Adolescents with Neuropsychiatric Disorders during the COVID-19 Pandemic: Focus on Emotional Well-Being and Parental Stress
Abstract
1. Introduction
2. Materials and Methods
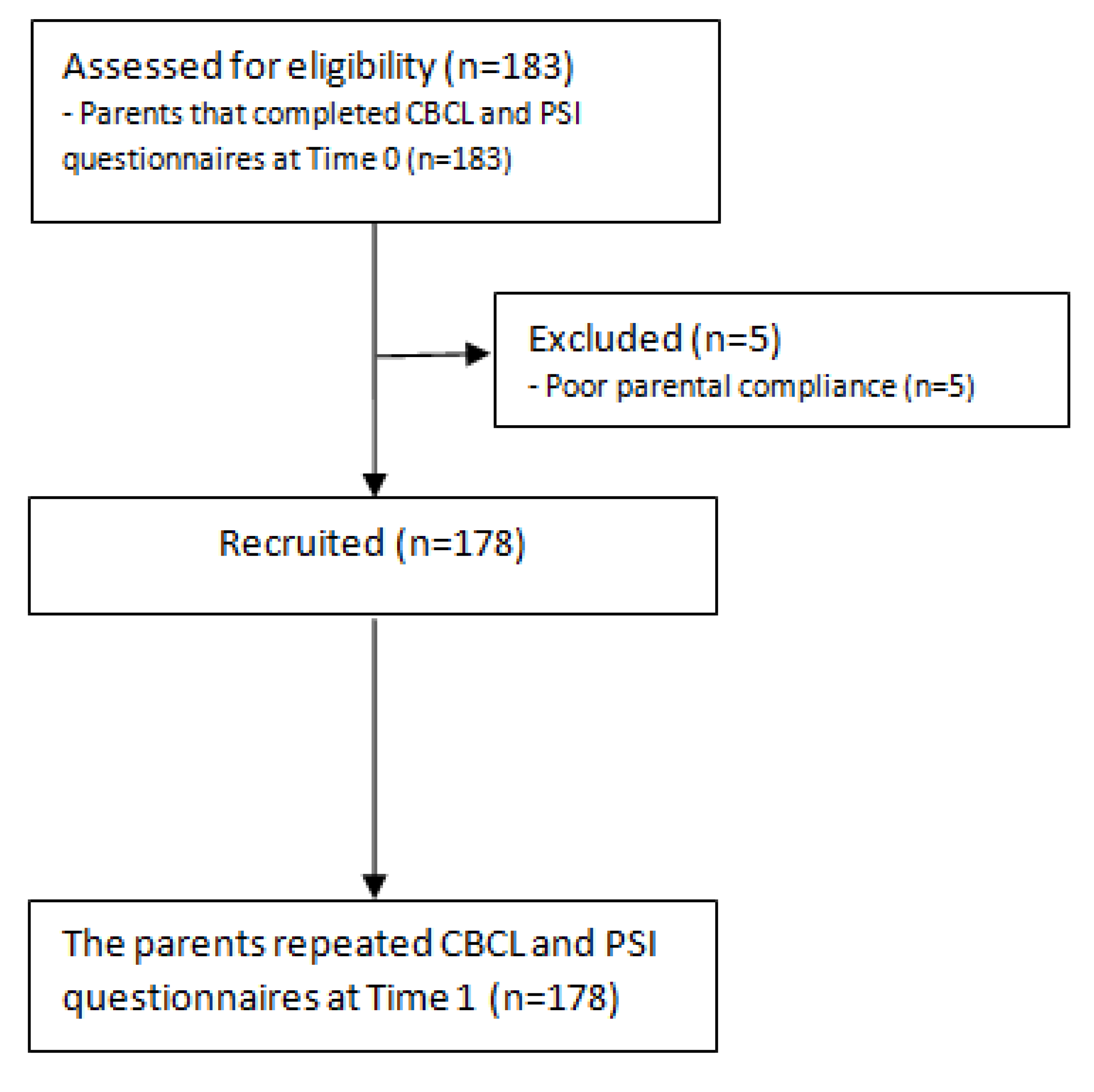
2.1. Participants
2.2. Child Behavior Check List
2.3. ParentingStress Index
2.4. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Mean Score Comparison of CBCL before/during the First Lockdown
3.3. Mean Score Comparison of PSI before/during the First Lockdown
3.4. Correlation Analysis between PSI and CBCL Scales
3.5. Multivariate Linear Regression Analysis at Time 1
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Park, S.E. Epidemiology, virology, and clinical features of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2; Coronavirus Disease-19). Clin. Exp. Pediatr. 2020, 63, 119–124. [Google Scholar] [CrossRef]
- Zhang, Y.; Ma, Z.F. Impact of the COVID-19 Pandemic on Mental Health and Quality of Life among Local Residents in Liaoning Province, China: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 2381. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [PubMed]
- Salanti, G.; Peter, N.; Tonia, T.; Holloway, A.; White, I.R.; Darwish, L.; Low, N.; Egger, M.; Haas, A.D.; Fazel, S.; et al. The Impact of the COVID-19 Pandemic and Associated Control Measures on the Mental Health of the General Population: A Systematic Review and Dose-Response Meta-analysis. Ann. Intern. Med. 2022, 175, 1560–1571. [Google Scholar] [CrossRef]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A Nationwide Survey of Psychological Distress among Italian People during the COVID-19 Pandemic: Immediate Psychological Responses and Associated Factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef] [PubMed]
- López-Ruiz, V.-R.; Alfaro-Navarro, J.L.; Huete-Alcocer, N.; Nevado-Peña, D. Psychological and Social Vulnerability in Spaniards’ Quality of Life in the Face of COVID-19: Age and Gender Results. Int. J. Environ. Res. Public Health 2022, 19, 10269. [Google Scholar] [CrossRef]
- Magson, N.R.; Freeman, J.Y.A.; Rapee, R.M.; Richardson, C.E.; Oar, E.L.; Fardouly, J. Risk and Protective Factors for Prospective Changes in Adolescent Mental Health during the COVID-19 Pandemic. J. Youth Adolesc. 2020, 50, 44–57. [Google Scholar] [CrossRef]
- Garagiola, E.R.; Lam, Q.; Wachsmuth, L.S.; Tan, T.Y.; Ghali, S.; Asafo, S.; Swarna, M. Adolescent Resilience during the COVID-19 Pandemic: A Review of the Impact of the Pandemic on Developmental Milestones. Behav. Sci. 2022, 12, 220. [Google Scholar] [CrossRef] [PubMed]
- Viner, R.; Russell, S.; Saulle, R.; Croker, H.; Stansfield, C.; Packer, J.; Nicholls, D.; Goddings, A.-L.; Bonell, C.; Hudson, L.; et al. School Closures During Social Lockdown and Mental Health, Health Behaviors, and Well-being Among Children and Adolescents During the First COVID-19 Wave. JAMA Pediatr. 2022, 176, 400–409. [Google Scholar] [CrossRef] [PubMed]
- Furstova, J.; Kascakova, N.; Sigmundova, D.; Zidkova, R.; Tavel, P.; Badura, P. Perceived stress of adolescents during the COVID-19 lockdown: Bayesian multilevel modeling of the Czech HBSC lockdown survey. Front. Psychol. 2022, 13, 964313. [Google Scholar] [CrossRef] [PubMed]
- de Figueiredo, C.S.; Sandre, P.C.; Portugal, L.C.L.; M´azala-de-Oliveira, T.; da Silva Chagas, L.; Raony, Í.; Ferreira, E.S.; Giestal-de-Araujo, E.; dos Santos, A.A.; Bomfim, P.O.S. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 106, 110171. [Google Scholar] [CrossRef]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef] [PubMed]
- Jones, E.A.K.; Mitra, A.K.; Bhuiyan, A.R. Impact of COVID-19 on Mental Health in Adolescents: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 2470. [Google Scholar] [CrossRef]
- Meherali, S.; Punjani, N.; Louie-Poon, S.; Abdul Rahim, K.; Das, J.K.; Salam, R.A.; Lassi, Z.S. Mental Health of Children and Adolescents Amidst COVID-19 and Past Pandemics: A Rapid Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 3432. [Google Scholar] [CrossRef]
- Alamolhoda, S.H.; Zare, E.; HakimZadeh, A.; Zalpour, A.; Vakili, F.; Chermahini, R.M.; Ebadifard, R.; Masoumi, M.; Khaleghi, N.; Nasiri, M. Adolescent mental health during COVID-19 pandemics: A systematic review. Int. J. Adolesc. Med. Health 2022. [Google Scholar] [CrossRef]
- Petruzzelli, M.G.; Furente, F.; Colacicco, G.; Annecchini, F.; Margari, A.; Gabellone, A.; Margari, L.; Matera, E. Implication of COVID-19 Pandemic on Adolescent Mental Health: An Analysis of the Psychiatric Counseling from the Emergency Room of an Italian University Hospital in the Years 2019–2021. J. Clin. Med. 2022, 11, 6177. [Google Scholar] [CrossRef] [PubMed]
- Taylor, B.K.; Fung, M.H.; Frenzel, M.R.; Johnson, H.J.; Willett, M.P.; Badura-Brack, A.S.; White, S.F.; Wilson, T.W. Increases in Circulating Cortisol during the COVID-19 Pandemic are Associated with Changes in Perceived Positive and Negative Affect among Adolescents. Res. Child Adolesc. Psychopathol. 2022, 50, 1543–1555. [Google Scholar] [CrossRef]
- Fazzi, E.; Galli, J. New clinical needs and strategies for care in children with neurodisability during COVID-19. Dev. Med. Child Neurol. 2020, 62, 879–880. [Google Scholar] [CrossRef]
- Jesus, T.S.; Bhattacharjya, S.; Papadimitriou, C.; Bogdanova, Y.; Bentley, J.; Arango-Lasprilla, J.C.; Kamalakannan, S.; Refugee Empowerment Task Force, International Networking Group of the American Congress of Rehabilitation Medicine. Lockdown-Related Disparities Experienced by People with Disabilities during the First Wave of the COVID-19 Pandemic: Scoping Review with Thematic Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6178. [Google Scholar] [CrossRef]
- Conti, E.; Sgandurra, G.; De Nicola, G.; Biagioni, T.; Boldrini, S.; Bonaventura, E.; Buchignani, B.; Della Vecchia, S.; Falcone, F.; Fedi, C.; et al. Behavioural and Emotional Changes during COVID-19 Lockdown in an Italian Paediatric Population with Neurologic and Psychiatric Disorders. Brain Sci. 2020, 10, 918. [Google Scholar] [CrossRef]
- Operto, F.F.; Coppola, G.; Vivenzio, V.; Scuoppo, C.; Padovano, C.; de Simone, V.; Rinaldi, R.; Belfiore, G.; Sica, G.; Morcaldi, L.; et al. Impact of COVID-19 Pandemic on Children and Adolescents with Neuropsychiatric Disorders: Emotional/Behavioral Symptoms and Parental Stress. Int. J. Environ. Res. Public Health 2022, 19, 3795. [Google Scholar] [CrossRef] [PubMed]
- Dal Pai, J.; Wolff, C.G.; Aranchipe, C.S.; Kepler, C.K.; Dos Santos, G.A.; Canton, L.A.L.; de Carvalho, A.B.; Richter, S.A.; Nunes, M.L. COVID-19 Pandemic and Autism Spectrum Disorder, Consequences to Children and Adolescents—A Systematic Review. Rev. J. Autism Dev. Disord. 2022, 1–26. [Google Scholar] [CrossRef]
- Corbett, B.A.; Muscatello, R.A.; Klemencic, M.E.; Schwartzman, J.M. The impact of COVID -19 on stress, anxiety, and coping in youth with and without autism and their parents. Autism Res. 2021, 14, 1496–1511. [Google Scholar] [CrossRef] [PubMed]
- Theis, N.; Campbell, N.; De Leeuw, J.; Owen, M.; Schenke, K.C. The effects of COVID-19 restrictions on physical activity and mental health of children and young adults with physical and/or intellectual disabilities. Disabil. Health J. 2021, 14, 101064. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Shuai, L.; Yu, H.; Wang, Z.; Qiu, M.; Lu, L.; Cao, X.; Xia, W.; Wang, Y.; Chen, R. Acute stress, behavioural symptoms and mood states among school-age children with attention-deficit/hyperactive disorder during the COVID-19 outbreak. Asian J. Psychiatry 2020, 51, 102077. [Google Scholar] [CrossRef]
- Karci, C.K.; Gurbuz, A.A. Challenges of children and adolescents with attention-deficit/hyperactivity disorder during the COVID-19 pandemic. Nord. J. Psychiatry 2021, 76, 372–379. [Google Scholar] [CrossRef] [PubMed]
- Pasca, L.; Zanaboni, M.P.; Grumi, S.; Totaro, M.; Ballante, E.; Varesio, C.; De Giorgis, V. Impact of COVID-19 pandemic in pediatric patients with epilepsy with neuropsychiatric comorbidities: A telemedicine evaluation. Epilepsy Behav. 2021, 115, 107519. [Google Scholar] [CrossRef]
- Reilly, C.; Muggeridge, A.; Cross, J.H. The perceived impact of COVID-19 and associated restrictions on young people with epilepsy in the UK: Young people and caregiver survey. Seizure 2021, 85, 111–114. [Google Scholar] [CrossRef]
- Sesso, G.; Bonaventura, E.; Buchignani, B.; Della Vecchia, S.; Fedi, C.; Gazzillo, M.; Micomonaco, J.; Salvati, A.; Conti, E.; Cioni, G.; et al. Parental Distress in the Time of COVID-19: A Cross-Sectional Study on Pediatric Patients with Neuropsychiatric Conditions during Lockdown. Int. J. Environ. Res. Public Health 2021, 18, 7902. [Google Scholar] [CrossRef]
- Raffagnato, A.; Iannattone, S.; Tascini, B.; Venchiarutti, M.; Broggio, A.; Zanato, S.; Traverso, A.; Mascoli, C.; Manganiello, A.; Miscioscia, M.; et al. The COVID-19 Pandemic: A Longitudinal Study on the Emotional-Behavioral Sequelae for Children and Adolescents with Neuropsychiatric Disorders and Their Families. Int. J. Environ. Res. Public Health 2021, 18, 9880. [Google Scholar] [CrossRef]
- Friesen, K.A.; Weiss, J.A.; Howe, S.J.; Kerns, C.M.; McMorris, C.A. Mental Health and Resilient Coping in Caregivers of Autistic Individuals during the COVID-19 Pandemic: Findings from the Families Facing COVID Study. J. Autism Dev. Disord. 2021, 52, 3027–3037. [Google Scholar] [CrossRef] [PubMed]
- Lee, V.; Albaum, C.; Modica, P.T.; Ahmad, F.; Gorter, J.W.; Khanlou, N.; McMorris, C.; Lai, J.; Harrison, C.; Hedley, T.; et al. The impact of COVID -19 on the mental health and wellbeing of caregivers of autistic children and youth: A scoping review. Autism Res. 2021, 14, 2477–2494. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, H.; Shang, C.; Liang, H.; Liu, W.; Han, B.; Xia, W.; Zou, M.; Sun, C. Mental health issues in parents of children with autism spectrum disorder: A multi-time-point study related to COVID-19 pandemic. Autism Res. 2022. [Google Scholar] [CrossRef]
- De Giacomo, A.; Pedaci, C.; Palmieri, R.; Simone, M.; Costabile, A.; Craig, F. Psychological impact of the SARS-CoV-2 pandemic in children with neurodevelopmental disorders and their families: Evaluation before and during COVID-19 outbreak among an Italian sample. Riv. Psichiatr. 2021, 56, 205–210. [Google Scholar] [CrossRef] [PubMed]
- Bailey, T.; Hastings, R.P.; Totsika, V. COVID-19 impact on psychological outcomes of parents, siblings and children with intellectual disability: Longitudinal before and during lockdown design. J. Intellect. Disabil. Res. 2021, 65, 397–404. [Google Scholar] [CrossRef]
- Cusinato, M.; Iannattone, S.; Spoto, A.; Poli, M.; Moretti, C.; Gatta, M.; Miscioscia, M. Stress, Resilience, and Well-Being in Italian Children and Their Parents during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2020, 17, 8297. [Google Scholar] [CrossRef]
- Marchetti, D.; Fontanesi, L.; Mazza, C.; Di Giandomenico, S.; Roma, P.; Verrocchio, M.C. Parenting-Related Exhaustion During the Italian COVID-19 Lockdown. J. Pediatr. Psychol. 2020, 45, 1114–1123. [Google Scholar] [CrossRef]
- Alhuzimi, T. Stress and emotional wellbeing of parents due to change in routine for children with Autism Spectrum Disorder (ASD) at home during COVID-19 pandemic in Saudi Arabia. Res. Dev. Disabil. 2021, 108, 103822. [Google Scholar] [CrossRef] [PubMed]
- Bitsika, V.; Sharpley, C.F.; Andronicos, N.M.; Agnew, L.L. Prevalence, structure and correlates of anxiety-depression in boys with an autism spectrum disorder. Res. Dev. Disabil. 2016, 49-50, 302–311. [Google Scholar] [CrossRef]
- Willner, P.; Rose, J.; Kroese, B.S.; Murphy, G.H.; Langdon, P.E.; Clifford, C.; Hutchings, H.; Watkins, A.; Hiles, S.; Cooper, V. Effect of the COVID-19 pandemic on the mental health of carers of people with intellectual disabilities. J. Appl. Res. Intellect. Disabil. 2020, 33, 1523–1533. [Google Scholar] [CrossRef] [PubMed]
- Rohwerder, B.; Wong, S.; Pokharel, S.; Khadka, D.; Poudyal, N.; Prasai, S.; Shrestha, N.; Wickenden, M.; Morrison, J. Describing adolescents with disabilities’ experiences of COVID-19 and other humanitarian emergencies in low- and middle-income countries: A scoping review. Glob. Health Action 2022, 15, 2107350. [Google Scholar] [CrossRef] [PubMed]
- Shorey, S.; Lau, L.S.T.; Tan, J.X.; Ng, E.D.; Aishworiya, R. Families with Children with Neurodevelopmental Disorders During COVID-19: A Scoping Review. J. Pediatr. Psychol. 2021, 46, 514–525. [Google Scholar] [CrossRef] [PubMed]
- Achenbach, T.; Rescorla, L. Manual for the ASEBA School-Age Forms and Profiles: An Integrated System of Multi-Informant Assessment; University of Vermont, Research Center for Children, Youth, & Families: Burlington, VT, USA, 2001. [Google Scholar]
- Guarino, A.; Laghi, F.; Serantoni, G.; Di Blasio, P.; Camisasca, E. Parenting Stress Index—Fourth Edition (PSI-4); Giunti, O.S.: Florence, Italy, 2016. [Google Scholar]
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect size estimates: Current use, calculations, and interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef]
- Racine, N.; Cooke, J.E.; Eirich, R.; Korczak, D.J.; McArthur, B.; Madigan, S. Child and adolescent mental illness during COVID-19: A rapid review. Psychiatry Res. 2020, 292, 113307. [Google Scholar] [CrossRef] [PubMed]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The Effect of COVID-19 on Youth Mental Health. Psychiatr. Q. 2020, 91, 841–852. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Kakade, M.; Fuller, C.J.; Fan, B.; Fang, Y.; Kong, J.; Guan, Z.; Wu, P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 2012, 53, 15–23. [Google Scholar] [CrossRef]
- Bai, M.-S.; Miao, C.-Y.; Zhang, Y.; Xue, Y.; Jia, F.-Y.; Du, L. COVID-19 and mental health disorders in children and adolescents (Review). Psychiatry Res. 2022, 317, 114881. [Google Scholar] [CrossRef]
- Rider, E.A.; Ansari, E.; Varrin, P.H.; Sparrow, J. Mental health and wellbeing of children and adolescents during the COVID-19 pandemic. BMJ 2021, 374, n1730. [Google Scholar] [CrossRef]
- Caffo, E.; Scandroglio, F.; Asta, L. Debate: COVID-19 and psychological well-being of children and adolescents in Italy. Child Adolesc. Ment. Health 2020, 25, 167–168. [Google Scholar] [CrossRef]
- Urban, T.H.; Friedman, D.; Kaskas, M.M.; Caruso, A.J.; Canenguez, K.M.; Rotter, N.; Wozniak, J.; Basu, A. Brief report of protective factors associated with family and parental well-being during the COVID-19 pandemic in an outpatient child and adolescent psychiatric clinic. Front. Psychol. 2022, 13, 883955. [Google Scholar] [CrossRef]
- Dollberg, D.G.; Hanetz-Gamliel, K.; Levy, S. COVID-19, child’s behavior problems, and mother’s anxiety and mentalization: A mediated moderation model. Curr. Psychol. 2021, Nov 9, 1–12. [Google Scholar] [CrossRef]
- Alenezi, S.; Temsah, M.-H.; Alyahya, A.S.; Almadani, A.H.; Almarshedi, A.; Algazlan, M.S.; Alnemary, F.; Bashiri, F.A.; Alkhawashki, S.H.; Altuwariqi, M.H.; et al. Mental health impact of COVID-19 on Saudi families and children with special educational needs and disabilities in Saudi Arabia: A national perspective. Front. Public Health 2022, 10, 992658. [Google Scholar] [CrossRef] [PubMed]
- Panda, P.K.; Gupta, J.; Chowdhury, S.R.; Kumar, R.; Meena, A.K.; Madaan, P.; Sharawat, I.K.; Gulati, S. Psychological and Behavioral Impact of Lockdown and Quarantine Measures for COVID-19 Pandemic on Children, Adolescents and Caregivers: A Systematic Review and Meta-Analysis. J. Trop. Pediatr. 2020, 67, fmaa122. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Zhou, S. Parental worry, family-based disaster education and children’s internalizing and externalizing problems during the COVID-19 pandemic. Psychol.Trauma 2021, 13, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Doyle, A.E.; Colvin, M.K.; Beery, C.S.; Koven, M.R.; Vuijk, P.J.; Braaten, E.B. Distinct patterns of emotional and behavioral change in child psychiatry outpatients during the COVID-19 pandemic. Child Adolesc. Psychiatry Ment. Health 2022, 16, 12. [Google Scholar] [CrossRef]
- Soriano-Ferrer, M.; Morte-Soriano, M.R.; Begeny, J.; Piedra-Martínez, E. Psychoeducational Challenges in Spanish Children with Dyslexia and Their Parents’ Stress During the COVID-19 Pandemic. Front. Psychol. 2021, 12, 648000. [Google Scholar] [CrossRef]
- Santa-Cruz, C.; Espinoza, V.; Donoso, J.; Rosas, R.; Badillo, D. How did the pandemic affect the socio-emotional well-being of Chilean schoolchildren? A longitudinal study. Sch. Psychol. 2022, 37, 85–96. [Google Scholar] [CrossRef]
- Germanò, E.; Gagliano, A.; Arena, C.; Cedro, C.; Vetri, L.; Operto, F.F.; Pastorino, G.M.G.; Marotta, R.; Roccella, M. Reading-writing di-sorder in children with idiopathic epilepsy. EpilepsyBehave 2020, 111, 107118. [Google Scholar] [CrossRef]
- Sadeghi, N.; Fors, P.Q.; Eisner, L.; Taigman, J.; Qi, K.; Gorham, L.S.; Camp, C.C.; O’Callaghan, G.; Rodriguez, D.; McGuire, J.; et al. Mood and Behaviors of Adolescents with Depression in a Longitudinal Study Before and During the COVID-19 Pandemic. J. Am. Acad. Child Adolesc. Psychiatry 2022, 61, 1341–1350. [Google Scholar] [CrossRef]
- Vasa, R.A.; Singh, V.; Holingue, C.; Kalb, L.G.; Jang, Y.; Keefer, A. Psychiatric problems during the COVID-19 pandemic in children with autism spectrum disorder. Autism Res. 2021, 14, 2113–2119. [Google Scholar] [CrossRef]
- Lugo-Marín, J.; Gisbert-Gustemps, L.; Setien-Ramos, I.; Español-Martín, G.; Ibañez-Jimenez, P.; Forner-Puntonet, M.; Arteaga-Henríquez, G.; Soriano-Día, A.; Duque-Yemail, J.D.; Ramos-Quiroga, J.A. COVID-19 pandemic effects in people with Autism Spectrum Disorder and their caregivers: Evaluation of social distancing and lockdown impact on mental health and general status. Res. Autism Spectr. Disord. 2021, 83, 101757. [Google Scholar] [CrossRef] [PubMed]
- Behrmann, J.T.; Blaabjerg, J.; Jordansen, J.; Jensen de López, K.M. Systematic Review: Investigating the Impact of COVID-19 on Mental Health Outcomes of Individuals with ADHD. J. Atten. Disord. 2021, 26, 959–975. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, R.; Karlov, L.; Maugeri, N.; Di Silvestre, S.; Eapen, V. Impact of the COVID-19 Pandemic on Family Wellbeing in the Context of Neurodevelopmental Disorders. Neuropsychiatr. Dis. Treat. 2021, 17, 3007–3014. [Google Scholar] [CrossRef] [PubMed]
- Costa, N.M.; Weems, C.F.; Pellerin, K.; Dalton, R. Parenting Stress and ChildhoodPsycho-pathology: An Examination of Specificity to Internalizing and Externalizing Symptoms. J. Psychopathol. Behav. Assess. 2006, 28, 113–122. [Google Scholar] [CrossRef]
- Operto, F.F.; Pastorino, G.M.G.; Scuoppo, C.; Padovano, C.; Vivenzio, V.; Pistola, I.; Belfiore, G.; Rinaldi, R.; de Simone, V.; Coppola, G. Adaptive Behavior, Emotional/Behavioral Problems and Parental Stress in Children with Autism Spectrum Disorder. Front. Neurosci. 2021, 15, 751465. [Google Scholar] [CrossRef] [PubMed]
- Operto, F.; Smirni, D.; Scuoppo, C.; Padovano, C.; Vivenzio, V.; Quatrosi, G.; Carotenuto, M.; Precenzano, F.; Pastorino, G. Neuropsychological Profile, Emotional/Behavioral Problems, and Parental Stress in Children with Neurodevelopmental Disorders. Brain Sci. 2021, 11, 584. [Google Scholar] [CrossRef]
- Operto, F.F.; Mazza, R.; Pastorino, G.M.G.; Campanozzi, S.; Verrotti, A.; Coppola, G. Parental stress in a sample of children with epilepsy. Acta Neurol. Scand. 2019, 140, 87–92. [Google Scholar] [CrossRef] [PubMed]
- Operto, F.F.; Mazza, R.; Pastorino, G.M.G.; Campanozzi, S.; Margari, L.; Coppola, G. Parental stress in pediatric epilepsy after therapy withdrawal. Epilepsy Behav. 2019, 94, 239–242. [Google Scholar] [CrossRef]
| Participants n = 178 | |
|---|---|
| child age (mean ± SD) | 15.34 ± 2.17 |
| sex | |
| male | 108 (61%) |
| female | 70 (39%) |
| father age (mean ± SD) | 46.28 ± 6.39 |
| mother age (mean ± SD) | 43.63 ± 5.70 |
| maternal education level (mean ± SD) * | 13.98 ± 4.16 |
| paternal education level (mean ± SD) * | 14.00 ± 3.97 |
| Principal Diagnosis | Age (Years) | Sex | Father Age (Years) | Mother Age (Years) | Neuro-Psychiatric Comorbidities | Other Clinical Conditions | Drug Therapy |
|---|---|---|---|---|---|---|---|
| epilepsy n = 66 | 15.99 ± 1.96 | male = 41 (62%) | 48.05±6.02 | 45.18±5.52 | 20 (30%) | 14 (21%) | 60 (91%) |
| autism spectrum disorder n = 26 | 15.35 ± 2.61 | male = 18 (69%) | 49.68±6.94 | 47.24±6.30 | 17 (65%) | 10 (38%) | 9 (345%) |
| specific learning disorders n = 26 | 13.96 ± 1.91 | male = 15 (58%) | 41.85±4.71 | 39.38±3.71 | 6 (23%) | 5 (19%) | 0 (0%) |
| anxiety disorders n = 15 | 15.17 ± 2.22 | male = 6 (40%) | 45.40±7.08 | 43.80±4.52 | 8 (53%) | 2 (13%) | 12 (80%) |
| intellectual disability n = 13 | 15.92 ± 1.85 | male = 10 (77%) | 45.31±4.75 | 42.31±5.53 | 8 (61%) | 4 (31%) | 3 (23%) |
| attention-deficit/hyperactivity disorder n = 11 | 15.09 ± 4.38 | male = 7 (64%) | 45.09±11.91 | 42.09±11.10 | 3 (27%) | 3 (27%) | 9 (82%) |
| behavioral disorders n = 11 | 15.09 ± 3.30 | male = 7 (64%) | 44.36±9.36 | 41.73±9.00 | 3 (27%) | 2 (18%) | 5 (45%) |
| mood disorders n = 10 | 14.70 ± 2.07 | male = 4 (40%) | 44.00±7.94 | 40.70±5.19 | 7 (70%) | 2 (20%) | 10 (100%) |
| Total sample n = 178 | 15.34 ± 2.17 | male = 108 (61%) | 46.28±6.39 | 43.63±5.70 | 72 (40%) | 42 (24%) | 108 (61%) |
| Standardized Neuropsychologicaltest | Time 0 (Mean ± SD) | Time 1 (Mean ± SD) | Statistic (Wilcoxon Test) | p-Value | η2 = z2/N − 1 | r = z/√(N × 2) |
|---|---|---|---|---|---|---|
| Parental Stress Index (PSI) | ||||||
| Parental Distress (PD) | 59.86 ± 28.64 | 72.67 ± 27.80 | z = −7.918 | p < 0.001 | 0.354 | 0.420 |
| Parent–child Difficult Interaction (P-CDI) | 63.82 ± 23.78 | 77.58 ± 23.44 | z = −7.703 | p < 0.001 | 0.335 | 0.409 |
| Difficult Child (DC) | 65.10 ± 26.35 | 77.48 ± 24.99 | z = −7.242 | p < 0.001 | 0.296 | 0.385 |
| Total Stress (TS) | 63.68 ± 25.09 | 77.19 ± 25.22 | z = −8.487 | p < 0.001 | 0.406 | 0.451 |
| Child Behavior Check List (CBCL) 6–18 years | p < 0.001 | |||||
| Anxiety/Depression | 59.52 ± 7.66 | 69.49 ± 13.24 | z = −9.113 | p < 0.001 | 0.469 | 0.484 |
| Withdrawal/Depression | 61.38 ± 8.60 | 69.92 ± 12.99 | z = −8.391 | p < 0.001 | 0.397 | 0.446 |
| Somatic complaints | 58.35 ± 7.86 | 69.60 ± 13.65 | z = −8.642 | p < 0.001 | 0.421 | 0.459 |
| Socialization | 62.59 ± 9.05 | 70.66 ± 13.04 | z = −7.974 | p < 0.001 | 0.359 | 0.423 |
| Thought problems | 61.67 ± 10.57 | 66.08 ± 11.90 | z= −5.342 | p < 0.001 | 0.161 | 0.283 |
| Attention problems | 62.01 ± 8.85 | 68.88 ± 11.78 | z = −8.255 | p < 0.001 | 0.385 | 0.438 |
| Rule-breaking behavior | 58.44 ± 7.43 | 65.61 ± 12.59 | z = −8.267 | p < 0.001 | 0.386 | 0.439 |
| Aggressive behavior | 61.28 ± 10.99 | 67.35 ± 13.26 | z = −7.695 | p < 0.001 | 0.334 | 0.409 |
| Affective problems | 61.93 ± 7.85 | 69.09 ± 11.73 | z = −8.501 | p < 0.001 | 0.408 | 0.451 |
| Anxiety problems | 61.96 ± 7.70 | 69.95 ± 11.70 | z = −8.796 | p < 0.001 | 0.437 | 0.467 |
| Somatic Problems | 56.90 ± 8.06 | 65.08 ± 11.39 | z = −8.058 | p < 0.001 | 0.366 | 0.428 |
| ADHD | 60.46 ± 7.66 | 66.62 ± 10.17 | z= −8.036 | p < 0.001 | 0.364 | 0.427 |
| Oppositional-defiant problems | 58.33 ± 7.66 | 64.57 ± 11.26 | z= −8.006 | p < 0.001 | 0.362 | 0.425 |
| Conduct problems | 57.28 ± 7.13 | 63.29 ± 11.08 | z = −8.110 | p < 0.001 | 0.371 | 0.431 |
| Internalizing problems | 59.66 ± 10.24 | 68.89 ± 13.35 | z = −9.017 | p < 0.001 | 0.459 | 0.479 |
| Externalizing problems | 57.65 ± 10.28 | 65.88 ± 14.22 | z = −8.198 | p < 0.001 | 0.379 | 0.435 |
| Total Problem | 60.17 ± 9.87 | 69.19 ± 13.93 | z = −9.159 | p < 0.001 | 0.473 | 0.486 |
| CBCL Total Problems | CBCL Externalizing Problems | CBCL Internalizing Problems | |||
|---|---|---|---|---|---|
| Parental stress | Parental Distress | r | 0.454 | 0.407 | 0.466 |
| p-value | <0.001 | <0.001 | <0.001 | ||
| Parent–child Difficult Interaction | r | 0.490 | 0.401 | 0.499 | |
| p-value | <0.001 | <0.001 | <0.001 | ||
| Difficult Child | r | 0.504 | 0.424 | 0.495 | |
| p-value | <0.001 | <0.001 | <0.001 | ||
| Total Stress | r | 0.546 | 0.466 | 0.556 | |
| p-value | <0.001 | <0.001 | <0.001 |
| Sex | Age | Diagnosis | ||
|---|---|---|---|---|
| Child Behavior Check List (CBCL) | Total Problems | p = 0.261 | p = 0.849 | p < 0.001 |
| Externalizing Problems | p = 0.657 | p = 0.879 | p < 0.001 | |
| Internalizing | p = 0.294 | p = 0.562 | p < 0.001 | |
| Parental Stress Index (PSI) | Parental Distress | p = 0.388 | p = 0.320 | p < 0.001 |
| Parent–child Dysfunctional Interaction | p = 0.644 | p = 0.669 | p = 0.001 | |
| Difficult Child | p = 0.822 | p = 0.710 | p = 0.005 | |
| Total Stress | p = 0.613 | p = 0.432 | p < 0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Operto, F.F.; Scaffidi Abbate, C.; Piscitelli, F.T.; Olivieri, M.; Rizzo, L.; Sica, G.; Labate, A.; Roccella, M.; Carotenuto, M.; Pastorino, G.M.G. Adolescents with Neuropsychiatric Disorders during the COVID-19 Pandemic: Focus on Emotional Well-Being and Parental Stress. Healthcare 2022, 10, 2368. https://doi.org/10.3390/healthcare10122368
Operto FF, Scaffidi Abbate C, Piscitelli FT, Olivieri M, Rizzo L, Sica G, Labate A, Roccella M, Carotenuto M, Pastorino GMG. Adolescents with Neuropsychiatric Disorders during the COVID-19 Pandemic: Focus on Emotional Well-Being and Parental Stress. Healthcare. 2022; 10(12):2368. https://doi.org/10.3390/healthcare10122368
Chicago/Turabian StyleOperto, Francesca Felicia, Costanza Scaffidi Abbate, Francesco Tommaso Piscitelli, Miriam Olivieri, Luigi Rizzo, Gianpiero Sica, Angelo Labate, Michele Roccella, Marco Carotenuto, and Grazia Maria Giovanna Pastorino. 2022. "Adolescents with Neuropsychiatric Disorders during the COVID-19 Pandemic: Focus on Emotional Well-Being and Parental Stress" Healthcare 10, no. 12: 2368. https://doi.org/10.3390/healthcare10122368
APA StyleOperto, F. F., Scaffidi Abbate, C., Piscitelli, F. T., Olivieri, M., Rizzo, L., Sica, G., Labate, A., Roccella, M., Carotenuto, M., & Pastorino, G. M. G. (2022). Adolescents with Neuropsychiatric Disorders during the COVID-19 Pandemic: Focus on Emotional Well-Being and Parental Stress. Healthcare, 10(12), 2368. https://doi.org/10.3390/healthcare10122368










