Relationship between Eccentric-Exercise-Induced Loss in Muscle Function to Muscle Soreness and Tissue Hardness
Abstract
:1. Introduction
2. Materials and Methods
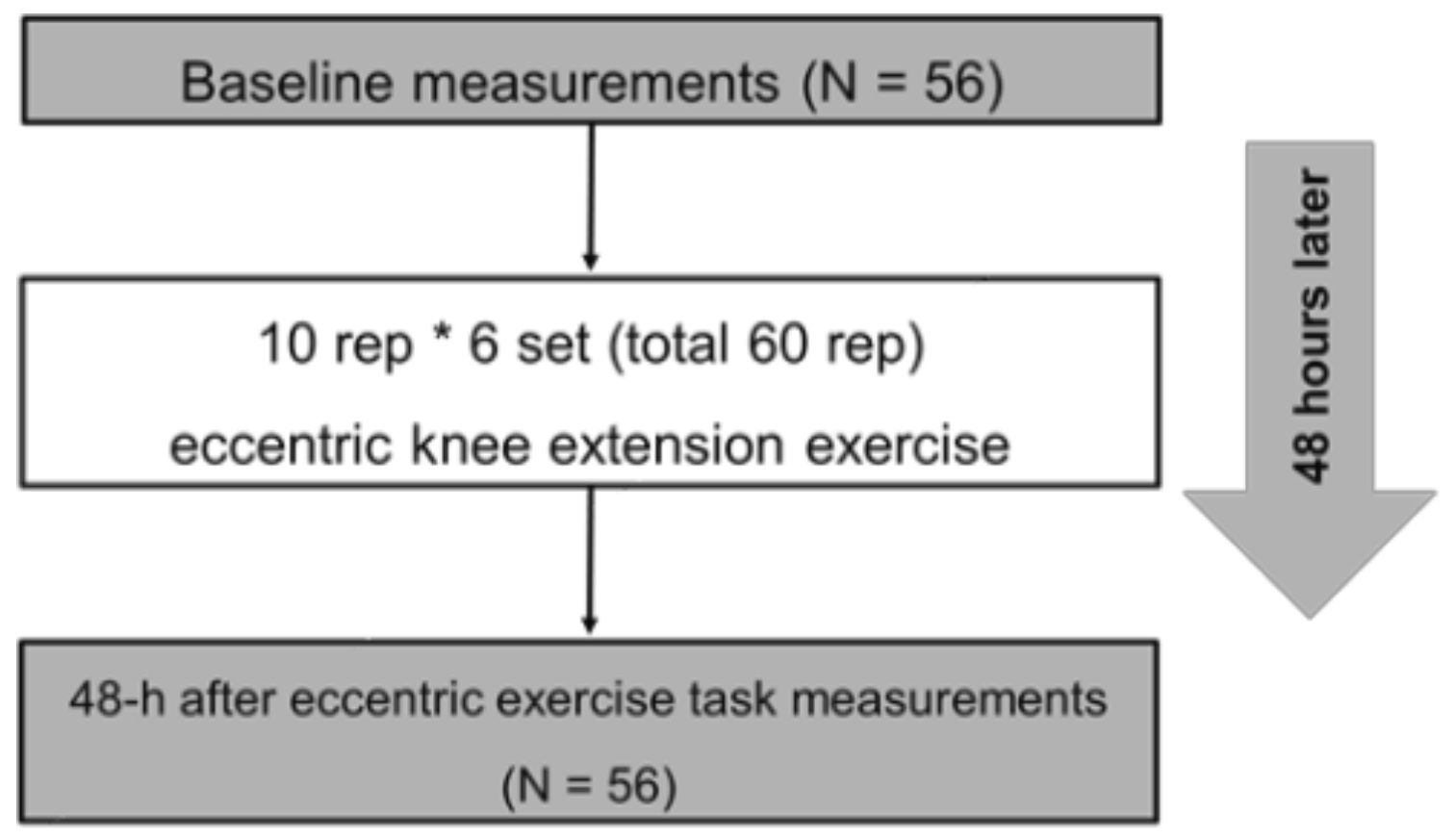
2.1. Experimental Design
2.2. Participants
2.3. Procedures
2.3.1. MVC-ISO and MVC-CON
2.3.2. Knee Flexion ROM
2.3.3. Muscle Soreness
2.3.4. PPT
2.3.5. Tissue Hardness
2.3.6. ECC Exercise Task
2.4. Test–Retest Reliability of the Measurements
2.5. Statistical Analysis
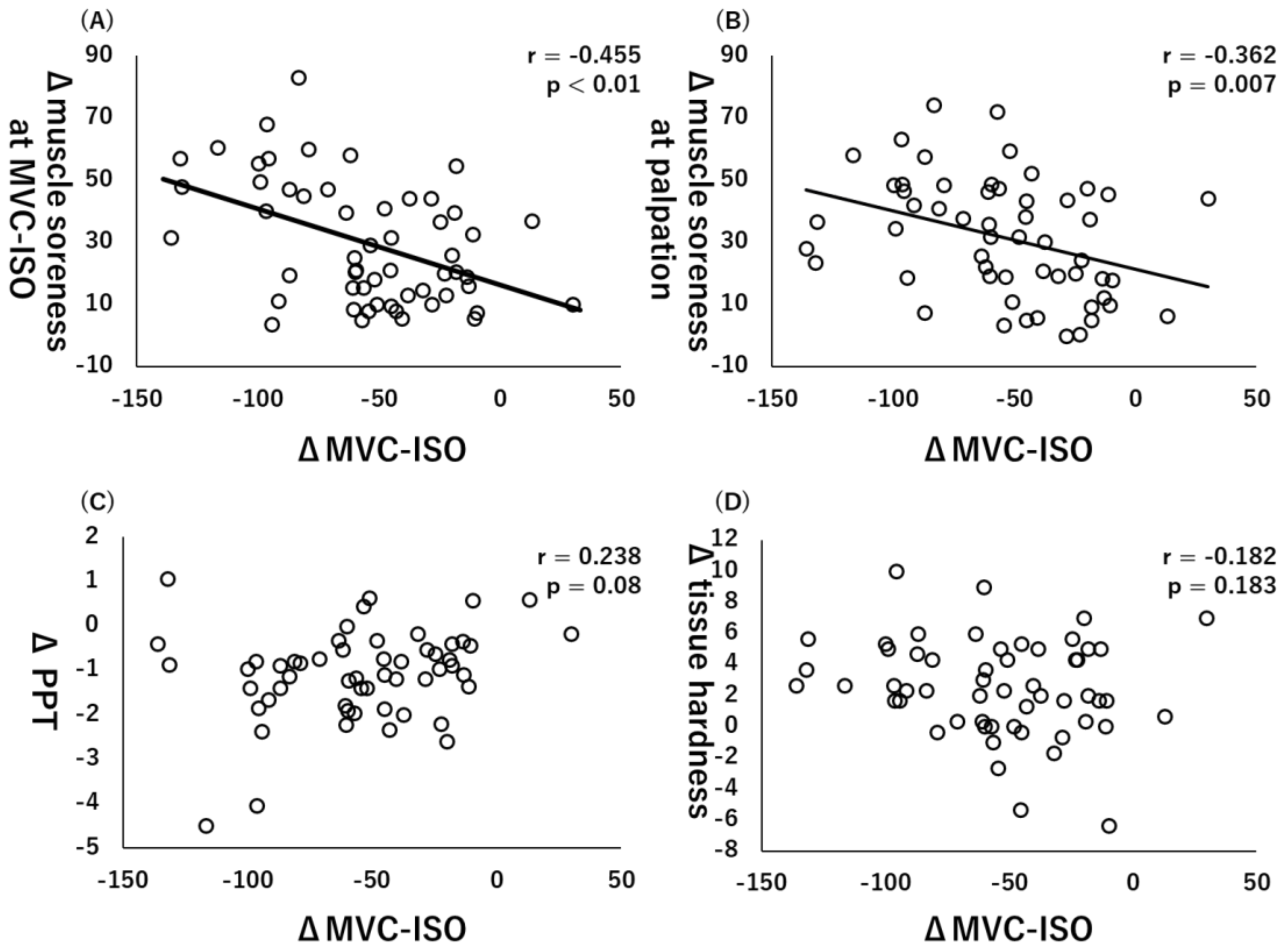
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Peake, J.M.; Neubauer, O.; Della Gatta, P.A.; Nosaka, K. Muscle damage and inflammation during recovery from exercise. J. Appl. Physiol. 2017, 122, 559–570. [Google Scholar] [CrossRef]
- Hyldahl, R.D.; Hubal, M.J. Lengthening our perspective: Morphological, cellular, and molecular responses to eccentric exercise. Muscle Nerve 2014, 49, 155–170. [Google Scholar] [CrossRef]
- Tseng, W.C.; Nosaka, K.; Tseng, K.W.; Chou, T.Y.; Chen, T.C. Contralateral Effects by Unilateral Eccentric versus Concentric Resistance Training. Med. Sci. Sports Exerc. 2020, 52, 474–483. [Google Scholar] [CrossRef] [Green Version]
- Chen, T.C.; Tseng, W.C.; Huang, G.L.; Chen, H.L.; Tseng, K.W.; Nosaka, K. Superior Effects of Eccentric to Concentric Knee Extensor Resistance Training on Physical Fitness, Insulin Sensitivity and Lipid Profiles of Elderly Men. Front. Physiol. 2017, 8, 209. [Google Scholar] [CrossRef] [Green Version]
- Sato, S.; Yoshida, R.; Kiyono, R.; Yahata, K.; Yasaka, K.; Nosaka, K.; Nakamura, M. Cross-education and detraining effects of eccentric vs. concentric resistance training of the elbow flexors. BMC Sports Sci. Med. Rehabil. 2021, 13, 105. [Google Scholar] [CrossRef]
- Nosaka, K.; Chapman, D.; Newton, M.; Sacco, P. Is isometric strength loss immediately after eccentric exercise related to changes in indirect markers of muscle damage? Appl. Physiol. Nutr. Metab. 2006, 31, 313–319. [Google Scholar] [CrossRef]
- Damas, F.; Nosaka, K.; Libardi, C.A.; Chen, T.C.; Ugrinowitsch, C. Susceptibility to Exercise-Induced Muscle Damage: A Cluster Analysis with a Large Sample. Int. J. Sports Med. 2016, 37, 633–640. [Google Scholar] [CrossRef]
- Peñailillo, L.; Blazevich, A.; Numazawa, H.; Nosaka, K. Rate of force development as a measure of muscle damage. Scand. J. Med. Sci. Sports 2015, 25, 417–427. [Google Scholar] [CrossRef]
- Brusco, C.M.; Radaelli, R.; Neske, R.; Peñailillo, L.E.; Pinto, R.S. Rate of torque development as an indirect marker of muscle damage in the knee flexors. Sport Sci. Health 2021, 1–9. [Google Scholar] [CrossRef]
- Fujita, K.; Nakamura, M.; Umegaki, H.; Kobayashi, T.; Nishishita, S.; Tanaka, H.; Ibuki, S.; Ichihashi, N. Effects of a Thermal Agent and Physical Activity on Muscle Tendon Stiffness, as Well as the Effects Combined With Static Stretching. J. Sport Rehabil. 2018, 27, 66–72. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, M.; Yasaka, K.; Kiyono, R.; Onuma, R.; Yahata, K.; Sato, S.; Konrad, A. The Acute Effect of Foam Rolling on Eccentrically-Induced Muscle Damage. Int. J. Environ. Res. Public Health 2020, 18, 75. [Google Scholar] [CrossRef]
- Nakamura, M.; Konrad, A.; Kiyono, R.; Sato, S.; Yahata, K.; Yoshida, R.; Yasaka, K.; Murakami, Y.; Sanuki, F.; Wilke, J. Local and Non-local Effects of Foam Rolling on Passive Soft Tissue Properties and Spinal Excitability. Front. Physiol. 2021, 12, 702042. [Google Scholar] [CrossRef]
- Nakamura, M.; Sato, S.; Kiyono, R.; Yoshida, R.; Yasaka, K.; Yahata, K.; Konrad, A. Comparison Between Foam Rolling With and Without Vibration on Passive and Active Plantar Flexor Muscle Properties. J. Strength Cond. Res. 2021. [Google Scholar] [CrossRef]
- Nakamura, M.; Ikezoe, T.; Kobayashi, T.; Umegaki, H.; Takeno, Y.; Nishishita, S.; Ichihashi, N. Acute effects of static stretching on muscle hardness of the medial gastrocnemius muscle belly in humans: An ultrasonic shear-wave elastography study. Ultrasound Med. Biol. 2014, 40, 1991–1997. [Google Scholar] [CrossRef]
- Chen, T.C.; Chen, H.L.; Lin, M.J.; Wu, C.J.; Nosaka, K. Potent protective effect conferred by four bouts of low-intensity eccentric exercise. Med. Sci. Sports Exerc. 2010, 42, 1004–1012. [Google Scholar] [CrossRef] [Green Version]
- Mavropalias, G.; Koeda, T.; Barley, O.R.; Poon, W.C.K.; Fisher, A.J.; Blazevich, A.J.; Nosaka, K. Comparison between high- and low-intensity eccentric cycling of equal mechanical work for muscle damage and the repeated bout effect. Eur. J. Appl. Physiol. 2020, 120, 1015–1025. [Google Scholar] [CrossRef]
- Kim, S.J.; Lee, J.H. Effects of sternocleidomastoid muscle and suboccipital muscle soft tissue release on muscle hardness and pressure pain of the sternocleidomastoid muscle and upper trapezius muscle in smartphone users with latent trigger points. Medicine 2018, 97, e12133. [Google Scholar] [CrossRef]
- Naderi, A.; Rezvani, M.H.; Degens, H. Foam Rolling and Muscle and Joint Proprioception After Exercise-Induced Muscle Damage. J. Athl. Train. 2020, 55, 58–64. [Google Scholar] [CrossRef]
- Magnusson, S.P.; Simonsen, E.B.; Aagaard, P.; Boesen, J.; Johannsen, F.; Kjaer, M. Determinants of musculoskeletal flexibility: Viscoelastic properties, cross-sectional area, EMG and stretch tolerance. Scand. J. Med. Sci. Sports 1997, 7, 195–202. [Google Scholar] [CrossRef]
- Weppler, C.H.; Magnusson, S.P. Increasing muscle extensibility: A matter of increasing length or modifying sensation? Phys. Ther. 2010, 90, 438–449. [Google Scholar] [CrossRef]
- Miyamoto, N.; Hirata, K.; Miyamoto-Mikami, E.; Yasuda, O.; Kanehisa, H. Associations of passive muscle stiffness, muscle stretch tolerance, and muscle slack angle with range of motion: Individual and sex differences. Sci. Rep. 2018, 8, 8274. [Google Scholar] [CrossRef]
- Hirata, K.; Yamadera, R.; Akagi, R. Associations between Range of Motion and Tissue Stiffness in Young and Older People. Med. Sci. Sports Exerc. 2020, 52, 2179–2188. [Google Scholar] [CrossRef]
- Nosaka, K.; Clarkson, P.M. Variability in serum creatine kinase response after eccentric exercise of the elbow flexors. Int. J. Sports Med. 1996, 17, 120–127. [Google Scholar] [CrossRef]
- Matsuo, S.; Suzuki, S.; Iwata, M.; Hatano, G.; Nosaka, K. Changes in force and stiffness after static stretching of eccentrically-damaged hamstrings. Eur. J. Appl. Physiol. 2015, 115, 981–991. [Google Scholar] [CrossRef]
- Nakamura, M.; Ikezoe, T.; Tokugawa, T.; Ichihashi, N. Acute effects of stretching on passive properties of human gastrocnemius muscle-tendon unit: Analysis of differences between hold-relax and static stretching. J. Sport Rehabil. 2015, 24, 286–292. [Google Scholar] [CrossRef]
- Konrad, A.; Nakamura, M.; Bernsteiner, D.; Tilp, M. The Accumulated Effects of Foam Rolling Combined with Stretching on Range of Motion and Physical Performance: A Systematic Review and Meta-Analysis. J. Sports Sci. Med. 2021, 20, 535–545. [Google Scholar] [CrossRef]


| ICC (1, 1) | CV (%) | |
|---|---|---|
| Knee flexion ROM (°) | 0.825 | 1.6 ± 1.3 |
| MVC-ISO (Nm) | 0.928 | 2.8 ± 1.6 |
| MVC-CON (Nm) | 0.958 | 2.3 ± 1.3 |
| Muscle soreness | ||
| At stretching (mm) | 0.987 | 4.9 ± 3.9 |
| At MVC-ISO (mm) | 0.946 | 5.5 ± 3.9 |
| At MVC-CON (mm) | 0.733 | 5.5 ± 3.3 |
| At palpation (mm) | 0.983 | 4.9 ± 1.8 |
| PPT (kg) | 0.966 | 7.9 ± 5.5 |
| Tissue hardness (N) | 0.838 | 5.3 ± 2.6 |
| Baseline | 48 h after ECC Exercise | Δ Change from Baseline to 48 h after ECC Exercise | |
|---|---|---|---|
| Knee flexion ROM (°) | 136.9 ± 6.7 | 116.5 ± 16.9 | −20.4 ± 16.1 |
| MVC-ISO (Nm) | 159.4 ± 26.0 | 104.5 ± 32.0 | −54.8 ± 36.0 |
| MVC-CON (Nm) | 166.4 ± 27.1 | 107.9 ± 38.6 | −58.5 ± 42.4 |
| Muscle soreness | |||
| At stretching (mm) | 5.5 ± 13.2 | 39.2 ± 22.1 | 33.7 ± 20.3 |
| At MVC-ISO (mm) | 6.6 ± 8.5 | 36.4 ± 20.9 | 29.7 ± 19.4 |
| At MVC-CON (mm) | 6.2 ± 8.5 | 35.6 ± 22.6 | 29.3 ± 22.2 |
| At palpation (mm) | 10.3 ± 9.8 | 42.6 ± 18.5 | 31.7 ± 18.8 |
| PPT (kg) | 2.6 ± 1.2 | 1.5 ± 1.0 | −1.1 ± 1.0 |
| Tissue hardness (N) | 18.0 ± 4.0 | 20.5 ± 3.8 | 2.6 ± 3.1 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Konrad, A.; Kasahara, K.; Yoshida, R.; Yahata, K.; Sato, S.; Murakami, Y.; Aizawa, K.; Nakamura, M. Relationship between Eccentric-Exercise-Induced Loss in Muscle Function to Muscle Soreness and Tissue Hardness. Healthcare 2022, 10, 96. https://doi.org/10.3390/healthcare10010096
Konrad A, Kasahara K, Yoshida R, Yahata K, Sato S, Murakami Y, Aizawa K, Nakamura M. Relationship between Eccentric-Exercise-Induced Loss in Muscle Function to Muscle Soreness and Tissue Hardness. Healthcare. 2022; 10(1):96. https://doi.org/10.3390/healthcare10010096
Chicago/Turabian StyleKonrad, Andreas, Kazuki Kasahara, Riku Yoshida, Kaoru Yahata, Shigeru Sato, Yuta Murakami, Kodai Aizawa, and Masatoshi Nakamura. 2022. "Relationship between Eccentric-Exercise-Induced Loss in Muscle Function to Muscle Soreness and Tissue Hardness" Healthcare 10, no. 1: 96. https://doi.org/10.3390/healthcare10010096
APA StyleKonrad, A., Kasahara, K., Yoshida, R., Yahata, K., Sato, S., Murakami, Y., Aizawa, K., & Nakamura, M. (2022). Relationship between Eccentric-Exercise-Induced Loss in Muscle Function to Muscle Soreness and Tissue Hardness. Healthcare, 10(1), 96. https://doi.org/10.3390/healthcare10010096








