Obstructive Giant Inflammatory Polyposis as a First Manifestation of Crohn’s Disease: A Case Report
Abstract
1. Introduction
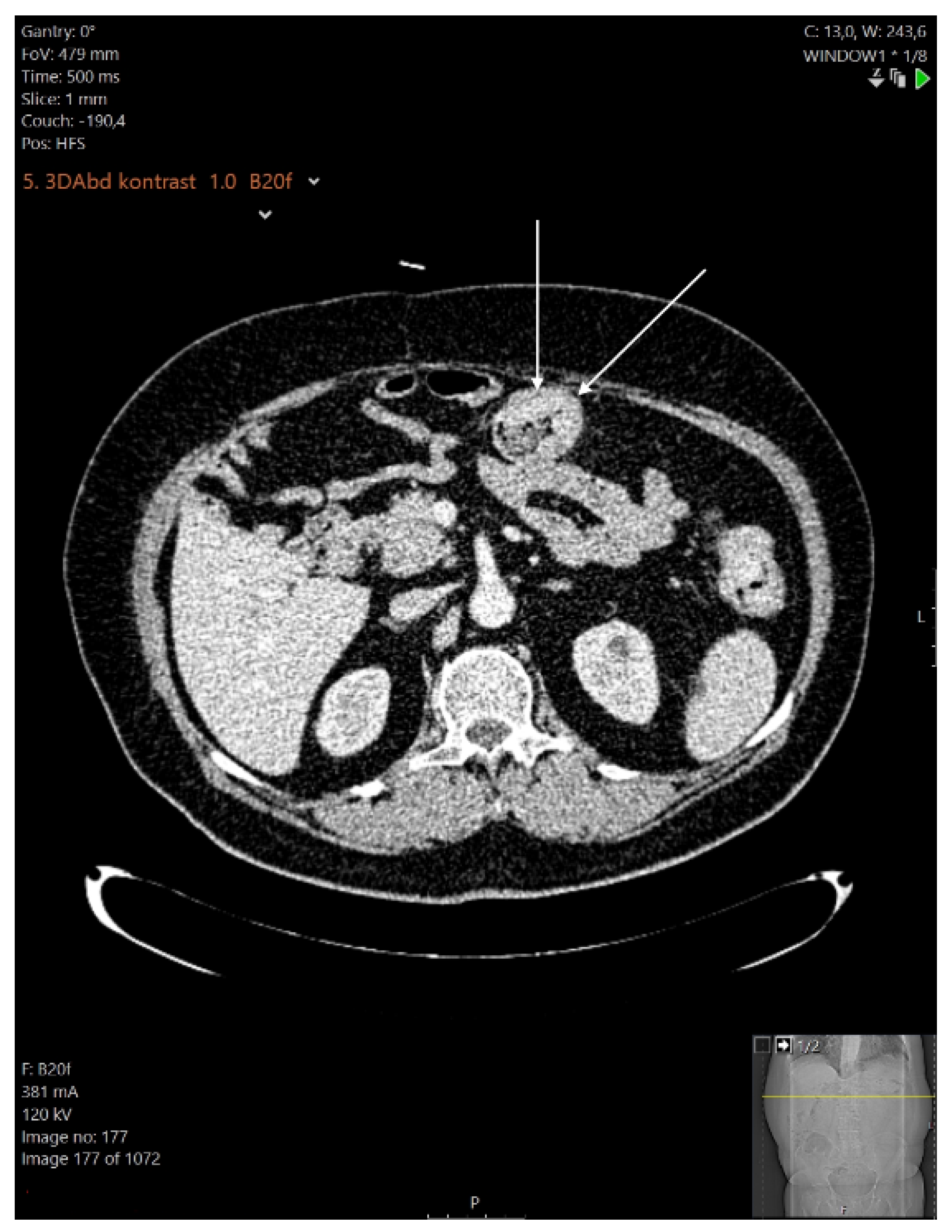
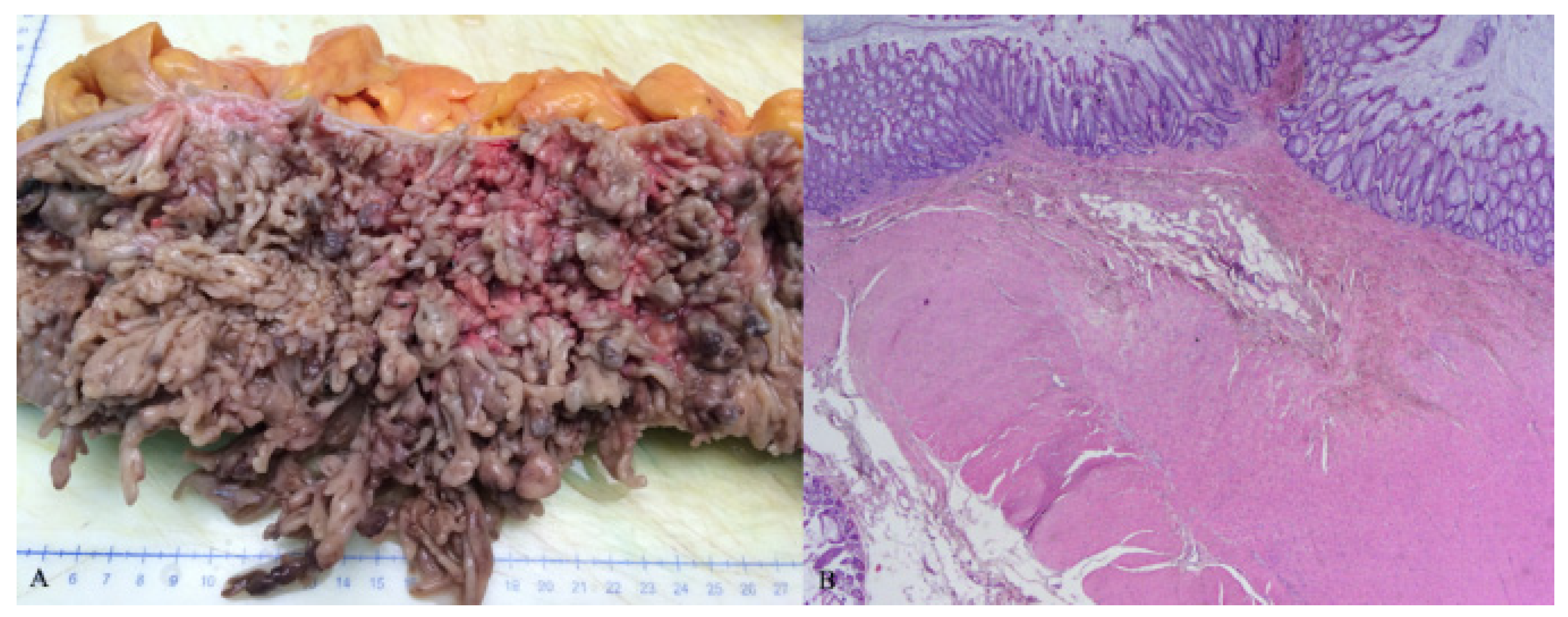
2. Case Report
3. Discussion
3.1. Development of Pseudopolyps
3.2. Clinical Presentation
3.3. Treatment
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Syal, G.; Budhraja, V. Recurrent Obstructive Giant Inflammatory Polyposis of the Colon. ACG Case Rep. J. 2016, 3, 89. [Google Scholar] [CrossRef]
- Choi, Y.S.; Suh, J.P.; Lee, I.T.; Kim, J.K.; Lee, S.H.; Cho, K.R.; Park, H.J.; Kim, D.S.; Lee, D.H. Regression of giant pseudopolyps in inflammatory bowel disease. J. Crohn’s Colitis 2012, 6, 240–243. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Maggs, J.R.L.; Browning, L.C.; Warren, B.F.; Travis, S.P.L. Obstructing giant post-inflammatory polyposis in ulcerative colitis: Case report and review of the literature. J. Crohn’s Colitis 2008, 2, 170–180. [Google Scholar] [CrossRef] [PubMed]
- Romero, C.; Sirsi, S.; Asarian, A.; Levine, J.; Xiao, P. Giant inflammatory polyposis, a phenomenon of inflammatory bowel disease, presenting as acute large bowel obstruction mimicking colonic neoplasm. J. Surg. Case Rep. 2017, 2017, 174. [Google Scholar] [CrossRef][Green Version]
- Goldgraber, M.B. Pseudopolyps in ulcerative colitis. Dis. Colon Rectum 1965, 8, 355–363. [Google Scholar] [CrossRef] [PubMed]
- Hinrichs, H.R.; Goldman, H. Localized giant pseudopolyps of the colon. JAMA 1968, 205, 248–249. [Google Scholar] [CrossRef] [PubMed]
- Lim, Y.J.; Choi, J.H.; Yang, C.H. What is the Clinical Relevance of Filiform Polyposis? Gut Liver 2012, 6, 524–526. [Google Scholar] [CrossRef]
- Shah, S.M.; Rogers, H.L.; Nagai, N. Localized giant pseudopolyposis in Crohn’s disease: Colonoscopic findings. Dis. Colon Rectum 1978, 21, 104–106. [Google Scholar] [CrossRef]
- Kelly, J.K.; Langevin, J.M.; Price, L.M.; Hershfield, N.B.; Share, S.; Blustein, P. Giant and symptomatic inflammatory polyps of the colon in idiopathic inflammatory bowel disease. Am. J. Surg. Pathol. 1986, 10, 420–428. [Google Scholar] [CrossRef]
- Murdaca, G.; Colombo, B.M.; Puppo, F. The role of Th17 lymphocytes in the autoimmune and chronic inflammatory diseases. Intern. Emerg. Med. 2011, 6, 487–495. [Google Scholar] [CrossRef]
- Naymagon, S.; Mikulasovich, M.; Gui, X.; Ullman, T.A.; Harpaz, N. Crohn’s-like clinical and pathological manifestations of giant inflammatory polyposis in IBD: A potential diagnostic pitfall. J. Crohn’s Colitis 2014, 8, 635–640. [Google Scholar] [CrossRef] [PubMed]
- Jalan, K.N.; Walker, R.J.; Sircus, W.; McManus, J.P.; Prescott, R.J.; Card, W.I. Pseudopolyposis in ulcerative colitis. Lancet 1969, 2, 555–559. [Google Scholar] [CrossRef]
- De Dombal, F.T.; Watts, J.M.; Watkinson, G.; Goligher, J.C. Local complications of ulcerative colitis: Stricture, pseudopolyposis, and carcinoma of colon and rectum. BMJ—Brit. Med. J. 1966, 1, 1442–1447. [Google Scholar] [CrossRef] [PubMed]
- Abou Rached, A.; Saba, J.; El Masri, L.; Nakhoul, M.; Razzouk, C. Obstructive Giant Inflammatory Polyposis: Is It Related to the Severity or the Duration of the Inflammatory Bowel Disease? Two Case Reports. Case Rep. Gastrointest. Med. 2018, 2018, 3251549. [Google Scholar] [CrossRef]
- Ooi, B.S.; Tjandra, J.J.; Pedersen, J.S.; Bhathal, P.S. Giant pseudopolyposis in inflammatory bowel disease. Aust. N. Z. J. Surg. 2000, 70, 389–393. [Google Scholar] [CrossRef]
- Yada, S.; Matsumoto, T.; Kudo, T.; Hirahashi, M.; Yao, T.; Mibu, R.; Iida, M. Colonic obstruction due to giant inflammatory polyposis in a patient with ulcerative colitis. J. Gastroenterol. 2005, 40, 536–539. [Google Scholar] [CrossRef]
- Nagashima, M.; Sugishita, Y.; Moriyama, A.; Ooshiro, M.; Kadoya, K.; Sato, A.; Kitahara, T.; Takagi, R.; Urita, T.; Yoshida, Y.; et al. Tumor-like growth of giant inflammatory polyposis in a patient with ulcerative colitis. Case Rep. Gastroenterol. 2013, 7, 352–357. [Google Scholar] [CrossRef]
- Nebbia, M.; Yassin, N.A.; Spinelli, A. Colorectal Cancer in Inflammatory Bowel Disease. Clin. Colon Rectal Surg. 2020, 33, 305–317. [Google Scholar] [CrossRef]
- Kusunoki, M.; Nishigami, T.; Yanagi, H.; Okamoto, T.; Shoji, Y.; Sakanoue, Y.; Yamamura, T.; Utsunomiya, J. Occult cancer in localized giant pseudopolyposis. Am. J. Gastroenterol. 1992, 87, 379–381. [Google Scholar]
- Politis, D.S.; Katsanos, K.H.; Tsianos, E.V.; Christodoulou, D.K. Pseudopolyps in inflammatory bowel diseases: Have we learned enough? World J. Gastroenterol. 2017, 23, 1541–1551. [Google Scholar] [CrossRef]
- Liatsos, C.; Kyriakos, N.; Panagou, E.; Karagiannis, S.; Salemis, N.; Mavrogiannis, C. Inflammatory polypoid mass treated with Infliximab in a Crohn’s disease patient. J. Crohn’s Colitis 2010, 4, 707–708. [Google Scholar] [CrossRef][Green Version]
- Attar, A.; Bon, C.; Sebbagh, V.; Béjou, B.; Bénamouzig, R. Endoscopic argon plasma coagulation for the treatment of hemorrhagic pseudopolyps in colonic Crohn’s disease. Endoscopy 2007, 39, 249. [Google Scholar] [CrossRef][Green Version]
- Forde, K.A.; Green, P.H. Laser ablation of symptomatic rectal pseudopolyps. Gastrointest. Endosc. 1989, 35, 135. [Google Scholar] [CrossRef]
- Rutter, M.; Saunders, B.; Emmanuel, A.; Price, A. Endoscopic snare polypectomy for bleeding postinflammatory polyps. Endoscopy 2003, 35, 788–790. [Google Scholar] [CrossRef] [PubMed]
- Corless, J.K.; Tedesco, F.J.; Griffin, J.W.; Panish, J.K. Giant ileal inflammatory polyps in Crohn’s disease. Gastrointest. Endosc. 1984, 30, 352–354. [Google Scholar] [CrossRef]
- Atten, M.J.; Attar, B.M.; Mahkri, M.A.; Del Pino, A.; Orsay, C.P. Giant pseudopolyps presenting as colocolic intussusception in Crohn’s colitis. Am. J. Gastroenterol. 1998, 93, 1591–1592. [Google Scholar] [CrossRef] [PubMed]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bratanic, A.; Despalatovic, B.R.; Pavic, B.; Bozikovic, T.; Ardalic, Z.; Grubisic, D.A.; Vilovic, K. Obstructive Giant Inflammatory Polyposis as a First Manifestation of Crohn’s Disease: A Case Report. Healthcare 2022, 10, 1995. https://doi.org/10.3390/healthcare10101995
Bratanic A, Despalatovic BR, Pavic B, Bozikovic T, Ardalic Z, Grubisic DA, Vilovic K. Obstructive Giant Inflammatory Polyposis as a First Manifestation of Crohn’s Disease: A Case Report. Healthcare. 2022; 10(10):1995. https://doi.org/10.3390/healthcare10101995
Chicago/Turabian StyleBratanic, Andre, Bruna Rosic Despalatovic, Berna Pavic, Tina Bozikovic, Zarko Ardalic, Danijel Antonio Grubisic, and Katarina Vilovic. 2022. "Obstructive Giant Inflammatory Polyposis as a First Manifestation of Crohn’s Disease: A Case Report" Healthcare 10, no. 10: 1995. https://doi.org/10.3390/healthcare10101995
APA StyleBratanic, A., Despalatovic, B. R., Pavic, B., Bozikovic, T., Ardalic, Z., Grubisic, D. A., & Vilovic, K. (2022). Obstructive Giant Inflammatory Polyposis as a First Manifestation of Crohn’s Disease: A Case Report. Healthcare, 10(10), 1995. https://doi.org/10.3390/healthcare10101995





