Abstract
(1) Introduction: Neurologic music therapy (NMT) is a non-pharmacological approach of interaction through the therapeutic use of music in motor, sensory and cognitive dysfunctions caused by damage or diseases of the nervous system. (2) Objective: This study aimed to critically appraise the available literature on the application of particular NMT techniques in the rehabilitation of geriatric disorders. (3) Methods: PubMed, ScienceDirect and EBSCOhost databases were searched. We considered randomized controlled trials (RCTs) from the last 12 years using at least one of the NMT techniques from the sensorimotor, speech/language and cognitive domains in the therapy of patients over 60 years old and with psychogeriatric disorders. (4) Results: Of the 255 articles, 8 met the inclusion criteria. All papers in the final phase concerned the use of rhythmic auditory stimulation (RAS) (sensorimotor technique) in the rehabilitation of both Parkinson’s disease (PD) patients (six studies) and stroke patients (SPs) (two studies). (5) Conclusion: All reports suggest that the RAS technique has a significant effect on the improvement of gait parameters and the balance of PD patients and SPs, as well as the risk of falls in PD patients.
1. Introduction
The ageing of the population is a long-term phenomenon that has been visible in Europe for several decades. The increasing number and participation of older people in society not only creates a number of opportunities but also new challenges, especially related to public health [1].
Psychopathology in geriatrics should be considered by taking into account the groups of causes of mental disorders in old age to which they belong: Psychological and social factors related to old age, Ageing of the body along with neurodegenerative processes, which are manifested by psycho-organic disorders, Somatic diseases and their treatment, The course of mental disorders that started in earlier stages of life and changes in their psychological image [2].
NMT is a non-pharmacological method of interaction through the therapeutic use of music in motor, sensory and cognitive dysfunctions caused by damage or diseases of the nervous system. The supporters of this approach treat music as a stimulus that directly affects the neurophysiological processes of the brain. The use of music in neurorehabilitation is based on neurophysiological theories and research on the influence of music production and perception on cognitive processes and principles of learning through movement [3,4,5].
NMT consists of 20 standardized and clinically applied techniques that rehabilitate three areas: sensorimotor, speech/language and cognitive (Table 1) [6]. Therapeutic activities are aimed at achieving non-musical goals. To optimize this process, NMT uses the Transformation Design Model (TDM) to translate theoretical knowledge into clinical practice. It promotes the effective assessment, design and implementation of therapeutic musical interventions [4,7].

Table 1.
The division of neurologic music therapy techniques into three main groups that rehabilitate certain areas and the specific techniques used in them.
With this systematic review we tried to find answers to the following questions: Can NMT, as a relatively low-cost and non-invasive method, be effective in the rehabilitation of geriatric patients? Which techniques and in which diseases and disorders is NMT successfully applied? In addition, we wanted to locate areas (therapy and rehabilitation of individual conditions) where RCTs are being conducted (providing strong evidence of effectiveness). This study aimed to critically appraise the literature on the application of NMT techniques in the rehabilitation of psychogeriatric disorders.
2. Materials and Methods
2.1. Search Strategy
We carried out a systematic review of randomized controlled trials (RCTs) on the benefits of NMT in the treatment of psychogeriatric disorders. The verification system was based on PRISMA guidelines and Cochrane Handbook for Systematic Reviews of Interventions to ensure transparent and complete reporting in our study [8,9,10]. We searched the following electronic databases: PubMed, ScienceDirect and EBSCOhost. In the selection of keywords, the names of individual NMT techniques from all three areas were considered [File S1]. Data extraction was performed by two researchers and then checked by a third one. Our strategy included three phases. Initially, potentially valuable articles were identified by their titles. Screening of abstracts was performed by two independent reviewers. Disagreements relating to the full text inclusion were solved by a third reviewer. After narrowing the number of articles to those meeting the inclusion criteria, we gained access to full versions of the publications, eventually qualifying the articles for review (Figure 1).
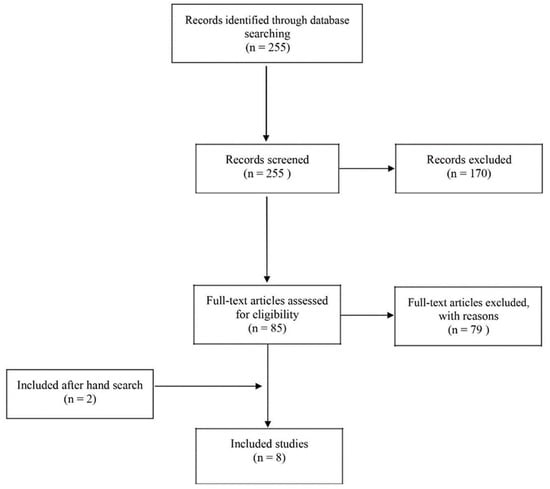
Figure 1.
Flow chart of systematic review process.
2.2. Inclusion Criteria
The articles selected for this literature review fulfilled the following inclusion criteria: published in English in the last 12 years, i.e., from 1 January 2010 to 1 March 2022, and including patients aged 60 years and over who have been diagnosed with geriatric disorders and who have been rehabilitated using at least one of the NMT techniques. The search excluded studies in the form of letters, preliminary findings, literature reviews and case studies. The following information was extracted from each article: year of publication, study group characteristics, therapies used, duration of intervention, questionnaire(s)/tool(s) used to measure and results indicating the degree of efficiency before and after therapy.
2.3. Assessment of Risk of Bias
Risk of bias for the included studies was assessed independently by two reviewers, who were supported by a third researcher in case of disagreement using the Risk of Bias 2 (RoB 2) tool (Figure 2). Assessment was conducted following the criteria stated by the Cochrane Collaboration in the Cochrane Handbook for Systematic Reviews of Interventions [11]. Methodological quality of studies was recorded in the risk of bias table [File S2].
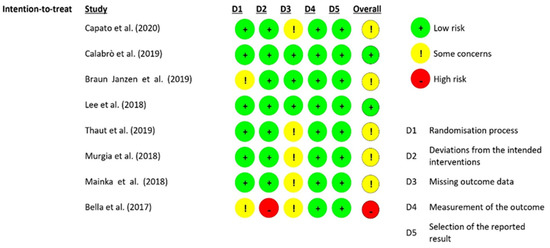
Figure 2.
Risk of bias in included studies [12,13,14,15,16,17,18,19].
3. Results
3.1. Literature Search
In the first phase of the electronic literature search, 255 potentially relevant publications were found. A total of 170 studies were rejected, because the abstracts did not meet the inclusion criteria. Based on the available summaries, 85 publications were accepted for further full-text analysis. In addition, a manual search of the cited literature within approved articles was carried out. Thus, two additional studies were included. Finally, we included eight articles in this systematic review. The most common reason for rejecting an article in the second phase was the use of music without therapy or a different method of music therapy. The second most common reasons for rejection were too big a difference in the ages of participants and the type of study. The characteristics of the studies qualifying for review and a full list of rejected papers with motivation are included in the Supplementary Materials [Files S3 and S4].
3.2. Participants and Study Characteristics
Due to the specificity of the population of elderly people with geriatric disorders in the selected studies, it was not possible to create unambiguously detailed characteristics of the studied groups. However, six of the studies that were qualified for the final stage concerned the use of rhythmic auditory stimulation (RAS) for gait rehabilitation in Parkinson’s disease (PD) patients and two studies concerned RAS in stroke patients (SPs).
3.3. RAS in Parkinson’s Disease
Six out of eight studies were concerned with the use of RAS in the rehabilitation of gait parameters in PD. It is difficult to compare the results because of the different modifications to the classic RAS training. However, the articles focused on evaluating the parameters of gait, balance, and falls. Multimodal balance training supported by RAS can improve balance performance in PD patients with mild cognitive impairment and stage 4 H&Y [12]. Significant improvements in PD gait were obtained after RAS training in parameters (speed; stride length; cadence; right and left ankle dorsiflexion; fall index and fear of falling; reduction in patient step time variability) [13,14,15]. Additionally, finger tapping training led to a significant increase in gait speed (p < 0.005) and gait cadence [16].
3.3.1. RAS and Multimodal Balance Training in PD
The study by Capato and colleagues (2020) compared RAS-supported multimodal balance training with regular multimodal training. Results revealed that, immediately after the intervention, both intervention groups improved significantly at the Mini-Best performance level. In both groups, the results remained at the level of 1 month of observation [12]. Outcomes were maintained only in the RAS-supported intervention group after 6 months of follow-up. In this group, improvements were registered in Part 3 of the Movement Disorder Society–Unified Parkinson’s Disease Rating Scale (MDS-UPDRS) and in the Berg Balance Scale (BBS) immediately after the intervention.
3.3.2. RAS and Treadmill Training in IPD
Calabrò and colleagues (2019) assessed the effectiveness of treadmill training in combination with RAS for mobility, balance and gait parameters by correlating electroencephalography (EEG) changes with behavioural changes (gait) in order to determine the alleged neurophysiological basis for gait improvement [15]. Significant improvements were observed in functional gait assessment (p < 0.001), gait quality index (p < 0.001), Unified Parkinson Disease Rating Scale (p = 0.001) and Tinetti Fall Performance Scale (p < 0.001) after RAS training.
3.3.3. RAS and Effects of Auditory–Motor Entrainment in IPD
Janzen and colleagues (2019) examined instantaneous effects of auditory–motor entrainment within effector systems [16]. The results implied that finger tapping training was followed by a significant increase in gait speed (p < 0.005). Significant changes in gait cadence were found in the finger tapping group (p < 0.005) after training, but not after arm swing (p = 0.879) and control (p = 0.759) training. Summarizing the available results, it can be concluded that auditory–motor entrainment in one effector system can stimulate the other effector system.
3.3.4. RAS and Falls in PD
Another study focused on RAS in fall reduction [13]. For this study, both the experimental and control groups had significant improvements in performance at week 8 from the start of the intervention. At week 16, significant improvements were registered for speed, stride length, cadence, right and left ankle dorsiflexion, fall index and fear of falling in the experimental group. It should be noted that bilateral ankle dorsiflexion correlated significantly with changes in gait, fear of falling and fall rate. This may indicate that ankle dorsiflexion is a potential kinematic mechanism by which RAS may be useful in reducing falls.
3.3.5. Ecological RAS vs. Artificial RAS in PD
The aim of the study by Murgia and colleagues (2018) was to examine if a PD rehabilitation combined with an ecological RAS could be more effective than the same programme integrated with an artificial RAS [17]. The results of the experiment suggest that both groups improved in most biomechanical and clinical measurements, regardless of the type of sound. Exploratory analyses were also performed for the separate groups, which showed improvements in spatiotemporal parameters only for the organic RAS group (p = 0.001).
3.3.6. RAS and Sensorimotor Timing Skills in Idiopathic Parkinson’s disease (IPD)
The last article by Bella and colleagues (2017) explored the role of sensorimotor time measurement skills, tested with walk and tap tasks, to assess the effectiveness of RAS in people with IPD [14]. Both gait speed and stride length improved significantly and were maintained one month after music gait training (MCGT; p < 0.05). Immediately after training, a significantly reduced variation in patients’ step time was noted (p < 0.05). The effect did not persist during the follow-up period (p = 0.13). An important aspect of the study is to explore individual factors such as initial gait speed or performance in timed (sensorimotor) tasks that influence the effectiveness of RAS.
3.4. RAS in Stroke
RAS also showed benefits for SPs. In the GTBR group, there were significant changes in gait symmetry and in the magnitude of decreases in gait symmetry per step time. The combination of treadmill training and RAS resulted in better functional gait performance (significant changes in speed, cadence and stride length) compared with standard treadmill training [18,19].
3.4.1. Bilateral RAS in SP
The first of two articles by Lee and colleagues (2018) considered the effect of gait training with bilateral RAS (GTBR) on lower limb rehabilitation in SP patients [18]. In the GTBR group, significant changes were obtained in gait symmetry (p < 0.05) and in the size of decreases in gait symmetry per step time. Both groups showed improvements in gait ability on velocity and cadence, and scored significantly better (p < 0.05) on the BBS, Timed Up and Go (TUG) and Fugl-Meyer assessment (FMA) tests relative to baseline measurements. Summarising the results of both groups, it can be concluded that GTBR allowed greater improvements in gait parameters in SP patients relative to the group receiving standard gait training.
3.4.2. RAS-Treadmill Training in SP
A study by Mainka and colleagues (2018) focused on comparing the effectiveness of a combination of treadmill training (RAS-TT) versus treadmill training (TT) in the rehabilitation of functional gait in stroke [19]. There were significant changes in speed (p < 0.001), cadence (p = 0.001) and stride length (p < 0.001) in the RAS-TT group before and after. There were also significant time effects for these parameters in the FGS test. The RAS-TT group had significantly higher scores compared with the other groups. The researchers used the fact that music allows for the correction of step frequency and improvement of gait pattern, mainly through the action of auditory motor feedback to reduce stress, both motor and psychological. File S4 [4,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92,93,94,95,96] presents the full characteristics of the studies included in the systematic review.
3.5. Risk of Bias in Included Studies
Included studies showed some concerns in the risk of bias assessment overall, in which randomization, concealment and missing outcome data were unclear. Two studies were assessed as low risk of bias. One study was rated as high risk of bias due to deviations from the intended intervention, as well as insufficient randomization information and missing results.
4. Discussion
The aim of this review was to critically assess the available literature on the application of NMT techniques in the rehabilitation of geriatric disorders. We found eight studies that met the inclusion criteria. All of them were based on the RAS technique (sensorimotor domain) in the movement rehabilitation of PD patients and SPs. RAS aims to develop and maintain a physiological rhythmic motor activity through rhythmic auditory cues. In a series of ground-breaking studies starting in the mid-1990s, it was discovered that this technique permanently improved walking speed, step length and cadence in PD [97,98]. In general, the positive effects of RAS training based on metronome or music are well grounded in terms of the PD literature. Therefore, it is not surprising that our review includes modifications to the RAS technique, combining this technique with multimodal balance training, treadmill training, gait training supported by bilateral RAS and comparison of rehabilitation programme effects integrated with ecological or artificial RAS.
The novelty of comparing RAS-supported multimodal balance training with regular multimodal training study is based on the fact that, for the first time, the importance of specialist physiotherapy with a specific exercise protocol with RAS has been demonstrated, which can improve the balance performance of PD patients in advanced stages of the disease and mild cognitive decline [12]. Researchers report that only a few studies have covered a subgroup of Hoehn and Yahr Scale stage 4 patients, but none of them specifically focused on RAS balance training in advanced stages of the disease. The message is that multimodal balance training (both with and without RAS) is possible in patients in advanced stages of the disease, because it did not cause falls and serious adverse events. The lack of influence on the gait rate results in both groups was interpreted as patients in advanced stages of the disease experience difficulties transferring the balance improvement to the gait task. However, as noted, the use of RAS can improve training effects by making them more pronounced than training without RAS. Reports of the efficacy of multimodal RAS intervention may provide important guidance for practitioners caring for PD patients in advanced stages, as there is still a lack of recommendations for the optimal approach in motor rehabilitation for this group [12,99].
The data presented by Calabrò and colleagues [15] imply that the use of RAS training compared with training without RAS allows for improved overall gait quality and better results in the areas of number and length of gaits and balance. However, the absence of a significant difference in RAS and non-RAS training in terms of improved gait, turning and stride duration may mean that the rehabilitation programme by itself, not cueing, influenced the improvement. Other main conclusion of this study is that only in the group receiving RAS training was frontotemporal connectivity involved in the α frequency range. This functional connectivity is strongly associated with cognitive performance in PD, due to deterioration with cognitive decline. Deterioration of α is a marker of degeneration of the ascending diffuse projection systems that control attention. Therefore, the use of music as an external cue allows for increased levels of attention, and thus improved performance and participation of subjects, as can be seen in the low variability of outcome measures after the RAS intervention.
Interesting conclusions appeared from the study about rhythmic priming across effector systems [16]. The possibility of modulating gait speed through RAS training of arm or finger movements was tested. The first group was asked to tap their fingers in synchrony with a metronome. Participants in the second group were asked to alternate sways synchronised to a metronome. Interestingly, only participants in the first group (finger tapping) achieved significant increases in gait speed and cadence before training. The second group showed no change in gait speed after training. These reports suggest that auditory–motor interaction in one effector system can stimulate the other effector system. Quite surprisingly, the priming effect on gait was only observed in the finger tapping condition. The authors emphasise that the results of the study are relevant for the development of motor rehabilitation. The study is an important step for further exploration of the mechanisms underlying the coupling between effectors, and consequently the development of new therapeutic pathways adapted to the capabilities of PD patients.
Additionally, the use of RAS was effective in reducing falls in PD patients. Discontinuation of the intervention resulted in an increase in falls and gait speed and a reduction in ankle dorsiflexion. Correlational analyses showed a noticeable association between the reduction in falls with improvements in dorsiflexion and gait speed [13]. Overall, the improvement in gait parameters (gait speed, velocity, stride length, and cadence) and balance due to the RAS training was confirmed in all studies. Temporal cues are recognised as important factors that reinforce the underlying physiology of temporal pattern formation in the basal ganglia. As a result, they enhance motor learning. RAS as a coordinative sensory input unifies the temporal functions of the basal ganglia loops and also to increase gait velocity and stride length [100]. It is worth noting that the low cost of therapy and the ability to safely implement training even in a home setting after brief instruction may prove to be an effective solution for patients facing various obstacles due to their inability to participate in therapy due to their place of residence or low economic status.
For RAS in post-stroke rehabilitation, we found that a programme involving GTBR (6 weeks), compared with standard gait training, was more effective for SP gait ability, balance and symmetry and lower limb function [18]. Moreover, when considering interventions to improve gait symmetry, it is worth considering the possible benefits of using GTBR beat frequency matching for fast step time. The researchers suggest that planned further research should focus on developing a method to use RAS in SPs for step time and step length. GTBR can be considered a useful method for functional rehabilitation in SPs. In addition, it may be applied in the home setting for outpatients. The reports analysed show that RAS-TT can contribute to the optimisation of gait rehabilitation in patients with SPs [19]. A significant improvement in gait velocity (p = 0.032) and cadence (p = 0.002) in the FGS was observed. The material analysed provides a starting point for inferring the greater effectiveness of RAS-TT over other approaches (i.e., TT and NDT) in functional gait rehabilitation and supports the development of a more optimal therapy by combining functional music with treadmill training.
Results from the current literature also indicate that RAS is beneficial for improving gait speed and overall gait quality, stride length, or cadence in SPs [95,101]. However, the researchers point out that these reports should be treated with caution due to the high risk of bias in most reports. In the case of our study, we also faced uncertainties caused by missing information regarding blinding, deviations from the intervention, and missing results. Evidence from randomized studies with large samples is still lacking [101].
Music-based interventions have shown high efficacy in the treatment of neurological and neuropsychiatric disorders associated with stroke [102]. However, they are not only limited to motor function, but also language and cognitive function, as well as quality of life. Other studies show that music therapy can effectively improve dysphagia, which is a serious problem in the post-stroke elderly [103,104]. Melodic intonation therapy in both SP and PD therapy is gaining increasing interest among therapists and researchers [21,105,106]. Unfortunately, strong evidence for its effectiveness is still lacking. Researchers point out, among other things, the problems of providing the intervention to people who have not received adequate specialized training (musicians/music therapists), the lack of appropriate assessment tools and under-sampling in clinical trials [106]. Therefore, it can be concluded that research in this area should continue with the inclusion of techniques focusing on the speech/language area as well. Schaffert and colleagues (2019) explored based on the available literature (review), investigated the relationships existing between sound and movement in the context of both sports training and physical rehabilitation. The data presented prove the impact of natural movement sounds, rhythmic auditory information and movement sonication on sports training and (re)learning [107]. Another review of music therapy in PD found that most of the studies analysed show a beneficial effect of music therapy on the non-pharmacological treatment of motor and non-motor symptoms and on the quality of life of people with PD. The research included in this review covered all interventions using music in PD rehabilitation, not just NMT. Therefore, it is only an indication of the effectiveness of music in the rehabilitation of this disease [108].
It is worth noting that NMT contains 20 standardized and clinically applied techniques, most of which are used in therapeutic practice in the rehabilitation of older people. However, only one of them has qualified for our review. For example, for behavioural and psychological symptoms of dementia (BPSD), music therapy has proven to be a more effective and economically preferable option for improvement compared with pharmacotherapy [109]. It was also reported to improve mood and reduce anxiety and depression [110]. Of the NMT techniques, many are applicable to dementia therapy, so it is surprising that we have not found studies focusing on this subject. However, this is quite a young approach that is still gaining in popularity, and further research in this area is necessary.
The ability to observe the brain while processing musical information has contributed to a better understanding of how music works in therapy and, in effect, to develop a more precise scientific basis for music therapy [111]. Clinical studies indicate that the processes in the brain triggered by music can be generalized and transferred to non-musical functions, giving desired and measurable therapeutic effects [7,97,111,112]. NMT techniques are used in neurorehabilitation as non-invasive and promising results that should be considered as a complement to conventional cognitive neurorehabilitation and stimulation therapy [113]. Studies included in this review confirm this statement.
5. Conclusions
Due to the global population ageing worldwide and the need to integrate psychogeriatric disorders therapy, there is a growing need for effective non-pharmacological treatment and support for rehabilitation in the broadest sense of the term. Interventions using the RAS technique indicate that it is effective in rehabilitation of gait and fall reduction in PD patients and improve mobility in SPs. The combination of multimodal balance training with RAS and treadmill training with RAS was evaluated as effective intervention that helps optimize rehabilitation. The combination of auditory cues and music in the therapeutic programme seems to be beneficial for geriatric patients in terms of mobility, balance, falls and gait parameters (stride length, cadence, speed). NMT is an effective, non-invasive, low-cost, and accessible intervention for elderly patients; therefore, it is worth considering among non-pharmacological strategies to support sensorimotor rehabilitation in patients with PD and SP. The review indicates that modifications of the RAS are effective and also allow a better adaptation to the individual needs and abilities of the patient. Particularly as this technique can be applied at home settings.
RCTs are mainly conducted in the sensorimotor area and tend to focus on the RAS technique. However, NMT is still a niche therapeutic intervention, and it is worth focusing on further research on the use of RAS in sensorimotor rehabilitation and other NMT techniques in older patients, particularly in the areas of cognition and speech under different conditions.
6. Limitations
The restrictions we encountered during the creation of the review mostly concerned the nomenclature in the article abstract. The lack of systematic nomenclature hindered the process of selecting articles and raised several questions regarding the fulfilment of the inclusion criteria. A broad understanding of the concept of music therapy and a lack of precision in the methodology of conducting research on its effectiveness made some of the research have low reliability, and there was an inability to compare the latest discoveries with already available knowledge.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/healthcare10112187/s1, File S1: PICO; File S2: Risk of Bias; File S3: Characteristics of studies qualifying for review; File S4: Exluded Fulltext.
Author Contributions
Conceptualization, J.R. and J.S.-G.; methodology, J.R. and P.K.; software, J.R.; validation, P.K. and J.S.-G.; formal analysis, J.R., J.S.-G. and P.K.; investigation, J.R.; resources, J.R., J.S.-G. and P.K.; data curation, J.R.; writing—original draft preparation, J.R.; writing—review and editing, J.S.-G. and P.K.; visualization, J.R.; supervision, P.K.; project administration, J.S.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available in Supplementary Materials—Files S1–S4.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Eurostat People in the EU—Statistics on Demographic Changes. Available online: https://ec.europa.eu/eurostat/statistics-explained/index.php/People_in_the_EU_-_statistics_on_demographic_changes#An_ageing_population (accessed on 22 March 2020).
- Dudek, D. Issues Related to the Psychology of the Elderly. Psychopathology. In Psychogeriatrics; PZWL: Warsaw, Poland, 2017; pp. 17–29. [Google Scholar]
- Bayona, N.A.; Bitensky, J.; Salter, K.; Teasell, R. The Role of Task-Specific Training in Rehabilitation Therapies. Top. Stroke Rehabil. 2005, 12, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Bukowska, A.A.; Krężałek, P.; Mirek, E.; Bujas, P.; Marchewka, A. Neurologic Music Therapy Training for Mobility and Stability Rehabilitation with Parkinson’s Disease–A Pilot Study. Front. Hum. Neurosci. 2016, 9, 710. [Google Scholar] [CrossRef] [PubMed]
- Kitago, T.; Krakauer, J.W. Motor Learning Principles for Neurorehabilitation. In Handbook of Clinical Neurology; Barnes, M.P., Good, D.C., Eds.; Elsevier: Amsterdam, The Netherlands, 2012; pp. 93–103. [Google Scholar]
- Thaut, M.; Hoemberg, V. (Eds.) Handbook of Neurologic Music Therapy; Oxford University Press: New York, NY, USA, 2014; ISBN 978-0-19-969546-1. [Google Scholar]
- Thaut, M.H. Music in Therapy and Medicine: From Social Science to Neuroscience. In Rhythm, Music, and the Brain: Scientific Foundations and Clinical Applications; Taylor and Francis Group: New York, NY, USA, 2005; pp. 113–136. [Google Scholar]
- PRISMA-P Group; Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. Syst. Rev. 2021, 10, 89. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 1st ed.; Wiley: New York, NY, USA, 2019; ISBN 978-1-119-53662-8. [Google Scholar]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; Welch, V.A.; Higgins, J.P.; Thomas, J. Updated Guidance for Trusted Systematic Reviews: A New Edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef]
- Capato, T.T.C.; Nonnekes, J.; de Vries, N.M.; IntHout, J.; Barbosa, E.R.; Bloem, B.R. Effects of Multimodal Balance Training Supported by Rhythmical Auditory Stimuli in People with Advanced Stages of Parkinson’s Disease: A Pilot Randomized Clinical Trial. J. Neurol. Sci. 2020, 418, 117086. [Google Scholar] [CrossRef]
- Thaut, M.H.; Rice, R.R.; Braun Janzen, T.; Hurt-Thaut, C.P.; McIntosh, G.C. Rhythmic Auditory Stimulation for Reduction of Falls in Parkinson’s Disease: A Randomized Controlled Study. Clin. Rehabil. 2019, 33, 34–43. [Google Scholar] [CrossRef]
- Bella, S.D.; Benoit, C.-E.; Farrugia, N.; Keller, P.E.; Obrig, H.; Mainka, S.; Kotz, S.A. Gait Improvement via Rhythmic Stimulation in Parkinson’s Disease Is Linked to Rhythmic Skills. Sci. Rep. 2017, 7, 42005. [Google Scholar] [CrossRef]
- Calabrò, R.S.; Naro, A.; Filoni, S.; Pullia, M.; Billeri, L.; Tomasello, P.; Portaro, S.; Di Lorenzo, G.; Tomaino, C.; Bramanti, P. Walking to Your Right Music: A Randomized Controlled Trial on the Novel Use of Treadmill plus Music in Parkinson’s Disease. J. NeuroEngineering Rehabil. 2019, 16, 68. [Google Scholar] [CrossRef]
- Braun Janzen, T.; Haase, M.; Thaut, M.H. Rhythmic Priming across Effector Systems: A Randomized Controlled Trial with Parkinson’s Disease Patients. Hum. Mov. Sci. 2019, 64, 355–365. [Google Scholar] [CrossRef]
- Murgia, M.; Pili, R.; Corona, F.; Sors, F.; Agostini, T.A.; Bernardis, P.; Casula, C.; Cossu, G.; Guicciardi, M.; Pau, M. The Use of Footstep Sounds as Rhythmic Auditory Stimulation for Gait Rehabilitation in Parkinson’s Disease: A Randomized Controlled Trial. Front. Neurol. 2018, 9, 348. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.; Lee, K.; Song, C. Gait Training with Bilateral Rhythmic Auditory Stimulation in Stroke Patients: A Randomized Controlled Trial. Brain Sci. 2018, 8, 164. [Google Scholar] [CrossRef] [PubMed]
- Mainka, S.; Wissel, J.; Völler, H.; Evers, S. The Use of Rhythmic Auditory Stimulation to Optimize Treadmill Training for Stroke Patients: A Randomized Controlled Trial. Front. Neurol. 2018, 9, 755. [Google Scholar] [CrossRef]
- Lyu, J.; Zhang, J.; Mu, H.; Li, W.; Champ, M.; Xiong, Q.; Gao, T.; Xie, L.; Jin, W.; Yang, W.; et al. The Effects of Music Therapy on Cognition, Psychiatric Symptoms, and Activities of Daily Living in Patients with Alzheimer’s Disease. J. Alzheimers Dis. 2018, 64, 1347–1358. [Google Scholar] [CrossRef]
- Haro-Martínez, A.M.; Lubrini, G.; Madero-Jarabo, R.; Díez-Tejedor, E.; Fuentes, B. Melodic Intonation Therapy in Post-Stroke Nonfluent Aphasia: A Randomized Pilot Trial. Clin. Rehabil. 2019, 33, 44–53. [Google Scholar] [CrossRef]
- Giovagnoli, A.R.; Manfredi, V.; Schifano, L.; Paterlini, C.; Parente, A.; Tagliavini, F. Combining Drug and Music Therapy in Patients with Moderate Alzheimer’s Disease: A Randomized Study. Neurol. Sci. 2018, 39, 1021–1028. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, A.; Maseda, A.; Marante-Moar, M.P.; de Labra, C.; Lorenzo-López, L.; Millán-Calenti, J.C. Comparing the Effects of Multisensory Stimulation and Individualized Music Sessions on Elderly People with Severe Dementia: A Randomized Controlled Trial. J. Alzheimers Dis. 2016, 52, 303–315. [Google Scholar] [CrossRef]
- Mahendran, R.; Gandhi, M.; Moorakonda, R.B.; Wong, J.; Kanchi, M.M.; Fam, J.; Rawtaer, I.; Kumar, A.P.; Feng, L.; Kua, E.H. Art Therapy Is Associated with Sustained Improvement in Cognitive Function in the Elderly with Mild Neurocognitive Disorder: Findings from a Pilot Randomized Controlled Trial for Art Therapy and Music Reminiscence Activity versus Usual Care. Trials 2018, 19, 615. [Google Scholar] [CrossRef]
- Gök Ugur, H.; Yaman Aktaş, Y.; Orak, O.S.; Saglambilen, O.; Aydin Avci, İ. The Effect of Music Therapy on Depression and Physiological Parameters in Elderly People Living in a Turkish Nursing Home: A Randomized-Controlled Trial. Aging Ment. Health 2017, 21, 1280–1286. [Google Scholar] [CrossRef]
- Han, J.W.; Lee, H.; Hong, J.W.; Kim, K.; Kim, T.; Byun, H.J.; Ko, J.W.; Youn, J.C.; Ryu, S.-H.; Lee, N.-J.; et al. Multimodal Cognitive Enhancement Therapy for Patients with Mild Cognitive Impairment and Mild Dementia: A Multi- Center, Randomized, Controlled, Double-Blind, Crossover Trial. J. Alzheimers Dis. 2016, 55, 787–796. [Google Scholar] [CrossRef]
- Pitkänen, A.; Alanen, H.-M.; Kampman, O.; Suontaka-Jamalainen, K.; Leinonen, E. Implementing Physical Exercise and Music Interventions for Patients Suffering from Dementia on an Acute Psychogeriatric Inpatient Ward. Nord. J. Psychiatry 2019, 73, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Doi, T.; Verghese, J.; Makizako, H.; Tsutsumimoto, K.; Hotta, R.; Nakakubo, S.; Suzuki, T.; Shimada, H. Effects of Cognitive Leisure Activity on Cognition in Mild Cognitive Impairment: Results of a Randomized Controlled Trial. J. Am. Med. Dir. Assoc. 2017, 18, 686–691. [Google Scholar] [CrossRef] [PubMed]
- Feng, K.; Shen, C.-Y.; Ma, X.-Y.; Chen, G.-F.; Zhang, M.-L.; Xu, B.; Liu, X.-M.; Sun, J.-J.; Zhang, X.-Q.; Liu, P.-Z.; et al. Effects of Music Therapy on Major Depressive Disorder: A Study of Prefrontal Hemodynamic Functions Using FNIRS. Psychiatry Res. 2019, 275, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Särkämö, T.; Laitinen, S.; Numminen, A.; Kurki, M.; Johnson, J.K.; Rantanen, P. Clinical and Demographic Factors Associated with the Cognitive and Emotional Efficacy of Regular Musical Activities in Dementia. J. Alzheimers Dis. 2015, 49, 767–781. [Google Scholar] [CrossRef] [PubMed]
- Shirani Bidabadi, S.; Mehryar, A. Music Therapy as an Adjunct to Standard Treatment for Obsessive Compulsive Disorder and Co-Morbid Anxiety and Depression: A Randomized Clinical Trial. J. Affect. Disord. 2015, 184, 13–17. [Google Scholar] [CrossRef]
- Silverman, M.J. Comparing Educational Music Therapy Interventions via Stages of Recovery with Adults in an Acute Care Mental Health Setting: A Cluster-Randomized Pilot Effectiveness Study. Community Ment. Health J. 2019, 55, 624–630. [Google Scholar] [CrossRef]
- Ho, R.T.; Fong, T.C.; Sing, C.; Lee, P.H.; Leung, A.B.; Chung, K.S.; Kwok, J.K. Managing Behavioral and Psychological Symptoms in Chinese Elderly with Dementia via Group-Based Music Intervention: A Cluster Randomized Controlled Trial. Dementia 2019, 18, 2785–2798. [Google Scholar] [CrossRef]
- Yap, A.F.; Kwan, Y.H.; Tan, C.S.; Ibrahim, S.; Ang, S.B. Rhythm-Centred Music Making in Community Living Elderly: A Randomized Pilot Study. BMC Complement. Altern. Med. 2017, 17, 311. [Google Scholar] [CrossRef]
- Marmelat, V.; Duncan, A.; Meltz, S.; Meidinger, R.L.; Hellman, A.M. Fractal Auditory Stimulation Has Greater Benefit for People with Parkinson’s Disease Showing More Random Gait Pattern. Gait Posture 2020, 80, 234–239. [Google Scholar] [CrossRef]
- Bunketorp-Käll, L.; Pekna, M.; Pekny, M.; Blomstrand, C.; Nilsson, M. Effects of Horse-Riding Therapy and Rhythm and Music-Based Therapy on Functional Mobility in Late Phase after Stroke. NeuroRehabilitation 2019, 45, 483–492. [Google Scholar] [CrossRef]
- Lee, C.-H.; Lai, C.-L.; Sung, Y.-H.; Lai, M.Y.; Lin, C.-Y.; Lin, L.-Y. Comparing Effects between Music Intervention and Aromatherapy on Anxiety of Patients Undergoing Mechanical Ventilation in the Intensive Care Unit: A Randomized Controlled Trial. Qual. Life Res. Int. J. Qual. Life Asp. Treat. Care Rehabil. 2017, 26, 1819–1829. [Google Scholar] [CrossRef] [PubMed]
- Fotakopoulos, G.; Kotlia, P. The Value of Exercise Rehabilitation Program Accompanied by Experiential Music for Recovery of Cognitive and Motor Skills in Stroke Patients. J. Stroke Cerebrovasc. Dis. Off. J. Natl. Stroke Assoc. 2018, 27, 2932–2939. [Google Scholar] [CrossRef] [PubMed]
- Impellizzeri, F.; Leonardi, S.; Latella, D.; Maggio, M.G.; Foti Cuzzola, M.; Russo, M.; Sessa, E.; Bramanti, P.; De Luca, R.; Calabrò, R.S. An Integrative Cognitive Rehabilitation Using Neurologic Music Therapy in Multiple Sclerosis: A Pilot Study. Medicine 2020, 99, e18866. [Google Scholar] [CrossRef]
- Street, A.J.; Magee, W.L.; Bateman, A.; Parker, M.; Odell-Miller, H.; Fachner, J. Home-Based Neurologic Music Therapy for Arm Hemiparesis Following Stroke: Results from a Pilot, Feasibility Randomized Controlled Trial. Clin. Rehabil. 2018, 32, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Cheung, M.-C.; Chan, A.S.; Liu, Y.; Law, D.; Wong, C.W.Y. Music Training Is Associated with Cortical Synchronization Reflected in EEG Coherence during Verbal Memory Encoding. PLoS ONE 2017, 12, e0174906. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.J.; Shin, Y.-K.; Yoo, G.E.; Chong, H.J.; Cho, S.-R. Changes in Gait Patterns Induced by Rhythmic Auditory Stimulation for Adolescents with Acquired Brain Injury. Ann. N. Y. Acad. Sci. 2016, 1385, 53–62. [Google Scholar] [CrossRef]
- van Alphen, R.; Stams, G.J.J.M.; Hakvoort, L. Musical Attention Control Training for Psychotic Psychiatric Patients: An Experimental Pilot Study in a Forensic Psychiatric Hospital. Front. Neurosci. 2019, 13, 570. [Google Scholar] [CrossRef]
- Raglio, A.; Oasi, O.; Gianotti, M.; Rossi, A.; Goulene, K.; Stramba-Badiale, M. Improvement of Spontaneous Language in Stroke Patients with Chronic Aphasia Treated with Music Therapy: A Randomized Controlled Trial. Int. J. Neurosci. 2016, 126, 235–242. [Google Scholar] [CrossRef]
- Baur, K.; Speth, F.; Nagle, A.; Riener, R.; Klamroth-Marganska, V. Music Meets Robotics: A Prospective Randomized Study on Motivation during Robot Aided Therapy. J. Neuroengineering Rehabil. 2018, 15, 79. [Google Scholar] [CrossRef]
- Pohl, P.; Carlsson, G.; Bunketorp Käll, L.; Nilsson, M.; Blomstrand, C. Experiences from a Multimodal Rhythm and Music-Based Rehabilitation Program in Late Phase of Stroke Recovery-A Qualitative Study. PLoS ONE 2018, 13, e0204215. [Google Scholar] [CrossRef]
- Bunketorp-Käll, L.; Lundgren-Nilsson, Å.; Samuelsson, H.; Pekny, T.; Blomvé, K.; Pekna, M.; Pekny, M.; Blomstrand, C.; Nilsson, M. Long-Term Improvements After Multimodal Rehabilitation in Late Phase After Stroke: A Randomized Controlled Trial. Stroke 2017, 48, 1916–1924. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-C.; Yeh, M.-L.; Chang, H.-J.; Lin, M.-F. Music, Heart Rate Variability, and Symptom Clusters: A Comparative Study. Support. Care Cancer Off. J. Multinatl. Assoc. Support. Care Cancer 2020, 28, 351–360. [Google Scholar] [CrossRef] [PubMed]
- van Vugt, F.T.; Kafczyk, T.; Kuhn, W.; Rollnik, J.D.; Tillmann, B.; Altenmüller, E. The Role of Auditory Feedback in Music-Supported Stroke Rehabilitation: A Single-Blinded Randomised Controlled Intervention. Restor. Neurol. Neurosci. 2016, 34, 297–311. [Google Scholar] [CrossRef] [PubMed]
- Santhosh, A.K.; Sangilirajan, M.; Nizar, N.; Radhamani, R.; Kumar, D.; Bodda, S.; Diwakar, S. Computational Exploration of Neural Dynamics Underlying Music Cues Among Trained and Amateur Subjects. Procedia Comput. Sci. 2020, 171, 1839–1847. [Google Scholar] [CrossRef]
- Gómez Gallego, M.; Gómez García, J. Music Therapy and Alzheimer’s Disease: Cognitive, Psychological, and Behavioural Effects. Neurol. Engl. Ed. 2017, 32, 300–308. [Google Scholar] [CrossRef]
- Burrai, F.; Sanna, G.D.; Moccia, E.; Morlando, F.; Cosentino, E.R.; Bui, V.; Micheluzzi, V.; Borghi, C.; Parodi, G. Beneficial Effects of Listening to Classical Music in Patients With Heart Failure: A Randomized Controlled Trial. J. Card. Fail. 2020, 26, 541–549. [Google Scholar] [CrossRef] [PubMed]
- Çetinkaya, F. Effect of Listening to Music on Postoperative Cognitive Function in Older Adults After Hip or Knee Surgery: A Randomized Controlled Trial. J. Perianesth. Nurs. 2019, 34, 919–928. [Google Scholar] [CrossRef]
- Kavakli, A.S.; Kavrut Ozturk, N.; Yavuzel Adas, H.; Kudsioglu, S.T.; Ayoglu, R.U.; Özmen, S.; Sagdic, K.; Yapici, N. The Effects of Music on Anxiety and Pain in Patients during Carotid Endarterectomy under Regional Anesthesia: A Randomized Controlled Trial. Complement. Ther. Med. 2019, 44, 94–101. [Google Scholar] [CrossRef]
- Tanaka, Y.; Nogawa, H. Evaluating the Effects of Singing Songs in Ethnic Music Therapy for Dementia Patients with a Novel Near-Infrared Spectroscopy (Data Analysis Method). Int. J. Gerontol. 2015, 9, 7–14. [Google Scholar] [CrossRef]
- Moon, S.; Park, J.; Yang, S. The Effects of Therapeutic Singing on Vocal Functions of the Elderly: A Study on Korean Elderly. J. Voice 2020, 36, 437. [Google Scholar] [CrossRef]
- Cho, H.; Kim, K. Effects of Action Observation Training with Auditory Stimulation on Static and Dynamic Balance in Chronic Stroke Patients. J. Stroke Cerebrovasc. Dis. 2020, 29, 104775. [Google Scholar] [CrossRef] [PubMed]
- Song, J.-H.; Zhou, P.-Y.; Cao, Z.-H.; Ding, Z.-G.; Chen, H.-X.; Zhang, G.-B. Rhythmic Auditory Stimulation with Visual Stimuli on Motor and Balance Function of Patients with Parkinson’s Disease. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 2001–2007. [Google Scholar]
- Rios Romenets, S.; Anang, J.; Fereshtehnejad, S.-M.; Pelletier, A.; Postuma, R. Tango for Treatment of Motor and Non-Motor Manifestations in Parkinson’s Disease: A Randomized Control Study. Complement. Ther. Med. 2015, 23, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Esmail, A.; Vrinceanu, T.; Lussier, M.; Predovan, D.; Berryman, N.; Houle, J.; Karelis, A.; Grenier, S.; Minh Vu, T.T.; Villalpando, J.M.; et al. Effects of Dance/Movement Training vs. Aerobic Exercise Training on Cognition, Physical Fitness and Quality of Life in Older Adults: A Randomized Controlled Trial. J. Bodyw. Mov. Ther. 2020, 24, 212–220. [Google Scholar] [CrossRef] [PubMed]
- do Amaral, J.A.T.; Guida, H.L.; de Abreu, L.C.; Barnabé, V.; Vanderlei, F.M.; Valenti, V.E. Effects of Auditory Stimulation with Music of Different Intensities on Heart Period. J. Tradit. Complement. Med. 2016, 6, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.-Y.; Chang, E.-T.; Lai, H.-L. Comparing the Effects of Music and Exercise with Music for Older Adults with Insomnia. Appl. Nurs. Res. 2016, 32, 104–110. [Google Scholar] [CrossRef]
- Guétin, S.; de Diego, E.; Mohy, F.; Adolphe, C.; Hoareau, G.; Touchon, J.; Thayer, J.F.; Koenig, J. A Patient-Controlled, Smartphone-Based Music Intervention to Reduce Pain—A Multi-Center Observational Study of Patients with Chronic Pain. Eur. J. Integr. Med. 2016, 8, 182–187. [Google Scholar] [CrossRef]
- Shanahan, J.; Morris, M.E.; Bhriain, O.N.; Volpe, D.; Lynch, T.; Clifford, A.M. Dancing for Parkinson Disease: A Randomized Trial of Irish Set Dancing Compared With Usual Care. Arch. Phys. Med. Rehabil. 2017, 98, 1744–1751. [Google Scholar] [CrossRef]
- Van Geel, F.; Van Asch, P.; Veldkamp, R.; Feys, P. Effects of a 10-Week Multimodal Dance and Art Intervention Program Leading to a Public Performance in Persons with Multiple Sclerosis—A Controlled Pilot-Trial. Mult. Scler. Relat. Disord. 2020, 44, 102256. [Google Scholar] [CrossRef]
- Saadatmand, V.; Rejeh, N.; Heravi-Karimooi, M.; Tadrisi, S.D.; Vaismoradi, M.; Jordan, S. Effects of Natural Sounds on Pain: A Randomized Controlled Trial with Patients Receiving Mechanical Ventilation Support. Pain Manag. Nurs. 2015, 16, 483–492. [Google Scholar] [CrossRef]
- Shi, E.R.; Zhang, Q. A Domain-General Perspective on the Role of the Basal Ganglia in Language and Music: Benefits of Music Therapy for the Treatment of Aphasia. Brain Lang. 2020, 206, 104811. [Google Scholar] [CrossRef] [PubMed]
- Facai, L.; Dehong, H.; Nana, H.; Yihuang, G.; Yunchuan, W. Effect of Music Therapy Derived from the Five Elements in Traditional Chinese Medicine on Post-Stroke Depression. J. Tradit. Chin. Med. 2017, 37, 675–680. [Google Scholar] [CrossRef]
- Baines, S.; Edwards, J. A Constructivist Grounded Theory Research Project Studying Music Therapy as an Anti-Oppressive Practice in Long-Term and Psychiatric Residential Care. Arts Psychother. 2018, 60, 1–8. [Google Scholar] [CrossRef]
- Froutan, R.; Eghbali, M.; Hoseini, S.H.; Mazloom, S.R.; Yekaninejad, M.S.; Boostani, R. The Effect of Music Therapy on Physiological Parameters of Patients with Traumatic Brain Injury: A Triple-Blind Randomized Controlled Clinical Trial. Complement. Ther. Clin. Pract. 2020, 40, 101216. [Google Scholar] [CrossRef]
- Deatrich, K.G.; Prout, M.F.; Boyer, B.A.; Yoder, S.E. Effectiveness of Group Music Therapy in a Psychiatric Hospital: A Randomized Pilot Study of Treatment Outcome. Int. J. Group Psychother. 2016, 66, 592–617. [Google Scholar] [CrossRef]
- Warth, M.; Kessler, J.; Koenig, J.; Wormit, A.F.; Hillecke, T.K.; Bardenheuer, H.J. Music Therapy to Promote Psychological and Physiological Relaxation in Palliative Care Patients: Protocol of a Randomized Controlled Trial. BMC Palliat. Care 2014, 13, 60. [Google Scholar] [CrossRef] [PubMed]
- Degli Stefani, M.; Biasutti, M. Effects of Music Therapy on Drug Therapy of Adult Psychiatric Outpatients: A Pilot Randomized Controlled Study. Front. Psychol. 2016, 7. [Google Scholar] [CrossRef]
- Imtiaz, D.; Anwar, Y.; Khan, A. Wearable Sensors and a Multisensory Music and Reminiscence Therapies Application: To Help Reduce Behavioral and Psychological Symptoms in Person with Dementia. Smart Health 2020, 100140. [Google Scholar] [CrossRef]
- Luvizutto, G.J.; Katlen da Silva, L.; Silva Brito, T.S.; Pascucci Sande de Souza, L.A. Music-Based Physical Therapy in Parkinson’s Disease: An Approach Based on International Classification of Functioning, Disability and Health. J. Bodyw. Mov. Ther. 2020, 26, 524–529. [Google Scholar] [CrossRef]
- Huang, C.-Y.; Chang, E.-T.; Hsieh, Y.-M.; Lai, H.-L. Effects of Music and Music Video Interventions on Sleep Quality: A Randomized Controlled Trial in Adults with Sleep Disturbances. Complement. Ther. Med. 2017, 34, 116–122. [Google Scholar] [CrossRef]
- Ready, E.A.; McGarry, L.M.; Rinchon, C.; Holmes, J.D.; Grahn, J.A. Beat Perception Ability and Instructions to Synchronize Influence Gait When Walking to Music-Based Auditory Cues. Gait Posture 2019, 68, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Kasdan, A.; Kiran, S. Please Don’t Stop the Music: Song Completion in Patients with Aphasia. J. Commun. Disord. 2018, 75, 72–86. [Google Scholar] [CrossRef] [PubMed]
- Tang, Q.; Zhou, Y.; Yang, S.; Thomas, W.K.S.; Smith, G.D.; Yang, Z.; Yuan, L.; Chung, J.W. Effect of Music Intervention on Apathy in Nursing Home Residents with Dementia. Geriatr. Nur. 2018, 39, 471–476. [Google Scholar] [CrossRef]
- Ji, L.; Bai, J.-J.; Sun, J.; Ming, Y.; Chen, L.-R. Effect of Combining Music Media Therapy with Lower Extremity Exercise on Elderly Patients with Diabetes Mellitus. Int. J. Nurs. Sci. 2015, 2, 243–247. [Google Scholar] [CrossRef][Green Version]
- Stegemöller, E.L.; Izbicki, P.; Hibbing, P. The Influence of Moving with Music on Motor Cortical Activity. Neurosci. Lett. 2018, 683, 27–32. [Google Scholar] [CrossRef] [PubMed]
- Argstatter, H.; Grapp, M.; Hutter, E.; Plinkert, P.K.; Bolay, H.-V. The Effectiveness of Neuro-Music Therapy According to the Heidelberg Model Compared to a Single Session of Educational Counseling as Treatment for Tinnitus: A Controlled Trial. J. Psychosom. Res. 2015, 78, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Espí-López, G.V.; Inglés, M.; Ruescas-Nicolau, M.-A.; Moreno-Segura, N. Effect of Low-Impact Aerobic Exercise Combined with Music Therapy on Patients with Fibromyalgia. A Pilot Study. Complement. Ther. Med. 2016, 28, 1–7. [Google Scholar] [CrossRef]
- Dauvergne, C.; Bégel, V.; Gény, C.; Puyjarinet, F.; Laffont, I.; Dalla Bella, S. Home-Based Training of Rhythmic Skills with a Serious Game in Parkinson’s Disease: Usability and Acceptability. Ann. Phys. Rehabil. Med. 2018, 61, 380–385. [Google Scholar] [CrossRef]
- Horin, A.P.; Harrison, E.C.; Rawson, K.S.; Earhart, G.M. Finger Tapping as a Proxy for Gait: Similar Effects on Movement Variability during External and Self-Generated Cueing in People with Parkinson’s Disease and Healthy Older Adults. Ann. Phys. Rehabil. Med. 2020, 64, 101402. [Google Scholar] [CrossRef]
- Gomes, R.L.; Vanderlei, L.C.M.; Garner, D.M.; de Marco, R.L.; Gonzaga, L.A.; Valenti, V.E. The Effects of Musical Auditory Stimulation on Cardiorespiratory Variables after Aerobic Exercise. Sci. Sports 2018, 33, 221–227. [Google Scholar] [CrossRef]
- Pau, M.; Corona, F.; Pili, R.; Casula, C.; Sors, F.; Agostini, T.; Cossu, G.; Guicciardi, M.; Murgia, M. Effects of Physical Rehabilitation Integrated with Rhythmic Auditory Stimulation on Spatio-Temporal and Kinematic Parameters of Gait in Parkinson’s Disease. Front. Neurol. 2016, 7. [Google Scholar] [CrossRef]
- Kadivar, Z.; Corcos, D.M.; Foto, J.; Hondzinski, J.M. Effect of Step Training and Rhythmic Auditory Stimulation on Functional Performance in Parkinson Patients. Neurorehabil. Neural Repair 2011, 25, 626–635. [Google Scholar] [CrossRef]
- Erra, C.; Mileti, I.; Germanotta, M.; Petracca, M.; Imbimbo, I.; Biase, A.; Rossi, S.; Ricciardi, D.; Pacilli, A.; Di SIpio, E.; et al. Immediate Effects of Rhythmic Auditory Stimulation on Gait Kinematics in Parkinson’s Disease ON/OFF Medication. Clin. Neurophysiol. 2019, 130. [Google Scholar] [CrossRef]
- Martínez-Molina, N.; Siponkoski, S.-T.; Kuusela, L.; Laitinen, S.; Holma, M.; Ahlfors, M.; Jordan-Kilkki, P.; Ala-Kauhaluoma, K.; Melkas, S.; Pekkola, J.; et al. Resting-State Network Plasticity Induced by Music Therapy after Traumatic Brain Injury. Neural Plast. 2021, 2021, 1–18. [Google Scholar] [CrossRef]
- Haire, C.M.; Vuong, V.; Tremblay, L.; Patterson, K.K.; Chen, J.L.; Thaut, M.H. Effects of Therapeutic Instrumental Music Performance and Motor Imagery on Chronic Post-Stroke Cognition and Affect: A Randomized Controlled Trial. NeuroRehabilitation 2021, 48, 195–208. [Google Scholar] [CrossRef]
- Geipel, J.; Koenig, J.; Hillecke, T.K.; Resch, F. Short-Term Music Therapy Treatment for Adolescents with Depression–A Pilot Study. Arts Psychother. 2022, 77, 101874. [Google Scholar] [CrossRef]
- Curzel, F.; Brigadoi, S.; Cutini, S. FNIRS & E-Drum: An Ecological Approach to Monitor Hemodynamic and Behavioural Effects of Rhythmic Auditory Cueing Training. Brain Cogn. 2021, 151, 105753. [Google Scholar] [CrossRef]
- Baker, F.A.; Lee, Y.-E.C.; Sousa, T.V.; Stretton-Smith, P.A.; Tamplin, J.; Sveinsdottir, V.; Geretsegger, M.; Wake, J.D.; Assmus, J.; Gold, C. Clinical Effectiveness of Music Interventions for Dementia and Depression in Elderly Care (MIDDEL): Australian Cohort of an International Pragmatic Cluster-Randomised Controlled Trial. Lancet Healthy Longev. 2022, 3, e153–e165. [Google Scholar] [CrossRef]
- Wang, Y.; Pan, W.-Y.; Li, F.; Ge, J.-S.; Zhang, X.; Luo, X.; Wang, Y.-L. Effect of Rhythm of Music Therapy on Gait in Patients with Stroke. J. Stroke Cerebrovasc. Dis. 2021, 30, 105544. [Google Scholar] [CrossRef]
- Kang, S.; Shin, J.-H.; Kim, I.Y.; Lee, J.; Lee, J.-Y.; Jeong, E. Patterns of Enhancement in Paretic Shoulder Kinematics after Stroke with Musical Cueing. Sci. Rep. 2020, 10, 18109. [Google Scholar] [CrossRef]
- Altenmüller, E.; Schlaug, G. Neurologic Music Therapy: The Beneficial Effects of Music Making on Neurorehabilitation. Acoust. Sci. Technol. 2013, 34, 5–12. [Google Scholar] [CrossRef]
- Buard, I.; Dewispelaere, W.B.; Thaut, M.; Kluger, B.M. Preliminary Neurophysiological Evidence of Altered Cortical Activity and Connectivity With Neurologic Music Therapy in Parkinson’s Disease. Front. Neurosci. 2019, 13, 105. [Google Scholar] [CrossRef] [PubMed]
- Keus, S.; Munneke, M.; Graziano, M.; Paltamaa, J.; Pelosin, E.; Domingos, J.; Brühlmann, S.; Ramaswamy, B.; Prins, J.; Struiksma, C.; et al. European Physiotherapy Guideline for Parkinson’s Disease; Royal Dutch Society for Physical Therapy (KNGF)/ParkinsonNet: London, UK, 2014; Available online: https://www.parkinsonnet.nl/app/uploads/sites/3/2019/11/eu_guideline_parkinson_development_and_justification.pdf (accessed on 25 September 2022).
- Lagasse, A.B.; Thaut, M.H. Music and Rehabilitation: Neurological Approaches. In Music Health, and Wellbeing; Oxford University Press: Oxford, UK, 2012; pp. 153–163. [Google Scholar]
- Magee, W.L.; Clark, I.; Tamplin, J.; Bradt, J. Music Interventions for Acquired Brain Injury. Cochrane Database Syst. Rev. 2017, 1, CD006787. [Google Scholar] [CrossRef]
- Sihvonen, A.J.; Särkämö, T.; Leo, V.; Tervaniemi, M.; Altenmüller, E.; Soinila, S. Music-Based Interventions in Neurological Rehabilitation. Lancet Neurol. 2017, 16, 648–660. [Google Scholar] [CrossRef]
- Xu, C.; He, Z.; Shen, Z.; Huang, F. Potential Benefits of Music Therapy on Stroke Rehabilitation. Oxid. Med. Cell. Longev. 2022, 2022, 9386095. [Google Scholar] [CrossRef]
- Kim, S.J.; Jo, U. Study of Accent-Based Music Speech Protocol Development for Improving Voice Problems in Stroke Patients with Mixed Dysarthria. Neurorehabilitation 2013, 32, 185–190. [Google Scholar] [CrossRef]
- Behaghel, E.; Zumbansen, A. Singing for the Rehabilitation of Acquired Neurogenic Communication Disorders: Continuing the Evidence Dialogue with a Survey of Current Practices in Speech-Language Pathology. Healthcare 2022, 10, 1010. [Google Scholar] [CrossRef]
- Zhang, X.; Li, J.; Du, Y. Melodic Intonation Therapy on Non-Fluent Aphasia After Stroke: A Systematic Review and Analysis on Clinical Trials. Front. Neurosci. 2022, 15, 753356. [Google Scholar] [CrossRef]
- Schaffert, N.; Braun Janzen, T.; Mattes, K.; Thaut, M.H. A Review on the Relationship Between Sound and Movement in Sports and Rehabilitation. Front. Psychol. 2019, 10, 244. [Google Scholar] [CrossRef]
- García-Casares, N.; Martín-Colom, J.E.; García-Arnés, J.A. Music Therapy in Parkinson’s Disease. J. Am. Med. Dir. Assoc. 2018, 19, 1054–1062. [Google Scholar] [CrossRef]
- Abe, M.; Tabei, K.; Satoh, M. The Assessments of Music Therapy for Dementia Based on the Cochrane Review. Dement. Geriatr. Cogn. Disord. Extra 2022, 12, 6–13. [Google Scholar] [CrossRef]
- Gassner, L.; Geretsegger, M.; Mayer-Ferbas, J. Effectiveness of Music Therapy for Autism Spectrum Disorder, Dementia, Depression, Insomnia and Schizophrenia: Update of Systematic Reviews. Eur. J. Public Health 2022, 32, 27–34. [Google Scholar] [CrossRef]
- Galińska, E. Music Therapy in Neurological Rehabilitation Settings. Psychiatr. Pol. 2015, 49, 835–846. [Google Scholar] [CrossRef]
- Altenmüller, E.; Schlaug, G. Apollo’s Gift. In Progress in Brain Research; Elsevier: Amsterdam, The Netherlands, 2015; Volume 217, pp. 237–252. ISBN 978-0-444-63551-8. [Google Scholar]
- Jauset-Berrocal, J.A.; Soria-Urios, G. Cognitive neurorehabilitation: The foundations and applications of neurologic music therapy. Rev. Neurol. 2018, 67, 303–310. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).