Abstract
Due to the increasing importance of caregivers in the treatment outcomes of patients with mental illness, this study aimed to systematically review studies investigating the former’s caregiver burden and determine its prevalence. An open search, without filters, was conducted. Articles were selected from Medline, Scopus, and PubMed from inception to 30 April 2022 using the PRISMA protocol. Subgroup analyses examined the between-group differences by study setting, measurements used, and disorder type. A total of 5034 caregivers from 23 countries were included in this review. Thirty-nine studies were included in the systematic review, and, among them, twenty-six were deemed eligible for meta-analysis. The overall pooled prevalence of caregiver burden among caregivers of individuals with mental illness was 31.67% (95% CI = 26.22–37.12). Pooled prevalence was the highest among care recipients receiving treatment in a hospital setting (36.06%; 95% CI = 22.50–49.63), followed by the community and clinic settings. Caregiver prevalence values were higher for burden measured using the Zarit Burden Interview (38.05%; 95% CI = 27.68–48.43). compared with other instruments, and for carers of care recipients with psychosis (35.88%; 95% CI = 27.03–44.72) compared with those without. Thus, targeted interventions should focus on caregivers of patients in hospital settings and with psychotic symptoms.
1. Introduction
Caregiving burden is defined as the stress that derives from caring for others, while caregiver burden is the sensation of emotional or physical tension felt by caregivers [1]. Such terms are multifaceted and aim to capture the concept behind the particular role of caring for people from different backgrounds with varying degrees of strength and resources, and who are dealing with illness-specific symptoms [2]. Treudley first proposed the concept in 1946, stating that caregiving has a negative impact on the caregiver’s mental health and quality of life [3]. In order to meet caregiving responsibilities, caregivers expend their physical, mental, social, and financial resources [4]. Caregiver burden is a widespread occurrence observed all around the world, with approximately 80% of caregivers experiencing it in their duties [3]. Factors such as the patient’s characteristics (e.g., female sex, a lower educational level), carers’ attributes, the relationship between the patient and carer (e.g., living in with the carer), time spent with the patient, and the nature and severity of the illness could impact the intensity of the caregiver burden [5,6].
Currently, an estimated 25% of the global population is suffering from mental health conditions, placing it as one of the most important factors contributing to the disease burden [7]. Correspondingly, around 450 million people across the world are experiencing mental or behavioral disorders [8]. Depression holds the highest proportion of 4.3% of the global burden of diseases and is among the largest single cause of mental illness worldwide [8]. Nearly 30% of people from all parts of the world suffer from mental illness in a year. With the increasing prevalence of psychiatric illnesses, more psychiatric patients are treated at home as compared to obtaining in-hospital treatment, which may unintentionally increase the burden of the caregivers of these psychiatric patients [9]. However, many informal caregivers who shoulder such responsibilities may not have had any proper training and education in providing care. Mental illness would thus have an influence not only on the person with the condition, but also on those who care for them [10]. Caregivers of patients with mental illness were found to have high rates of mental health difficulties compared to the general population [11]. While the benefits and drawbacks of providing care are not always obvious, they tend to result in high levels of caregiver stress [6].
Due to the considerable disability associated with their condition, those suffering from major mental illness become increasingly dependent on their caretakers. When a person suffers from severe mental illness, he or she experiences significant functional and role impairment, as well as employment disability. Approximately 90% of people with serious mental illnesses are assisted practically and emotionally on a daily basis by family carers [12]. However, many caregivers experience a significant amount of psychological pressure and are heavily burdened as a result of their lack of preparedness for the job as an informal caregiver [12,13,14]. The need and obligation to provide care deeply influence the carers’ health, employment, social life, and relationships, leading to feelings of unhappiness and dissatisfaction [10,15,16]. Suffering psychological distress and shouldering burdens while caring for a mentally ill relative affects not only the caregiver’s quality of life and health, but also their productivity as an individual and their ability to provide quality care for the ill relative, thereby worsening the ill relative’s health and decreasing the likelihood of recovery or health improvements [17,18].
Several reviews have looked into caregiver burden across various caregiving groups, including carers living with patients who have dementia [6,19,20,21,22,23]. These reviews [6,19,20,21,22,23] found that, in the 149 studies reviewed, carers’ quality of life was associated with burden and burnout syndrome, as dementia caregivers are isolated from society because of the nature of their caregiving responsibilities [19]. The findings also showed that there is a great need within this population for interventions that are successful at lowering the burden and depression symptoms [19,20]. Another review on caregivers of dementia patients reported that female caregivers tend to be more burdened than male caregivers as females undertake a greater amount of caregiving work [23]. Other reviews were conducted on carers living with older relatives [24,25,26] and carers of cancer patients [27,28]. A number of meta-analyses have also studied the association between caregiver burden and psychological distress, such as depression, anxiety, and stress [29,30,31]. Del-Pino-Casado et al. [29] reported on the association between subjective caregiver burden and symptoms of anxiety across caring groups in accordance with the COSMOS-E guide’s recommendations. Del-Pino-Casado et al. [30] examined the relationship between the subjective caregiver load of caregivers of elderly relatives and depressive symptoms. Park and Park [31] analyzed the impact of family support programs on the caregiving burden, depression, and stress experienced by family caregivers of dementia patients. Others have focused on the effectiveness of interventions to ameliorate caregiver burden among carers [32,33]. Although there are several reviews and meta-analyses on caregiver burden across different populations, especially in the area of dementia or neurocognitive disorders, there have not been any studies investigating the prevalence of caregiver burden among caregivers of individuals with mental illnesses. Data surrounding this area are thus lacking, warranting further research.
This study aimed to provide a systematic review and meta-analysis by addressing the prevalence of burden among caregivers of individuals with mental illness; this study thus hopes to give more detailed insights and shed further light in the practice and research of this particular area. The specific questions addressed in this review were as follows:
- What is the prevalence of caregiver burden among caregivers of individuals with mental illness?
- Does the prevalence of caregiver burden differ according to study setting, measurements used, and type of disorder?
2. Materials and Methods
2.1. Protocol
The present review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and was registered with PROSPERO (CRD42021255863).
2.2. Design
The present study was a systematic review and meta-analysis of quantitative studies on caregiver burden among caregivers of patients with mental illness.
2.3. Literature Search
In compiling articles for this study, the electronic databases Medline, Scopus, and PubMed were used. The articles were selected regardless of publication date and study location, so long as it was published before or on 30 April 2022. An open search, without filters, was conducted to maximize sensitivity. A combination of search terms was used to look for relevant studies, i.e., burden* OR caregiver burden* OR burnout OR exhaustion OR strain OR overload* OR frustrate* OR stress AND caregiver* OR informal caregiver OR family caregiver OR carer* AND mental* OR mental illness OR mental disorder OR mental issues OR schizophrenia OR psychiatric disorder OR psych* problem OR mental health OR bipolar disorder OR substance abuse OR psychiatric illness OR depression OR anxiety OR psychotic disorder OR obsessive-compulsive disorder OR behaviour disorder OR behavioural disorder. Forward and backward searches were conducted as well to identify suitable articles. The search strategies are shown in Table 1.

Table 1.
Search terms and strategy used in PubMed, Scopus, and MEDLINE.
2.4. Study Selection
Firstly, relevant articles identified through the databases were imported into the Endnote program X5 version and any duplicate publications were removed. This step was performed by two investigators (C.Q.C. and C.R.K.) independently. Secondly, the two investigators (C.Q.C. and C.R.K.) independently screened the titles and abstracts to ensure the eligibility of the articles. Thirdly, full-text articles were assessed independently by the same two investigators, based on the inclusion criteria mentioned below. Any disagreements that arose were resolved through a discussion before the commencement of the quantitative analysis.
2.5. Inclusion Criteria
Cohort studies and cross-sectional studies were eligible for quantitative analysis if the participants in the study were the caregivers of individuals with mental illness. The studies must also have been published in an English peer-reviewed journal. Any articles that reported on the percentage, prevalence, or mean score of burden with any screening or diagnostic tools were included in this study. The disorders that are listed in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition [34] were included in the study. Studies on caregivers of patients with mental illness, in general, were also included.
2.6. Exclusion Criteria
Based on the authors’ consensus, we decided to exclude major neurocognitive disorders or dementia, as a recent meta-analytic study had addressed this condition [21]. If the first and second investigators (C.Q.C. and C.R.K.) had doubts concerning the eligibility of a study to be included, then the third and fourth reviewers (K.W.L. and C.S.S.) were involved in the decision-making process. We also excluded pilot, qualitative, validation, psychometric, preliminary, randomized controlled trial, systematic review, meta-analysis, treatment-related, and interventional studies. Unpublished reports, seminar presentations, doctoral and master’s theses, and grey literature searches were not included in the study.
2.7. Data Extraction
The data were extracted and managed in a pre-designed form in Microsoft Excel. A form listing the name of the first author, publication year, study location, study design, study setting, sample size, and measuring instruments was then used to assess article characteristics. Data extraction was conducted independently by three reviewers (C.Q.C., C.S.S., and C.R.K.), and the results of the data extraction were compared between the three reviewers to ensure that there were no errors.
2.8. Quality Assessment
The quality of the included articles was assessed based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist [35]. The results of the assessment are shown in Table S1. There are 22 proposed items in the checklist, with items 6, 12, 14, and 15 having specific variations, which assessed 6 components for cohort, case–control, and cross-sectional studies. The absence or presence of a component stated in each item from the article was graded with a “0” or a “1”, respectively. Each article was graded as “low risk of bias” if the STROBE score was ≥14/22; or “high risk of bias” if the score was <14/22. Two investigators (C.Q.C and C.R.K.) individually assessed the study’s quality, and any discrepancies were resolved by discussion with the third investigator (C.S.S.). Fifteen studies scored ≥14 and were graded as having “low risk of bias”, while 24 studies scored ≤14 and were graded as having “high risk of bias”. Studies were nevertheless included in the analysis regardless of the STROBE score and grading (refer to Table S1).
2.9. Statistical Analysis
A meta-analysis using a continuous random-effect model (DerSimonian and Laird method) was performed. Random-effects meta-analyses allow for heterogeneity by assuming that underlying effects follow a normal distribution, but they must be interpreted carefully. Heterogeneity between the trials was assessed by considering the I2 inconsistency statistic. An I2 estimate greater than or equal to 70% was interpreted as an indication of substantial levels of heterogeneity. If the quantitative analysis was unsuitable due to the heterogeneity and/or a small number of studies, a narrative overview of the findings of the included studies was presented with tabular summaries of extracted data.
Since the mean of burden was available from 26 of the articles, the mean of burden was used to conduct the meta-analysis of this study to estimate the pooled prevalence of caregiver burden [36,37]. Percentages and 95% confidence intervals were used as summary statistics for the pooled prevalence. Sensitivity analyses were used to examine whether overall findings were robust to potentially influential decisions. Prediction intervals from random-effects meta-analyses are a useful device for presenting the extent of between-study variation. The data from each study (care recipients, country, study design, study setting, and measures for burden) were used to build tables for an overall description of the included studies. As study populations and data sources differed among the included studies, an evaluation of studies was conducted to determine whether they were suitable for meta-analysis, and only suitable studies were included in the quantitative analysis. Open Meta (Analyst) [38] was used to conduct the meta-analysis for this study.
2.10. Subgroup Analyses
Subgroup analyses are useful to examine the between-group differences in terms of the prevalence as a possible cause of heterogeneity across studies. The prevalence of caregivers of individuals with mental illness was examined by subgrouping the study setting, measurements used, and type of disorder. The prevalence of caregiver burden was reported in percentages with a 95% confidence interval (CI).
2.11. Sensitivity Analysis
We performed sensitivity analysis by using the leave-one-out meta-analysis to examine how each particular study altered the overall performance of the rest of the studies, especially with regard to the pooled prevalence estimates and heterogeneity. We used the I2 (Higgins et al. [39]) to measure the proportion of heterogeneity due to the variability of effect estimates amongst individual studies, with values of 25, 50, and 75% indicative of mild, moderate, and severe heterogeneity, respectively.
3. Results
3.1. Description of Included Studies
A total of 4983 articles were identified in the initial screening. After removing the duplicate articles (n = 598), 4385 articles were retrieved for further assessment. After screening for suitability based on the title and abstract, 4341 articles were excluded, and 44 articles were selected for full-text assessment. After a thorough evaluation, a total of 27 articles were identified to be suitable to be included in the systematic review. Another 52 articles were identified through forward and backward searches. However, of these 52 articles, only 12 articles were deemed suitable to be included in the systematic review. Therefore, a total of 39 articles were included in the systematic review. Among the 39 articles, 26 articles were deemed eligible for meta-analysis (refer to Figure 1).
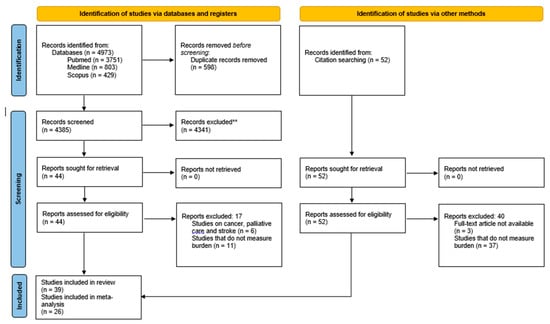
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram of the literature screening process.
The main characteristics of the included studies (n = 39) were tabulated as shown in Table S2. Among the included studies, 23 studies used a cross-sectional design. A total of 5034 caregivers from 23 countries were included in the analysis. Six studies were conducted in Nigeria [18,40,41,42,43,44], five studies in Brazil [45,46,47,48,49], three studies each in Nepal [50,51,52] and Turkey [53,54,55], two studies each in Hong Kong [56,57], the USA [58,59], and Taiwan [60,61], and one study each in Africa [62], China [63], Chile [64], Egypt [65], Greece [66], India [67], Ireland [68], Italy [69], Japan [70], Jordan [71], Kuwait [72], Poland [73], Portugal [74], Singapore [75], Spain [76], and the Netherlands [77]. In terms of study setting, 11 studies were conducted in the community, 18 studies in the hospital, and nine studies in the clinic (refer to Table S2).
With regard to the care recipients of the caregivers, 12 studies were conducted on patients with mental illness in general, 12 studies focused on patients with schizophrenia, while five studies focused on bipolar affective disorders with schizophrenia-related disorders. Two studies focused on patients with depressive disorders. One study each was conducted on patients who were suffering from autism spectrum disorders, down syndrome, neurodevelopmental disorders, neuropsychiatric illness, minor psychiatric disorders, and obsessive-compulsive disorders.
The most used instrument to measure caregiver burden was the Zarit Burden Interview [78], which was used in 17 of the studies. Three studies each used the Family Burden Interview Schedule [79] and the Involvement Evaluation [80]. Two studies each employed the Caregiver Strain Index [81] and Burden Assessment Scale [82]. Other studies, on the other hand, utilized the Caregiver Burden Inventory [83], Family Burden Scale [84], Family Problems Questionnaire [85], Feetham Family Functioning Scale [86], Perceived Chronic Strains Scale [87], Self-Perceived Pressure by Informal Care Scale [88], Social Behavior Assessment Schedule [89], Burden Assessment Schedule [90], Burden Questionnaire [91], and Caregiver Burden Scale [92]. In two of the studies [45,50], the researchers constructed their own questionnaire to measure caregiver burden.
3.2. Pooled Prevalence of Caregiver Burden among Caregivers of Patients with Mental Illness
A summary of the pooled prevalence of caregiver burden among caregivers of patients with mental illness is shown in Figure 2. The pooled prevalence was conducted on the 26 articles that were deemed eligible for meta-analysis. The overall pooled prevalence was 31.67% (95% CI = 26.22–37.12). The highest prevalence of caregiver burden recorded was 86.51% (95% CI = 82.54–90.48), while the lowest prevalence was 3.13% (95% CI = 2.36–3.90). More than half of the studies (n = 14) recorded a prevalence of caregiver burden below the average prevalence of 30%, while twelve studies recorded a prevalence of caregiver burden above the average (refer to Figure 2).
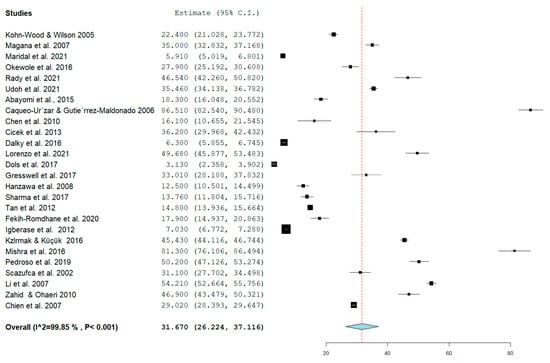
Figure 2.
Pooled prevalence of caregiver burden among caregivers of patients with mental illness [18,40,41,44,48,49,50,51,52,54,55,56,58,59,60,62,63,64,65,68,69,70,71,72,75,77].
3.3. Subgroup Analysis for the Prevalence of Caregiver Burden among Caregivers of Patients with Mental Illness According to Study Setting, Instruments, and Type of Mental Illness
Table 2 summarizes the subgroup analysis of the pooled prevalence of caregiver burden among caregivers of patients with mental illness according to study setting and instruments used, as well as the disorders. Forest plots for study setting, the instruments used, and the disorders are shown in Figure 3, Figure 4, and Figure 5, respectively (refer to Figure 3, Figure 4 and Figure 5). The pooled prevalence of caregiver burden was highest among the care recipients who received treatment in a hospital setting (36.06%; 95% CI = 22.50–49.63), followed by the community setting (28.28%; 95% CI = 18.97–37.58), while the lowest pooled prevalence of caregiver burden among the care recipients who received treatment was in a clinic setting (27.52%; 95% CI = 14.78–40.26). Subgroup analysis according to the instrument used showed that the highest burden of care was were reported in studies using the Zarit Burden Interview (36.90%; 95% CI = 28.17–45.62). In terms of the type of disorder, the pooled prevalence of caregiver burden was highest among the caregivers of care recipients who suffered from psychotic disorders (35.88%; 95% CI = 27.03–44.72) (refer to Table 2).

Table 2.
Subgroup analysis of pooled prevalence of caregiver burden among caregivers of patient with mental illness.
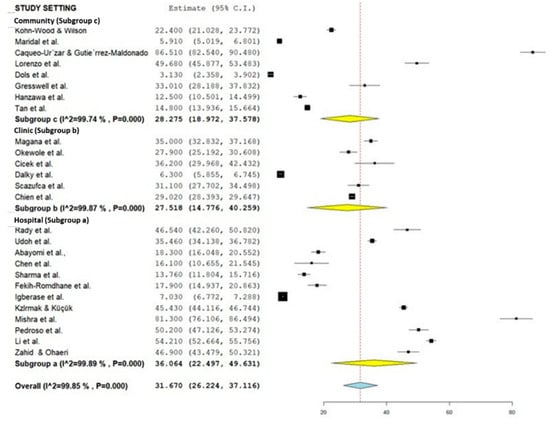
Figure 3.
Subgroup forest plot on the study setting (Community: [50,58,64,68,69,70,75,77]; Clinic: [40,49,54,56,59,71]; Hospital: [18,41,44,48,51,52,55,60,62,63,65,72]).
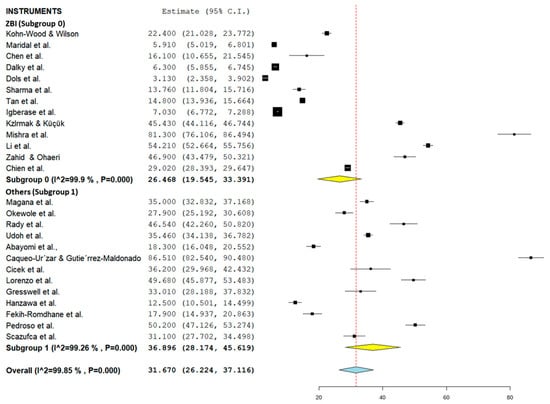
Figure 4.
Subgroup forest plot on the types of measurement used (Zarit: [44,50,51,52,55,56,58,60,63,71,72,75,77]; Others: [6,18,40,41,48,49,54,62,64,65,68,69,70]).
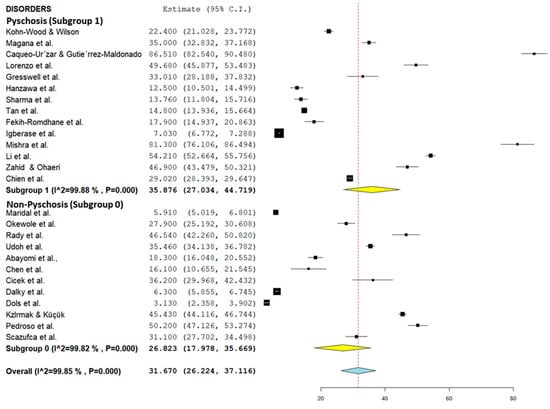
Figure 5.
Subgroup forest plot of psychotic and non-psychotic disorders (Psychosis: [44,51,52,56,58,59,62,64,68,69,70,72,75]; Non-psychosis: [18,40,41,48,49,50,54,55,60,65,71,77]).
4. Discussion
To the best of our knowledge, this review is the first systematic review and meta-analysis on the caregiver burden of carers for individuals with mental illness. We aimed to investigate the prevalence of burden among caregivers of individuals with mental illness. A total of 5034 caregivers from 23 countries were included in the analysis. Thirty-nine articles were included in the systematic review and 26 articles were deemed eligible for meta-analysis. Subgroup comparisons across study settings, the measurement used, and the type of mental illness were conducted. The main finding of this study was that the overall pooled prevalence of caregiver burden among caregivers of individuals with mental illness was 31.67%. Subgroup analyses showed that caregivers in hospital settings (36.06%), studies using the Zarit Burden Interview (36.90%), and caregivers of individuals suffering from psychosis (35.88%) recorded significantly higher prevalence values.
In this study, we found that nearly one third of caregivers of individuals with mental illness, excluding major cognitive disorders, suffered from caregiver burden. The caregiver burden prevalence of 31.67%% found in our study, however, is lower than the prevalence of caregiver burden found in other meta-analytic studies [20,93] which cover a wide range of conditions, including physical and mental illnesses. For example, the pooled prevalence of caregiver burden among caregivers of dementia patients was nearly twice as high, at 49.26% [20]. On the other hand, a meta-analysis conducted in Iran on the caregiver burden of carers for chronic illness patients showed that more than half (53.28%) had caregiver burden, and the prevalence of caregiver burden for mentally ill patients (58.7%) was comparable to that of Alzheimer’s patients (57.1%) [93]. A meta-analysis that compared the caregiver burden of carers for physical vs. mental illnesses showed that carers for patients with physical illnesses recorded significantly lower caregiver burden mean scores than those with cognitive impairment or dementia, Alzheimer’s, and mental illnesses [94]. As the heterogeneity between studies included in this meta-analysis was high, there may be a need to examine further the factors that contributed to the high variances, and the reasons contributing to the lower prevalence.
This study also found that carers for mentally ill individuals within the schizophrenia spectrum disorder or with psychosis recorded a higher caregiver burden prevalence (35.88%) than for carers in studies that did not mention the presence of psychosis in the patients (26.82%). Caregivers who care for patients with psychotic symptoms face a greater burden than those who care for patients with bipolar disorders, with a higher burden reported by laborers and housewives [95]. Symptoms of psychosis, such as disorganized thoughts, hallucinations, and delusions, may require constant supervision to ensure the patient’s personal hygiene and grooming and prevent the patient from engaging in negative behaviors such as skipping medication [95,96]. The greater burden felt by caregivers of schizophrenia patients may also be due to the need for caregiving even during remission, and the social exclusion experienced by the caregivers or patients [95]. The caregiver burden of schizophrenia patients was higher among older and unemployed individuals, mothers, those reporting lower educational levels, and caretakers of younger patients [64]. Moreover, a study further found that the caregiver burden may be due to higher psychological morbidity and maladaptive coping in caregivers or schizophrenia patients [97]. Another study reported that, compared to carers of patients with depression, a significantly higher percentage of carers of patients with schizophrenia reported worrying about the future and finances of the patient [98]. Carers of schizophrenia patients also reported providing more motivation and encouragement to schizophrenia patients in the latter’s care [98]. Greater worry and the provision of nursing care may have contributed to a greater burden among carers for patients with psychosis or schizophrenia spectrum disorders. Moreover, the higher stigma against individuals with schizophrenia vs. depression or other mental illnesses, particularly in terms of perceptions of dangerousness and negative stereotyping for schizophrenia patients [99,100], may further isolate the caregiver from sources of social support.
Caregivers of individuals with mental illness in hospital settings in this study reported a higher caregiver burden compared with those in clinic and community settings. The characteristics of the patients requiring hospitalization may indicate a need for greater care, such as a more severe presentation of the mental illness symptoms or exhibiting self-harm or suicidal behaviors [101,102]. A study found that patients who were involuntarily admitted to the hospital had a higher likelihood of more severe psychotic symptoms, aggressive behavior, and medication non-adherence [101]. Caregiver burden may be a factor determining the decision to institutionalize older people in hospital settings [103]. Limited engagement with the healthcare system due to a lack of health literacy, perceptions of ineffective healthcare provided, and limited access to healthcare services has been associated with greater caregiver burden [2]. In another study on caregiver burden among carers of children with neurodevelopmental disabilities, caregivers experienced a greater burden when they found it difficult to access and navigate within the healthcare system or reported unmet healthcare needs [104]. Therefore, caregivers of hospital-dwelling patients may be experiencing a higher caregiver burden as they may lack the support provided by the healthcare system.
The Zarit Burden Interview (ZBI) is the most commonly used instrument to measure caregiver burden. The findings are consistent with a review of instruments measuring caregiver burden for mental illness patients conducted by Schulze and Rössler [105]. The other instruments used to measure caregiver burden are the Family Burden Interview Schedule [80], Involvement Evaluation [80], Caregiver Strain Index [81], Burden Assessment Scale [82], Caregiver Burden Inventory [83], Family Burden Scale [84], Family Problems Questionnaire [85], Feetham Family Functioning Scale [86], Perceived Chronic Strains Scale [87], Self-Perceived Pressure by Informal Care Scale [88], Social Behavior Assessment Schedule [89], Burden Assessment Schedule [90], Burden Questionnaire [91], and Caregiver Burden Scale [92].
Despite the use of a number of validated questionnaires, two of the studies reviewed used a self-designed or adapted questionnaire [45,50]. It was interesting to note that the caregiver burden prevalence using the Zarit Burden Interview was higher (36.90%) in comparison with studies utilizing other instruments (26.47%). The difference may be attributed to the fact that these questionnaires were originally developed for measuring caregiver burden among different populations, and they have different factor structures and target populations. For example, the ZBI was developed with the purpose of measuring the burden of caregivers for dementia patients and is now considered the gold standard and a generic measurement for caregiver burden for diverse diseases. Meanwhile, the Involvement Evaluation Questionnaire was used more specifically to assess the caregiver burden among those caring for patients with severe mental illnesses such as schizophrenia [74]. The Caregiver Burden Inventory, on the other hand, provides a multidimensional view of caregiver burden (time dependence, developmental, physical, social, and emotional burden) and may be useful in providing specific areas for intervening with caregiver burden based on these dimensions [83]. Future studies estimating the prevalence of caregiver burden should specify which questionnaire they are using and note the tendency for the ZBI to yield a higher estimated prevalence of caregiver burden.
More than half (62%) of the included studies in our review had a high risk of bias. There were 24 articles with a “high risk of bias”, while the remaining studies were graded as having a “low risk of bias” (n = 15). Items in the STROBE checklist, such as “use of a flow diagram”, “sources of bias”, and “sample size calculation”, were not commonly reported. Two studies used self-designed questionnaires to measure caregiver burden, which may have resulted in limited comparison with studies using commonly used scales such as the Zarit Burden Interview. As a result of the high risk of bias of 24 studies and variations in the caregiver burden measurement tools, only a small selection of research could be included for meta-analysis. This research has some limitations. The search technique was confined to peer-reviewed and published articles in international databases. Unpublished reports, seminar presentations, doctoral and master’s theses, and grey literature searches were not included in the study. The pre-specified criteria for this study may be too narrow, resulting in the exclusion of potentially relevant studies from our analysis. All the research considered in this review used cross-sectional designs, which prevented causal conclusions from being drawn. The use of several scales to measure caregiver burden may have contributed to the higher heterogeneity between studies. In addition, we found high levels of within-group heterogeneity to be present among subgroups, indicating that these groups may not account for the variance between studies and that the results of subgroup analyses may need to be interpreted with caution because of uneven covariate distributions among groups. As a result, it would be worthwhile to conduct additional studies to address these constraints.
5. Implications
The results of this study support a renewed emphasis on interventions to identify the caregiver burden for the growing number of informal caregivers. The findings of this study have drawn attention to the possibility that caregivers of individuals with mental illness may require psychological help in order to cope with the burden that they face. By taking care of loved ones at home, caregivers significantly contribute to the reduction of expenses and resources for the healthcare system. Therefore, it is essential to provide a support framework to lessen the burden on caregivers. There also appears to be a lack of cohort studies addressing caregiver burden, which could provide higher-quality evidence of caregiver burden across time. Researchers choosing measurement tools to measure caregiver burden should be aware that the Zarit Burden Interview may provide higher burden scores in comparison with other instruments measuring caregiver burden.
6. Conclusions
In conclusion, this study revealed that nearly one third of the caregivers experienced a burden when taking care of individuals with mental illness. This study suggests that the prevalence of caregiver burden was significantly higher for carers in hospital settings, studies utilizing the Zarit Burden Interview, and caregivers of individuals with psychosis. Given their increasing importance in the treatment outcomes of psychiatric patients in the age of deinstitutionalization, caregivers of people with mental illness should therefore receive more attention.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare10122423/s1, Table S1: Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) of Included Studies, Table S2: Characteristics of Included Studies.
Author Contributions
Conceptualization, C.Q.C., C.S.S., K.W.L. and N.I.; Data curation, C.Q.C., C.S.S. and C.R.K.; Formal analysis, C.Q.C., K.W.L. and C.S.S.; Methodology, C.Q.C., K.W.L. and N.I.; Supervision, N.I. and C.S.S.; Validation, A.N.Y., U.V., F.N.A.R. and S.R.; Visualization, C.Q.C.; Writing—original draft, C.Q.C., M.C.H., N.I., K.W.L., C.S.S., C.R.K., A.N.Y., U.V., F.N.A.R. and S.R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received its funding from the Fundamental Research Grant Scheme (FRGS/1/2020/SS0/UCSI/02/1) from the Ministry of Higher Education, Malaysia. The funder had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We would like to thank H.W.Y. for proofreading this manuscript.
Conflicts of Interest
The authors declare that they have no competing interests.
References
- Mosley, P.E.; Moodie, R.; Dissanayaka, N. Caregiver Burden in Parkinson Disease: A Critical Review of Recent Literature. J. Geriatr. Psychiatry Neurol. 2017, 30, 235–252. [Google Scholar] [CrossRef] [PubMed]
- Tamizi, Z.; Fallahi-Khoshknab, M.; Dalvandi, A.; Mohammadi-Shahboulaghi, F.; Mohammadi, E.; Bakhshi, E. Caregiving Burden in Family Caregivers of Patients with Schizophrenia: A Qualitative Study. J. Educ. Health Promot. 2020, 9, 12. [Google Scholar] [CrossRef] [PubMed]
- Chadda, R.K. Caring for the Family Caregivers of Persons with Mental Illness. Indian J. Psychiatry 2014, 56, 221. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.Y.; Lu, H.L.; Tsai, Y.F. Caregiver Burden and Health-Related Quality of Life among Primary Family Caregivers of Individuals with Schizophrenia: A Cross-Sectional Study. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2020, 29, 2745–2757. [Google Scholar] [CrossRef] [PubMed]
- Adelman, R.D.; Tmanova, L.L.; Delgado, D.; Dion, S.; Lachs, M.S. Caregiver Burden: A Clinical Review. JAMA 2014, 311, 1052–1059. [Google Scholar] [CrossRef]
- Alves, L.C.D.S.; Monteiro, D.Q.; Bento, S.R.; Hayashi, V.D.; Pelegrini, L.N.D.C.; Vale, F.A.C. Burnout Syndrome in Informal Caregivers of Older Adults with Dementia: A Systematic Review. Dement. Neuropsychol. 2019, 13, 415–421. [Google Scholar] [CrossRef]
- Cheah, Y.K.; Azahadi, M.; Phang, S.N.; Abd Manaf, N.H. Sociodemographic, Lifestyle, and Health Factors Associated With Depression and Generalized Anxiety Disorder among Malaysian Adults. J. Prim. Care Community Health 2020, 11, 2. [Google Scholar] [CrossRef]
- Walke, S.C.; Chandrasekaran, V.; Mayya, S.S. Caregiver Burden among Caregivers of Mentally Ill Individuals and Their Coping Mechanisms. J. Neurosci. Rural Pract. 2018, 9, 180–185. [Google Scholar] [CrossRef]
- Ahmad, N.A.; Muhd Yusoff, F.; Ratnasingam, S.; Mohamed, F.; Nasir, N.H.; Mohd Sallehuddin, S.; Mahadir Naidu, B.; Ismail, R.; Aris, T. Trends and Factors Associated with Mental Health Problems among Children and Adolescents in Malaysia. Int. J. Cult. Ment. Health 2015, 8, 125–136. [Google Scholar] [CrossRef]
- Azman, A.; Jamir Singh, P.S.; Sulaiman, J. The Mentally Ill and Their Impact on Family Caregivers: A Qualitative Case Study. Int. Soc. Work 2017, 62, 461–471. [Google Scholar] [CrossRef]
- Lian, C.W.; Shui, I.V.J.; Hazmi, H. Mental Health Status and Its Associated Factors among Caregivers of Psychiatric Patients in Kuching, Sarawak. Malays. Fam. Physician Off. J. Acad. Fam. Physicians Malays. 2019, 14, 18. [Google Scholar]
- Gharavi, Y.; Stringer, B.; Hoogendoorn, A.; Boogaarts, J.; van Raaij, B.; van Meijel, B. Evaluation of an Interaction-Skills Training for Reducing the Burden of Family Caregivers of Patients with Severe Mental Illness: A Pre-Posttest Design. BMC Psychiatry 2018, 18, 84. [Google Scholar] [CrossRef] [PubMed]
- Akbari, M.; Alavi, M.; Irajpour, A.; Maghsoudi, J. Challenges of Family Caregivers of Patients with Mental Disorders in Iran: A Narrative Review. Iran. J. Nurs. Midwifery Res. 2018, 23, 329–337. [Google Scholar] [CrossRef] [PubMed]
- Stanley, S.; Balakrishnan, S.; Ilangovan, S. Psychological Distress, Perceived Burden and Quality of Life in Caregivers of Persons with Schizophrenia. J. Ment. Health Abingdon Engl. 2017, 26, 134–141. [Google Scholar] [CrossRef]
- Neong, S.C.; Rashid, A. Quality of Life of Caregivers of Patients with Psychiatric Illness in Penang. J. Clin. Psychiatry Cogn. Psychol. 2018, 2, 12–13. [Google Scholar] [CrossRef]
- Siddiqui, S.; Khalid, J. Determining the Caregivers’ Burden in Caregivers of Patients with Mental Illness. Pak. J. Med. Sci. 2019, 35, 1329. [Google Scholar] [CrossRef]
- Maeng, S.-R.; Kim, W.-H.; Kim, J.-H.; Bae, J.-N.; Lee, J.-S.; Kim, C.-E. Factors Affecting Quality of Life and Family Burden among the Families of Patients with Schizophrenia. Korean J. Schizophr. Res. 2016, 19, 78. [Google Scholar] [CrossRef][Green Version]
- Udoh, E.E.; Omorere, D.E.; Sunday, O.; Osasu, O.S.; Amoo, B.A. Psychological Distress and Burden of Care among Family Caregivers of Patients with Mental Illness in a Neuropsychiatric Outpatient Clinic in Nigeria. PLoS ONE 2021, 16, e0250309. [Google Scholar] [CrossRef]
- Aledeh, M.; Adam, P.H. Caring for Dementia Caregivers in Times of the COVID-19 Crisis: A Systematic Review. Am. J. Nurs. Res. 2020, 8, 552–561. [Google Scholar] [CrossRef]
- Collins, R.N.; Kishita, N. Prevalence of Depression and Burden among Informal Care-Givers of People with Dementia: A Meta-Analysis. Ageing Soc. 2020, 40, 2355–2392. [Google Scholar] [CrossRef]
- Leng, M.; Zhao, Y.; Xiao, H.; Li, C.; Wang, Z. Internet-Based Supportive Interventions for Family Caregivers of People with Dementia: Systematic Review and Meta-Analysis. J. Med. Internet Res. 2020, 22, e19468. [Google Scholar] [CrossRef] [PubMed]
- Van der Lee, J.; Bakker, T.J.E.M.; Duivenvoorden, H.J.; Dröes, R.M. Multivariate Models of Subjective Caregiver Burden in Dementia: A Systematic Review. Ageing Res. Rev. 2014, 15, 76–93. [Google Scholar] [CrossRef] [PubMed]
- Xiong, C.; Biscardi, M.; Nalder, E.; Colantonio, A. Sex and Gender Differences in Caregiving Burden Experienced by Family Caregivers of Persons with Dementia: A Systematic Review Protocol. BMJ Open 2018, 8, e022779. [Google Scholar] [CrossRef] [PubMed]
- Domingues, N.S.; Verreault, P.; Hudon, C. Reducing Burden for Caregivers of Older Adults With Mild Cognitive Impairment: A Systematic Review. Am. J. Alzheimers Dis. Other Dement. 2018, 33, 401–414. [Google Scholar] [CrossRef] [PubMed]
- Wing, W.; Lam, Y.; Nielsen, K.; Sprigg, C.A.; Kelly, C.M. The Demands and Resources of Working Informal Caregivers of Older People: A Systematic Review. Work Stress 2022, 36, 105–127. [Google Scholar] [CrossRef]
- Namasivayam-MacDonald, A.M.; Shune, S.E. The Burden of Dysphagia on Family Caregivers of the Elderly: A Systematic Review. Geriatrics 2018, 3, 30. [Google Scholar] [CrossRef]
- Geng, H.M.; Chuang, D.M.; Yang, F.; Yang, Y.; Liu, W.M.; Liu, L.H.; Tian, H.M. Prevalence and Determinants of Depression in Caregivers of Cancer Patients: A Systematic Review and Meta-Analysis. Medicine 2018, 97, 2–4. [Google Scholar] [CrossRef]
- Jadalla, A.; Page, M.; Ginex, P.A.; Coleman, M.; Vrabel, M.; Bevans, M. Family Caregiver Strain and Burden: A Systematic Review of Evidence-Based Interventions When Caring for Patients with Cancer. Clin. J. Oncol. Nurs. 2020, 24, 31–50. [Google Scholar] [CrossRef]
- Del-Pino-Casado, R.; Priego-Cubero, E.; López-Martínez, C.; Orgeta, V. Subjective Caregiver Burden and Anxiety in Informal Caregivers: A Systematic Review and Meta-Analysis. PLoS ONE 2021, 16, e0247143. [Google Scholar] [CrossRef]
- Del-Pino-Casado, R.; Cardosa, M.R.; López-Martínez, C.; Orgeta, V. The Association between Subjective Caregiver Burden and Depressive Symptoms in Carers of Older Relatives: A Systematic Review and Meta-Analysis. PLoS ONE 2019, 14, e0217648. [Google Scholar] [CrossRef]
- Park, S.; Park, M. Effects of Family Support Programs for Caregivers of People with Dementia—Caregiving Burden, Depression, and Stress: Systematic Review and Meta-Analysis. J. Korean Acad. Nurs. 2015, 45, 627–640. [Google Scholar] [CrossRef]
- Li, Y.; Li, J.; Zhang, Y.; Ding, Y.; Hu, X. The Effectiveness of E-Health Interventions on Caregiver Burden, Depression, and Quality of Life in Informal Caregivers of Patients with Cancer: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. J. Nurs. Stud. 2022, 127, 104179. [Google Scholar] [CrossRef]
- Williams, F.; Moghaddam, N.; Ramsden, S.; de Boos, D. Interventions for Reducing Levels of Burden amongst Informal Carers of Persons with Dementia in the Community. A Systematic Review and Meta-Analysis of Randomised Controlled Trials. Aging Ment. Health 2019, 23, 1629–1642. [Google Scholar] [CrossRef] [PubMed]
- Psychiatry. Org—DSM. Available online: https://www.psychiatry.org/psychiatrists/practice/dsm (accessed on 20 September 2022).
- Vandenbrouckel, J.P.; von Elm, E.; Altman, D.G.; Gotzsche, P.C.; Mulrow, C.D.; Pocock, S.J.; Poole, C.; Schlesselman, J.J.; Egger, M. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and Elaboration. PLoS Med. 2007, 4, 1628–1655. [Google Scholar]
- Samara, M.T.; Spineli, L.M.; Furukawa, T.A.; Engel, R.R.; Davis, J.M.; Salanti, G.; Leucht, S. Imputation of Response Rates from Means and Standard Deviations in Schizophrenia. Schizophr. Res. 2013, 151, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the Mean and Variance from the Median, Range, and the Size of a Sample. BMC Med. Res. Methodol. 2005, 5, 13. [Google Scholar] [CrossRef]
- Wallace, B.C.; Dahabreh, I.J.; Trikalinos, T.A.; Lau, J.; Trow, P.; Schmid, C.H. Closing the Gap between Methodologists and End-Users: R as a Computational Back-End. J. Stat. Softw. 2012, 49, 1–15. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring Inconsistency in Meta-Analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Okewole, A.O.; Dada, M.U.; Bello-Mojeed, M.; Ogun, O.C. A Comparison of Clinician and Caregiver Assessment of Functioning in Patients Attending a Child and Adolescent Mental Health Clinic in Nigeria. SAJCH S. Afr. J. Child Health 2016, 10, 8–11. [Google Scholar] [CrossRef]
- Abayomi, O.; Akinhanmi, A.O.; Adelufosi, A.O. Psychiatric Morbidity and Subjective Burden Among Carers of Outpatients of a Psychogeriatric Clinic in Southwestern Nigeria. J. Cross Cult. Gerontol. 2015, 30, 439–450. [Google Scholar] [CrossRef]
- Dada, M.U.; Okewole, N.O.; Ogun, O.C.; Bello-Mojeed, M.A. Factors Associated with Caregiver Burden in a Child and Adolescent Psychiatric Facility in Lagos, Nigeria: A Descriptive Cross Sectional Study. BMC Pediatr. 2011, 11, 110. [Google Scholar] [CrossRef] [PubMed]
- Inogbo, C.F.; Olotu, S.O.; James, B.O.; Nna, E.O. Burden of Care amongst Caregivers Who Are First Degree Relatives of Patients with Schizophrenia. Pan Afr. Med. J. 2017, 28, 4–8. [Google Scholar] [CrossRef] [PubMed]
- Igberase, O.O.; Morakinyo, O.; Lawani, A.O.; James, B.O.; Omoaregba, J.O. Burden of Care among Relatives of Patients with Schizophrenia in Midwestern Nigeria. Int. J. Soc. Psychiatry 2012, 58, 131–137. [Google Scholar] [CrossRef] [PubMed]
- Penteado, C.T.; Loureiro, J.C.; Pais, M.V.; Carvalho, C.L.; Sant’Ana, L.F.G.; Valiengo, L.C.L.; Stella, F.; Forlenza, O.V. Mental Health Status of Psychogeriatric Patients During the 2019 New Coronavirus Disease (COVID-19) Pandemic and Effects on Caregiver Burden. Front. Psychiatry 2020, 11, 578672. [Google Scholar] [CrossRef]
- Andrade, J.J.d.C.; Silva, A.C.O.; Frazão, I.d.S.; Perrelli, J.G.A.; Silva, T.T.d.M.; Cavalcanti, A.M.T.S. Family Functionality and Burden of Family Caregivers of Users with Mental Disorders. Rev. Bras. Enferm. 2021, 74, e20201061. [Google Scholar] [CrossRef]
- Dos Santos, C.A.; Jardim, V.M.d.; Tomasi, E.; Kantorski, L.P.; de Oliveira, M.M.; Coimbra, V.C.C. Minor Psychiatric Disorders among Family Caregivers of Users of Psychosocial Care Centers: Prevalence and Associated Factors. Cienc. E Saude Coletiva 2020, 25, 461–472. [Google Scholar] [CrossRef]
- Pedroso, T.G.; Araújo, A.d.S.; Santos, M.T.S.; Galera, S.A.F.; Cardoso, L. Caregiver Burden and Stress in Psychiatric Hospital Admission. Rev. Bras. Enferm. 2019, 72, 1699–1706. [Google Scholar] [CrossRef]
- Scazufca, M.; Menezes, P.R.; Almeida, O.P. Caregiver Burden in an Elderly Population with Depression in São Paulo, Brazil. Soc. Psychiatry Psychiatr. Epidemiol. 2002, 37, 416–422. [Google Scholar] [CrossRef]
- Maridal, H.K.; Bjørgaas, H.M.; Hagen, K.; Jonsbu, E.; Mahat, P.; Malakar, S.; Dørheim, S. Psychological Distress among Caregivers of Children with Neurodevelopmental Disorders in Nepal. Int. J. Environ. Res. Public. Health 2021, 18, 2460. [Google Scholar] [CrossRef]
- Sharma, R.; Sharma, S.C.; Pradhan, S.N. Assessing Caregiver Burden in Caregivers of Patients with Schizophrenia and Bipolar Affective Disorder in Kathmandu Medical College. J. Nepal Health Res. Counc. 2018, 15, 258–263. [Google Scholar] [CrossRef]
- Mishra, S.K.; Pandey, A.K.; Adhikari, B.R.; Nepal, S. Caregiver Burden and Coping Strategies in Schizophrenia: A Hospital Based Study. J. Psychiatr. Assoc. Nepal 2017, 5, 26–31. [Google Scholar] [CrossRef][Green Version]
- Baykal, S.; Karakurt, M.N.; Çakır, M.; Karabekiroğlu, K. An Examination of the Relations Between Symptom Distributions in Children Diagnosed with Autism and Caregiver Burden, Anxiety and Depression Levels. Community Ment. Health J. 2019, 55, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Cicek, E.; Cicek, I.E.; Kayhan, F.; Uguz, F.; Kaya, N. Quality of Life, Family Burden and Associated Factors in Relatives with Obsessive-Compulsive Disorder. Gen. Hosp. Psychiatry 2013, 35, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Kizilirmak, B.; Küçük, L. Care Burden Level and Mental Health Condition of the Families of Individuals with Mental Disorders. Arch. Psychiatr. Nurs. 2016, 30, 47–54. [Google Scholar] [CrossRef]
- Chien, W.T.; Chan, S.W.C.; Morrissey, J. The Perceived Burden among Chinese Family Caregivers of People with Schizophrenia. J. Clin. Nurs. 2007, 16, 1151–1161. [Google Scholar] [CrossRef]
- Wong, D.F.K.; Lam, A.Y.K.; Chan, S.K.; Chan, S.F. Quality of Life of Caregivers with Relatives Suffering from Mental Illness in Hong Kong: Roles of Caregiver Characteristics, Caregiving Burdens, and Satisfaction with Psychiatric Services. Health Qual. Life Outcomes 2012, 10, 15. [Google Scholar] [CrossRef]
- Kohn-Wood, L.P.; Wilson, M.N. The Context of Caretaking in Rural Areas: Family Factors Influencing the Level of Functioning of Seriously Mentally Ill Patients Living at Home. Am. J. Community Psychol. 2005, 36, 1–13. [Google Scholar] [CrossRef]
- Magaña, S.M.; Ramírez García, J.I.; Hernández, M.G.; Cortez, R. Psychological Distress among Latino Family Caregivers of Adults with Schizophrenia: The Roles of Burden and Stigma. Psychiatr. Serv. 2007, 58, 378–384. [Google Scholar] [CrossRef]
- Chen, H.M.; Hou, S.Y.; Yeh, Y.C.; Chang, C.Y.; Yen, J.Y.; Ko, C.H.; Yen, C.F.; Chen, C.S. Frontal Function, Disability and Caregiver Burden in Elderly Patients with Major Depressive Disorder. Kaohsiung J. Med. Sci. 2010, 26, 548–554. [Google Scholar] [CrossRef]
- Fan, C.C.; Chen, Y.Y. Factors Associated with Care Burden and Quality of Life among Caregivers of the Mentally Ill in Chinese Society. Int. J. Soc. Psychiatry 2011, 57, 195–206. [Google Scholar] [CrossRef]
- Fekih-Romdhane, F.; Ben Ali, S.; Ghazouani, N.; Tira, S.; Cheour, M. Burden in Tunisian Family Caregivers of Older Patients with Schizophrenia Spectrum and Bipolar Disorders; Associations with Depression, Anxiety, Stress, and Quality of Life. Clin. Gerontol. 2020, 43, 545–557. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Lambert, C.E.; Lambert, V.A. Predictors of Family Caregivers’ Burden and Quality of Life When Providing Care for a Family Member with Schizophrenia in the People’s Republic of China. Nurs. Health Sci. 2007, 9, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Caqueo-Urízar, A.; Gutiérrez-Maldonado, J. Burden of Care in Families of Patients with Schizophrenia. Qual. Life Res. 2006, 15, 719–724. [Google Scholar] [CrossRef] [PubMed]
- Rady, A.; Mouloukheya, T.; Gamal, E. Posttraumatic Stress Symptoms, Quality of Life, and Stress Burden in Caregivers of Patients With Severe Mental Illness: An Underestimated Health Concern. Front. Psychiatry 2021, 12, 623499. [Google Scholar] [CrossRef] [PubMed]
- Koutra, K.; Simos, P.; Triliva, S.; Lionis, C.; Vgontzas, A.N. Linking Family Cohesion and Flexibility with Expressed Emotion, Family Burden and Psychological Distress in Caregivers of Patients with Psychosis: A Path Analytic Model. Psychiatry Res. 2016, 240, 66–75. [Google Scholar] [CrossRef]
- Grover, S.; Chakrabarti, S.; Ghormode, D.; Dutt, A. A Comparative Study of Caregivers Perceptions of Health-Care Needs and Burden of Patients with Bipolar Affective Disorder and Schizophrenia. Nord. J. Psychiatry 2015, 69, 629–636. [Google Scholar] [CrossRef]
- Gresswell, I.; Lally, L.; Adamis, D.; McCarthy, G.M. Widening the Net: Exploring Social Determinants of Burden of Informal Carers. Ir. J. Psychol. Med. 2018, 35, 43–51. [Google Scholar] [CrossRef]
- Di Lorenzo, R.; Girone, A.; Panzera, N.; Fiore, G.; Pinelli, M.; Venturi, G.; Magarini, F.; Ferri, P. Empathy and Perceived Burden in Caregivers of Patients with Schizophrenia Spectrum Disorders. BMC Health Serv. Res. 2021, 21, 250. [Google Scholar] [CrossRef]
- Hanzawa, S.; Tanaka, G.; Inadomi, H.; Urata, M.; Ohta, Y. Burden and Coping Strategies in Mothers of Patients with Schizophrenia in Japan. Psychiatry Clin. Neurosci. 2008, 62, 256–263. [Google Scholar] [CrossRef]
- Dalky, H.F.; Qandil, A.M.; Natour, A.S.; Janet, M.C. Quality of Life, Stigma and Burden Perception Among Family Caregivers and Patients with Psychiatric Illnesses in Jordan. Community Ment. Health J. 2017, 53, 266–274. [Google Scholar] [CrossRef]
- Zahid, M.A.; Ohaeri, J.U. Relationship of Family Caregiver Burden with Quality of Care and Psychopathology in a Sample of Arab Subjects with Schizophrenia. BMC Psychiatry 2010, 10, 71. [Google Scholar] [CrossRef]
- Hadryś, T.; Adamowski, T.; Kiejna, A. Mental Disorder in Polish Families: Is Diagnosis a Predictor of Caregiver’s Burden? Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 363–372. [Google Scholar] [CrossRef] [PubMed]
- Gonçalves-Pereira, M.; Xavier, M.; van Wijngaarden, B.; Papoila, A.L.; Schene, A.H.; Caldas-De-Almeida, J.M. Impact of Psychosis on Portuguese Caregivers: A Cross-Cultural Exploration of Burden, Distress, Positive Aspects and Clinical-Functional Correlates. Soc. Psychiatry Psychiatr. Epidemiol. 2013, 48, 325–335. [Google Scholar] [CrossRef] [PubMed]
- Tan, S.C.; Yeoh, A.L.; Choo, I.B.; Huang, A.P.; Ong, S.H.; Ismail, H.; Ang, P.P.; Chan, Y.H. Burden and Coping Strategies Experienced by Caregivers of Persons with Schizophrenia in the Community. J. Clin. Nurs. 2012, 21, 2410–2418. [Google Scholar] [CrossRef]
- Reinares, M.; Vieta, E.; Colom, F.; Martínez-Arán, A.; Torrent, C.; Comes, M.; Goikolea, J.M.; Benabarre, A.; Daban, C.; Sánchez-Moreno, J. What Really Matters to Bipolar Patients’ Caregivers: Sources of Family Burden. J. Affect. Disord. 2006, 94, 157–163. [Google Scholar] [CrossRef] [PubMed]
- Dols, A.; Thesing, C.; Wouters, M.; Theunissen, J.; Sonnenberg, C.; Comijs, H.; Stek, M.L. Burden on Caregivers of Older Patients with Bipolar Disorder. Aging Ment. Health 2018, 22, 686–691. [Google Scholar] [CrossRef]
- Zarit, S.H.; Reever, K.E.; Bach-Peterson, J. Relatives of the Impaired Elderly: Correlates of Feelings of Burden. Gerontologist 1980, 20, 649–655. [Google Scholar] [CrossRef]
- Pai, S.; Kapur, R.L. The Burden on the Family of a Psychiatric Patient: Development of an Interview Schedule. Br. J. Psychiatry J. Ment. Sci. 1981, 138, 332–334. [Google Scholar] [CrossRef]
- Van Wijngaarden, B.; Schene, A.H.; Koeter, M.; Vázquez-Barquero, J.L.; Knudsen, H.C.; Lasalvia, A.; McCrone, P. Caregiving in Schizophrenia: Development, Internal Consistency and Reliability of the Involvement Evaluation Questionnaire—European Version: EPSILON Study 4. Br. J. Psychiatry 2000, 177, s21–s27. [Google Scholar] [CrossRef]
- Robinson, B.C. Validation of a Caregiver Strain Index. J. Gerontol. 1983, 38, 344–348. [Google Scholar] [CrossRef]
- Reinhard, S.C.; Gubman, G.D.; Horwitz, A.V.; Minsky, S. Burden Assessment Scale for Families of the Seriously Mentally Ill. Eval. Program Plan. 1994, 17, 261–269. [Google Scholar] [CrossRef]
- Novak, M.; Guest, C. Application of a Multidimensional Caregiver Burden Inventory. Gerontologist 1989, 29, 798–803. [Google Scholar] [CrossRef] [PubMed]
- Levene, J.E.; Lancee, W.J.; Seeman, M.V. The Perceived Family Burden Scale: Measurement and Validation. Schizophr. Res. 1996, 22, 151–157. [Google Scholar] [CrossRef]
- Morosini, P.I.; Roncone, R.I.; Veltro, F.R.; Palomba, U.; Casacchia, M.A. Routine Assessment Tool in Psychiatry: A Case of Questionnaire of Family Attitudes and Burden. Ital. J. Psychiatry Behav. Sci. 1660, 1, 95–102. [Google Scholar]
- Roberts, C.S.; Feetham, S.L. Assessing Family Functioning across Three Areas of Relationships. Nurs. Res. 1982, 31, 231–235. [Google Scholar] [CrossRef]
- Wong, D.F.K. Stress Factors and Mental Health of Carers with Relatives Suffering from Schizophrenia in Hong Kong: Implications for Culturally Sensitive Practices. Br. J. Soc. Work 2000, 30, 365–382. [Google Scholar] [CrossRef]
- Pot, A.M.; van Dyck, R.; Deeg, D.J.H. Perceived Stress Caused by Informal Caregiving. Construction of a Scale. Tijdschr. Gerontol. Geriatr. 1995, 26, 214–219. [Google Scholar]
- Platt, S.; Weyman, A.; Hirsch, S.; Hewett, S. The Social Behaviour Assessment Schedule (SBAS): Rationale, Contents, Scoring and Reliability of a New Interview Schedule. Soc. Psychiatry 1980, 15, 43–55. [Google Scholar] [CrossRef]
- Thara, R.; Padmavati, R.; Kumar, S.; Srinivasan, L. Burden Assessment Schedule. Indian J. Psychiatry 2022, 40, 21. [Google Scholar]
- Ohaeri, J.U.; Campbell, O.B.; Ilesanmi, A.O.; Omigbodun, A.O. The Psychosocial Burden of Caring for Some Nigerian Women with Breast Cancer and Cervical Cancer. Soc. Sci. Med. 1999, 49, 1541–1549. [Google Scholar] [CrossRef]
- Montgomery, R.J.; Montgomery, R.J.V. Using and Interpreting the Montgomery Borgatta Caregiving Burden Scale. Available online: https://www.researchgate.net/publication/265679222_Using_and_Interpreting_the_Montgomery_Borgatta_Caregiving_Burden_Scale (accessed on 22 September 2022).
- Rezaei, H.; Niksima, S.H.; Ghanei Gheshlagh, R. Burden of Care in Caregivers of Iranian Patients with Chronic Disorders: A Systematic Review and Meta-Analysis. Health Qual. Life Outcomes 2020, 18, 261. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-González, A.M.; Rodríguez-Míguez, E. A Meta-Analysis of the Association between Caregiver Burden and the Dependent’s Illness. J. Women Aging 2019, 32, 220–235. [Google Scholar] [CrossRef] [PubMed]
- Tanna, K.J. Evaluation of Burden Felt by Caregivers of Patients with Schizophrenia and Bipolar Disorder. Ind. Psychiatry J. 2021, 30, 299. [Google Scholar] [CrossRef] [PubMed]
- Cleary, M.; West, S.; Hunt, G.E.; McLean, L.; Kornhaber, R. A Qualitative Systematic Review of Caregivers’ Experiences of Caring for Family Diagnosed with Schizophrenia. Issues Ment. Health Nurs. 2020, 41, 667–683. [Google Scholar] [CrossRef] [PubMed]
- Kate, N.; Grover, S.; Kulhara, P.; Nehra, R. Relationship of Caregiver Burden with Coping Strategies, Social Support, Psychological Morbidity, and Quality of Life in the Caregivers of Schizophrenia. Asian J. Psychiatry 2013, 6, 380–388. [Google Scholar] [CrossRef]
- Van Wijngaarden, B.; Koeter, M.; Knapp, M.; Tansella, M.; Thornicroft, G.; Vázquez-Barquero, J.L.; Schene, A. Caring for People with Depression or with Schizophrenia: Are the Consequences Different? Psychiatry Res. 2009, 169, 62–69. [Google Scholar] [CrossRef]
- Wood, L.; Birtel, M.; Alsawy, S.; Pyle, M.; Morrison, A. Public Perceptions of Stigma towards People with Schizophrenia, Depression, and Anxiety. Psychiatry Res. 2014, 220, 604–608. [Google Scholar] [CrossRef]
- Pescosolido, B.A.; Halpern-Manners, A.; Luo, L.; Perry, B. Trends in Public Stigma of Mental Illness in the US, 1996-2018. JAMA Netw. Open 2021, 4, e2140202. [Google Scholar] [CrossRef]
- Silva, B.; Golay, P.; Morandi, S. Factors Associated with Involuntary Hospitalisation for Psychiatric Patients in Switzerland: A Retrospective Study. BMC Psychiatry 2018, 18, 401. [Google Scholar] [CrossRef]
- Park, J.M.; Kim, M.J. Epidemiologic Characteristics of Hospitalised Patients after Suicidal Acts from 2005 to 2016 in Korea: Analysis of the Korean National Hospital Discharge Survey. J. Affect. Disord. 2020, 275, 238–246. [Google Scholar] [CrossRef]
- Donnelly, N.A.; Hickey, A.; Burns, A.; Murphy, P.; Doyle, F. Systematic Review and Meta-Analysis of the Impact of Carer Stress on Subsequent Institutionalisation of Community-Dwelling Older People. PLoS ONE 2015, 10, e0128213. [Google Scholar] [CrossRef] [PubMed]
- McManus, B.M.; Carle, A.; Acevedo-Garcia, D.; Ganz, M.; Hauser-Cram, P.; McCormick, M. Modeling the Social Determinants of Caregiver Burden among Families of Children with Developmental Disabilities. Am. J. Intellect. Dev. Disabil. 2011, 116, 246–260. [Google Scholar] [CrossRef] [PubMed]
- Schulze, B.; Rössler, W. Caregiver Burden in Mental Illness: Review of Measurement, Findings and Interventions in 2004–2005. Curr. Opin. Psychiatry 2005, 18, 684–691. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).