Implementation of an Advance Care Planning Inventory and Its Possible Effect on Quality of Dying: A Nationwide Cross-Sectional Study in Group Homes for Persons with Dementia in Japan
Abstract
1. Introduction
2. Materials and Methods
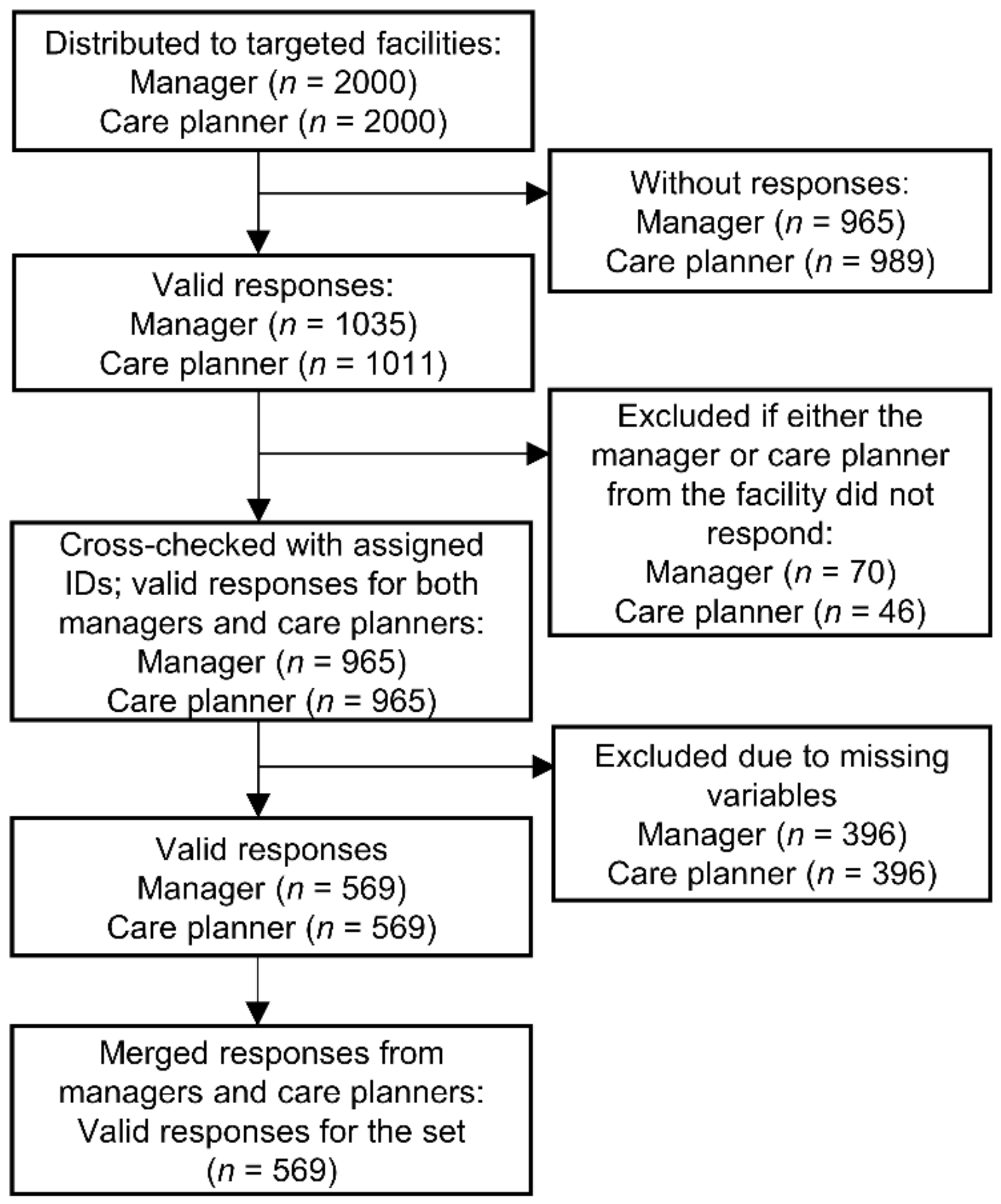
2.1. Participants and Procedure
2.2. Measures
2.2.1. Demographic Characteristics
2.2.2. ACP Practice Inventory (ACP-PI)
2.2.3. Quality of Dying
2.2.4. Covariates
2.2.5. Japanese Version of the Frommelt Attitudes toward Care of the Dying Scale, Short Version (FATCOD-B-J-S)
2.3. Analysis
2.3.1. Validity and Reliability of the ACP-PI
2.3.2. Logistic Regression Analysis
2.4. Ethical Considerations
3. Results
3.1. Validity and Reliability of the ACP-PI
3.2. Association between ACP-PI and QOD-LTC
4. Discussion
4.1. Structure of the ACP-PI for Group Homes for PWD
4.2. Description of Factors of the ACP-PI
4.3. Association of the ACP-PI with QOD-LTC
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Alzheimer’s Disease International. World Alzheimer Report 2019—Attitudes to Dementia; Alzheimer’s Disease International: London, UK, 2019; Available online: https://www.alzint.org/resource/world-alzheimer-report-2019/ (accessed on 10 March 2021).
- Cabinet Office of Japan. White Paper on the Aging Society (Summary Version) Health and Welfare of the Elderly; Cabinet Office of Japan: Tokyo, Japan, 2016; p. FY2016. Available online: https://www8.cao.go.jp/kourei/whitepaper/w-2016/html/gaiyou/s1_2_3.html (accessed on 10 March 2021).
- International Longevity Center, Japan. Overview of the Revision of the Long-Term Care Insurance System—Amendment of the Long-Term Care Insurance Law and Long-Term Care Fee; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2008; Available online: http://www.ilcjapan.org/linksE/doc/Overview_of_the_Revision_of_LTCI.pdf (accessed on 10 March 2021).
- Social Security Council. Overview of Group Homes for Person with Dementia; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2009; Available online: https://www.mhlw.go.jp/shingi/2009/05/dl/s0521-3c_0018.pdf (accessed on 10 March 2021).
- Social Security Council, Subcommittee on Nursing Care Benefits. Support for Dementia; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2011; Available online: https://www.mhlw.go.jp/stf/shingi/2r9852000001va0b-att/2r9852000001va2g.pdf (accessed on 10 March 2021).
- National Association of Group Homes for Dementia. Research Project on End-of-Life Care in Group Homes for Dementia; National Association of Group Homes for Dementia: Tokyo, Japan, 2007; Available online: https://www.ghkyo.or.jp/news/wp-content/uploads/2017/02/chousakenkyuujigyouhoukoku-02.pdf (accessed on 10 March 2021).
- Ogawara, H.; Fukahori, H.; Hirooka, K.; Miyashita, M. Quality evaluation and improvement for end-of-life care toward residents in long term care facilities in Japan: A Literature Review. Palliat. Care Res. 2016, 11, 401–412. [Google Scholar] [CrossRef]
- Sudore, R.L.; Lum, H.D.; You, J.J.; Hanson, L.C.; Meier, D.E.; Pantilat, S.Z.; Matlock, D.D.; Rietjens, J.A.C.; Korfage, I.J.; Ritchie, C.S.; et al. Defining advance care planning for adults: A consensus definition from a multidisciplinary Delphi panel. J. Pain Symptom Manag. 2017, 53, 821–832.e1. [Google Scholar] [CrossRef]
- Dixon, J.; Karagiannidou, M.; Knapp, M. The effectiveness of advance care planning in improving end-of-life outcomes for people with dementia and their carers: A systematic review and critical discussion. J. Pain Symptom Manag. 2018, 55, 132–150.e1. [Google Scholar] [CrossRef]
- Pivodic, L.; Smets, T.; Van den Noortgate, N.; Onwuteaka-Philipsen, B.D.; Engels, Y.; Szczerbińska, K.; Finne-Soveri, H.; Froggatt, K.; Gambassi, G.; Deliens, L.; et al. Quality of dying and quality of end-of-life care of nursing home residents in six countries: An epidemiological study. Palliat. Med. 2018, 32, 1584–1595. [Google Scholar] [CrossRef]
- Garden, G.; Green, S.; Pieniak, S.; Gladman, J. The Bromhead Care Home Service: The impact of a service for care home residents with dementia on hospital admission and dying in preferred place of care. Clin. Med. 2016, 16, 114–118. [Google Scholar] [CrossRef]
- Brazil, K.; Carter, G.; Cardwell, C.; Clarke, M.; Hudson, P.; Froggatt, K.; McLaughlin, D.; Passmore, P.; Kernohan, W.G. Effectiveness of advance care planning with family carers in dementia nursing homes: A paired cluster randomized controlled trial. Palliat. Med. 2018, 32, 603–612. [Google Scholar] [CrossRef]
- Detering, K.M.; Hancock, A.D.; Reade, M.C.; Silvester, W. The impact of advance care planning on end of life care in elderly patients: Randomised controlled trial. BMJ 2010, 340, c1345. [Google Scholar] [CrossRef]
- Ministry of Health, Labour and Welfare. Search for Nursing Care Facilities and Living-Related Information—Nursing Care Service Information Publication System; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2021; Available online: https://www.kaigokensaku.mhlw.go.jp/ (accessed on 10 March 2021).
- Mokkink, L.B.; Terwee, C.B.; Patrick, D.L.; Alonso, J.; Stratford, P.W.; Knol, D.L.; Bouter, L.M.; de Vet, H.C.W. COSMIN Checklist Manual; University Medical Center: Amsterdam, The Netherlands, 2012. [Google Scholar]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Japan Medical Association. Guidelines for Medical Care and Treatment in the End-of-Life Stage; Japan Medical Association: Tokyo, Japan, 2018; Available online: https://www.med.or.jp/dl-med/doctor/r0205_acp_guideline.pdf (accessed on 10 December 2021).
- National Health Service. Advance Care Planning: A Guide for Health and Social Care Staff; National Health Service: London, UK, 2007; Available online: https://www.stlukes-hospice.org.uk/wp-content/uploads/2017/06/ACP-Guide-for-Health-and-Social-Care-Staff-.pdf (accessed on 12 December 2021).
- Fitch, K.; Bernstein, S.J.; Aguilar, M.D.; Burnand, B.; LaCalle, J.R.; Lazaro, P.; van het Loo, M.; McDonnell, J.; Vader, J.; Kahan, J.P. The RAND/UCLA Appropriateness Method User’s Manual; RAND Corporation: Santa Monica, CA, USA, 2001; Available online: https://www.rand.org/pubs/monograph_reports/MR1269.html (accessed on 16 December 2021).
- Munn, J.C.; Zimmerman, S.; Hanson, L.C.; Williams, C.S.; Sloane, P.D.; Clipp, E.C.; Tulsky, J.A.; Steinhauser, K.E. Measuring the quality of dying in long-term care. J. Am. Geriatr. Soc. 2007, 55, 1371–1379. [Google Scholar] [CrossRef]
- Sclan, S.G.; Reisberg, B. Functional Assessment Staging (FAST) in Alzheimer’s disease: Reliability, validity, and ordinality. Int. Psychogeriatr. 1992, 4 (Suppl. S1), 55–69. [Google Scholar] [CrossRef] [PubMed]
- Tay, R.Y.; Hum, A.Y.M.; Ali, N.B.; Leong, I.Y.O.; Wu, H.Y.; Chin, J.J.; Lee, A.O.K.; Koh, M.Y.H. Comfort and satisfaction with care of home-dwelling dementia patients at the end of life. J. Pain Symptom Manag. 2020, 59, 1019–1032.e1. [Google Scholar] [CrossRef] [PubMed]
- Social Security Council. [Theme 1] End-of-Life Care, Reference Materials; Ministry of Health, Labour and Welfare: Tokyo, Japan, 2017; Available online: https://www.mhlw.go.jp/file/05-Shingikai-12404000-Hokenkyoku-Iryouka/0000156003.pdf (accessed on 10 March 2021).
- Frommelt, K.H. The effects of death education on nurses’ attitudes toward caring for terminally ill persons and their families. Am. J. Hosp. Palliat. Care 1991, 8, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Nakai, Y.; Miyashita, M.; Sasahara, T.; Koyama, Y.; Shimizu, Y.; Kawa, M. Factor structure and reliability of the Japanese version of the Frommelt Attitudes Toward Care of the Dying Scale (FATCOD-B-J). Jpn. J. Cancer Care 2006, 11, 723–729. [Google Scholar] [CrossRef]
- Moshagen, M.; Musch, J. Sample size requirements of the robust weighted least squares estimator. Methodology 2014, 10, 60–70. [Google Scholar] [CrossRef]
- Hu, L.T.; Bentler, P.M. Cutoff Criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Struct. Equ. Model. Multidiscip. J. 1999, 6, 1–55. [Google Scholar] [CrossRef]
- MacCallum, R.C.; Browne, M.W.; Sugawara, H.M. Power analysis and determination of sample size for covariance structure modeling. Psychol. Methods 1996, 1, 130–149. [Google Scholar] [CrossRef]
- Terwee, C.B.; Bot, S.D.; de Boer, M.R.; van der Windt, D.A.; Knol, D.L.; Dekker, J.; Bouter, L.M.; de Vet, H.C. Quality criteria were proposed for measurement properties of health status questionnaires. J. Clin. Epidemiol. 2007, 60, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Dormann, C.F.; Elith, J.; Bacher, S.; Buchmann, C.; Carl, G.; Carré, G.; Marquéz, J.R.G.; Gruber, B.; Lafourcade, B.; Leitão, P.J.; et al. Collinearity: A review of methods to deal with it and a simulation study evaluating their performance. Ecography 2013, 36, 27–46. [Google Scholar] [CrossRef]
- Brown, T.A.; Little, T.D. Confirmatory Factor Analysis for Applied Research, 2nd ed.; Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- Lüdecke, D.; von dem Knesebeck, O.; Kofahl, C. Public knowledge about dementia in Germany—Results of a population survey. Int. J. Public Health 2016, 61, 9–16. [Google Scholar] [CrossRef]
- Hirakawa, Y.; Masuda, Y.; Uemura, K.; Kuzuya, M.; Kimata, T.; Iguchi, A. End-of-life care at group homes for patients with dementia in Japan. Findings from an analysis of policy-related differences. Arch. Gerontol. Geriatr. 2006, 42, 233–245. [Google Scholar] [CrossRef]
- Sudore, R.L.; Boscardin, J.; Feuz, M.A.; McMahan, R.D.; Katen, M.T.; Barnes, D.E. Effect of the PREPARE website vs. an easy-to-read advance directive on advance care planning documentation and engagement among veterans: A randomized clinical trial. JAMA Intern. Med. 2017, 177, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Katahira, N.; Tsukasaki, K. Nursing care in multifunctional small group homes providing day, visiting and overnight services for older people living at home. Int. J. Nurs. Pract. 2016, 22, 605–615. [Google Scholar] [CrossRef] [PubMed]
| Variables | Frequency (%) | Mean (SD) |
|---|---|---|
| Facility | ||
| Established by | ||
| Social welfare corporations | 115 (20.2) | |
| Medical corporations | 103 (18.1) | |
| For-profit corporations | 300 (52.7) | |
| Other or no response | 51 (9.0) | |
| Number of units | ||
| 1 | 150 (26.4) | |
| 2 | 370 (65.0) | |
| 3 or more | 38 (6.7) | |
| No response | 11(1.9) | |
| Year of establishment (A.D.) | 2007.0 (6.2) | |
| Number of full-time nurses | 0.8 (2.5) | |
| Number of residents | 15.9 (6.5) | |
| Managers | ||
| Sex | ||
| Male | 229 (40.2) | |
| Female | 333 (58.5) | |
| No response | 7 (1.2) | |
| Type of work † | ||
| Care worker | 429 (75.4) | |
| Care manager | 252 (44.3) | |
| Nurse | 40 (7.0) | |
| Age (years) | 49.8 (10.5) | |
| Experience at the facility (years) | 9.8 (5.7) | |
| Experience as a manager (years) | 5.9 (4.8) | |
| Care Planners | ||
| Sex | ||
| Male | 152 (26.7) | |
| Female | 410 (72.1) | |
| No response | 7 (1.2) | |
| Type of work † | ||
| Care worker | 446 (78.4) | |
| Care manager | 410 (72.1) | |
| Nurse | 32 (5.6) | |
| Age (years) | 50.0 (10.9) | |
| Experience at the facility (years) | 8.4 (5.3) | |
| FATCOD-B-J-S score | ||
| Total | 23.1 (2.8) | |
| Sub-scale 1 | 11.4 (1.8) | |
| Sub-scale 2 | 11.7 (2.0) |
| Variables | Frequency (%) | Mean (SD) |
|---|---|---|
| Sex | ||
| Male | 124 (21.8) | |
| Female | 445 (78.2) | |
| FAST level at the time of death | 6.4 (1.1) | |
| 6 or less | 224 (39.4) | |
| 7 | 345 (60.6) | |
| Presence of end-of-life bonus | ||
| Yes | 359 (63.1) | |
| Length of stay in the facility (years) | 4.6 (3.8) | |
| Age at the time of death (years) | 91.4 (6.4) | |
| QOD-LTC score | ||
| Composite score | 3.3 (0.7) | |
| Sub-scale 1 | 3.9 (0.6) | |
| Sub-scale 2 | 3.3 (0.8) | |
| Sub-scale 3 | 2.7 (1.2) | |
| QOD-LTC score | ||
| High | 354 (62.2) |
| Frequency (%) | ||||||
|---|---|---|---|---|---|---|
| No. | Items | Did Not Implement | More or Less Did Not Implement | More or Less Implemented | Implemented | Mean (SD) |
| 23 | We asked Mr./Ms. A’s family members and other relevant parties about what Mr./Ms. wished regarding the final stage of life. | 16 (2.8) | 6 (1.1) | 80 (14.1) | 467 (82.1) | 3.8 (0.6) |
| 24 | We talked with A’s family members about Mr./Ms. A’s medical treatment/care options for the final stage of life. | 16 (2.8) | 2 (0.4) | 60 (10.5) | 491 (86.3) | 3.8 (0.6) |
| 25 | We talked with Mr./Ms. A’s family members or other relevant parties about relief and comfort care for distressing symptoms (e.g., breathlessness or discomfort from being unable to move) at the final stage of life. | 17 (3.0) | 9 (1.6) | 72 (12.7) | 472 (83.0) | 3.8 (0.6) |
| 26 | We facilitated and supported Mr./Ms. A’s discussions with their family members so that they could all reach a consensus concerning the policies and procedures regarding the final stage of life. | 26 (4.6) | 29 (5.1) | 112 (19.7) | 402 (70.7) | 3.6 (0.8) |
| 27 | In cases where family members or other relevant parties requested, staff members always accepted calls for consultation regarding the final stage of Mr./Ms. A’s life. | 13 (2.3) | 4 (0.7) | 107 (18.8) | 445 (78.2) | 3.7 (0.6) |
| 28 | After discussing Mr./Ms. A’s medical treatment/care policies with both family and staff members, we documented the details in Mr./Ms. A’s records. | 16 (2.8) | 16 (2.8) | 85 (14.9) | 452 (79.4) | 3.7 (0.7) |
| 29 | We asked family members and relevant parties whether or not there were any changes in their wishes regarding Mr./Ms. A’s medical treatment/care, as needed. | 16 (2.8) | 22 (3.9) | 109 (19.2) | 422 (74.2) | 3.7 (0.7) |
| 31 | We recorded wishes Mr./Ms. A had in relation to the kind of medical treatment/care. | 55 (9.7) | 53 (9.3) | 127 (22.3) | 334 (58.7) | 3.3 (1.0) |
| 32 | Information about Mr./Ms. A, even if it was not medical treatment/care-related, was kept in the records. | 7 (1.2) | 17 (3.0) | 139 (24.4) | 406 (71.4) | 3.7 (0.6) |
| 33 | The medical treatment/care policies for the final stage of Mr./Ms. A’s life were discussed and decided by the team at the facility. | 8 (1.4) | 22 (3.9) | 139 (24.4) | 400 (70.3) | 3.6 (0.6) |
| 34 | We shared Mr./Ms. A’s wishes regarding medical treatment/care with the relevant doctors. | 14 (2.5) | 11 (1.9) | 112 (19.7) | 432 (75.9) | 3.7 (0.6) |
| 35 | We shared Mr./Ms. A’s wishes regarding their medical treatment/care, as well as other relevant matters, with facility staff members. | 11 (1.9) | 14 (2.5) | 128 (22.5) | 416 (73.1) | 3.7 (0.6) |
| 36 | We shared Mr./Ms. A’s wishes about medical treatment/care with the long-term care insurance facilities and medical institution staff with whom we work. | 25 (4.4) | 34 (6.0) | 126 (22.1) | 384 (67.5) | 3.5 (0.8) |
| 37 | We kept a record of observations and significant changes pertaining to Mr./Ms. A. | 6 (1.1) | 4 (0.7) | 85 (14.9) | 474 (83.3) | 3.8 (0.5) |
| 38 | In making decisions about Mr./Ms. A’s medical treatment/care, as well as other matters, we took into consideration the wishes Mr./Ms. A expressed regarding the final stage of life and everyday routines. | 41 (7.2) | 61 (10.7) | 184 (32.3) | 283 (49.7) | 3.3 (0.9) |
| 39 | We took Mr./Ms. A’s quality of life into account when making decisions about medical treatment/care. | 4 (0.7) | 17 (3.0) | 193 (33.9) | 355 (62.4) | 3.6 (0.6) |
| No. | Item | Factor Loading | ||
|---|---|---|---|---|
| Factor 1. Provision of information and conversation with the resident to encourage them to express their end-of-life wishes | ||||
| 1 | We judged from Mr./Ms. A’s words, actions, and appearance whether or not they were willing to talk about the final stage of life. | 0.48 | −0.09 | 0.15 |
| 2 | We informed Mr./Ms. A about the medical treatment/care available and how they could spend the final stage of life, as detailed within the facility’s policies. | 0.86 | −0.01 | −0.02 |
| 3 | We informed Mr./Ms. A of the significance of communicating their wishes regarding the final stage of life and everyday routines to family and the facility’s staff members while they were still able to express wishes. | 0.86 | 0.06 | −0.08 |
| 4 | We informed Mr./Ms. A of what things they should tell family and staff members while they were still able to express wishes. | 0.77 | 0.09 | −0.02 |
| 5 | We presented Mr./Ms. A with specific details about what medical treatment/care options were available as they entered the final stage of life (note: this statement includes cases where part-time doctors or similar staff presented the information). | 0.77 | 0.04 | −0.01 |
| 7 | We talked with Mr./Ms. A about what kind of medical treatment/care they wished for at the final stage of life. | 0.93 | −0.01 | −0.05 |
| 8 | We talked with Mr./Ms. A about where they would like to spend the final stages of life. | 0.87 | −0.05 | −0.06 |
| 9 | We discussed with the patient the kind of care they would like to receive to get relief and comfort from distressing symptoms (e.g., breathlessness or discomfort from being unable to move) at the final stage of life. | 0.79 | 0.00 | 0.05 |
| 10 | We discussed with Mr./Ms. A whether or not there were any changes in the their wishes regarding medical treatment/care each time it happened. | 0.67 | 0.02 | 0.07 |
| 11 | Whenever Mr./Ms. A’s condition changed, we spoke with them to establish whether or not there were any changes in wishes regarding medical treatment/care. | 0.71 | 0.04 | 0.07 |
| Factor 2. Preparations in case the resident becomes unable to express their own end-of-life wish | ||||
| 13 | We asked Mr./Ms. A to put their wishes regarding their medical treatment/care, as well as any other wishes, in writing. | 0.05 | 0.65 | −0.03 |
| 14 | At Mr./Ms. A’s request, we gave a copy of the written document to their spouse stating their wishes regarding medical treatment/care and other matters. | −0.06 | 0.76 | 0.01 |
| 15 | We asked Mr./Ms. A who they wished to participate in discussions about medical treatment/care and other matters relating to the time when they would no longer be able to make their own decisions. | 0.04 | 0.78 | 0.02 |
| 16 | We asked Mr./Ms. A whether or not they had informed the person they mentioned in Point 15 about their desire to have them participate in such discussions. | 0.05 | 0.88 | 0.00 |
| 17 | We informed Mr./Ms. A about representatives and/or systems that handle legal aspects after they pass away (e.g., implementing a will). | −0.04 | 0.71 | 0.02 |
| Factor 3. Devising to encourage the resident to express their wish with consideration for their dementia | ||||
| 19 | We considered the topics of discussion regarding the final stage of Mr./Ms. A’s life depending on their cognitive functioning. | −0.07 | 0.02 | 0.86 |
| 20 | The ways in which I explained the final stage of life were modified depending on Mr./Ms. A’s cognitive functions. | −0.01 | −0.01 | 0.98 |
| 21 | When discussing the final stage of life with Mr./Ms. A, we checked that they understood the content. | 0.27 | 0.03 | 0.55 |
| Cronbach’s α ☨ | 0.94 | 0.86 | 0.87 | |
| Composite score, mean (SD) | 2.0 (0.7) | |||
| Factor 1, mean (SD) | 2.1 (0.8) | |||
| Factor 2, mean (SD) | 1.5 (0.7) | |||
| Factor 3, mean (SD) | 2.5 (0.9) | |||
| Instruction text: Circle the Corresponding Number to Indicate Which of the Following Items Have Been Conducted in Relation to Mr./Ms. A. | |||||
|---|---|---|---|---|---|
| No. | Items | Did not Implement | More or less Did not Implement | More or less Implemented | Implemented |
| 1 | We judged from Mr./Ms. A’s words, actions, and appearance whether or not they were willing to talk about the final stage of life. | 1 | 2 | 3 | 4 |
| 2 | We informed Mr./Ms. A about the medical treatment/care available and how they could spend the final stage of life, as detailed within the facility’s policies. | 1 | 2 | 3 | 4 |
| 3 | We informed Mr./Ms. A of the significance of communicating their wishes regarding the final stage of life and the everyday routines to the family and the facility’s staff members while they were still able to express wishes. | 1 | 2 | 3 | 4 |
| 4 | We informed Mr./Ms. A of what things they should tell family and staff members while they were still able to express wishes. | 1 | 2 | 3 | 4 |
| 5 | We presented Mr./Ms. A with specific details about what medical treatment/care options were available as they entered the final stage of life (note: this statement includes cases where part-time doctors or similar staff presented the information). | 1 | 2 | 3 | 4 |
| 6 | We talked with Mr./Ms. A about what kind of medical treatment/care they wished for at the final stage of life. | 1 | 2 | 3 | 4 |
| 7 | We talked with Mr./Ms. A about where they would like to spend the final stages of life. | 1 | 2 | 3 | 4 |
| 8 | We discussed with the patient about the kind of care they would like to receive to get relief and comfort from distressing symptoms (e.g., breathlessness or discomfort from being unable to move) at the final stage of life. | 1 | 2 | 3 | 4 |
| 9 | We discussed with Mr./Ms. A about whether or not there were any changes in the wishes of Mr./Ms. A regarding medical treatment/care, each time it happens. | 1 | 2 | 3 | 4 |
| 10 | Whenever Mr./Ms. A’s condition changed, we spoke with them to establish whether or not there were any changes in wishes regarding medical treatment/care. | 1 | 2 | 3 | 4 |
| 11 | We asked Mr./Ms. A to put their wishes regarding their medical treatment/care, as well as any other wishes, in writing. | 1 | 2 | 3 | 4 |
| 12 | At Mr./Ms. A’s request, we gave a copy of the written document to Mr./Ms. A stating the wishes regarding medical treatment/care and other matters. | 1 | 2 | 3 | 4 |
| 13 | We asked Mr./Ms. A who they wished to participate in discussions about medical treatment/care and other matters relating to the time when they would no longer be able to make their own decisions. | 1 | 2 | 3 | 4 |
| 14 | We asked Mr./Ms. A whether or not they had informed the person they mentioned in Point 17 about their desire to have them participate in such discussions. | 1 | 2 | 3 | 4 |
| 15 | We informed Mr./Ms. A about representatives and/or systems that handle legal aspects after they pass away (e.g., implementing a will). | 1 | 2 | 3 | 4 |
| 16 | We considered the topics of discussion regarding the final stage of Mr./Ms. A’s life depending on their cognitive functioning. | 1 | 2 | 3 | 4 |
| 17 | The ways in which I explained the final stage of life were modified depending on Mr./Ms. A’s cognitive functions. | 1 | 2 | 3 | 4 |
| 18 | When discussing the final stage of life with Mr./Ms. A, we checked that they understood the content. | 1 | 2 | 3 | 4 |
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | OR (95%CI) | |
| Residents’ characteristics | |||||
| Female sex † | 0.90 (0.57–1.42) | 0.97 (0.61–1.54) | 0.91 (0.58–1.42) | 0.87 (0.55–1.35) | 0.93 (0.59–1.48) |
| Length of stay (years) ‡ | 0.92 (0.54–1.55) | 0.87 (0.52–1.48) | 0.88 (0.52–1.47) | 0.95 (0.56–1.59) | 0.89 (0.53–1.51) |
| Age at death (years) | 1.05 (1.02–1.08) ** | 1.05 (1.02–1.08) ** | 1.05 (1.02–1.09) ** | 1.05 (1.02–1.08) ** | 1.05 (1.02–1.08) ** |
| FAST § | 1.10 (0.76–1.61) | 1.12 (0.76–1.63) | 1.06 (0.73–1.53) | 1.03 (0.71–1.48) | 1.12 (0.77–1.64) |
| GHPWD’s characteristics | |||||
| Number of full-time nurses | 1.13 (1.03–1.25) * | 1.13 (1.02–1.24) * | 1.12 (1.02–1.24) * | 1.13 (1.02–1.25) * | 1.13 (1.03–1.25) * |
| End-of-life care bonus ¶ | 1.64 (1.12–2.38) * | 1.69 (1.16–2.47) ** | 1.57 (1.08–2.27) * | 1.67 (1.16–2.42) ** | 1.66 (1.13–2.42) ** |
| ACP-PI | |||||
| Composite score | 2.62 (1.95–3.53) *** | ||||
| Factor 1 | 2.15 (1.70–2.73) *** | 1.75 (1.28–2.40) *** | |||
| Factor 2 | 2.16 (1.57–2.97) *** | 1.27 (0.87–1.87) | |||
| Factor 3 | 1.65 (1.35–2.01) *** | 1.17 (0.92–1.49) | |||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Takada, S.; Ogata, Y.; Yumoto, Y.; Ikeda, M. Implementation of an Advance Care Planning Inventory and Its Possible Effect on Quality of Dying: A Nationwide Cross-Sectional Study in Group Homes for Persons with Dementia in Japan. Healthcare 2022, 10, 62. https://doi.org/10.3390/healthcare10010062
Takada S, Ogata Y, Yumoto Y, Ikeda M. Implementation of an Advance Care Planning Inventory and Its Possible Effect on Quality of Dying: A Nationwide Cross-Sectional Study in Group Homes for Persons with Dementia in Japan. Healthcare. 2022; 10(1):62. https://doi.org/10.3390/healthcare10010062
Chicago/Turabian StyleTakada, Seira, Yasuko Ogata, Yoshie Yumoto, and Masaomi Ikeda. 2022. "Implementation of an Advance Care Planning Inventory and Its Possible Effect on Quality of Dying: A Nationwide Cross-Sectional Study in Group Homes for Persons with Dementia in Japan" Healthcare 10, no. 1: 62. https://doi.org/10.3390/healthcare10010062
APA StyleTakada, S., Ogata, Y., Yumoto, Y., & Ikeda, M. (2022). Implementation of an Advance Care Planning Inventory and Its Possible Effect on Quality of Dying: A Nationwide Cross-Sectional Study in Group Homes for Persons with Dementia in Japan. Healthcare, 10(1), 62. https://doi.org/10.3390/healthcare10010062






