamiento; Sociedad Argentina de Pediatría, Ed.; Sociedad Argentina de Pediatría: Buenos Aires, Argentina, 1996; pp. 305–318. [Google Scholar]
- Anderson, S.M. Spinal curves and scoliosis. Radiol. Technol. 2007, 79, 44–65. [Google Scholar]
- Hume, K. Scoliosis: To screen or not to screen. Br. J. Sch. Nurs. 2008, 3, 214–218. [Google Scholar] [CrossRef]
- Chin, K.; Price, J.S.; Zimbler, S. A guide to early detection of scoliosis. Contemp. Pediatr. 2001, 18, 77. [Google Scholar]
- Chorley, J.N.; Neinstein, L.S. Scoliosis and Kyphosis. In Adolescent Health Care: A Practical Guide, 4th ed.; Neinstein, L.S., Ed.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2002; pp. 369–382. [Google Scholar]
- Kim, H.; Kim, H.S.; Moon, E.S.; Yoon, C.-S.; Chung, T.-S.; Song, H.-T.; Suh, J.-S.; Lee, Y.H.; Kim, S. Scoliosis imaging: What radiologists should know. Radiographics 2010, 30, 1823–1842. [Google Scholar] [CrossRef]
- Kyoungkyu, J.; Dong-il, K. The association between low body weight and scoliosis among korean elementary school students. Int. J. Environ. Res. Public Health 2018, 15, 2613. [Google Scholar] [CrossRef]
| Studies | Subjects | Medical History | Symptoms | Clinical Findings | Diagnosis | Intervention | Follow-Up |
|---|---|---|---|---|---|---|---|
| Khan et al. [27] | 42 Female 9 Male 18–75 years | Ipsilateral flank pain aggravated by walking. 13/51 moving mass. 9/51 lithiasis in the ptotic kidney. | PE: depression of abdominal mass in 13/51 in the SUP. Ultrasound: right renal descent. IU: shows a shortened and descended ureter. | Right 44/51 left 7/51 nephroptosis | Nephropexy | 2 months: kidney well positioned. 3.5 years on average: 3/51 with symptoms, 2/51 remain ptosis. | |
| Machado Bairo et al. [28] | 6 Female 34.3 average years | 1/6 appendectomy | Long symptomatic course. No lithiasis. | IU: superior renal descent when UP versus SUP. Renal scintigraphy: 5/6 obstructive pattern and 1/6 ischaemia when UP. | Right nephroptosis | Right nephropexy | 21,6 months: 5/6 with no pain, no obstructive pattern, correct position. 1/6 less pain, no ischaemia and reduced descent. |
| Lezrek et al. [29] | 4 Female 30.5 average years | Abdominal pain on the right side when UP for a prolonged time. | Ultrasound: right renal descent when UP. IU: inclination with shortening of the ureter when UP. | Right nephroptosis | Right nephropexy | 28 average months: 4/4 no symptoms. Ultrasound and IU kidney higher when UP. | |
| O’Reilly et al. [30] | 1 Female 30 years | Right abdominal pain and presence of a right paraumbilical mass. | PE: palpable right abdominal mass, visible and painful when UP. IU: descended right kidney. Renography: abnormal mobility of the right kidney when UP. | Right nephroptosis | Right nephropexy | Renography normal in both positions. No symptoms. | |
| Marcovich et al. [31] | 1 Female 38 years | L3-4 spinal fusion. Total hysterectomy. | Right flank pain worse when UP, relief in SUP. | IU: in any position rotation and right nephroptosis. Diuretic renogram: 30% right renal function without obstruction in the SUP. | Right nephroptosis | Right nephropexy | 6 weeks: renal ptosis resolution. 29 weeks: no pain. |
| Leong et al. [32] | 1 Female 34 years | Intermittent right upper abdominal protrusion. No abdominal pain. | CT: medial deviation of the right kidney with moderate hidronephrosis. IU: minimal deviation of the right ureter when UP. | Right medial nephroptosis | Right nephropexy | 6 months: normal anatomical position of the right kidney. | |
| Jungling et al. 1º [33] | 1 Female 26 years | Recurrent dull pain in the right lower AQ. Increased pain when UP, relief in SUP. | PE: mobile mass on the right flank when UP. IU: ptotic kidney with hidronephrosis when UP. | Right nephroptosis | Nephropexy and right pyeloplasty | IU when UP normal and complete resolution of symptoms (6 weeks). | |
| Jungling et al. 2º [33] | 1 Female 31 years | Dull, intermittent pain in the right lower AQ. Increased pain when UP, relief in SUP. | PE: mobile mass on the right flank when UP. IU: right kidney descended and rotated when UP. Arteriography: two anomalously located renal arteries. | Right nephroptosis | Right nephropexy | No pain. IU no description. | |
| Tunc et al. [34] | 1 Female 34 years | Right flank pain which decreases in the SUP. Feeling of falling into the abdomen when UP. | IU and abdominopelvic ultrasound: both positions show minimal dilatation of the collecting system, shortening of the right ureter and nephroptosis. VAS: 10/10. | Right nephroptosis | Pain unit and physiotherapy. Right nephropexy. | VAS 1/10. 60 days: IU cephalic position right kidney. 210 days: IU without complications. | |
| Boylu et al. [35] | 1 Female 22 years | Persistent non-specific right flank pain when UP and relief in the SUP. | Ultrasound: moderate to severe right hidronephrosis without dilatation of the ureter. IU and fluoroscopy: right renal descent when UP. | Right nephroptosis and right UPJO | Simultaneous right pyeloplasty and nephropexy | 3 weeks: unobstructed | |
| Baldassarre et al. [36] | 1 Female 34 years | Right flank pain when UP. | Renal ultrasound and IU: 5 to 6 cm descent of the right kidney when UP. | Right nephroptosis | Right nephropexy | 2 months: slight pyelectasis and clinical improvement. 6 months: improvement of ptosis | |
| Sood et al. [37] | 1 Female 28 years | Intermittent right abdominal pain that worsens when UP. | IU: 6 cm craniocaudal migration of the right kidney when UP. | Right nephroptosis | Right nephropexy | 4 weeks: symptoms improvement, not pain. 6 years: decrease of symptoms. | |
| Wroclawski et al. [38] | 1 Female 29 years | Pain on right side. | PE: mobile and palpable right kidney. Ultrasound, IU and renal scintigraphy: confirms right renal ptosis when UP. | Right nephroptosis | Right nephropexy | 1 month: symptoms improvement, normal function and appropriate position. | |
| Hua Chan et al. [39] | 1 Female 40 years | Long-term right-sided pain. | PE: soft abdomen without pain, kidneys not votable. Intravenous pyelography: descent of the right kidney when UP. | Right nephroptosis | Conservative TX and clinical follow-up | ||
| Yoshida et al. [40] | 1 Female 38 years | Caesarean section at the age of 26. Hyperaldosteronism. | Recurrent abdominal pain of more than 12 months’ duration. | PE: no acute findings. LT: slight elevation of C-reactive protein. Ultrasound: showed the positional changes of the right kidney. | Right nephroptosis | ||
| Carola et al. [41] | 1 Female 26 years | Lower back pain and discomfort in the right lower AQ. | LT: low creatinine and urine creatinine values. Renal scintigraphy and IU: renal ptosis. | Right nephroptosis | |||
| Matsuda et al. [42] | 1 Female 44 years | Herniated disc | Dull pain in the right side of the spine when UP, relief in SUP. | IU: renal descent when UP. Renography: reduced renal plasma flow. | Right nephroptosis | Retained TX 1 year. Right nephropexy | 1 month: IU when UP does not descend and renography improves flow. 3 months: no pain. |
| Clark et al. [43] | 1 Female 25 years | Joint hyperlaxity, morning stiffness in the lumbar spine, hands and legs. | Constant dull pain in the abdomen and right side, radiating to the groin. 10 months postpartum. | PE: joint laxity, mobile abdominal mass from right mid to lower quadrant. IU: right renal descent greater than 2 vertebral bodies when standing upright. | Formerly psychosomatic disorder, intestinal pathology. Right nephroptosis. | Psychiatry. Conservative TX with strengthening exercises and use of elastic corset. | Less intense symptomatology |
| Nanayakkara et al. [44] | 1 Female 28 years | Abdominal pain from right lower back to groin and vomiting. | PE: tender palpation of the right abdominal area. IU: lowering and ventral rotation of the right kidney when UP. Renogram: reduced renal function. | Right nephroptosis | For 10 years, psychiatric TX. Right nephropexy. | 1 year after nephropexy: kidney well positioned and pain-free. | |
| Lim et al. [45] | 1 Female 43 years | Focal and palpable intermittent abdominal mass in the SUP but not when UP. No pain. | PE: no palpable abdominal mass. Abdominal rx: right kidney small, rounded and descended when UP. | Right nephroptosis | Observation and follow-up |
| STUDIES | SUPINE DECUBITUS | STANDING | CSS | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RP | UPK | VI | LHR | HIC | FC/PA | RP | UPK | VI | LHR | HIC | FC/PA | ||
| Khan et al. [27] | L4 | L2-3-4-5 | ↑ | YES/ YES | |||||||||
| Machado Bairo et al. [28] | L2 | L3-4 | YES/ YES | L4 | L2-3-4-5 | YES/ YES | YES | ||||||
| Lezrek et al. [29] | L4-5 | L3-4 | T12 L-1-2-3-4-5 | ↓ | ↑ | YES/ YES | |||||||
| O’Reilly et al. [30] | L2 | L1 | L3-4-5 | ↓ | ↑ | YES/ YES | |||||||
| Marcovich et al. [31] | L2-3 | L1 | L3-4-5 | YES/ YES | L5 | L3-4 | L1-2-3-4-5 | ↑ | YES/ YES | YES | |||
| Leong et al. [32] | L2-3 | L1-2-3-4-5 | ↓ | ↑ | YES/ YES | ||||||||
| Jungling et al. [33] Case 1 | L2-3 | L1 | NO/NO | L2-3 | T12 L4 | ↓ | YES/ YES | YES | |||||
| Jungling et al. [33] Case 2 | L3 | ↑ | YES/ YES | S | S | NO/NO | YES | ||||||
| Tunc et al. [34] | L2-3 | L1 | T12 L2-3-4-5 | ↓ | YES/ YES | ||||||||
| Boylu et al. [35] | L1 | L3-4-5 | YES/ YES | L4 | L2-3 | L3-4-5 | ↓ | YES/ YES | YES | ||||
| Baldassarre et al. [36] | L3-4 | L3 | L1-2-3-4-5 | ↑ | YES/ YES | L5 | L4 | L2-3-4-5 | ↑ | YES/ YES | YES | ||
| Sood et al. [37] | L3 | L2 | L2-3-5 | YES/ YES | L4-5 | L3-4 | L2-3-4-5 | YES/ YES | YES | ||||
| Wroclawski et al. [38] | L2 | L1 | L1-2-3-4-5 | ↑ | YES/ YES | L3-4 | L2-3 | L1-2-3-4-5 | ↑ | NO/ YES | YES | ||
| Hua Chan et al. [39] | L2-3 | L1 | T12 L1-2-3-4 | ↓ | YES/ YES | L4-5 | L3 | T12 L1-2-3-4-5 | ↓ | ↑ | YES/ YES | YES | |
| Yoshida et al. [40] | L2-3 | L1 | L4-5 | L3 | L1-2-3 | ↑ | YES/ YES | YES | |||||
| Carola et al. [41] | L3 | L2 | L1-2-3-4-5 | ↓ | YES/ YES | ||||||||
| Matsuda et al. [42] | L1-2-3 | YES/ YES | |||||||||||
| Clark et al. [43] | L2-3 | L1 | L2-3-4 | ↓ | YES/ YES | L4 | L3 | L1-2-3-4-5 | ↓ | YES/ YES | YES | ||
| Nanayakkara et al. [44] | L2-3 | L1 | L3-4-5 | ↑ | YES/ YES | L4 | L3 | L3-4-5 | ↑ | YES/ YES | YES | ||
| Lim et al. [45] | L2 | T12 L1-2-3 | YES/ YES | L3-4 | LDV T12 L1-2-3-4-5 | ↓ | ↑ | YES/ YES | YES | ||||
| STUDIES | SUPINE DECUBITUS | STANDING | CSS | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RP | UPK | VI | LHR | HIC | FC/PA | PPC | RP | UPK | VI | LHR | HIC | FC/PA | PPC | ||
| Khan et al. [27] | L2 | T12 L1-2-3 | NO/ YES | L2 | L2-3-4 | ↑ | YES/ YES | YES | YES | ||||||
| Machado Bairo et al. [28] | L2 | L2-3-4-5 | ↓ | YES/ YES | YES | ||||||||||
| Lezrek et al. [29] | L3-4 | L2 | L3-4-5 | ↓ | ↑ | YES/ YES | YES | ||||||||
| O’Reilly et al. [30] | |||||||||||||||
| Marcovich et al. [31] | L2 | L3-4-5 | ↑ | YES/ YES | YES | L3 | L1-2-3-4-5 | ↑ | YES/ YES | YES | NO | ||||
| Leong et al. [32] | |||||||||||||||
| Jungling et al. [33] Case 1 | L2 | YES/ YES | YES | ||||||||||||
| Jungling et al. [33] Case 2 | L3-4 | L2 | L4-5 | ↑ | YES/ YES | YES | |||||||||
| Tunc et al. [34] | L1-2 | T12 L1 | T12 L1-2-3-4-5 | ↓ | YES/ YES | YES | |||||||||
| Boylu et al. [35] | |||||||||||||||
| Baldassarre et al. [36] | |||||||||||||||
| Sood et al. [37] | |||||||||||||||
| Wroclawski et al. [38] | |||||||||||||||
| Hua Chan et al. [39] | |||||||||||||||
| Yoshida et al. [40] | |||||||||||||||
| Carola et al. [41] | |||||||||||||||
| Matsuda et al. [42] | L2-3 | L1-2-3 | YES/ YES | YES | |||||||||||
| Clark et al. [43] | |||||||||||||||
| Nanayakkara et al. [44] | |||||||||||||||
| Lim et al. [45] | |||||||||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliva-Pascual-Vaca, Á.; Castillo-Cañuelo, M.J.; Oliva-Pascual-Vaca, J.; Pérez-Montalbán, M.; Ordonez, F.J.; Martínez-Fernández, J.A. A Systematic Review on Spinal Asymmetries in Case Studies of Unilateral Nephroptosis from a Viscerosomatic Point of View. Healthcare 2022, 10, 2422. https://doi.org/10.3390/healthcare10122422
Oliva-Pascual-Vaca Á, Castillo-Cañuelo MJ, Oliva-Pascual-Vaca J, Pérez-Montalbán M, Ordonez FJ, Martínez-Fernández JA. A Systematic Review on Spinal Asymmetries in Case Studies of Unilateral Nephroptosis from a Viscerosomatic Point of View. Healthcare. 2022; 10(12):2422. https://doi.org/10.3390/healthcare10122422
Chicago/Turabian StyleOliva-Pascual-Vaca, Ángel, María José Castillo-Cañuelo, Jesús Oliva-Pascual-Vaca, María Pérez-Montalbán, Francisco Javier Ordonez, and José Antonio Martínez-Fernández. 2022. "A Systematic Review on Spinal Asymmetries in Case Studies of Unilateral Nephroptosis from a Viscerosomatic Point of View" Healthcare 10, no. 12: 2422. https://doi.org/10.3390/healthcare10122422
APA StyleOliva-Pascual-Vaca, Á., Castillo-Cañuelo, M. J., Oliva-Pascual-Vaca, J., Pérez-Montalbán, M., Ordonez, F. J., & Martínez-Fernández, J. A. (2022). A Systematic Review on Spinal Asymmetries in Case Studies of Unilateral Nephroptosis from a Viscerosomatic Point of View. Healthcare, 10(12), 2422. https://doi.org/10.3390/healthcare10122422







