Analysis of Antidepressants Utilization for Patients Visiting Psychiatric Out-Patient Clinic in a Tertiary Care Hospital
Abstract
:1. Introduction
2. Materials and Methods
2.1. Method
2.1.1. Inclusion Criteria
2.1.2. Exclusion Criteria
2.2. Statistical Analysis
3. Results
- The patients were diagnosed based on the severity of depression—the distribution is visually elucidated in Figure 1. The highest number of patients (103, 66.9%) were diagnosed with moderate depressive episodes.
- Moreover, the study revealed that 35 (22.7%) patients had other comorbid conditions, with generalized idiopathic epilepsy and epileptic syndromes (12/35, 34.2%) being the most common (Table 2).
| Comorbid Conditions | ICD-10 Code | No. of Patients (%) |
|---|---|---|
| Generalized idiopathic epilepsy and epileptic syndromes | G40.3 | 12 (7.8) |
| Dyspepsia (Somatoform autonomic dysfunction) | F45.3 | 11 (7.1) |
| Primary hypertension | I10 | 5 (3.2) |
| Migraine, unspecified | G43.9 | 3 (1.9) |
| Alzheimer’s disease, unspecified | G30.9 | 2 (1.3) |
| Old myocardial infarction | I25.2 | 1 (0.6) |
| Parkinson disease | G20 | 1 (0.6) |

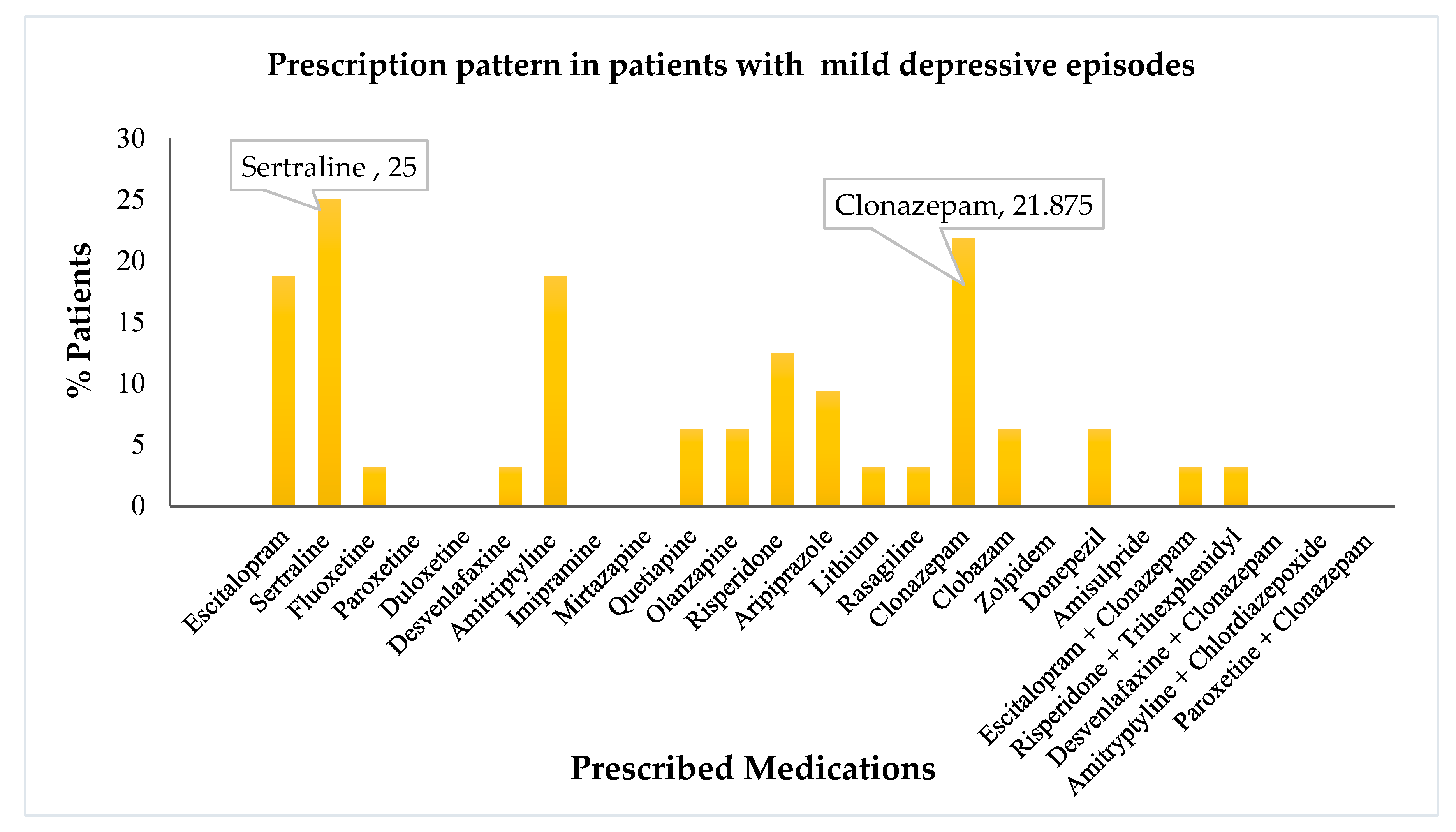
- Amongst the drugs prescribed, escitalopram, amitriptyline, and clonazepam, were the most common. Further, we evaluated the distribution and utilization of various drugs based on the use percentage in different diagnoses. The drug use pattern in mild depressive patients is visually depicted in Figure 2.
- It is noteworthy that sertraline and clonazepam were the most commonly prescribed agents for mild depressive disorder. Escitalopram and amitriptyline followed in succession. Risperidone and aripiprazole were used occasionally.
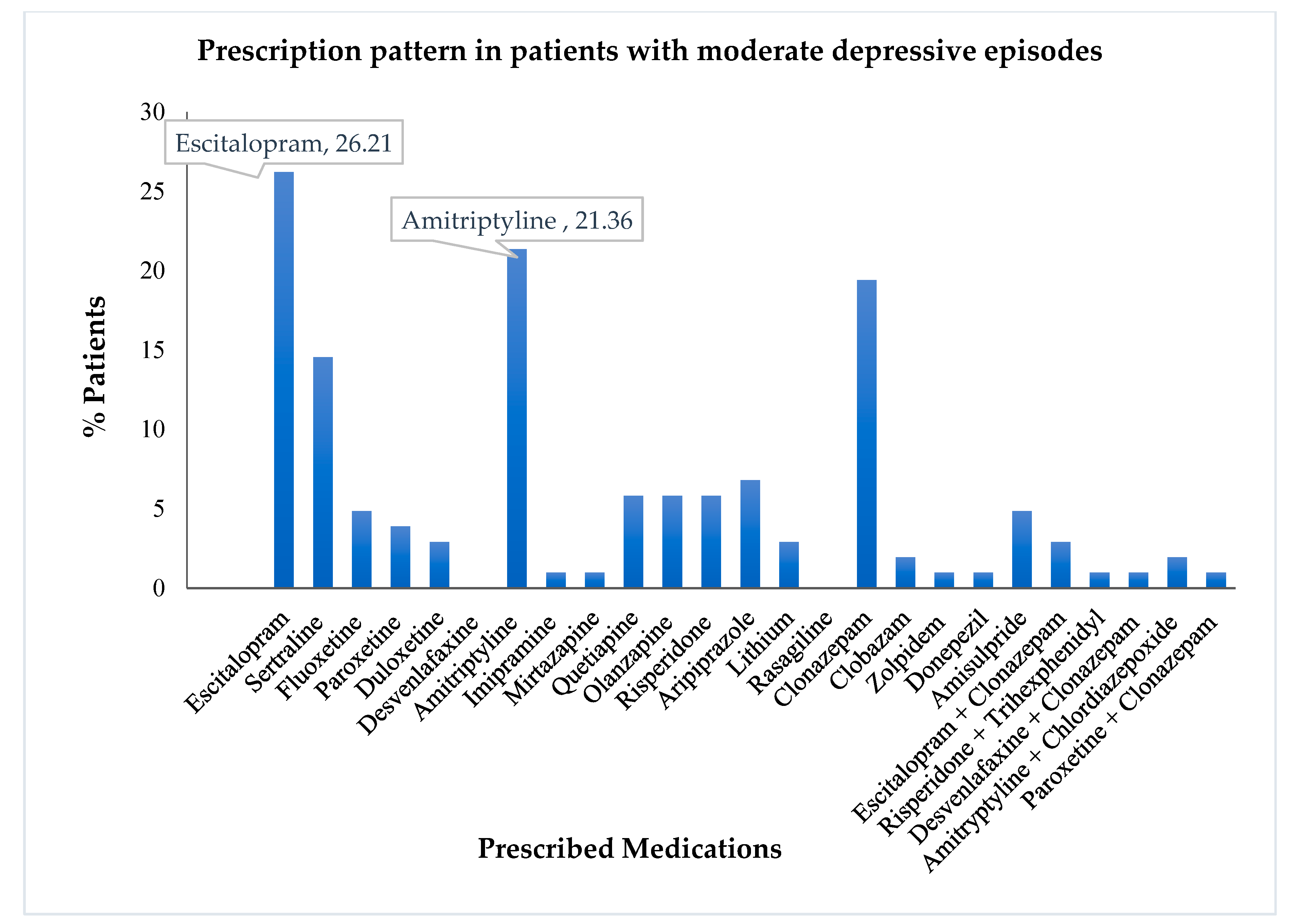
- A similar analysis was performed using the drug use pattern data among moderately depressive patients. The visual representation of the same is depicted in Figure 3. Similar to the treatment pattern discussed previously, moderate depressive episodes utilized escitalopram, amitriptyline, sertraline, and clonazepam, as the most commonly prescribed drugs.
- It was found that most patients were treated either with monotherapy or dual therapy. These patients amounted to a cumulative total of 92.67%. Only 6.67% of patients were treated with triple therapy, while an even smaller number (0.67%) were treated using the quadruple therapeutic approach.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Avanthi, E.; Somashekar, H.; Kumar, L.; Sushma, H.; Sudarshan, C.; Raja, B. Prescribing pattern of antidepressants in psychiatric unit of a tertiary care hospital. Int. J. Basic Clin. Pharmacol. 2014, 3, 667–670. [Google Scholar] [CrossRef]
- Chand, S.P.; Arif, H.; Kutlenios, R.M. Depression (Nursing); StatPearls Publishing: Treasure Island, FL, USA, 2021. [Google Scholar]
- O’Donnell, J.M.; Shelton, R.C. Drug Therapy of Depression and Anxiety Disorders. In Goodman and Gilman’s the Pharmacological Basis of Therapeutics; McGraw-Hill: New York, NY, USA, 2012; pp. 397–415. [Google Scholar]
- Funk, C.S.M.; Hart, X.M.; Gründer, G.; Hiemke, C.; Elsner, B.; Kreutz, R.; Riemer, T.G. Is therapeutic drug monitoring relevant for antidepressant drug therapy? Implications from a systematic review and meta-analysis with focus on moderating factors. Front. Psychiatry 2022, 13, E184. [Google Scholar] [CrossRef] [PubMed]
- Uchida, N.; Chong, M.Y.; Tan, C.H.; Nagai, H.; Tanaka, M.; Lee, M.S.; Fujii, S.; Yang, S.Y.; Si, T.; Sim, K.; et al. International study on antidepressant prescription pattern at 20 teaching hospitals and major psychiatric institutions in East Asia: Analysis of 1898 cases from China, Japan, Korea, Singapore and Taiwan. Psychiatry Clin. Neurosci. 2007, 61, 522–528. [Google Scholar] [CrossRef]
- Lunghi, C.; Antonazzo, I.C.; Burato, S.; Raschi, E.; Zoffoli, V.; Forcesi, E.; Sangiorgi, E.; Menchetti, M.; Roberge, P.; Poluzzi, E. Prevalence and Determinants of Long-Term Utilization of Antidepressant Drugs: A Retrospective Cohort Study. Neuropsychiatr. Dis. Treat. 2020, 16, 1157–1170. [Google Scholar] [CrossRef] [PubMed]
- Pillai, A.; Keyes, K.M.; Susser, E. Antidepressant prescriptions and adherence in primary care in India: Insights from a cluster randomized control trial. PLoS ONE 2021, 16, e0248641. [Google Scholar] [CrossRef]
- Gilså Hansen, D.; Søndergaard, J.; Vach, W.; Freng Gram, L.; Rosholm, J.U.; Kragstrup, J. Antidepressant drug use in general practice: Inter-practice variation and association with practice characteristics. Eur. J. Clin. Pharmacol. 2003, 59, 143–149. [Google Scholar] [CrossRef]
- Pirraglia, P.A.; Stafford, R.S.; Singer, D.E. Trends in prescribing of selective serotonin reuptake inhibitors and other newer antidepressant agents in adult primary care. Prim. Care Companion J. Clin. Psychiatry 2003, 5, 153–157. [Google Scholar] [CrossRef] [Green Version]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Saleem, S.M.; Jan, S.S. Modified Kuppuswamy socioeconomic scale updated for the year 2021. Indian J. Foren. Community Med. 2021, 8, 1–3. [Google Scholar] [CrossRef]
- WHO Fact Sheet Depression. Available online: https://www.who.int/news-room/fact-sheets/detail/depression (accessed on 21 August 2022).
- Alonso, J.; Angermeyer, M.C.; Bernert, S.; Bruffaerts, R.; Brugha, T.S.; Bryson, H.; De Girolamo, G.; De Graaf, R.; Demyttenaere, K.; Gasquet, I.; et al. Psychotropic drug utilization in Europe: Results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr. Scand. Suppl. 2004, 109, 55–64. [Google Scholar] [CrossRef]
- Freeman, A.; Tyrovolas, S.; Koyanagi, A.; Chatterji, S.; Leonardi, M.; Ayuso-Mateos, J.L.; Tobiasz-Adamczyk, B.; Koskinen, S.; Rummel-Kluge, C.; Haro, J.M. The role of socioeconomic status in depression: Results from the COURAGE (aging survey in Europe). BMC Public Health 2016, 16, E1098. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shidhaye, R.; Patel, V. Association of socioeconomic, gender and health factors with common mental disorders in women: A population-based study of 5703 married rural women in India. Int. J. Epidemiol. 2010, 39, 1510–1521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cohen, A.K.; Nussbaum, J.; Weintraub, M.L.R.; Nichols, C.R.; Yen, I.H. Association of adult depression with educational attainment, aspirations, and expectations. Prev. Chronic Dis. 2020, 17, E94. [Google Scholar] [CrossRef] [PubMed]
- Jain, R.; Larsuphrom, P.; Degremont, A.; Latunde-Dada, G.O.; Philippou, E. Association between vegetarian and vegan diets and depression: A systematic review. Nutr. Bull. 2022, 47, 27–49. [Google Scholar] [CrossRef]
- Gorwood, P.; Weiller, E.; Lemming, O.; Katona, C. Escitalopram prevents relapse in older patients with major depressive disorder. Am. J. Geriatr. Psychiatry 2007, 15, 581–593. [Google Scholar] [CrossRef] [PubMed]
- Kirino, E. Escitalopram for the management of major depressive disorder: A review of its efficacy, safety, and patient acceptability. Patient Prefer. Adherence 2012, 6, 853–861. [Google Scholar] [CrossRef] [Green Version]
- Hegerl, U.; Hautzinger, M.; Mergl, R.; Kohnen, R.; Schütze, M.; Scheunemann, W.; Allgaier, A.K.; Coyne, J.; Henkel, V. Effects of pharmacotherapy and psychotherapy in depressed primary-care patients: A randomized, controlled trial including a patients’ choice arm. Int. J. Neuropsychopharmacol. 2010, 13, 31–44. [Google Scholar] [CrossRef] [Green Version]
- National Collaborating Centre for Mental Health (UK). Depression in Adults with a Chronic Physical Health Problem. 2010. Available online: https://pubmed.ncbi.nlm.nih.gov/22259826/ (accessed on 20 August 2022).
- Fochtmann, L.J.; Gelenberg, A.J. Guideline watch: Practice guideline for the treatment of patients with major depressive disorder. Focus 2005, 3, 34–42. [Google Scholar] [CrossRef]
- Trivedi, J.K.; Dhyani, M.; Sareen, H.; Yadav, V.S.; Rai, S.B. Anti-depressant drug prescription pattern for depression at a tertiary health care center of Northern India. Med. Pract. Rev. 2010, 1, 16–18. [Google Scholar]
- Grover, S.; Avasth, A.; Kalita, K.; Dalal, P.; Rao, G.; Chadda, R.; Lakdawala, B.; Bang, G.; Chakraborty, K.; Kumar, S.; et al. IPS multicentric study: Antidepressant prescription patterns. Indian J. Psychiatry 2013, 55, 41–45. [Google Scholar] [CrossRef]
- Tripathi, A.; Avasthi, A.; Desousa, A.; Bhagabati, D.; Shah, N.; Kallivayalil, R.A.; Grover, S.; Trivedi, J.K.; Shinfuku, N. Prescription pattern of antidepressants in five tertiary care psychiatric centres of India. Indian J. Med. Res. 2016, 143, 507–513. [Google Scholar] [CrossRef] [PubMed]
- Goto, M.; Yoshimura, R.; Kakihara, S.; Shinkai, K.; Yamada, Y.; Kaji, K.; Ueda, N.; Nakamura, J. Risperidone in the treatment of psychotic depression. Prog. Neuropsychopharmacol. Biol. Psychiatry 2006, 30, 701–707. [Google Scholar]
- WJPR-Abstract. Available online: https://wjpr.net/abstract_show/15314 (accessed on 20 August 2022).
- WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC Classification and DDD Assignment, 5th ed.; WHO: Oslo, Norway, 2002; ISBN 9788290312386. [Google Scholar]
- Aburamadan, H.A.; Sridhar, S.B.; Tadross, T.M.; Shariff, A. Assessment of Prescription Pattern of Antipsychotic Medications in a Psychiatry Inpatient Setting of a Secondary Care Hospital of United Arab Emirates. Clin Schizophr Relat Psychoses. 2021, 15, S8. [Google Scholar]



| Demographics | No. of Patients (%) |
|---|---|
| Gender | |
| Male | 49 (31.8) |
| Female | 105 (68.2) |
| Education | |
| Illiterate | 44 (28.5) |
| High school certificate | 43 (28) |
| Intermediate/diploma | 20 (13) |
| Graduate | 22 (14.3) |
| Primary school certificate | 17 (11) |
| Middle school certificate | 8 (5.2) |
| Occupation | |
| Professionals | 7 (4.5) |
| Clerks | 1 (0.6) |
| Skilled Workers and Shop & Market Sales Workers | 11 (7.1) |
| Skilled Agricultural & Fishery Workers | 9 (5.8) |
| Plant & Machine Operators and Assemblers | 2 (1.3) |
| Elementary Occupation | 4 (2.6) |
| Unemployed | 120 (78) |
| Monthly income (INR) | |
| 46,129–61,662 | 8 (5.2) |
| 30,831–46,128 | 79 (51.3) |
| 18,497–30,830 | 45 (29.2) |
| 6175–18,496 | 22 (14.3) |
| Socioeconomic class | |
| Upper Middle (II) | 7 (4.5) |
| Lower Middle (III) | 31 (20.1) |
| Upper Lower (IV) | 98 (63.6) |
| Lower (V) | 18 (11.7) |
| Marital status | |
| Single | 23 (14.9) |
| Married | 126 (81.8) |
| Widow | 5 (3.2) |
| Social habits | |
| Alcohol use | 8 (5.2) |
| Tobacco use | 13 (8.4) |
| Alcohol and tobacco use | 10 (6.5) |
| None | 123 (79.8) |
| Residence | |
| Rural | 97 (63) |
| Urban | 57 (37) |
| Diet habits | |
| Non-vegetarian | 113 (73.3) |
| Vegetarian | 41 (26.6) |
| Drug Name | No. of Patients (%) | ATC Code | PDD (mg) | DDD (mg) | PDD/DDD | Mild Depression [n = 32 (%)] | Moderate Depression [n = 103 (%)] | Moderately Severe [n = 15 (%)] | Moderately Severe with Psychotic Symptoms [n = 4 (%)] |
|---|---|---|---|---|---|---|---|---|---|
| Selective serotonin reuptake inhibitors (SSRIs) | |||||||||
| Escitalopram | 37 | N06AB10 | 16 | 10 | 1.6 | 6 (18.75) | 27 (26.21) | 3 (20) | 1 (25) |
| Sertraline | 26 | N06AB06 | 57 | 50 | 1.1 | 8 (25) | 15 (14.56) | 2 (13.33) | 1 (25) |
| Fluoxetine | 9 | N06AB03 | 9.7 | 20 | 0.5 | 1 (3.125) | 5 (4.85) | 3 (20) | 0 |
| Paroxetine | 4 | N06AB05 | 22 | 20 | 1.1 | 0 | 4 (3.88) | 0 | 0 |
| Serotonin and norepinephrine reuptake inhibitors (SNRIs) | |||||||||
| Duloxetine | 3 | N06AX21 | 33 | 60 | 0.5 | 0 | 3 (2.91) | 0 | 0 |
| Desvenlafaxine | 1 | N06AX23 | 50 | 50 | 1 | 1 (3.125) | 0 | 0 | 0 |
| Tricyclic antidepressants | |||||||||
| Amitriptyline | 33 | N06AA09 | 20 | 75 | 0.26 | 6 (18.75) | 22 (21.36) | 4 (26.67) | 0 |
| Imipramine | 1 | N06AA02 | 25 | 100 | 0.25 | 0 | 1 (0.97) | 0 | 0 |
| Serotonin and α-2 adrenergic antagonists | |||||||||
| Mirtazapine | 2 | N06AX11 | 7.5 | 30 | 0.25 | 0 | 1 (0.97) | 1 (6.67) | 0 |
| Diazepines, oxazepines, thiazepines and oxepines | |||||||||
| Quetiapine | 10 | N05AH04 | 108 | 400 | 0.27 | 2 (6.25) | 6 (5.83) | 0 | 2 (50) |
| Olanzapine | 8 | N05AH03 | 8.75 | 10 | 0.87 | 2 (6.25) | 6 (5.83) | 0 | 0 |
| Other antipsychotics | |||||||||
| Risperidone | 15 | N05AX08 | 1.63 | 5 | 0.32 | 4 (12.5) | 6 (5.83) | 0 | 0 |
| Aripiprazole | 11 | N05AX12 | 8.45 | 15 | 0.56 | 3 (9.375) | 7 (6.80) | 0 | 1 (25) |
| Lithium | 5 | N05AN01 | 482.6 | 1773.3 | 0.27 | 1 (3.125) | 3 (2.91) | 0 | 1 (25) |
| Monoamine oxidase B inhibitors | |||||||||
| Rasagiline | 1 | N04BD02 | 1 | 1 | 1 | 1 (3.125) | 0 | 0 | 0 |
| Benzodiazepine derivative | |||||||||
| Clonazepam | 31 | N03AE01 | 1.9 | 8 | 0.23 | 7 (21.875) | 20 (19.42) | 5 (33.33) | 0 |
| Clobazam | 4 | N05BA09 | 7.5 | 20 | 0.37 | 2 (6.25) | 2 (1.94) | 0 | 0 |
| Zolpidem | 1 | N05CF02 | 5 | 10 | 0.5 | 0 | 1 (0.97) | 0 | 0 |
| Anticholinergics | |||||||||
| Donepezil | 3 | N06DA02 | 5 | 7.5 | 0.66 | 2 (6.25) | 1 (0.97) | 0 | 0 |
| Benzamides | |||||||||
| Amisulpride | 5 | N05AL05 | 160 | 400 | 0.4 | 0 | 5 (4.85) | 0 | 0 |
| Fixed dose combination therapy | |||||||||
| Escitalopram + Clonazepam | 5 | Not Applicable | 1 (3.125) | 3 (2.91) | 1 (6.67) | 0 | |||
| Risperidone + Trihexyphenidyl | 4 | Not Applicable | 1 (3.125) | 1 (0.97) | 0 | 2 (50) | |||
| Desvenlafaxine + Clonazepam | 3 | Not Applicable | 0 | 1 (0.97) | 2 (13.33) | 0 | |||
| Amitryptyline + Chlordiazepoxide | 2 | Not Applicable | 0 | 2 (1.94) | 0 | 0 | |||
| Paroxetine + Clonazepam | 2 | Not Applicable | 0 | 1 (0.97) | 1 (6.67) | 0 | |||
| Type of Drug Therapy | Drug Name | No. of Patients [n = 150 (%)] |
|---|---|---|
| Monotherapy | 70 (46.6) | |
| One antidepressant (n = 40, 26.6%) | Amitriptyline | 14 (9.3) |
| Escitalopram | 13 (8.6) | |
| Sertraline | 6 (4) | |
| Fluoxetine | 4 (2.6) | |
| Desvenlafaxine | 1 (0.6) | |
| Imipramine | 1 (0.6) | |
| Mirtazapine | 1 (0.6) | |
| One psychotropic drug (n = 30, 20%) | Clonazepam | 8 (5.3) |
| Risperidone | 8 (5.3) | |
| Quetiapine | 6 (4) | |
| Aripiprazole | 3 (2) | |
| Olanzapine | 2 (1.3) | |
| Amisulpride | 2 (1.3) | |
| Lithium | 1 (0.6) | |
| Dual therapy | 69 (46) | |
| Two antidepressants (n = 13, 8.6%) | Escitalopram and amitriptyline | 9 (6) |
| Sertraline and amitriptyline | 2 (1.3) | |
| Escitalopram and mirtazapine | 1 (0.6) | |
| Paroxetine and amitriptyline | 1 (0.6) | |
| Two psychotropic drugs (n = 7, 4.6%) | Clonazepam and risperidone | 1 (0.6) |
| Rasagiline and donepezil | 1 (0.6) | |
| Quetiapine and aripiprazole | 1 (0.6) | |
| Amisulpride and aripiprazole | 1 (0.6) | |
| Olanzapine and lithium | 1 (0.6) | |
| Olazapine and clobazam | 1 (0.6) | |
| Clobazam and donepezil | 1 (0.6) | |
| One antidepressant and one psychotropic drug (n = 39, 26%) | Sertraline and clonazepam | 8 (5.3) |
| Escitalopram and clonazepam | 6 (4) | |
| Escitalopram and aripiprazole | 4 (2.6) | |
| Sertraline and risperidone | 4 (2.6) | |
| Fluoxetine and clonazepam | 2 (1.3) | |
| Duloxetine and quetiapine | 2 (1.3) | |
| Escitalopram and lithium | 2 (1.3) | |
| Amitriptyline and clonazepam | 1 (0.6) | |
| Duloxetine and clonazepam | 1 (0.6) | |
| Paroxetine and aripiprazole | 1 (0.6) | |
| Sertraline and amisulpride | 1 (0.6) | |
| Paroxetine and amisulpride | 1 (0.6) | |
| Fluoxetine and zolpidem | 1 (0.6) | |
| Escitalopram and olanzapine | 1 (0.6) | |
| Sertraline and olanzapine | 1 (0.6) | |
| Amitriptyline and olanzapine | 1 (0.6) | |
| Escitalopram and clobazam | 1 (0.6) | |
| Amitriptyline and clobazam | 1 (0.6) | |
| Combination therapy (n = 10, 6.6%) | Desvenalafaxine + clonazepam | 3 (2) |
| Escitalopram + clonazepam | 3 (2) | |
| Risperidone + trihexyphenidyl | 2 (1.3) | |
| Amitriptyline + chlordiazepoxide | 2 (1.3) | |
| Triple therapy | 10 (6.6) | |
| Two antidepressants and one psychotropic drug (n = 1, 0.6%) | Sertraline, fluoxetine and clonazepam | 1 (0.6) |
| One antidepressant and two psychotropic drug (n = 4, 2.6%) | Fluoxetine, donepezil and risperidone | 1 (0.6) |
| Sertraline, clonazepam and risperidone | 1 (0.6) | |
| Sertraline, clonazepam and olanzapine | 1 (0.6) | |
| Paroxetine, clonazepam and aripiprazole | 1 (0.6) | |
| One combination therapy and one antidepressant (n = 5, 3.3%) | Escitalopram + clonazepam and amitriptyline | 2 (1.3) |
| Paroxetine + clonazepam and amitriptyline | 1 (0.6) | |
| Paroxetine + clonazepam and amitriptyline | 1 (0.6) | |
| Risperidone + trihexyphenidyl and sertraline | 1 (0.6) | |
| Quadruple therapy (n = 1, 0.6%) | Risperidone + trihexyphenidyl, quetiapine, and lithium | 1 (0.6) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mehdi, S.; Manohar, K.; Shariff, A.; Wani, S.U.D.; Almuqbil, M.; Alshehri, S.; Shakeel, F.; Imam, M.T.; Krishna, K.L. Analysis of Antidepressants Utilization for Patients Visiting Psychiatric Out-Patient Clinic in a Tertiary Care Hospital. Healthcare 2022, 10, 2081. https://doi.org/10.3390/healthcare10102081
Mehdi S, Manohar K, Shariff A, Wani SUD, Almuqbil M, Alshehri S, Shakeel F, Imam MT, Krishna KL. Analysis of Antidepressants Utilization for Patients Visiting Psychiatric Out-Patient Clinic in a Tertiary Care Hospital. Healthcare. 2022; 10(10):2081. https://doi.org/10.3390/healthcare10102081
Chicago/Turabian StyleMehdi, Seema, Kishor Manohar, Atiqulla Shariff, Shahid Ud Din Wani, Mansour Almuqbil, Sultan Alshehri, Faiyaz Shakeel, Mohammad T. Imam, and Kamsagara L. Krishna. 2022. "Analysis of Antidepressants Utilization for Patients Visiting Psychiatric Out-Patient Clinic in a Tertiary Care Hospital" Healthcare 10, no. 10: 2081. https://doi.org/10.3390/healthcare10102081
APA StyleMehdi, S., Manohar, K., Shariff, A., Wani, S. U. D., Almuqbil, M., Alshehri, S., Shakeel, F., Imam, M. T., & Krishna, K. L. (2022). Analysis of Antidepressants Utilization for Patients Visiting Psychiatric Out-Patient Clinic in a Tertiary Care Hospital. Healthcare, 10(10), 2081. https://doi.org/10.3390/healthcare10102081







