Hospital Management and Public Health Role of National Hospitals after Transformation into Independent Administrative Agencies
Abstract
1. Introduction
2. Materials and Methods
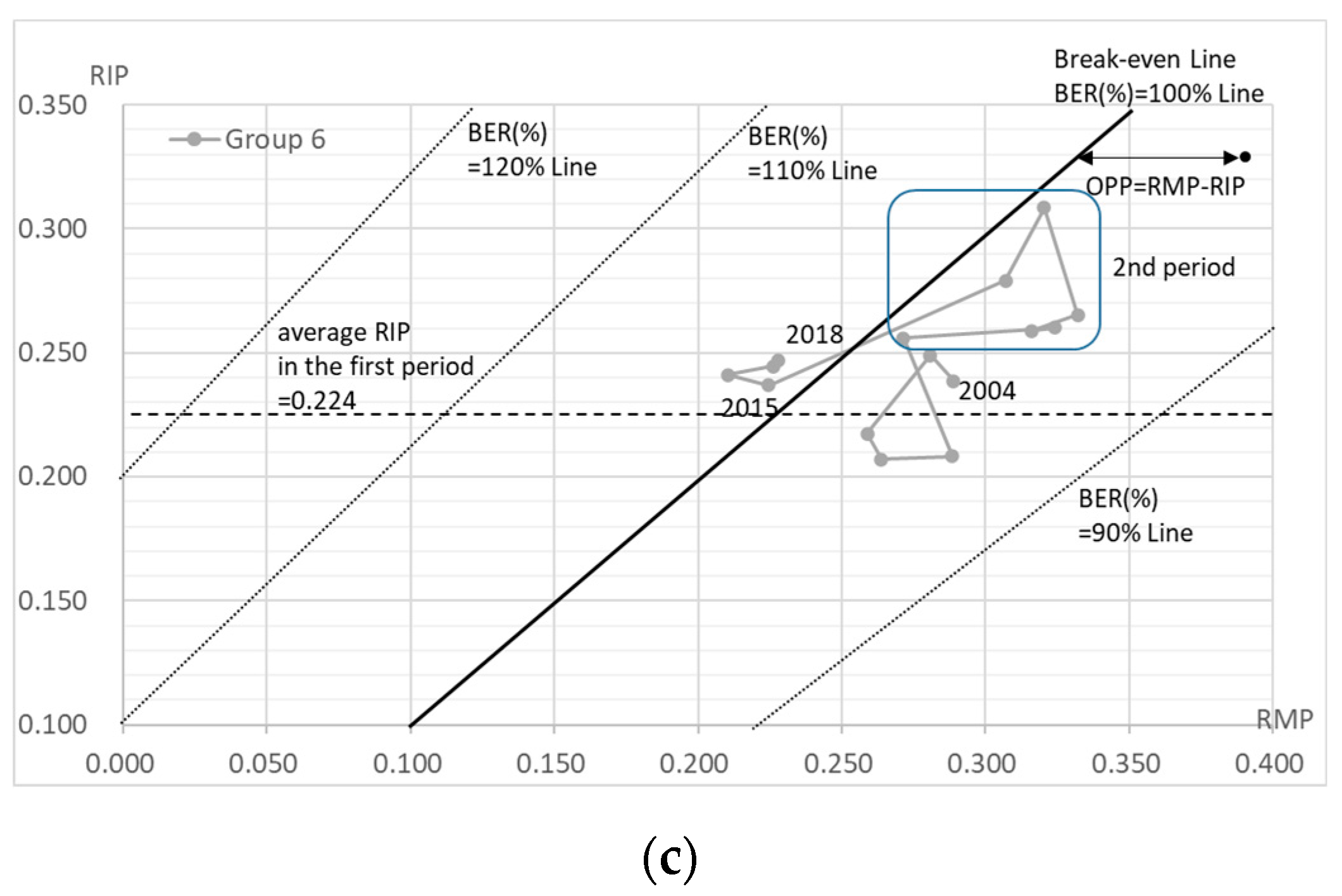
- Indicator 1: Ratio of the marginal profit after personnel cost per personnel cost (RMP), as follows:
- Indicator 2: Ratio of investment (= indirect cost) per personnel cost (RIP), as follows:
- Indicator 3: Operation profit per USD 1 of personnel cost (OPP) (difference between the RMP and the RIP), follows:
- The indicator OPP represents the efficiency of medical management.
3. Results
3.1. Medical Revenue
3.2. Personnel-Related Expenses
3.3. Material Costs
3.4. Capital Investment Expenses
3.5. RMP, RIP, OPP, and BER
3.6. Free Cash Flow (FCF)
3.7. Number of Hospital Beds
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ikegami, N.; Campbell, J.C. Health care reform in Japan: The virtues of muddling through. Health Aff. 1999, 18, 56–75. [Google Scholar] [CrossRef] [PubMed]
- Ikegami, N.; Yoo, B.; Hashimoto, H.; Matsumoto, M.; Ogata, H.; Babazono, A.; Watanabe, R.; Shibuya, K.; Yang, B.M.; Reich, M.R.; et al. Japan: Universal Health Care at 50 Years 2: Japanese universal health coverage: Evolution, achievements, and challenges. Lancet 2011, 378, 1106–1115. [Google Scholar] [CrossRef]
- Huntington, D. Public Hospital Governance in the Asia Pacific Region–Drivers of Change. In Public Hospital Governance in Asia and the Pacific; Huntington, D., Hort, K., Eds.; World Health Organization Regional Office for the Western Pacific: Manila, Philippines, 2015; pp. 2–25. [Google Scholar]
- Nakagawa, Y.; Ito, M.; Nakagawa, Y. Analysis of financial status and personnel investment of National Hospital Organization (NHO) in Japan. J. Jpn. Soc. Health Care Manag. 2018, 19, 109–114. [Google Scholar]
- Tagawa, Y.; Tsugawa, Y.; Ikegami, N. National Hospital Reform in Japan: Results and Challenges. In Universal Health Coverage for Inclusive and Sustainable Development: Lessons from Japan; Ikegami, N., Ed.; World Bank Group: Washington, DC, USA, 2014; pp. 149–162. [Google Scholar]
- Act on the National Hospital Organization, Independent Administrative Agency. 2002. Available online: https://elaws.e-gov.go.jp/document?law_unique_id=414AC0000000191_20150801_000000000000000 (accessed on 18 October 2022).
- Results of the Final Evaluation of the Performance of the Independent Administrative Agencies National Hospital Agency in Relation to its Mid-Term Objectives.–1st Period. Available online: https://nho.hosp.go.jp/files/000027938.pdf (accessed on 3 October 2022).
- Results of the Final Evaluation of the Performance of the Independent Administrative Agencies National Hospital Agency in Relation to Its Mid-Term Objectives.–2nd Period. Available online: https://nho.hosp.go.jp/files/000034104.pdf (accessed on 3 October 2022).
- Results of the Final Evaluation of the Performance of the Independent Administrative Agencies National Hospital Agency in Relation to Its Mid-Term Objectives.–3rd Period. Available online: https://nho.hosp.go.jp/files/000115005.pdf (accessed on 3 October 2022).
- Nakanishi, W. Independent administrative institutions (dokuritsu gyosei hojin): Passage of revised and maintenance Acts. Law Res. 2014, 357, 3–22. [Google Scholar]
- Furukawa, S. Independent administrative institutions (dokuritsu gyosei hojin): Institutional design and political process. J. Public Policy Stud. 2001, 1, 166–178. [Google Scholar]
- Uchiyama, Y. Policy Diffusion and political institutions: Comparing administrative reforms in Japan and the United Kingdom. J. Public Policy Stud. 2005, 5, 119–129. [Google Scholar]
- Shibata, Y. National Hospital Special Accounting. In Heisei Fiscal History: 1989–2000; Hayashi, K., Ishi, H., Horiuchi, A., Eds.; Ministry of Finance, Policy Research Institute: Tokyo, Japan, 2012; Volume 3, pp. 206–212. [Google Scholar]
- Outline of the National Hospital Special Account Scheme. Available online: https://www.mhlw.go.jp/wp/yosan/other/zaimu0307/dl/1-3.pdf (accessed on 24 May 2022).
- National Hospital Special Accounting. Available online: https://www.mhlw.go.jp/wp/yosan/other/syocho02/dl/6.pdf (accessed on 24 May 2022).
- Report on the Inspection of Accounts for 2003. Available online: https://report.jbaudit.go.jp/org/h15/2003-h15-1325-0.htm (accessed on 24 May 2022).
- Nakagawa, Y.; Takemura, T.; Yoshihara, H.; Nakagawa, Y. Financial analysis at the National Hospital Organization’s hospitals-introducing new financial management indicators based on personnel cost. J. Jpn. Soc. Health Care Manag. 2010, 11, 15–23. [Google Scholar]
- Report on the Inspection of the Financial Statements for the Financial Year 2017. pp. 928–948. Available online: https://report.jbaudit.go.jp/org/pdf/H29kensahoukoku.pdf (accessed on 24 May 2022).
- National Hospital Organization-Financial Statements. Available online: https://nho.hosp.go.jp/disclosure/disclosure_zaimu.html (accessed on 24 May 2022).
- Nakagawa, Y.; Yoshihara, H.; Nakagawa, Y. A new cost accounting model and new indicators for hospital management based on personnel cost. In Management Engineering for Effective Healthcare Delivery: Principles and Applications; Pierce, S., Alexander, K., Eds.; IGI Global: Hershey, PA, USA, 2011; pp. 419–434. [Google Scholar]
- Nakagawa, Y.; Yoshihara, H.; Nakagawa, Y. New indicators based on personnel cost for management efficiency in a hospital. J. Med. Syst. 2011, 35, 625–637. [Google Scholar] [CrossRef]
- Kakinaka, M.; Kato, R. Regulated medical fee schedule of the Japanese health care system. Int. J. Health Care Financ. Econ. 2013, 13, 301–317. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ikegami, N. Controlling Health Expenditures by Revisions to the Fee Schedule in Japan. In Universal Health Coverage for Inclusive and Sustainable Development: Lessons from Japan; Ikegami, N., Ed.; World Bank Group: Washington, DC, USA, 2014; pp. 69–100. [Google Scholar]
- World Health Statistics 2022: Monitoring Health for the SDGs, Sustainable Development Goals. Available online: https://apps.who.int/iris/rest/bitstreams/1435584/retrieve (accessed on 3 October 2022).
- Health at a Glance 2021. Available online: https://www.oecd-ilibrary.org/deliver/ae3016b9-en.pdf?itemId=%2Fcontent%2Fpublication%2Fae3016b9-en&mimeType=pdf (accessed on 3 October 2022).
- The Small and Medium Enterprise Agency. Part 2: The Ability to Overcome the Crisis-Chapter 1: The Financial Basis of Small and Medium-Sized Enterprises and Management Strategies in the Face of the Impact of Infectious Diseases. 2021 White Paper on Small and Medium Enterprises in Japan; The Small and Medium Enterprise Agency, Ed.; The Small and Medium Enterprise Agency: Tokyo, Japan, 2021; pp. II-6–II-7. [Google Scholar]
- Campbell, J.C.; Takagi, Y. The political economy of the fee schedule in Japan. In Universal Health Coverage for Inclusive and Sustainable Development: Lessons from Japan; Ikegami, N., Ed.; World Bank Group: Washington, DC, USA, 2014; pp. 101–118. [Google Scholar]
- Social Insurance Medical Council Act. 1950. Available online: https://www.japaneselawtranslation.go.jp/en/laws/view/3266/en (accessed on 25 September 2022).
- List of members of the Central Social Insurance Medical Council. Available online: https://www.mhlw.go.jp/content/12404000/000851671.pdf (accessed on 24 May 2022).
- Yuta, K. Impact of university reform on research performance aggregated and disaggregated across research fields: A case study of the partial privatization of Japanese national universities. Jpn. Econ. Rev. 2021, 6, 1–27. Available online: https://link.springer.com/article/10.1007/s42973-021-00074-y (accessed on 24 May 2022).









| Classification by Type of Establishment | National | NHO | Public Hospital | Private |
|---|---|---|---|---|
| Act on Basis for Establishment | Law for Establishing Jurisdiction | Act on the National Hospital Organization, Independent Administrative Agency. | Local Public Enterprise Act/Articles of Incorporation | Medical Care Act. |
| Establishers | The competent minister | Chairman of the board of directors | Head of the local government/Business Manager | Hospital Administrator |
| Appointing authority of the establisher | The competent minister | Minister of Health, Labor and Welfare, National | Head of the local government | Hospital Administrators |
| Status of the establisher | Specialized National Public Servants | Non-government officer | Local government officer | Non-government officer |
| Director Appointee | - | The competent minister | - | Establishers |
| Method of Election of Executive Board Members | - | The competent minister | - | Board of directors/Establishers |
| Management organization | The ministry in charge | Board of directors | Hospital Organization | Board of directors/Establishers |
| Operation Plans | The ministry in charge | Board of directors | Hospital Organization/Local government that has established | Board of directors/Establishers |
| Approval of operating plan | The competent minister | The competent minister | Local government that has established | Board of directors/Establishers |
| Approval of Management Report | The competent minister/Council in charge | The competent minister/Council in charge | Local government that has established | Board of directors/Establishers |
| Sponsor of a capital | National government | National government | Local government that has established | Own private financial resources |
| Budget Approval | Congress | Board of directors | parliament | Board of directors/Establishers |
| Financial Repor | Congress | The competent minister | Ministry of Internal Affairs and Communications/Established local governments | Board of directors/Establishers |
| Advisory board | Council of Ministries and Agencies | Committee on the system of evaluating incorporated administrative agencies | Local Self-Governance Committee | Consultant firms, etc. |
| Investment funds | Special Accounts | FILP system/Own Assets | Municipal accounting | Own Assets/Bank |
| Hospital Administrator (Hospital Director) | A person who has been registered under Article 16-6, paragraph (1) of the Medical Practitioners’ Act as stipulated in Article 7, paragraph (1) of the Medical Care Act. | |||
| Hospital administrator’s appointee | The competent minister | Chairman of the board of directors | Head of the local government | Chairman of the board of directors/Hospital Administrator |
| Licensor for the establishment of hospitals | Prefectural Governor | |||
| Limitations of opening | Prefectural Governor | |||
| Authority to limit the number of hospital beds | Prefectural Governor | |||
| Status of Employees | Government officer | Private | Local government officer | Private |
| Status under the Criminal Code | Government officer | Public officer | Local government officer | Private |
| Government’s right to command and control | Has command and control authority. | The Minister of Health, Labor and Welfare may request the implementation of operations in the event of a disaster or public health crisis. | - | - |
| Operational Supervisory Authority | The competent minister | Prefectural Governor | ||
| Public audits on insurance treatment | Regional Bureau of Health and Welfare (Ministry of Health, Labour and Welfare) | |||
| Surplus Profit | Surpluses must in principle be paid into the national treasury | Surpluses after the end of the medium-term target period are managed by the agency for the next medium-term target period if they are approved by the competent minister, and if permission is not granted, the part of the surplus that has not been planned for use in the next plan must be returned to the national treasury. | Local government | Transfer of assets |
| Target item | Final review of medium-term | ||||
| Medium-term plan | 1 | 2 | 3 | ||
| I. Matters concerning the improvement of the quality of services and other operations provided to the public | |||||
| Clinical Services | |||||
| Providing Medical Care | A | A | B | ||
| Providing Safe and Reliable Medical Care | A | A | |||
| High-Quality Medical Care | S | S | Reclassified. | ||
| Contribution to National Health Care Policy | ― | ― | A | ||
| Contribution to Local Medical Services | ― | S | A | ||
| Clinical Research Business | S | S | A | ||
| Education and Training Business | A | S | B | ||
| II. Matters related to the efficiency of business management | |||||
| Efficient Business Operation Structure | A | A | B | ||
| Improvement of Efficiency of Business Operation, etc. | A | A | |||
| Effective Utilization of Medical Resources | S | S | |||
| Reduction of Expenses Related to Businesses Other Than Clinical Services, etc. | A | ― | |||
| Promotion of Information Technology | A | ― | |||
| Securing Revenue | ― | A | |||
| III. Matters Related to Improvement of Financial Status | |||||
| Budget, Income and Expenditure Plan and Financial Plan | ― | ― | B | ||
| Improvement of Management | S | A | |||
| Improvement of Fixed Liabilities Ratio | S | S | |||
| IV. Other matters | |||||
| Other Matters Concerning Business Operation as Provided for in the Ordinance of the Competent Ministry | A | A | B | ||
| Group | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | Average of 1st Period | Average of 2nd Period | Average of 3rd Period | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rate of increase in medical revenue | Group 1 | - | −0.1% | 0.3% | 6.3% | 2.6% | 6.2% | 9.1% | 5.1% | 2.7% | 2.4% | 0.8% | 1.3% | 3.3% | 0.3% | 4.3% | 2.3% | 5.1% | 2.0% |
| Group 2 | - | 3.3% | 0.4% | 6.7% | 1.2% | 5.9% | 9.6% | 4.3% | 4.5% | 2.5% | 1.9% | 5.1% | 0.5% | 3.6% | 5.0% | 2.9% | 5.4% | 3.2% | |
| Group 3 | - | 6.4% | 2.3% | 8.5% | 2.7% | 3.8% | 7.8% | 2.3% | 3.7% | 4.2% | 1.8% | 3.2% | 0.9% | 3.4% | 3.8% | 5.0% | 4.3% | 2.6% | |
| Group 4 | - | 5.9% | −2.4% | 2.9% | 3.3% | 2.1% | 2.9% | 1.1% | 0.4% | 3.7% | 2.2% | 2.2% | −0.7% | 0.6% | 4.9% | 2.4% | 2.1% | 1.8% | |
| Group 5 | - | 5.6% | 2.7% | 11.7% | 7.0% | 1.5% | 2.4% | 3.6% | −0.6% | 2.3% | 2.6% | −0.8% | −1.0% | 3.5% | 1.7% | 6.7% | 1.8% | 1.2% | |
| Group 6 | - | −0.8% | 0.3% | 3.6% | 9.1% | 2.6% | 5.6% | 2.5% | 3.3% | 8.3% | 0.0% | 3.1% | 3.2% | 4.1% | −3.1% | 3.1% | 4.5% | 1.5% | |
| Total | - | 3.4% | 0.0% | 5.6% | 4.0% | 3.7% | 6.4% | 2.9% | 2.7% | 4.0% | 1.3% | 2.2% | 1.1% | 2.1% | 2.9% | 3.3% | 4.0% | 1.9% | |
| Rate of increase in personnel -related expenses | Group 1 | - | 1.7% | 2.8% | 6.9% | 7.1% | 4.2% | 4.1% | 5.6% | 0.8% | 2.9% | 2.1% | 5.9% | 3.1% | 0.7% | 3.0% | 4.6% | 3.5% | 2.9% |
| Group 2 | - | 6.0% | 1.5% | 5.7% | 3.1% | 8.2% | 4.4% | 5.0% | 4.0% | 3.2% | 4.0% | 9.2% | 2.2% | 3.7% | 4.9% | 4.1% | 4.9% | 4.8% | |
| Group 3 | - | 8.9% | 4.1% | 8.2% | 4.1% | 5.3% | 3.8% | 4.4% | 2.5% | 5.9% | 4.6% | 7.2% | 2.8% | 2.0% | 2.4% | 6.3% | 4.4% | 3.8% | |
| Group 4 | - | 5.4% | −3.1% | 1.7% | 1.1% | 1.6% | 2.0% | 1.8% | 0.6% | 2.6% | 4.4% | 7.1% | 0.8% | 0.9% | 4.6% | 1.3% | 1.7% | 3.6% | |
| Group 5 | - | 12.5% | 2.6% | 6.8% | −0.2% | 1.4% | 1.3% | 1.1% | 0.9% | 2.7% | 3.3% | 5.4% | 1.6% | 1.6% | 1.3% | 5.4% | 1.5% | 2.6% | |
| Group 6 | - | −1.0% | 1.8% | 3.1% | 7.3% | 3.9% | 1.4% | 3.4% | 1.7% | 7.5% | 1.6% | 8.4% | 3.5% | 2.8% | −3.2% | 2.8% | 3.6% | 2.6% | |
| Total | - | 4.6% | 0.8% | 4.5% | 3.8% | 4.1% | 2.8% | 3.5% | 1.9% | 4.1% | 3.3% | 7.0% | 2.2% | 1.7% | 2.4% | 3.4% | 3.3% | 3.3% | |
| Rate of increase in material costs | Group 1 | - | −3.1% | 2.1% | 4.2% | 1.1% | 7.5% | 7.0% | 4.2% | −1.7% | 4.7% | −0.1% | 1.0% | 4.4% | −0.3% | 4.0% | 1.1% | 4.3% | 1.8% |
| Group 2 | - | 3.9% | −0.1% | 6.1% | 0.0% | 7.5% | 4.4% | 5.5% | 2.0% | 5.3% | 3.1% | 9.1% | 2.1% | 4.9% | 5.5% | 2.5% | 4.9% | 4.9% | |
| Group 3 | - | 6.9% | 3.1% | 7.1% | 3.2% | 6.2% | 5.5% | 4.0% | 3.5% | 7.0% | 5.8% | 7.5% | 1.9% | 2.9% | 2.9% | 5.1% | 5.2% | 4.2% | |
| Group 4 | - | 4.2% | −4.7% | 4.0% | 4.2% | 5.1% | 1.7% | 1.0% | 2.5% | 6.1% | 4.3% | 5.4% | −1.5% | −0.5% | 4.4% | 1.9% | 3.3% | 2.4% | |
| Group 5 | - | 5.6% | −2.1% | 4.9% | 3.0% | 0.8% | −0.5% | 5.4% | 4.5% | 2.4% | −0.4% | 5.7% | −3.5% | −3.0% | 3.8% | 2.9% | 2.5% | 0.5% | |
| Group 6 | - | 1.4% | 0.8% | 3.5% | 11.2% | 3.5% | 4.0% | 2.4% | 2.7% | 10.5% | 1.9% | 9.0% | 7.8% | 2.7% | −3.4% | 4.2% | 4.6% | 3.6% | |
| Total | - | 3.2% | 0.3% | 5.2% | 3.6% | 6.0% | 4.4% | 3.8% | 2.0% | 6.3% | 2.8% | 5.6% | 2.8% | 1.7% | 2.8% | 3.1% | 4.5% | 3.1% | |
| Rate of increase in capital investme nt expenses | Group 1 | - | −7.5% | −6.5% | 1.0% | 4.3% | 26.7% | 8.8% | 4.4% | 3.8% | 13.2% | 3.7% | −7.2% | 0.8% | 0.2% | −0.8% | −2.2% | 11.4% | −0.6% |
| Group 2 | - | 11.4% | 0.3% | −1.0% | 4.5% | 44.3% | 8.2% | 1.6% | 6.1% | 3.9% | 3.8% | −8.0% | −1.3% | 1.7% | 7.2% | 3.8% | 12.8% | 0.7% | |
| Group 3 | - | 2.6% | −11.6% | −0.7% | 1.2% | 32.8% | 8.7% | 0.8% | 5.9% | 11.9% | −0.1% | −11.7% | −3.4% | −3.7% | −1.1% | −2.1% | 12.0% | −4.0% | |
| Group 4 | - | 13.2% | −14.0% | −2.5% | 3.1% | 24.4% | 6.3% | 1.6% | 4.2% | 12.2% | 4.0% | −7.8% | −2.1% | 4.3% | 4.9% | 0.0% | 9.7% | 0.7% | |
| Group 5 | - | 18.0% | −7.5% | −4.4% | 1.6% | 27.7% | 7.4% | −10.9% | 11.0% | 8.0% | 0.7% | −6.5% | −5.9% | 0.7% | 3.5% | 1.9% | 8.6% | −1.5% | |
| Group 6 | - | 1.3% | −10.4% | −1.4% | 7.6% | 27.9% | 2.6% | 2.3% | 4.3% | 19.6% | −3.6% | −8.3% | 6.2% | 6.2% | −3.7% | −0.7% | 11.3% | −0.7% | |
| Total | - | 6.0% | −8.9% | −1.4% | 4.1% | 31.1% | 6.6% | 1.3% | 5.2% | 11.5% | 1.3% | −8.8% | −0.3% | 2.0% | 2.0% | 0.0% | 11.1% | −0.8% | |
| FCF (US$1 million) | Group 1 | −34.4 | 11.2 | 1.4 | 6.3 | −6.8 | −12.5 | −26.4 | −24.5 | −7.7 | −8.0 | −51.6 | −39.9 | 3.3 | −4.9 | 36.0 | −4.5 | −15.8 | −11.4 |
| Group 2 | 36.7 | −22.8 | 25.6 | 72.4 | −103.5 | −142.2 | 52.5 | 130.2 | 131.8 | 112.3 | 38.6 | −31.1 | 18.7 | 2.2 | −151.1 | 1.7 | 56.9 | −24.5 | |
| Group 3 | 45.7 | 113.4 | 139.3 | 141.5 | 123.9 | 78.7 | 145.4 | 96.0 | 97.3 | 119.0 | 81.2 | 89.7 | −19.9 | 71.7 | 22.0 | 112.8 | 107.3 | 48.9 | |
| Group 4 | −23.6 | 24.2 | 75.2 | 71.8 | 74.0 | 75.6 | 73.3 | 58.9 | 31.0 | −27.8 | −63.5 | −18.7 | 33.0 | −34.4 | −61.4 | 44.3 | 42.2 | −29.0 | |
| Group 5 | −14.4 | −1.5 | −7.8 | 9.6 | 21.4 | 23.8 | 17.2 | 27.4 | 4.1 | 3.6 | −21.0 | −51.5 | −2.1 | −4.0 | −3.1 | 1.5 | 15.2 | −16.3 | |
| Group 6 | 4.4 | 42.9 | 52.7 | 53.1 | 51.3 | 37.8 | 39.6 | 56.8 | 71.7 | −47.4 | −49.0 | −51.6 | −77.9 | −118.2 | −6.7 | 40.9 | 31.7 | −60.7 | |
| Total | 14.4 | 167.4 | 286.5 | 354.6 | 160.2 | 61.3 | 301.7 | 344.7 | 328.3 | 151.8 | −65.3 | −103.0 | −44.9 | −87.6 | −164.3 | 196.6 | 237.6 | −93.0 | |
| Number of Beds | Group 1 | 4854 | 4708 | 4558 | 4352 | 4014 | 3922 | 3899 | 3884 | 3929 | 3693 | 3793 | 4187 | 4187 | 4274 | 4222 | 4408 | 3865 | 4133 |
| Group 2 | 9454 | 9751 | 9858 | 9767 | 9784 | 9631 | 9728 | 9775 | 9735 | 9744 | 9725 | 9295 | 9271 | 8851 | 8711 | 9790 | 9723 | 9171 | |
| Group 3 | 8420 | 8412 | 8384 | 8357 | 8357 | 8369 | 8350 | 8324 | 8299 | 8164 | 8103 | 8051 | 8019 | 7984 | 7832 | 8378 | 8301 | 7998 | |
| Group 4 | 13,934 | 13,881 | 13,986 | 13,819 | 13,601 | 13,529 | 13,388 | 13,331 | 13,235 | 13,218 | 13,570 | 14,747 | 14,851 | 14,761 | 14,846 | 13,822 | 13,340 | 14,555 | |
| Group 5 | 4963 | 4816 | 4838 | 4574 | 4555 | 4554 | 4458 | 4459 | 4386 | 4322 | 4306 | 4312 | 4362 | 4291 | 4284 | 4696 | 4436 | 4311 | |
| Group 6 | 13,263 | 13,727 | 13,450 | 13,164 | 12,724 | 12,493 | 12,639 | 12,501 | 12,366 | 12,471 | 11,968 | 10,641 | 10,648 | 10,975 | 10,795 | 13,266 | 12,494 | 11,005 | |
| Total | 54,888 | 55,295 | 55,074 | 54,033 | 53,035 | 52,498 | 52,462 | 52,274 | 51,950 | 51,612 | 51,465 | 51,233 | 51,338 | 51,136 | 50,690 | 54,359 | 52,159 | 51,172 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nakagawa, Y.; Irisa, K.; Nakagawa, Y.; Kanatani, Y. Hospital Management and Public Health Role of National Hospitals after Transformation into Independent Administrative Agencies. Healthcare 2022, 10, 2084. https://doi.org/10.3390/healthcare10102084
Nakagawa Y, Irisa K, Nakagawa Y, Kanatani Y. Hospital Management and Public Health Role of National Hospitals after Transformation into Independent Administrative Agencies. Healthcare. 2022; 10(10):2084. https://doi.org/10.3390/healthcare10102084
Chicago/Turabian StyleNakagawa, Yoshiaki, Kaoru Irisa, Yoshinobu Nakagawa, and Yasuhiro Kanatani. 2022. "Hospital Management and Public Health Role of National Hospitals after Transformation into Independent Administrative Agencies" Healthcare 10, no. 10: 2084. https://doi.org/10.3390/healthcare10102084
APA StyleNakagawa, Y., Irisa, K., Nakagawa, Y., & Kanatani, Y. (2022). Hospital Management and Public Health Role of National Hospitals after Transformation into Independent Administrative Agencies. Healthcare, 10(10), 2084. https://doi.org/10.3390/healthcare10102084







