Factors Related to Locomotive Syndrome in School-Aged Children in Okazaki: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
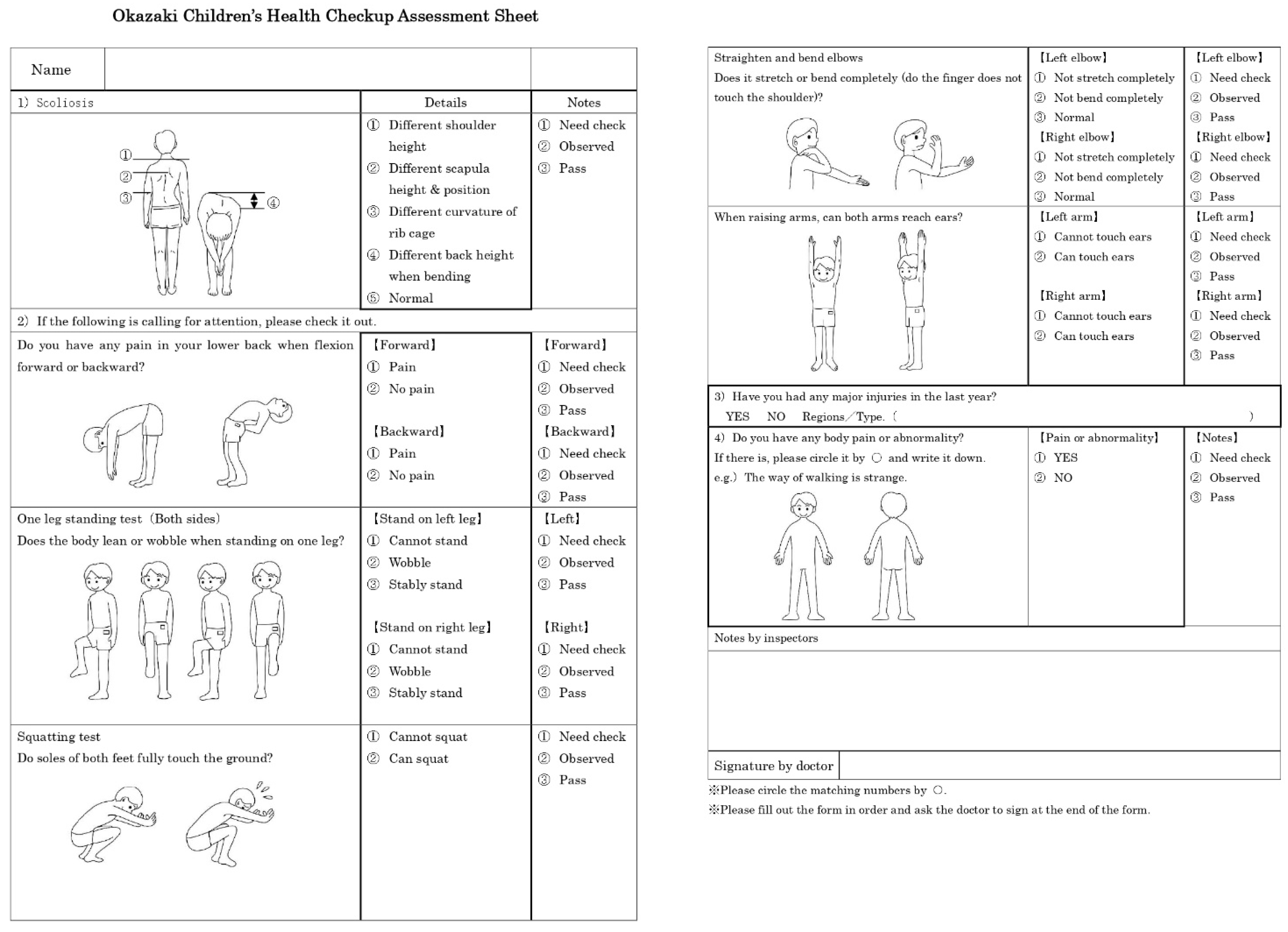
2.2.1. Health-Checkup Assessment Sheet
- (1)
- Scoliosis
- (2)
- Forward and backward flexion
- (3)
- Standing on one leg
- (4)
- Squatting
- (5)
- Elbow-straightening and bending
- (6)
- Arm-raising
- (7)
- Major injuries in the last year (yes/no)
- (8)
- Current body pain or abnormality (yes/no)
2.2.2. Measurement of Variables
- (9)
- Body-fat percentage
- (10)
- Bone stiffness index
- (11)
- Grip strength
- (12)
- Two-step value
- (13)
- Gait deviation index (GDI)
- (14)
- Gait speed
- (15)
- Lifestyle-assessment questionnaire
- How much time does your child spend performing sports per week?
- How much time does your child spend watching TV (including Internet content) per day?
- How much time does your child spend playing video games per day?
2.3. Sample Size
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/musculoskeletal-conditions (accessed on 8 February 2021).
- Nakamura, K.; Ogata, T. Locomotive Syndrome: Definition and Management. Clin. Rev. Bone Miner. Metab. 2016, 14, 56–67. [Google Scholar] [CrossRef] [Green Version]
- Hayashi, S.; Shibata, T.; Samejima, H. Child locomotive syndrome and school medical examination of locomotive organs. J. Jpn. Orthop. Assoc. 2017, 91, 338–344. [Google Scholar]
- Tan, A.; Strauss, V.Y.; Protheroe, J.; Dunn, K.M. Epidemiology of paediatric presentations with musculoskeletal problems in primary care. BMC Musculoskelet. Disord. 2018, 19, 40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yamaguchi, N.; Chosa, E.; Yamamoto, K.; Kawahara, K.; Hamada, H.; Taniguchi, N.; Tajima, T.; Funamoto, T.; Kurogi, S.; Ota, T.; et al. Screening for musculoskeletal problems in Japanese schoolchildren: A cross-sectional study nested in a cohort. Public Health 2016, 139, 189–197. [Google Scholar] [CrossRef]
- Defranco, M.J.; Carl, R.; Goodwin, R.C.; Bergfeld, J.A. Musculoskeletal disease in children and teenagers: Addressing an emerging epidemic. J. Musculoskelet. Med. 2009, 26, 54–57. [Google Scholar]
- Henschke, N.; Harrison, C.; McKay, D.; Broderick, C.; Latimer, J.; Britt, H.; Maher, C.G. Musculoskeletal conditions in children and adolescents managed in Australian primary care. BMC Musculoskelet. Disord. 2014, 15, 164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, J.H.; Hoshino, Y.; Nakamura, K.; Kariya, Y.; Saita, K.; Ito, K. Trunk Muscle Weakness as a Risk Factor for Low Back Pain: A 5-Year Prospective Study. Spine 1999, 24, 54–57. [Google Scholar] [CrossRef]
- Hrysomallis, C. Balance ability and athletic performance. Sports Med. 2011, 41, 221–232. [Google Scholar] [CrossRef] [Green Version]
- Sabui, T.K.; Samanta, M.; Mondal, R.K.; Banerjee, I.; Saren, A.; Hazra, A. Survey of musculoskeletal abnormalities in school-going children of hilly and foothill regions of Eastern Himalayas using the pediatric Gait, Arms, Legs, Spine screening method. Int. J. Rheum. Dis. 2016, 21, 1127–1134. [Google Scholar] [CrossRef]
- Krul, M.; Van Der Wouden, J.C.; Schellevis, F.G.; Van Suijlekom-Smit, L.W.A.; Koes, B.W. Musculoskeletal Problems in Overweight and Obese Children. Ann. Fam. Med. 2009, 7, 352–356. [Google Scholar] [CrossRef]
- Lazarou, C.; Soteriades, E.S. Children’s physical activity, TV watching and obesity in Cyprus: The CYKIDS study. Eur. J. Public Health 2009, 20, 70–77. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Raven, J.; Raven, J.C.; Court, J.H. Manual for Raven’s Progressive Matrices and Vocabulary Scales, 1998 ed.; Oxford Psychologists Press: Oxford, UK, 1998. [Google Scholar]
- Janicki, J.A.; Alman, B. Scoliosis: Review of diagnosis and treatment. Paediatr. Child Health 2007, 12, 771–776. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomaru, Y.; Kamada, H.; Tsukagoshi, Y.; Nakagawa, S.; Tanaka, K.; Takeuchi, R.; Mataki, Y.; Miyakawa, S.; Yamazaki, M. Screening for musculoskeletal problems in children using a questionnaire. J. Orthop. Sci. 2019, 24, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Oshima, Y.; Doi, T.; Kato, S.; Taniguchi, Y. Association between ossification of the longitudinal ligament of the cervical spine and arteriosclerosis in the carotid artery. Sci Rep. 2020, 25, 3369. [Google Scholar] [CrossRef] [Green Version]
- Kojima, K.; Kamai, D.; Ishitani, S.; Watanabe, S. Availability of the Two-step Test to evaluate balance in frail people in a day care service. J. Phys. Ther. Sci. 2017, 29, 1025–1028. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, M.H.; Rozumalski, A. The gait deviation index: A new comprehensive index of gait pathology. Gait Posture 2008, 28, 351–357. [Google Scholar] [CrossRef]
- Ito, T.; Noritake, K.; Sugiura, H.; Kamiya, Y. Association between Gait Deviation Index and Physical Function in Children with Bilateral Spastic Cerebral Palsy: A Cross-Sectional Study. J. Clin. Med. 2020, 9, 28. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Liu, J.H.; Jones, S.J.; Sun, H.; Probst, J.C.; Merchant, A.T.; Cavicchia, P. Diet, Physical Activity, and Sedentary Behaviors as Risk Factors for Childhood Obesity: An Urban and Rural Comparison. Child. Obes. 2012, 8, 440–448. [Google Scholar] [CrossRef]
- Kwok, S.W.H.; Lee, P.H.; Lee, R.L.T. Smart Device Use and Perceived Physical and Psychosocial Outcomes among Hong Kong Adolescents. Int. J. Environ. Res. Public Health 2017, 14, 205. [Google Scholar] [CrossRef] [Green Version]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U.; Lancet Physical Activity Series Working Group. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- Coleman, J.; Straker, L.; Ciccarelli, M. Why do children think they get discomfort related to daily activities? Work 2009, 32, 267–274. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lebrun, D.G.; Talwar, D.; Pham, T.A.; Banskota, B.; Spiegel, D.A. Predictors of healthcare seeking delays among children with chronic musculoskeletal disorders in Nepal. J. Epidemiol. Glob. Health 2017, 7, 299. [Google Scholar] [CrossRef] [PubMed]
- Ishii, K.; Shibata, A.; Adachi, M.; Nonoue, K.; Oka, K. Gender and grade differences in objectively measured physical activity and sedentary behavior patterns among Japanese children and adolescents: A cross-sectional study. BMC Public Health 2015, 15, 1254. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohen, D.E.; Soubhi, H.; Raina, P. Maternal reports of child injuries in Canada: Trends and patterns by age and gender. Inj. Prev. 2000, 6, 223–228. [Google Scholar] [CrossRef] [Green Version]
- Akahane, M.; Yoshihara, S.; Maeyashiki, A.; Tanaka, Y.; Imamura, T. Lifestyle factors are significantly associated with the locomotive syndrome: A cross-sectional study. BMC Geriatr. 2017, 17, 241. [Google Scholar] [CrossRef]
- Li, Y.; McClure, P.W.; Pratt, N. The Effect of Hamstring Muscle Stretching on Standing Posture and on Lumbar and Hip Motions During Forward Bending. Phys. Ther. 1996, 76, 836–845. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Spady, D.W.; Saunders, D.L.; Schopflocher, D.P.; Svenson, L.W. Patterns of injury in children: A population-based approach. Pediatrics 2004, 113 Pt 1, 522–529. [Google Scholar] [CrossRef]

| Variables | Children with Locomotive Syndrome (n = 115) | Children without Locomotive Syndrome (n = 170) | p-Value |
|---|---|---|---|
| Age (years) 1 | 9 (6–12) | 8 (6–12) | 0.004 * |
| Sex, male/female 2 | 76/39 | 68/102 | 0.001 * |
| Height (cm) 1 | 133.0 (106.5–164.2) | 127.8 (108.8–158.2) | 0.002 * |
| Weight (kg) 1 | 28.7 (16.1–57.7) | 25.1 (16.6–59.6) | 0.001 * |
| Body mass index (kg/m2) 1 | 16.0 (13.1–26.6) | 15.2 (13.0–24.2) | 0.002 * |
| Variables | Children with Locomotive Syndrome (n = 115) | Children without Locomotive Syndrome (n = 170) | p-Value |
|---|---|---|---|
| Body fat percentage (%) | 12.9 (3.9–42.7) | 11.7 (3.3–35.7) | 0.159 |
| Stiffness index | 81.7 ± 11.4 | 80.3 ± 12.6 | 0.205 |
| Grip strength (kg) | 12.0 (5.25–21.4) | 11.0 (5.6–26.8) | 0.142 |
| Two-step value | 1.6 (0.8–2.0) | 1.6 (1.0–1.9) | 0.386 |
| Gait deviation index | 94.1 ± 7.4 | 94.5 ± 7.1 | 0.586 |
| Gait speed (m/s) | 1.2 (0.7–1.8) | 1.1 (0.8–1.7) | 0.405 |
| Physical activity (h/week) | 5.0 (0–20.0) | 4.0 (0–25.5) | 0.127 |
| Watching television (h/day) | 2.0 (0.5–10.0) | 1.5 (0–9.0) | 0.022 * |
| Playing video games (h/day) | 0.5 (0–4.0) | 0.5 (0–7.0) | 0.002 * |
| Variables | Odds Ratio | 95% Confidence Interval | p-Value 1 |
|---|---|---|---|
| Age | 1.421 | 1.039–1.945 | 0.028 * |
| Sex (male) | 4.011 | 2.189–7.347 | 0.001 * |
| Height | 1.040 | 0.986–1.098 | 0.150 |
| Body fat percentage | 1.064 | 1.014–1.117 | 0.012 * |
| Stiffness index value | 0.985 | 0.959–1.011 | 0.256 |
| Grip strength | 0.854 | 0.757–0.964 | 0.010 * |
| Two-step value | 0.993 | 0.978–1.008 | 0.358 |
| Gait deviation index | 0.996 | 0.960–1.033 | 0.836 |
| Gait speed | 0.589 | 0.122–2.838 | 0.510 |
| Physical activity | 1.012 | 0.949–1.080 | 0.715 |
| Watching television | 1.281 | 1.001–1.640 | 0.049 * |
| Playing video games | 0.982 | 0.663–1.457 | 0.929 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gu, Y.; Ito, T.; Ito, Y.; Noritake, K.; Ochi, N.; Matsunaga, N.; Takahashi, D.; Sugiura, H. Factors Related to Locomotive Syndrome in School-Aged Children in Okazaki: A Cross-Sectional Study. Healthcare 2021, 9, 1595. https://doi.org/10.3390/healthcare9111595
Gu Y, Ito T, Ito Y, Noritake K, Ochi N, Matsunaga N, Takahashi D, Sugiura H. Factors Related to Locomotive Syndrome in School-Aged Children in Okazaki: A Cross-Sectional Study. Healthcare. 2021; 9(11):1595. https://doi.org/10.3390/healthcare9111595
Chicago/Turabian StyleGu, Yingzhi, Tadashi Ito, Yuji Ito, Koji Noritake, Nobuhiko Ochi, Naomichi Matsunaga, Daiki Takahashi, and Hideshi Sugiura. 2021. "Factors Related to Locomotive Syndrome in School-Aged Children in Okazaki: A Cross-Sectional Study" Healthcare 9, no. 11: 1595. https://doi.org/10.3390/healthcare9111595
APA StyleGu, Y., Ito, T., Ito, Y., Noritake, K., Ochi, N., Matsunaga, N., Takahashi, D., & Sugiura, H. (2021). Factors Related to Locomotive Syndrome in School-Aged Children in Okazaki: A Cross-Sectional Study. Healthcare, 9(11), 1595. https://doi.org/10.3390/healthcare9111595







