The Increased Mortality Rate with Lower Incidence of Traumatic Brain Injury during the COVID-19 Pandemic: A National Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Background
2.2. Study Design
2.3. Participants
2.4. Outcome Measures
2.5. Statistical Analysis
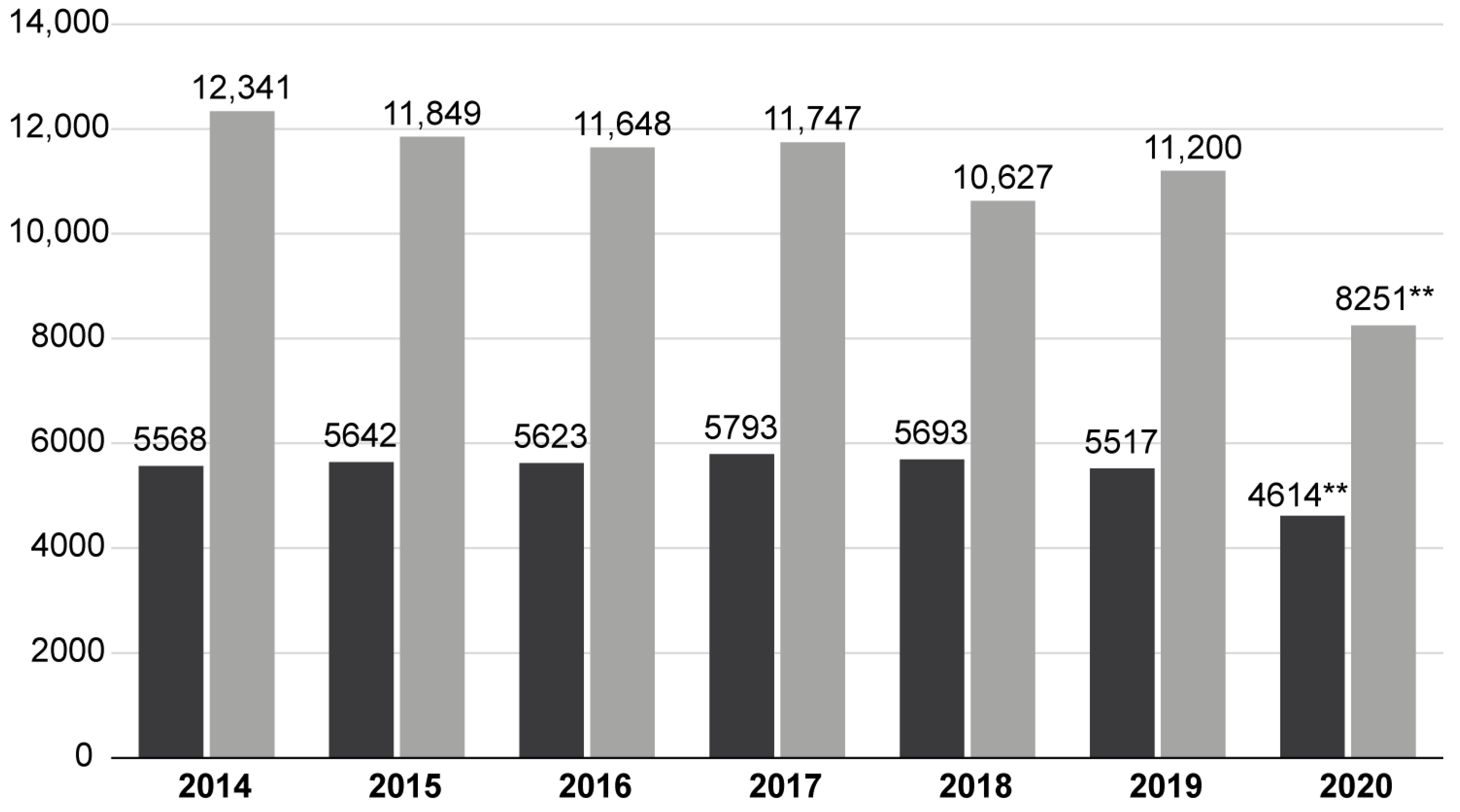
3. Results
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Brooks, J.C.; Strauss, D.J.; Shavelle, R.M.; Paculdo, D.R.; Hammond, F.M.; Harrison-Felix, C.L. Long-Term Disability and Survival in Traumatic Brain Injury: Results from the National Institute on Disability and Rehabilitation Research Model Systems. Arch. Phys. Med. Rehabil. 2013, 94, 2203–2209. [Google Scholar] [CrossRef] [PubMed]
- Alkhaibary, A.; Alshalawi, A.; Althaqafi, R.M.; Alghuraybi, A.A.; Basalamah, A.; Shammaa, A.M.; Altalhy, A.A.; Abdelrahman, T.M. Traumatic Brain Injury: A Perspective on the Silent Epidemic. Cureus 2021, 13, e15318. [Google Scholar] [CrossRef]
- Dewan, M.C.; Rattani, A.; Gupta, S.; Baticulon, R.E.; Hung, Y.C.; Punchak, M.; Agrawal, A.; Adeleye, A.O.; Shrime, M.G.; Rubiano, A.M.; et al. Estimating the Global Incidence of Traumatic Brain Injury. J. Neurosurg. 2019, 130, 1080–1097. [Google Scholar] [CrossRef] [PubMed]
- Iaccarino, C.; Carretta, A.; Nicolosi, F.; Morselli, C. Epidemiology of Severe Traumatic Brain Injury. J Neurosurg. Sci. 2018, 62, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Chuck, C.C.; Martin, T.J.; Kalagara, R.; Shaaya, E.; Kheirbek, T.; Cielo, D. Emergency Medical Services Protocols for Traumatic Brain Injury in the United States: A Call for Standardization. Injury 2021, 52, 1145–1150. [Google Scholar] [CrossRef]
- Jean, W.C.; Ironside, N.T.; Sack, K.D.; Felbaum, D.R.; Syed, H.R. The Impact of COVID-19 on Neurosurgeons and the Strategy for Triaging Non-Emergent Operations: A Global Neurosurgery Study. Acta. Neurochir. 2020, 162, 1229–1240. [Google Scholar] [CrossRef]
- Chang, D.; Xu, H.; Rebaza, A.; Sharma, L.; dela Cruz, C.S. Protecting Health-Care Workers from Subclinical Coronavirus Infection. Lancet Respir. Med. 2020, 8, e13. [Google Scholar] [CrossRef]
- COVID-19: Recommendations for Management of Elective Surgical Procedures|ACS. Available online: https://www.facs.org/for-medical-professionals/covid-19/clinical-guidance/elective-surgery/ (accessed on 20 September 2022).
- Rault, F.; Terrier, L.; Leclerc, A.; Gilard, V.; Emery, E.; Derrey, S.; Briant, A.R.; Gakuba, C.; Gaberel, T. Decreased Number of Deaths Related to Severe Traumatic Brain Injury in Intensive Care Unit during the First Lockdown in Normandy: At Least One Positive Side Effect of the COVID-19 Pandemic. Acta. Neurochir. 2021, 163, 1829–1836. [Google Scholar] [CrossRef]
- Damara, F.A.; Muchamad, G.R.; Anton, A.; Ramdhani, A.N.; Channel, I.C.; Faried, A. Epidemiological Pattern of Traumatic Brain Injury in the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. World Neurosurg. 2022, 161, e698. [Google Scholar] [CrossRef]
- Główny Urząd Statystyczny/Obszary Tematyczne/Ludność/Ludność/Rezydenci (Ludność Rezydująca). Available online: https://stat.gov.pl/obszary-tematyczne/ludnosc/ludnosc/ludnosc-stan-i-struktura-ludnosci-oraz-ruch-naturalny-w-przekroju-terytorialnym-stan-w-dniu-30-06-2021,6,30.html (accessed on 21 September 2022).
- WDI—The World by Income and Region. Available online: https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html (accessed on 21 September 2022).
- Narodowy Fundusz Zdrowia Statystyka NFZ. Available online: https://statystyki.nfz.gov.pl/ (accessed on 31 August 2021).
- Lowry, R. Significance of the Difference Between Two Independent Proportions. Available online: http://vassarstats.net/propdiff_ind.html (accessed on 21 September 2022).
- Julious, S.A. Two-Sided Confidence Intervals for the Single Proportion: Comparison of Seven Methods. Stat. Med. 2005, 24, 3383–3384. [Google Scholar] [CrossRef] [PubMed]
- MZ Raport Zakażeń Koronawirusem (SARS-CoV-2)–Koronawirus: Informacje i Zalecenia-Portal Gov.Pl. Available online: https://www.gov.pl/web/koronawirus/wykaz-zarazen-koronawirusem-sars-cov-2 (accessed on 31 August 2021).
- Berg, G.M.; Wyse, R.J.; Morse, J.L.; Chipko, J.; Garland, J.M.; Slivinski, A.; Lieser, M.; Biswas, S.; Carrick, M.M.; Rhodes, H.; et al. Decreased Adult Trauma Admission Volumes and Changing Injury Patterns during the COVID-19 Pandemic at 85 Trauma Centers in a Multistate Healthcare System. Trauma. Surg. Acute. Care. Open 2021, 6, e000642. [Google Scholar] [CrossRef] [PubMed]
- Pinggera, D.; Klein, B.; Thomé, C.; Grassner, L. The Influence of the COVID-19 Pandemic on Traumatic Brain Injuries in Tyrol: Experiences from a State under Lockdown. Eur. J. Trauma Emerg. Surg. 2020, 47, 653–658. [Google Scholar] [CrossRef]
- Luostarinen, T.; Virta, J.; Satopää, J.; Bäcklund, M.; Kivisaari, R.; Korja, M.; Raj, R. Intensive Care of Traumatic Brain Injury and Aneurysmal Subarachnoid Hemorrhage in Helsinki during the Covid-19 Pandemic. Acta Neurochir. 2020, 162, 2715–2724. [Google Scholar] [CrossRef] [PubMed]
- Figueroa, J.M.; Boddu, J.; Kader, M.; Berry, K.; Kumar, V.; Ayala, V.; Vanni, S.; Jagid, J. The Effects of Lockdown During the Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Pandemic on Neurotrauma-Related Hospital Admissions. World Neurosurg. 2021, 146, e1. [Google Scholar] [CrossRef] [PubMed]
- Ozoner, B.; Gungor, A.; Hasanov, T.; Toktas, Z.O.; Kilic, T. Neurosurgical Practice During Coronavirus Disease 2019 (COVID-19) Pandemic. World Neurosurg. 2020, 140, 198. [Google Scholar] [CrossRef] [PubMed]
- Katrakazas, C.; Michelaraki, E.; Sekadakis, M.; Yannis, G. A Descriptive Analysis of the Effect of the COVID-19 Pandemic on Driving Behavior and Road Safety. Transp. Res. Interdiscip. Perspect. 2020, 7, 100186. [Google Scholar] [CrossRef] [PubMed]
- Grassner, L.; Petr, O.; Warner, F.M.; Dedeciusova, M.; Mathis, A.M.; Pinggera, D.; Gsellmann, S.; Meiners, L.C.; Freigang, S.; Mokry, M.; et al. Trends and Outcomes for Non-Elective Neurosurgical Procedures in Central Europe during the COVID-19 Pandemic. Sci. Rep. 2021, 11, 6171. [Google Scholar] [CrossRef] [PubMed]
- Miekisiak, G.; Czyz, M.; Tykocki, T.; Kaczmarczyk, J.; Zaluski, R.; Latka, D. Traumatic Brain Injury in Poland from 2009-2012: A National Study on Incidence. Brain Inj. 2015, 30, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.A.; Eaton, A.; Tignanelli, C.J.; Carrabre, K.J.; Gerges, C.; Yang, G.L.; Hemmila, M.R.; Ngwenya, L.B.; Wright, J.M.; Parr, A.M.; et al. Changes in Patterns of Traumatic Brain Injury in the Michigan Trauma Quality Improvement Program Database Early in the COVID-19 Pandemic. J. Neurosurg. 2022, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Miękisiak, G.; Pettersson, S.D.; Szarek, D.; Morasiewicz, P.; Fercho, J.; Adamski, S.; Kipiński, L.; Szmuda, T. Acute Stroke Care during COVID-19: National Data. Infect. Dis. Rep. 2022, 14, 198. [Google Scholar] [CrossRef] [PubMed]
- Meza, H.T.; Lambea Gil, Á.; Saldaña, A.S.; Martínez-Zabaleta, M.; Juez, P.; Juez, P.d.l.R.; Martínez, E.L.C.; Apilánez, M.C.; Isasi, M.H.; Enguita, J.M. Impact of COVID-19 Outbreak on Ischemic Stroke Admissions and in-Hospital Mortality in North-West Spain. Int. J. Stroke 2020, 15, 755–762. [Google Scholar] [CrossRef] [PubMed]
- Nioi, M.; Napoli, P.E.; Finco, G.; Demontis, R.; Fossarello, M.; D’aloja, E. Fear of the Covid-19 and Medical Liability. Insights from a Series of 130 Consecutives Medico-Legal Claims Evaluated in a Single Institution during Sars-Cov-2-Related Pandemic. Signa Vitae 2021, 17, 79–85. [Google Scholar] [CrossRef]
- Waseem, S.; Nayar, S.K.; Hull, P.; Carrothers, A.; Rawal, J.; Chou, D.; Khanduja, V. The Global Burden of Trauma during the COVID-19 Pandemic: A Scoping Review. J. Clin. Orthop. Trauma 2021, 12, 200–207. [Google Scholar] [CrossRef]
- Raitio, A.; Ahonen, M.; Jääskelä, M.; Jalkanen, J.; Luoto, T.T.; Haara, M.; Nietosvaara, Y.; Salonen, A.; Pakkasjärvi, N.; Laaksonen, T.; et al. Reduced Number of Pediatric Orthopedic Trauma Requiring Operative Treatment during COVID-19 Restrictions: A Nationwide Cohort Study. Scand. J. Surg. 2020, 110, 254–257. [Google Scholar] [CrossRef]
- Peeters, W.; van den Brande, R.; Polinder, S.; Brazinova, A.; Steyerberg, E.W.; Lingsma, H.F.; Maas, A.I.R. Epidemiology of Traumatic Brain Injury in Europe. Acta Neurochir. 2015, 157, 1683–1696. [Google Scholar] [CrossRef]
- Kirkman, M.A.; Jenks, T.; Bouamra, O.; Edwards, A.; Yates, D.; Wilson, M.H. Increased Mortality Associated with Cerebral Contusions Following Trauma in the Elderly: Bad Patients or Bad Management? J. Neurotrauma 2013, 30, 1385–1390. [Google Scholar] [CrossRef]
- Lara-Reyna, J.; Yaeger, K.A.; Rossitto, C.P.; Camara, D.; Wedderburn, R.; Ghatan, S.; Bederson, J.B.; Margetis, K. “Staying Home”—Early Changes in Patterns of Neurotrauma in New York City During the COVID-19 Pandemic. World Neurosurg. 2020, 143, e344–e350. [Google Scholar] [CrossRef]
- Petr, O.; Grassner, L.; Warner, F.M.; Dedeciusová, M.; Voldřich, R.; Geiger, P.; Brawanski, K.; Gsellmann, S.; Meiners, L.C.; Bauer, R.; et al. Current Trends and Outcomes of Non-Elective Neurosurgical Care in Central Europe during the Second Year of the COVID-19 Pandemic. Sci. Rep. 2022, 12, 14631. [Google Scholar] [CrossRef]
- American College of Surgeons ACS Statement on the Importance of Maintaining the Emergency Care System during the COVID-19 Pandemic. Available online: https://www.facs.org/covid-19/clinical-guidance/statement-maintaining (accessed on 1 September 2021).
- Karthigeyan, M.; Dhandapani, S.; Salunke, P.; Sahoo, S.K.; Kataria, M.S.; Singh, A.; Gendle, C.; Panchal, C.; Chhabra, R.; Jain, K.; et al. The Collateral Fallout of COVID19 Lockdown on Patients with Head Injury from North-West India. Acta Neurochir. 2021, 163, 1053–1060. [Google Scholar] [CrossRef]
- Goyal, N.; Swain, S.K.; Gupta, K.; Chaturvedi, J.; Arora, R.K.; Sharma, S.K. “Locked up inside Home” - Head Injury Patterns during Coronavirus Disease of 2019 Pandemic. Surg. Neurol. Int. 2020, 11, 395. [Google Scholar] [CrossRef] [PubMed]
- Hecht, N.; Wessels, L.; Werft, F.O.; Schneider, U.C.; Czabanka, M.; Vajkoczy, P. Need for Ensuring Care for Neuro-Emergencies-Lessons Learned from the COVID-19 Pandemic. Acta Neurochir. 2020, 162, 1795–1801. [Google Scholar] [CrossRef] [PubMed]
- Horan, J.; Duddy, J.C.; Gilmartin, B.; Amoo, M.; Nolan, D.; Corr, P.; Husien, M.B.; Bolger, C. The Impact of COVID-19 on Trauma Referrals to a National Neurosurgical Centre. Ir. J. Med. Sci. 2021, 190, 1281–1293. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Creteur, J. Ethical Aspects of the COVID-19 Crisis: How to Deal with an Overwhelming Shortage of Acute Beds. Eur. Heart J. Acute. Cardiovasc. Care 2020, 9, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Manivannan, S.; Sharouf, F.; Mayo, I.; Albaqer, H.; Mehrez, M.; Jaber, H.; Nicholls, Z.; Woodward, B.O.; Watkins, W.J.; Zaben, M. Management of Neurotrauma during COVID-19: A Single Centre Experience and Lessons for the Future. Brain Inj. 2021, 35, 957–963. [Google Scholar] [CrossRef] [PubMed]
- Karlinsky, A.; Kobak, D. Tracking Excess Mortality across Countries during the Covid-19 Pandemic with the World Mortality Dataset. Elife 2021, 10, e69336. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Xu, S.; Yu, M.; Wang, K.; Tao, Y.; Zhou, Y.; Shi, J.; Zhou, M.; Wu, B.; Yang, Z.; et al. Risk Factors for Severity and Mortality in Adult COVID-19 Inpatients in Wuhan. J. Allergy Clin. Immunol. 2020, 146, 110–118. [Google Scholar] [CrossRef]
| Diagnosis | ICD 10 | Surgical | Conservative | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2020 | 2014–2019 | 2020 | 2014–2019 | ||||||
| n | % | n | % | n | % | n | % | ||
| Diffuse brain injury | S06.2 | 143 | 3.11 | 1109 | 3.28 | 0 | 0 | 0 | 0 |
| Focal brain injury | S06.3 | 87 | 1.89 * | 837 | 2.47 * | 1511 | 18.31 * | 11,897 | 17.36 * |
| Epidural haemorrhage | S06.4 | 443 | 9.64 * | 3643 | 10.77 * | 257 | 3.11 | 2093 | 3.05 |
| Traumatic subdural haemorrhage | S06.5 | 3639 | 79.16 ** | 26.113 | 77.17 ** | 1610 | 19.51 ** | 10,241 | 14.95 ** |
| Traumatic subarahnoid hemorrhage | S06.6 | 0 | 0 | 0 | 0 | 685 | 8.3 ** | 4011 | 5.85 ** |
| Cranial vault fracture | S02.0 | 0 | 0 | 0 | 0 | 1464 | 17.74 ** | 7667 | 11.19 ** |
| Skull base fracture | S02.1 | 0 | 0 | 0 | 0 | 271 | 3.28 ** | 3181 | 4.64 ** |
| Complex cranial fracture | S02.7 | 0 | 0 | 0 | 0 | 374 | 4.53 * | 3535 | 5.16 * |
| Other | - | 285 | 6.2 | 2136 | 6.31 | 2079 | 25.2 ** | 25,889 | 37.79 ** |
| total | 4597 | 100 | 33,838 | 100 | 8251 | 100 | 68,514 | 100 | |
| Surgical Procedure | 2020 | 2014–2019 | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Burr hole | 01.243 01.092 | 1728 | 34.26 | 12,222 | 34.15 |
| Craniotomy for epidural hematoma | 01.245 | 545 | 10.8 | 4115 | 11.5 |
| Craniotomy for subdural hematoma | 01.247 | 2510 | 49.76 | 17,771 | 49.66 |
| Other | - | 261 | 5.17 | 1677 | 4.69 |
| total | 5044 | 100 | 35,785 | 100 | |
| Age Category | Surgical | Conservative | ||||||
|---|---|---|---|---|---|---|---|---|
| 2020 | 2014–2019 | 2020 | 2014–2019 | |||||
| n | % | n | % | n | % | n | % | |
| under 18 | 84 | 1.83 | 729 | 2.15 | 1044 | 12.65 ** | 11,736 | 17.13 ** |
| 18–40 | 582 | 12.66 | 4640 | 13.71 | 1643 | 19.91 ** | 16,128 | 23.54 ** |
| 41–60 | 1255 | 27.3 | 9218 | 27.25 | 2148 | 26.03 * | 17,036 | 24.86 * |
| 61–80 | 1808 | 39.33 * | 12.811 | 37.87 * | 2252 | 27.29 ** | 16,073 | 23.46 ** |
| 80+ | 868 | 18.88 | 6435 | 19.02 | 1164 | 14.11 ** | 7541 | 11.01 ** |
| total | 4597 | 100 | 33,833 | 100 | 8251 | 100 | 68,514 | 100 |
| Surgical | Conservative | All | ||||
|---|---|---|---|---|---|---|
| 2020 | 2014–2019 | 2020 | 2014–2019 | 2020 | 2014–2019 | |
| N of deaths | 1196 | 7675 | 560 | 3361 | 1756 | 11,036 |
| Deaths per annum | 1196 | 1279.17 | 560 | 560.17 | 1756 | 1839.34 |
| N of hospitalizations | 4597 | 33,833 | 8251 | 68,514 | 12,848 | 102,347 |
| Mortality rate (CI95%) [%] | 26.02 (24.77–27.31) ** | 22.68 (22.24–23.13) ** | 6.79 (6.27–7.35) ** | 4.91 (4.75–5.07) ** | 13.68 (13.09–14.27) ** | 10.78 (10.59–10.97) ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miękisiak, G.; Szarek, D.; Pettersson, S.D.; Pezowicz, C.; Morasiewicz, P.; Kubaszewski, Ł.; Szmuda, T. The Increased Mortality Rate with Lower Incidence of Traumatic Brain Injury during the COVID-19 Pandemic: A National Study. Healthcare 2022, 10, 1954. https://doi.org/10.3390/healthcare10101954
Miękisiak G, Szarek D, Pettersson SD, Pezowicz C, Morasiewicz P, Kubaszewski Ł, Szmuda T. The Increased Mortality Rate with Lower Incidence of Traumatic Brain Injury during the COVID-19 Pandemic: A National Study. Healthcare. 2022; 10(10):1954. https://doi.org/10.3390/healthcare10101954
Chicago/Turabian StyleMiękisiak, Grzegorz, Dariusz Szarek, Samuel D. Pettersson, Celina Pezowicz, Piotr Morasiewicz, Łukasz Kubaszewski, and Tomasz Szmuda. 2022. "The Increased Mortality Rate with Lower Incidence of Traumatic Brain Injury during the COVID-19 Pandemic: A National Study" Healthcare 10, no. 10: 1954. https://doi.org/10.3390/healthcare10101954
APA StyleMiękisiak, G., Szarek, D., Pettersson, S. D., Pezowicz, C., Morasiewicz, P., Kubaszewski, Ł., & Szmuda, T. (2022). The Increased Mortality Rate with Lower Incidence of Traumatic Brain Injury during the COVID-19 Pandemic: A National Study. Healthcare, 10(10), 1954. https://doi.org/10.3390/healthcare10101954












