Abstract
During the COVID-19 confinement, we converted our clinical simulation sessions into simulated video consultations. This study aims to evaluate the effects of virtual simulation-based training on developing and cultivating humanization competencies in undergraduate nursing students. A quasi-experimental study was conducted with 60 undergraduate nursing students. A validated questionnaire was used to evaluate the acquisition of humanization competencies (self-efficacy, sociability, affection, emotional understanding, and optimism). The development of humanization competencies in this group composed of undergraduate nursing students was evaluated using virtual simulation-based training, comparing the levels obtained in these competencies at baseline (pre-test) and after the virtual simulation experience (post-test). After the virtual simulation sessions, students improved their levels in humanization total score and the emotional understanding and self-efficacy competencies, obtaining large effects sizes in all of them (rB = 0.508, rB = 0.713, and rB = 0.505 respectively). This virtual simulation modality enables training in the humanization of care with the collaboration of standardized patients in the form of simulated nursing video consultations and the performance of high-fidelity simulation sessions that comply with the requirements of best practices. Therefore, this methodology could be considered as another choice for virtual simulation. Additionally, this virtual modality could be a way to humanize virtual simulation.
1. Introduction
During the COVID-19 pandemic, governments around the world have declared social distancing measures to ensure the confinement of the population, including the closure of schools and universities. In this sense, this pandemic represents a challenge not only to health services but also to nursing education. In response to this exceptional situation, simulation-based education had to adapt through the use of virtual simulation modalities, thus highly increasing its use, leading to virtual simulation becoming a primary teaching strategy to provide simulated experiences [] using online platforms, specific software or mobile devices [,]. Virtual simulation modalities comprise immersive simulation, screen-based simulation, serious games, virtual reality, virtual simulation/virtual patients, virtual reality simulation, and web-based simulation []. All these modalities provide students with near-reality, interactive virtual simulation learning experiences when face-to-face simulations are not possible [].
To adapt our high-fidelity clinical simulation sessions to virtual simulation, we implemented simulated nursing video consultations in our university during the COVID-19 confinement [,]. Additionally, we considered that nursing students should practice simulated video consultations to train in this healthcare modality that has become both popular and necessary during this pandemic. In this sense, among the different telemedicine modalities, video consultations have been significantly increased [,], implementing them in many countries has been a digital health strategy to provide healthcare [,]. This modality of healthcare has multiple benefits such as avoiding agglomerations owing to social distancing restrictions, patient satisfaction, and cost reduction [,]. However, we were concerned about virtual interactions between nursing students and a standardized patient using virtual simulation sessions, since the distancing between them and the inability to perform an in-person consultation could lead to providing dehumanized and depersonalized nursing care training.
According to David Gaba, considered to be one of the fathers of clinical simulation, simulation is a technique not a technology [], because simulation sessions must not be exclusively based on the use of technological equipment or devices. A simulation setting can help train students in nursing clinical skills, procedures, or techniques, and also the art of nursing generally []. Additionally, it can help students recognize the totality of the human being, providing patient-centered care []. This approach to healthcare is closely linked to the humanization of care construct [].
Nowadays, humanization of care is a fashionable construct within healthcare services, possibly owing to society perceive they are dehumanized and depersonalized []. In short, humanizing healthcare means putting the human being at the center to promote and protect the health, cure diseases, or provide the best care []. However, there is not a consensus on the humanization of care definition to date, but most approaches to this construct offer a definition based on responding to patient’s needs []. The humanization of care construct implies a set of personal competencies that healthcare professionals should have to care for patients effectively and humanely []. In this sense, Pérez-Fuentes et al. [] have recently proposed a humanization of care model which comprises 5 competencies required in healthcare clinical practice: optimism (to generate positive future expectations), sociability (to relate to others appropriately with assertiveness and empathy), emotional understanding (to empathize cognitively with others, placing ourselves in their place), self-efficacy (to manage successfully complex and stressful situations), and affection (to empathize emotionally with the affective state of another person).
Previous studies have demonstrated the effectiveness of simulation-based training mainly in the self-efficacy [] and empathy [] competencies, but no research to date has studied the effects of simulation training in all competencies required to provide humanized nursing care. Specifically, this could represent a significant challenge if this training is conducted through a virtual simulation modality, owing to the virtual interaction and distancing between nursing students and virtual patients. Therefore, this study aimed to evaluate the effects of virtual simulation-based training on developing and cultivating humanization competencies in undergraduate nursing students.
2. Materials and Methods
2.1. Research Context and Setting
A quasi-experimental study was conducted using a single-group pre-test post-test design. The development of humanization competencies in this group composed of undergraduate nursing students was evaluated using virtual simulation-based training, comparing the levels obtained in these competencies at baseline (pre-test) and after the virtual simulation experience (post-test).
2.2. Setting and Sample
The study was performed in a public University between 20 April and 21 May 2020, including 3rd-year undergraduate students enrolled in nursing degree (66 students). These students performed virtual simulation sessions. A total of 60 nursing students participateD in the study (90.9% response rate).
2.3. Simulation Design Process
All simulated nursing video consultations followed the INACSL Standards of Best Practice: SimulationSM [,,,]. During these simulated sessions, all stages included in high-fidelity clinical simulation were accomplished: pre-briefing, briefing, simulated scenario, and debriefing. A virtual platform of online video conferences provided by the university (Blackboard Collaborate LauncherTM) was used to develop all simulation stages [,].
We designed six simulated scenarios related to basic healthcare at patients’ homes who presented the following clinical cases: a patient diagnosed with arterial hypertension, a post-surgical patient (laparoscopic cholecystectomy), a woman with an anxiety disorder (potential case of gender-based violence), a bed-ridden patient with a pressure ulcer, a child diagnosed with attention deficit hyperactivity disorder (ADHD), and a child with a febrile syndrome.
Besides attending to each reason for consultation, adequate management and protection measures to COVID-19 were considered, since all patients were confined during this pandemic. Standardized patients played the role of patients’ homes. These standardized patients were also facilitators during the simulated sessions, and they were changed during the different simulated scenarios. It should be noted a standardized patient played the role of caregiver in the clinical case of a bed-ridden patient with a pressure ulcer, and another played the role of mother when a child needed to be treated. To ensure a high-fidelity level of the simulation experience, we chose all standardized patients for their experience in clinical simulation methodology, and we trained them to play their roles according to recommendations by Lewis et al. [].
All nursing students were divided into 4 groups of 12–16 students per group. In this sense, they formed 6 operational work teams of 2–3 students per group, performing a simulated scenario together and portraying the role of nursing professionals online. Meanwhile, the rest of the work teams were at home, observing their performance in their computer screen using the corresponding virtual platform for online video conferences. In this way, they could learn from the mistakes of their classmates who were performing a simulated scenario. Each simulated session lasted 4 h, and each student completed 3 simulation sessions (1 session of pre-briefing and 2 sessions where 6 simulated scenarios were performed), so each student completed a total of 12 h of simulation experience.
2.4. Data Collection Instrument
To evaluate the acquisition of humanization competencies, the Healthcare Professional Humanization Scale (HUMAS) [] was used. This questionnaire consists of 19 items with a 5-point Likert response scale (from 1 = ‘never’ to 5 = ‘always’). HUMAS comprises the 5 dimensions of humanization of care construct: self-efficacy (5 items), sociability (3 items), affection (5 items), emotional understanding (3 items), and optimism (3 items). To examine the humanization questionnaire reliability, the coefficient omega (ω) [] was calculated. In this way, the internal consistency obtained by its creators for each dimension was satisfactory: optimism (pre-test: ω = 0.78, post-test: ω = 0.84), sociability (pre-test: ω = 0.81, post-test: ω = 0.85), emotional understanding (pre-test: ω = 0.74, post-test: ω = 0.74), self-efficacy (pre-test: ω = 0.79, post-test: ω = 0.78), affection (pre-test: ω = 0.88, post-test: ω = 0.90), and total score (pre-test: ω = 0.88, post-test: ω = 0.88). It should be noted, some items were minimally adapted since the participants were students, and not healthcare professionals (e.g., ‘I feel nervous when I am caring for my patients’ was changed by ‘I feel nervous when I think about caring for patients during my clinical practices.’ The humanization questionnaire was completed online pre- and post-virtual simulation sessions, through a link provided to the participating students.
2.5. Statistical Analysis
Descriptive statistics were calculated (minimal, maximal and mean scores, standard deviation, and percentages) to analyze the results obtained for demographic data and each item, subscale, and the total score obtained in HUMAS. Additionally, the coefficients omega (ω) were calculated to analyze the reliability of this questionnaire. Subsequently, the assumption of normality was tested using the Kolmogorov–Smirnov test, confirming that data did not follow a normal probability distribution. Consequently, to analyze the differences at baseline (pre-test) and after the virtual simulation experience (post-test), the Wilcoxon test was used. Additionally, to determine the effect size of the statistically significant differences obtained, the rank-biserial correlation (rB) was calculated, considering the following cut-off points: 0.10 (small), 0.30 (medium), and 0.50 (large) []. These data were analyzed using IBM SPSS Statistics version 24.0 software for Windows (IBM Corp., Armonk, NY, USA).
2.6. Ethical Considerations
This study was carried out following ethical principles for medical research of the international Declaration of Helsinki []. Additionally, this study was approved by the Research and Ethics Board of the Department of Nursing, Physiotherapy, and Medicine of A. University (Approval no. EFM-75/2020). All nursing students were informed about the study and who accepted to participate voluntarily, signed a written consent.
3. Results
A total of 60 nursing students participated in the study. The age of students ranged from 20 to 50 years (mean = 23.83; SD = 6.63). Most students were women (n = 52; 86.7%).
Descriptive data and reliabilities for each item, subscale, and the total score obtained in HUMAS at baseline (pre-test) and after virtual simulation sessions (post-test) are shown in Table 1. It should be noted that the reliability coefficients calculated for each subscale and the total score in HUMAS were quite similar to values obtained by its creators, indicating satisfactory reliability.

Table 1.
Descriptive data (minimal, maximal and mean scores, and standard deviation) and reliabilities for each item, subscale and the total score obtained in HUMAS at baseline (pre-test) and after virtual simulation sessions (post-test) (N = 60).
The mean scores obtained in each humanization dimension at baseline (pre-test) and after virtual simulation sessions (post-test) were compared (Table 2). Statistically significant differences were obtained in emotional understanding and self-efficacy dimensions, as well as in total score for the humanization scale applied, obtaining large effects sizes in all of them (rB = 0.505, rB = 0.713, and rB = 0.508 respectively).

Table 2.
Differences in mean scores for each humanization dimension and the total score obtained in HUMAS at baseline (pre-test) and after virtual simulation sessions (post-test) (N = 60).
Figure 1 shows graphically the magnitude of the statistically significant differences in emotional understanding and self-efficacy dimensions, and the total score obtained in HUMAS at baseline (pre-test) and after virtual simulation sessions (post-test). It should be noted that the rest of the humanization dimensions are not shown in this figure since only non-statistically significant differences were obtained.
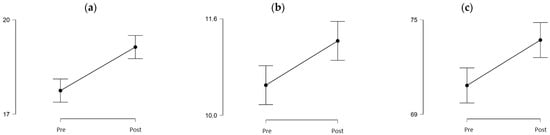
Figure 1.
Statistically significant differences in self-efficacy and emotional understanding dimensions, and the total score obtained in HUMAS at baseline (pre-test) and after virtual simulation sessions (post-test). (a) Self-efficaccy, (b) Emotional understanding, (c) Total score.
4. Discussion
We converted our face-to-face simulated scenarios into a virtual format using simulated nursing video consultations in response to the closure of universities during the confinement due to the COVID-19 pandemic. We performed high-fidelity simulation sessions that complied with the requirements proposed by the INACSL Standards of Best Practice. In previous studies, nursing students expressed high satisfaction with this virtual simulation modality [,], perceiving that it was positively improving their learning process. However, we considered studying whether our conversion could lead nursing students to provide dehumanized and depersonalized nursing care, since virtual interactions are not the same as simulation sessions in a laboratory room.
Our results indicate the positive effects of virtual simulation-based training on developing and cultivating humanization competencies in undergraduate nursing students. After virtual simulation sessions, they improved their levels in humanization total score and the emotional understanding and self-efficacy competencies. It should be noted that emotional understanding is closely related to empathy []. Although there is a lack of studies analyzing the effects on the humanization of care of using clinical simulation methodology, improvements to empathy and self-efficacy in nursing students have been widely demonstrated [,,].
Firstly, empathy is considered as the heart of all nurse-patient interactions [], being a basic component of therapeutic relationships and a crucial factor in quality care []. Additionally, the positive impact of empathic healthcare interactions on patient outcomes has been widely demonstrated [,]. Numerous studies have demonstrated improvement to empathy levels using clinical simulation methodology []. Particularly, single-group studies have demonstrated a significant change in empathy between pre-test and post-test using standardized patients. However, the obtained effect sizes have been often low [,]. Notably, Strekalova et al. [] used a virtual patient during simulated health history interviews and obtained emphatic responses from nursing students. In our study, we obtained increases in empathy levels and a large effect size in this humanization competency using standardized patients during virtual simulation sessions.
Regarding self-efficacy, this competency consists of a future-oriented optimistic belief that increases motivation, equating to improved performance []. Self-efficacy is considered as a healthcare professional’s skill in successfully managing complex and stressful situations []. In this sense, there is ample evidence in the literature to suggest simulation is effective at increasing this competency []. Specifically, single-group pre-test and post-test design studies have reported increases in self-efficacy after simulation sessions using standardized patients [,,]. However, the effect sizes of simulation in self-efficacy reported by these studies are inconsistent and range from low to large. In contrast, we reported a large effect size in this humanization competence using not only standardized patients but also virtual simulation sessions.
Logically, simulated nursing video consultations mainly promote the development of non-technical skills (mainly communication skills, active listening, presence, empathy, and teamwork) [,]. In this sense, humanization of care and its related competencies could be included in these skills required to provide quality nursing care and decrease burnout []. However, while face-to-face simulation sessions usually improve technical skill performance [,,], more studies are needed to analyze non-technical skill performance using virtual simulation modalities [].
Lastly, although simulated nursing video consultations are not included among virtual simulation modalities in the evidence [,], this methodology could be considered as another choice for virtual simulation, according to their high level of fidelity in compliance with the requirements proposed by the INACSL Standards of Best Practice and the high satisfaction and positive perception expressed by nursing students in previous studies [,]. However, Cant et al. [] consider clarification of the nomenclature of virtual simulation to be needed in terms of fidelity, since interactions between learners and virtual patients are different from face-to-face simulation experiences. Additionally, its use could be extended to other contexts, not only in the confinement due to the COVID-19 pandemic.
The main limitation of our study is related to the specific disadvantage of both simulated and real-life nursing video consultations: technical issues. Ensuring adequate network access and the correct functioning of virtual platforms could mitigate these potential problems [,]. Regarding methodological limitations, although our sample size was small, the response rate was high. Additionally, while our study did not analyze either self-efficacy or empathy using the specific validated scales, a validated scale that comprised both humanization competencies was utilized []. In this sense, the use of validated scales for evaluating these competencies is not consistent in the majority of the studies [,]. Finally, the positive effects of virtual simulation-based training on developing and cultivating humanization competencies should be confirmed by future research, so more studies are needed. These future studies should extend the sample recruited and compare it with a control group, using quasi-experimental or experimental designs and evaluating the outcomes obtained in follow-up periods (for instance, 3, 6 and/or 12 months later). Additionally, future research should also assess the acquisition of humanization of care competencies by nursing students or registered nurses using this virtual simulation modality and extend it to other settings and education centers.
5. Conclusions
This methodology allows nurses to be trained in the humanization of care using a virtual simulation format, in the form of simulated nursing video consultations by performing high-fidelity simulation sessions that comply with the requirements proposed by the INACSL Standards of Best Practice. Therefore, this methodology could be considered as another choice for virtual simulation. Additionally, this virtual modality allows the collaboration of standardized patients and, consequently, could be a way to humanize virtual simulation. Our results could be confirmed by future research projects using quasi-experimental or experimental designs and follow-up periods, recruiting more nursing students, including registered nurses, and extending this virtual simulation modality to other settings and education centers.
Author Contributions
Conceptualization, D.J.-R., M.d.M.M.J., M.d.C.P.-F. and O.A.; methodology, D.J.-R., M.d.M.M.J., M.d.C.P.-F. and O.A.; formal analysis, D.J.-R., M.d.M.M.J., M.d.C.P.-F. and O.A.; investigation, D.J.-R. and O.A.; data curation, D.J.-R., M.d.M.M.J., M.d.C.P.-F. and O.A.; writing—original draft preparation, D.J.-R., M.d.M.M.J., M.d.C.P.-F., M.P.-H. and O.A.; writing—review and editing, D.J.-R., M.P.-H. and O.A.; supervision, D.J.-R. and O.A.; project administration, D.J.-R., M.P.-H. and O.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Research and Ethics Board of the Department of Nursing, Physiotherapy, and Medicine of the A. University (Approval no. EFM-75/2020).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Harder, N. Simulation amid the COVID-19 pandemic. Clin. Simul. Nurs. 2020, 43, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Bogossian, F.; Cooper, S.; Kelly, M.; Levett-Jones, T.; McKenna, L.; Slark, J.; Seaton, P. Best practice in clinical simulation education—Are we there yet? A cross-sectional survey of simulation in Australian and New Zealand pre-registration nursing education. Clin. Simul. Nurs. 2018, 25, 327–334. [Google Scholar] [CrossRef]
- Cant, R.; Cooper, S.; Sussex, R.; Bogossian, F. What’s in a name? Clarifying the nomenclature of virtual simulation. Clin. Simul. Nurs. 2017, 27, 26–30. [Google Scholar] [CrossRef]
- Lioce, L.; Lopreiato, J.; Downing, D.; Chang, T.P.; Robertson, J.M.; Anderson, M.; Diaz, D.A.; Spain, A.E.; Terminology and Concepts Working Group. Healthcare Simulation Dictionary, 2nd ed.; Lioce, L., Lopreiato, J., Downing, D., Chang, T.P., Robertson, J.M., Anderson, M., Diaz, D.A., Spain, A.E., Eds.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2020. [CrossRef]
- Jiménez-Rodríguez, D.; Arrogante, O. Simulated video consultations as a learning tool in undergraduate nursing: Students’ perceptions. Healthcare 2020, 8, 280. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Rodríguez, D.; Torres Navarro, M.D.M.; Plaza Del Pino, F.J.; Arrogante, O. Simulated nursing video consultations: An innovative proposal during COVID-19 confinement. Clin. Simul. Nurs. 2020, 48, 29–37. [Google Scholar] [CrossRef]
- Contreras, C.M.; Metzger, G.A.; Beane, J.D.; Dedhia, P.H.; Ejaz, A.; Pawlik, T.M. Telemedicine: Patient-provider clinical engagement during the COVID-19 pandemic and beyond. J. Gastrointes. Surg. 2020, 24, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Hong, Y.R.; Lawrence, J.; Williams, D., Jr.; Mainous, A., III. Population-level interest and telehealth capacity of us hospitals in response to COVID-19: Cross-sectional analysis of google search and national hospital survey data. JMIR Public Health Surveill. 2020, 6, e18961. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Wherton, J.; Shaw, S.; Morrison, C. Video consultations for COVID-19. BMJ 2020, 368, m998. [Google Scholar] [CrossRef] [Green Version]
- Ohannessian, R.; Duong, T.A.; Odone, A. Global telemedicine implementation and integration within health systems to fight the COVID-19 pandemic: A Call to Action. JMIR Public Health Surveill. 2020, 6, e18810. [Google Scholar] [CrossRef]
- de la Torre-Diez, I.; López-Coronado, M.; Vaca, C.; Sáez Aguado, J.; de Castro, C. Cost-utility and cost-effectiveness studies of telemedicine, electronic, and mobile health systems in the literature: A systematic review. Telemed. J. E Health 2015, 21, 81–85. [Google Scholar] [CrossRef] [Green Version]
- Ignatowicz, A.; Atherton, H.; Bernstein, C.J.; Bryce, C.; Court, R.; Sturt, J.; Griffiths, F. Internet videoconferencing for patient-clinician consultations in long-term conditions: A review of reviews and applications in line with guidelines and recommendations. Digit. Health 2019, 5, 2055207619845831. [Google Scholar] [CrossRef] [Green Version]
- Gaba, D.M. The future vision of simulation in health care. Qual. Saf. Health Care 2004, 13, i2–i10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tarnow, K.G. Humanizing the learning laboratory. J. Nurs. Educ. 2005, 44, 43–44. [Google Scholar] [CrossRef]
- Cohen, B.S.; Boni, R. Holistic nursing simulation: A concept analysis. J. Holist. Nurs. 2018, 36, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Busch, I.M.; Moretti, F.; Travaini, G.; Wu, A.W.; Rimondini, M. Humanization of care: Key elements identified by patients, caregivers, and healthcare providers. A systematic review. Patient 2019, 12, 461–474. [Google Scholar] [CrossRef] [PubMed]
- Heras, G.; Oviés, Á.A.; Gómez, V. A plan for improving the humanisation of intensive care units. Intensive Care Med. 2017, 43, 547–549. [Google Scholar] [CrossRef] [PubMed]
- Pérez-Fuentes, M.C.; Herrera-Peco, I.; Molero, M.M.; Oropesa, N.F.; Ayuso-Murillo, D.; Gázquez, J.J. The development and validation of the healthcare professional humanization scale (HUMAS) for nursing. Int. J. Environ. Res. Public Health 2019, 16, 3999. [Google Scholar] [CrossRef] [Green Version]
- Cant, R.P.; Cooper, S.J. Use of simulation-based learning in undergraduate nurse education: An umbrella systematic review. Nurse Educ. Today 2017, 49, 63–71. [Google Scholar] [CrossRef]
- Levett-Jones, T.; Cant, R.; Lapkin, S. A systematic review of the effectiveness of empathy education for undergraduate nursing students. Nurse Educ. Today 2019, 75, 80–94. [Google Scholar] [CrossRef] [Green Version]
- INACSL Standards Committee. INACSL standards of best practice: SimulationSM Simulation design. Clin. Simul. Nurs. 2016, 12, 5–12. [Google Scholar] [CrossRef] [Green Version]
- INACSL Standards Committee. INACSL standards of best practice: SimulationSM Facilitation. Clin. Simul. Nurs. 2016, 12, 16–20. [Google Scholar] [CrossRef] [Green Version]
- INACSL Standards Committee. INACSL standards of best practice: SimulationSM Simulation glossary. Clin. Simul. Nurs. 2016, 12, 39–47. [Google Scholar] [CrossRef]
- INACSL Standards Committee. INACSL standards of best practice: SimulationSM Debriefing. Clin. Simul. Nurs. 2016, 12, 21–25. [Google Scholar] [CrossRef] [Green Version]
- Lewis, K.L.; Bohnert, C.A.; Gammon, W.L.; Hölzer, H.; Lyman, L.; Smith, C.; Thompson, T.M.; Wallace, A.; Gliva-McConvey, G. The Association of Standardized Patient Educators (ASPE) Standards of Best Practice (SOBP). Adv. Simul. 2017, 2, 1–8. [Google Scholar] [CrossRef]
- McDonald, R.P. Test Theory: A Unified Approach; Lawrence Erlbaum Associates: Mahwah, NJ, USA, 1999. [Google Scholar]
- Coolican, H. Research Methods and Statistics in Psychology, 5th ed.; Hodder Education Group: London, UK, 2009. [Google Scholar]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Li, X.; Gu, L.; Zhang, R.; Zhao, R.; Cai, Q.; Lu, Y.; Wang, H.; Meng, Q.; Wei, H. Effects of simulation-based deliberate practice on nursing students’ communication, empathy, and self-efficacy. J. Nurs. Educ. 2019, 58, 681–689. [Google Scholar] [CrossRef] [PubMed]
- Ward, J. The empathy enigma: Does it still exist? Comparison of empathy using students and standardized actors. Nurse Educ. 2016, 41, 134–138. [Google Scholar] [CrossRef]
- Hojat, M.; Louis, D.Z.; Maio, V.; Gonnella, J.S. Empathy and health care quality. Am. J. Med. Qual. 2013, 28, 6–7. [Google Scholar] [CrossRef]
- Trzeciak, S.; Roberts, B.W.; Mazzarelli, A.J. Compassionomics: Hypothesis and experimental approach. Med. Hypotheses 2017, 107, 92–97. [Google Scholar] [CrossRef]
- Bas-Sarmiento, P.; Fernández-Gutiérrez, M.; Baena-Baños, M.; Romero-Sánchez, J.M. Efficacy of empathy training in nursing students: A quasi-experimental study. Nurse Educ. Today 2017, 59, 59–65. [Google Scholar] [CrossRef]
- Strekalova, Y.A.; Krieger, J.L.; Kleinheksel, A.J.; Kotranza, A. Empathic communication in virtual education for nursing students: I’m sorry to hear that. Nurse Educ. 2017, 42, 18–22. [Google Scholar] [CrossRef] [Green Version]
- Bandura, A. Self-Efficacy: The Exercise of Control; W.H. Freeman and Company: New York, NY, USA, 1997. [Google Scholar]
- Orgambídez, A.; Borrego, Y.; Vázquez-Aguado, O. Self-efficacy and organizational commitment among Spanish nurses: The role of work engagement. Int. Nurs. Rev. 2019, 66, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Foronda, C.; Liu, S.; Bauman, E.B. Evaluation of simulation in undergraduate nurse education: An integrative review. Clin. Simul. Nurs. 2013, 9, e409–e416. [Google Scholar] [CrossRef]
- Franklin, A.E.; Lee, C.S. Effectiveness of simulation for improvement in self-efficacy among novice nurses: A meta-analysis. J. Nurs. Educ. 2014, 53, 607–614. [Google Scholar] [CrossRef] [PubMed]
- Oh, P.J.; Jeon, K.D.; Koh, M.S. The effects of simulation-based learning using standardized patients in nursing students: A meta-analysis. Nurse Educ. Today 2015, 35, e6–e15. [Google Scholar] [CrossRef]
- Pérez-Fuentes, M.C.; Molero, M.M.; Gázquez, J.J.; Simón, M.M. Analysis of Burnout Predictors in Nursing: Risk and Protective Psychological Factors. Eur. J. Psychol. Appl. Leg. Context 2019, 11, 33–40. [Google Scholar] [CrossRef] [Green Version]
- Bracq, M.S.; Michinov, E.; Jannin, P. Virtual Reality Simulation in Nontechnical Skills Training for Healthcare Professionals: A Systematic Review. Simul. Healthc. 2019, 14, 188–194. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).