Challenges Associated with Effective Implementation of CT Dose Check Standards and Radiation Monitoring Index in Computed Tomography: Healthcare Sector Experience
Abstract
:1. Introduction
2. Materials and Methods
Study Design and Data Collection
3. Results
3.1. Dose Configuration and Features
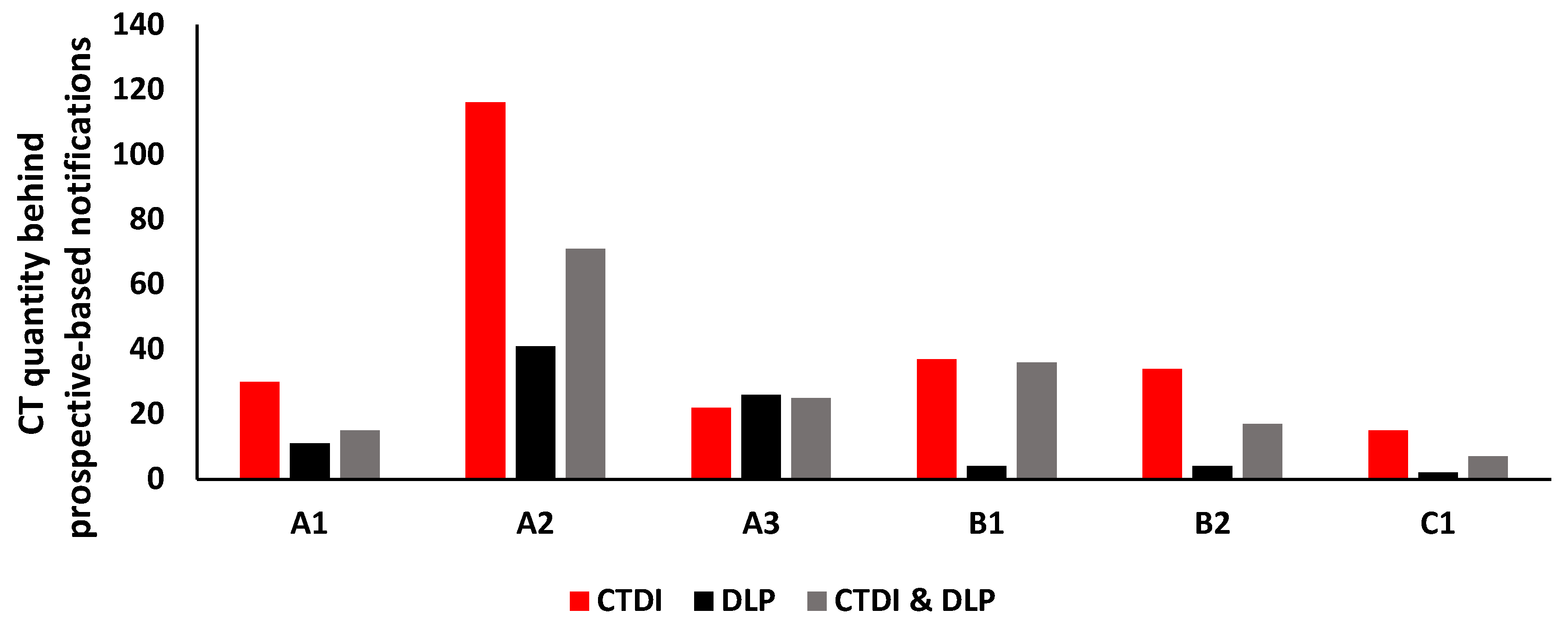
3.2. Dose Notification Counts
3.3. Notification Studies
3.4. Radiographer Justifications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cody, D.; Dillon, C.; Fisher, T.; Liu, X.; McNitt-Gray, M.; Patel, V. AAPM Medical Physics Practice Guideline 1.b: CT protocol management and review practice guideline. J. Appl. Clin. Med. Phys. 2021, 22, 4–10. [Google Scholar] [CrossRef] [PubMed]
- American Association of Physicists in Medicine. AAPM Recommendations Regarding Notification and Alert Values for CT Scanners: Guidelines for Use of the NEMA XR 25 CT Dose-Check Standard. 2011. Available online: http://www.aapm.org/pubs/CTProtocols/documents/NotificationLevelsStatement_2011-04-27.pdf (accessed on 17 July 2022).
- Gress, D.A.; Dickinson, R.L.; Erwin, W.D.; Jordan, D.W.; Kobistek, R.J.; Stevens, D.M.; Supanich, M.P.; Wang, J.; Fairobent, L.A. AAPM medical physics practice guideline 6.a.: Performance characteristics of radiation dose index monitoring systems. J. Appl. Clin. Med. Phys. 2017, 18, 12–22. [Google Scholar] [CrossRef] [PubMed]
- Howard, M.; McCollough, C.; Leng, S.; Yu, L.; Bruesewitz, M. Use of CT Dose Notification and Alert Values in Routine Clinical Practice. J. Am. Coll. Radiol. 2014, 11, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Brill, P.; Hentel, K.; Mahmood, U.; Min, J.; Min, R.; Phillips, C. GE Blueprint A Guide to CT Radiation Dose Management Developed in conjunction with Weill Cornell Imaging at New York–Presbyterian Lower Dose by Design. Weill Cornell Imaging at NewYork-Presbyterian. 2012. Available online: https://services.gehealthcare.sa/ (accessed on 17 July 2022).
- Denison, K. Dose Check Overview. GE Healthcare. 2011. Available online: http://www.gehealthcare.com/LowerDoseByDesign (accessed on 17 July 2022).
- Vano, E.; Fernández, J.; Ten, J.; Sanchez, R. Benefits and limitations for the use of radiation dose management systems in medical imaging. Practical experience in a university hospital. Br. J. Radiol. 2022, 95, 20211340. [Google Scholar] [CrossRef] [PubMed]
- Boone, J.M.; Strauss, K.J.; Cody, D.D.; McCollough, C.H.; McNitt-Gray, M.F.; Toth, T.L. Size-specific dose estimates (SSDE) in pediatric and adult body CT examinations. American Association of Physics in Medicine (AAPM TG-204); American Association of Physicists in Medicine: College Park, MD, USA, 2011. [Google Scholar]
- Crowley, C.; Ekpo, E.U.; Carey, B.W.; Joyce, S.; Kennedy, C.; Grey, T.; Duffy, B.; Kavanagh, R.; James, K.; Moloney, F.; et al. Radiation dose tracking in computed tomography: Red alerts and feedback. Implementing a radiation dose alert system in CT. Radiography 2021, 27, 67–74. [Google Scholar] [CrossRef]
- Dalah, E.Z.; Alsuwaidi, J.S.; Hamed, M.S.; Gani, A.H.A.; Beevi, H.A.A.; Panangatil, A.G.; Funtelar, C.O.; Ferrer, A.Y.; Al Hussein, S.G.A.B.; Albedwawi, S.A. Challenges Experienced in Establishing Clinical Indication Based Diagnostic Reference Levels: Pilot Study. Eur. J. Radiol. 2022, 148, 110046. [Google Scholar] [CrossRef]
- Vañó, E.; Miller, D.L.; Martin, C.J.; Rehani, M.M.; Kang, K.; Rosenstein, M.; Ortiz-López, P.; Mattsson, S.; Padovani, R.; Rogers, A. ICRP Publication 135: Diagnostic Reference Levels in Medical Imaging. Ann. ICRP 2017, 46, 1–144. [Google Scholar] [CrossRef] [PubMed]
- IAEA: SSG-46. Radiation Protection and Safety in Medical Uses of Ionizing Radiation; IAEA: Vienna, Austria, 2018; pp. 1–340. [Google Scholar]
- Lau, L.; Perez, M. Global Initiative on Radiation Safety in Healthcare Settings. In Technical Meeting Report. 15th to 17th December; WHO: Geneva, Switzerland, 2008; pp. 1–100. [Google Scholar]
- Marsha, R.; Silosky, M. The effects of patient positioning when interpreting CT dose metrics: A phantom study. Med. Phys. 2017, 44, 1514–1524. [Google Scholar] [CrossRef] [PubMed]
- Barreto, I.; Lamoureux, R.; Olguin, C.; Quails, N.; Correa, N.; Rill, L.; Arreola, M. Impact of patient centering in CT on organ dose and the effect of using a positioning compensation system: Evidence from OSLD measurements in postmortem subjects. J. Appl. Clin. Med. Phys. 2019, 20, 141–151. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Parakh, A.; Euler, A.; Szucs-Farkas, Z.; Schindera, S. Transatlantic Comparison of CT Radiation Doses in the Era of Radiation Dose–Tracking Software. Am. J. Roentgenol. 2017, 209, 1302–1307. [Google Scholar] [CrossRef]
- Maldjian, P.; Goldman, A. Reducing Radiation Dose in Body CT: A Primer on Dose Metrics and Key CT Technical Parameters. Am. J. Roentgenol. 2013, 200, 741–747. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.; Bhargavan-Chatfield, M.; Armstrong, M.; Butler, P. Clinical Implementation of the National Electrical Manufacturers Association CT Dose Check Standard at ACR Dose Index Registry Sites. J. Am. Coll. Radiol. 2014, 11, 989–994. [Google Scholar] [CrossRef] [PubMed]
- Loose, R.W.; Vano, E.; Mildenberger, P.; Tsapaki, V.; Caramella, D.; Sjöberg, J.; Paulo, G.; Torresin, A.; Schindera, S.; Frija, G.; et al. Radiation dose management systems—requirements and recommendations for users from the ESR EuroSafe Imaging initiative. Eur. Radiol. 2020, 31, 2106–2114. [Google Scholar] [CrossRef] [PubMed]
- NEMA. Computed Tomography Dose Check. 2019. Available online: https://www.nema.org/Standards/view/Computed-Tomography-Dose-Check (accessed on 17 July 2022).
- Mahesh, M. What Is the CT Dose Check Standard, and Why Do CT Scanners Need to Be in Compliance? J. Am. Coll. Radiol. 2016, 13, 64–66. [Google Scholar] [CrossRef] [PubMed]
- Szczykutowicz, T.; Bour, R.; Ranallo, F.; Pozniak, M. The Current State of CT Dose Management Across Radiology: Well Intentioned but Not Universally Well Executed. Am. J. Roentgenol. 2018, 211, 405–408. [Google Scholar] [CrossRef]
- Osman, N.D.; Isa, S.M.; Karim, N.K.; Ismail, N.; Roslee, M.A.; Naharuddin, H.M.; Razali, M.A. Radiation dose management in CT imaging: Initial experience with commercial dose watch software. J. Phys. Conf. Ser. 2020, 1497, 012020. [Google Scholar] [CrossRef]
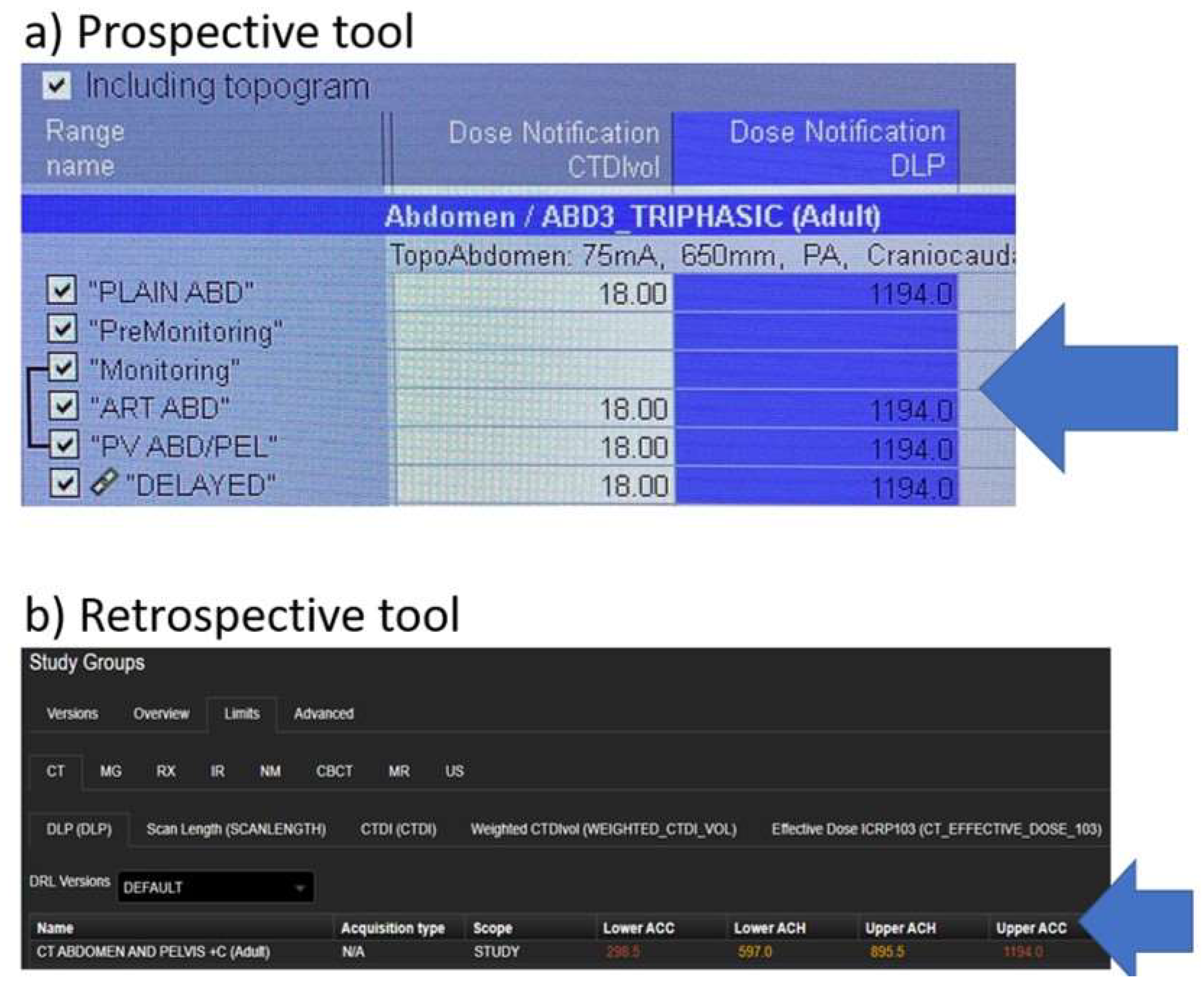


| Feature | CT Console (Prospective) | DOSE TQM (Retrospective) |
|---|---|---|
| NV can be entered for both CT dose quantities, CTDI and DLP | Yes | Yes |
| Dose NV configured per series/phase | Per series/phase | Whole study |
| Different NV values can be used depending on the series or phase | Yes | Yes (e.g., upper ACC/ACH and lower ACC/ACH) but for the whole study |
| Statistical comparison to aid | No | Yes |
| Patients’ accumulative dose history | No | Yes |
| Allows dose alteration/reduction | Yes | No, it’s retrospective |
| Positioning evaluation tool | No, limited scanners | Yes, very effective |
| Credentials needed to override NV alerts | No | No |
| Comparison using the same device, same study description, and even same protocol | No | Yes |
| Common CT Exam | |
|---|---|
| CT Console (Prospective) | DOSE TQM (Retrospective) |
| CT Abdomen/Pelvis + Contrast | CT Polytrauma |
| CT Chest/Abdomen/Pelvis + Contrast | CT Brain Stroke With CTA |
| CT Cardiac Angiogram | CT Abdomen/Pelvis + Contrast |
| CT KUB (Kidney Ureter Bladder) | CT Chest/Abdomen/Pelvis + Contrast |
| CT Chest/CT Chest + Contrast | CT Cardiac Angiogram |
| CT Chest Pulmonary Angiogram | CT KUB (Kidney Ureter Bladder) |
| CT Chest/CT Chest + Contrast | |
| CT High Resolution | |
| Our Institutional Standardized Justifications | Radiographers’ Common Justifications | ||||
|---|---|---|---|---|---|
| CT System Console (Prospective) | DOSE TQM (Retrospective) | ||||
| Actual or Suspected Justification | Justification | Notification Type | Justification | CT System Console (Prospective) | DOSE TQM (Retrospective) |
| Urgent case “No time to write a justification note” | In the diagnosis reason window type 1 | CTDI | Off center > 15 mm; Patient size-obese; Pitch < 1 Hands down; High kV due to (beam hardening, non-typical scan, patient size, pitch, off center, hands down); Combined study | Patient size-obese | Patient size-obese |
| Patient size-obese | Obese patient | DLP | High CTDI; High scan length | High scan length—added delay scan(s) | Off-center |
| Off center | To include ROI (e.g., Knee/Ankle/Foot); External fixator; Difficult positioning (e.g., bulky patient, big abdomen, restless patient, trauma patient, uncooperative patient, etc.); Female patient positioned by male radiographer | High scan length—cover pathology | Blind scan (out of scout) | ||
| High scan length | Due to patient height; To cover pathology; Radiologists request; Add delay scan (s); Repeated scan due to artifact (e.g., breathing, movement), technical error, etc. Combined study | High scan length—combined study | |||
| Alternative positioning | Disoriented patient; Arms in the FOV | Alternative positioning—arms in the FOV | |||
| Non-typical scan | Due to using: Dual energy; 4D-Care Dose Modulation; Pitch adjusted; Combined scan | Beam hardening—metallic implant | |||
| Beam hardening | In case of: Metallic implant; Metallic ornament; External fixator Metallic item in FOV | Repeated—technical error | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dalah, E.Z.; Al Musfari, Y.M.; Ali, B.M.H.; Al Hammadi, A.A.; Beevi, H.A.A.; Jaber, M.I.; Al-Ali, A.A.; Alkharoossi, A.K.; Hashemi, F.H.A.; Alkhatib, F.M.; et al. Challenges Associated with Effective Implementation of CT Dose Check Standards and Radiation Monitoring Index in Computed Tomography: Healthcare Sector Experience. Healthcare 2022, 10, 1970. https://doi.org/10.3390/healthcare10101970
Dalah EZ, Al Musfari YM, Ali BMH, Al Hammadi AA, Beevi HAA, Jaber MI, Al-Ali AA, Alkharoossi AK, Hashemi FHA, Alkhatib FM, et al. Challenges Associated with Effective Implementation of CT Dose Check Standards and Radiation Monitoring Index in Computed Tomography: Healthcare Sector Experience. Healthcare. 2022; 10(10):1970. https://doi.org/10.3390/healthcare10101970
Chicago/Turabian StyleDalah, Entesar Zawam, Yousuf Mohammad Al Musfari, Badriya Mohd Hassan Ali, Anwaar Abdulrahim Al Hammadi, Hashim Abdul Azeez Beevi, Manal Ibrahim Jaber, Alyazya Akeel Al-Ali, Ayesha Khalid Alkharoossi, Fairooz Hussain Al Hashemi, Fatma Mahmood Alkhatib, and et al. 2022. "Challenges Associated with Effective Implementation of CT Dose Check Standards and Radiation Monitoring Index in Computed Tomography: Healthcare Sector Experience" Healthcare 10, no. 10: 1970. https://doi.org/10.3390/healthcare10101970
APA StyleDalah, E. Z., Al Musfari, Y. M., Ali, B. M. H., Al Hammadi, A. A., Beevi, H. A. A., Jaber, M. I., Al-Ali, A. A., Alkharoossi, A. K., Hashemi, F. H. A., Alkhatib, F. M., & Khan, S. A. A. (2022). Challenges Associated with Effective Implementation of CT Dose Check Standards and Radiation Monitoring Index in Computed Tomography: Healthcare Sector Experience. Healthcare, 10(10), 1970. https://doi.org/10.3390/healthcare10101970





