How Does Health Literacy Modify Indicators of Health Behaviour and of Health? A Longitudinal Study with Trainees in North Germany †
Abstract
:1. Introduction
1.1. Definition of Health Literacy (HL)
1.2. Prevalence of Limited HL, Determinants and Associated Outcomes
1.3. Target Group
1.4. Research Question
- (i)
- Trainees with high initial HL at T0 exhibit in a longitudinal section better health behaviour at T1 (alcohol consumption, smoking, nutrition, exercise) than trainees with low initial HL.
- (ii)
- In a longitudinal section, trainees with high initial HL at T0 exhibit better health at T1 (BMI, subjective health status, psychological well-being) than trainees with low initial HL.
2. Materials and Methods
2.1. Study Design and Cohort
- Health: geriatric nurses, medical nurses, medical assistants;
- Cosmetics: hairdressers;
- Education: educators;
- Engineering: plant mechanics for plumbing, heating and air conditioning, electricians for plant and building technology;
- Office: office management assistants, wholesale and export sales managers, industrial sales manager;
- Retail sales: retail sales manager.
2.2. Survey Instrument
2.2.1. Health Literacy
2.2.2. Health Status
2.2.3. Health Behaviour
- Sporting activity yes (1): 2–<4 h per week/> = 4 h per week, no (0): none/<1 h per week/1–<2 h per week
- Nutrition favourable pattern (1): normal/optimal pattern, unfavourable (0): unfavourable pattern
- Fast Food: no (1): <= once/week, yes (0): >once/week
- Smoking no (1), yes (0)
- Risky alcohol consumption no (1), yes (0)
2.3. Statistical Analysis
3. Results
3.1. Description of the Study Cohort
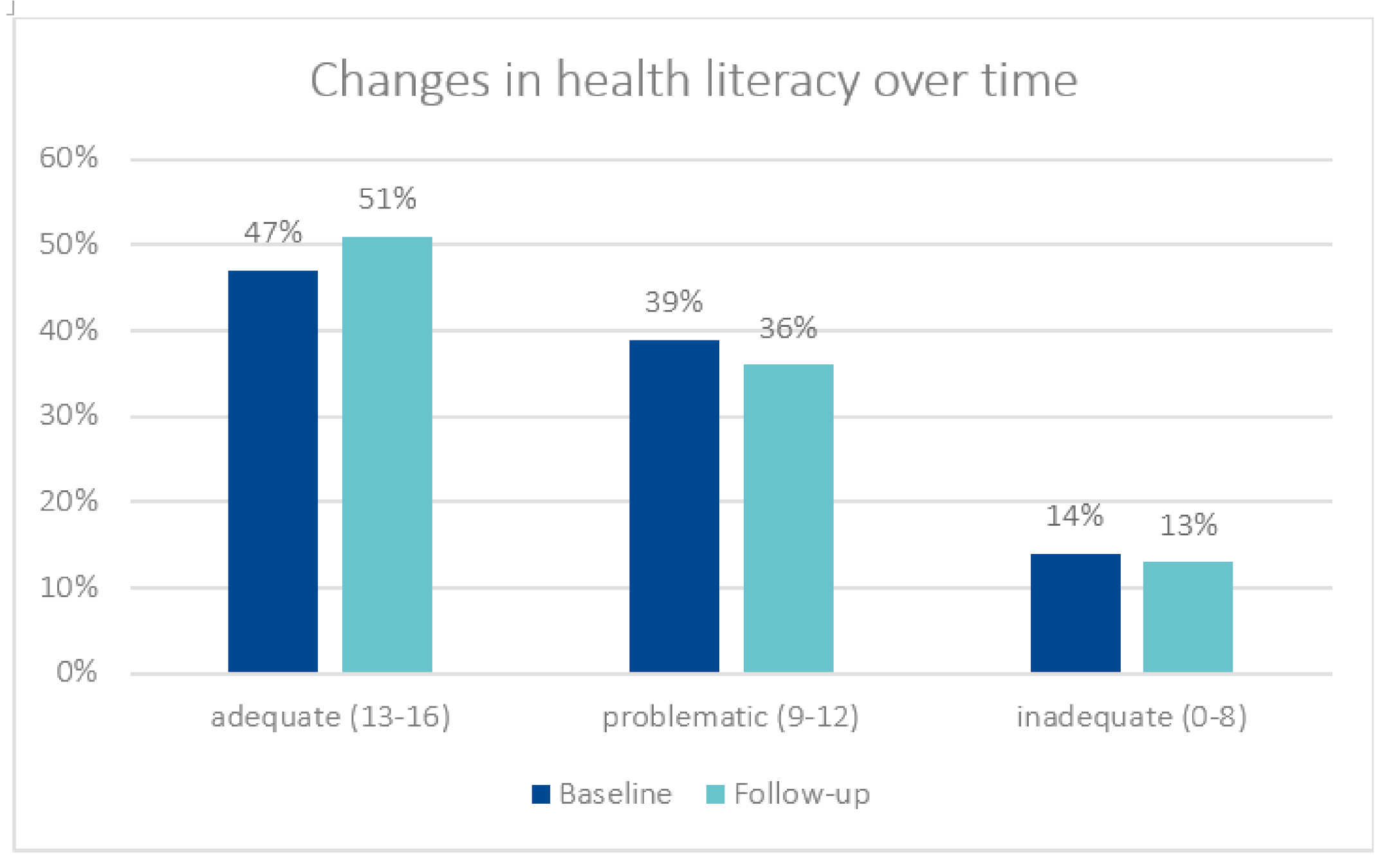
3.2. Health Literacy
3.3. Health Behaviour and Health Status
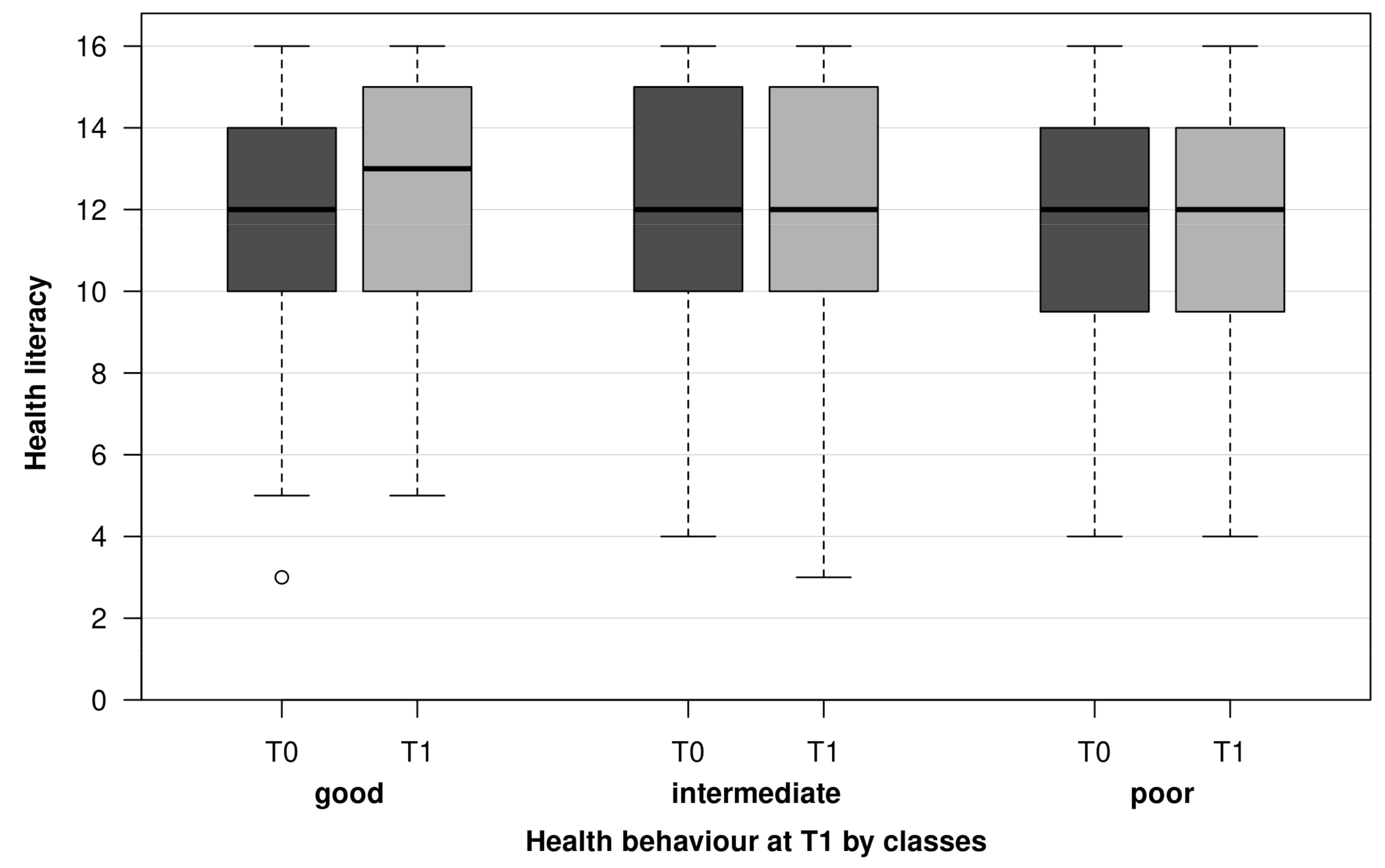
3.4. Associations of Health and Health Behaviour with HL
4. Discussion
4.1. HL and Demographic Parameters
4.2. HL and Health Education
4.3. HL and Health Outcomes
4.4. HL and Health Behaviour
4.5. Prevention
4.6. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Federal Center for Health Education (BZgA). Health Literacy/Gesundheitskompetenz. Available online: https://www.leitbegriffe.bzga.de/alphabetisches-verzeichnis/health-literacy-gesundheitskompetenz/ (accessed on 20 November 2021).
- Jakab, Z.; Tsouros, A.D. Health 2020—Achieving health and development in today’s Europe. Maced. J. Med. Sci. 2014, 7, 499–505. [Google Scholar] [CrossRef] [Green Version]
- Schaeffer, D.; Hurrelmann, K.; Bauer, U.; Kolpatzik, K. Nationaler Aktionsplan Gesundheitskompetenz. In Die Gesundheitskompetenz in Deutschland Stärken; KomPart: Berlin, Germany, 2018. [Google Scholar]
- Sørensen, K.; Van den Broucke, S.; Fullam, J.; Doyle, G.; Pelikan, J.; Slonska, Z.; Brand, H.; (HLS-EU) Consortium Health Literacy Project European. Health literacy and public health: A systematic review and integration of definitions and models. BMC Public Health 2012, 12, 80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bitzer, E.M.; Sørensen, K. Gesundheitskompetenz—Health Literacy. Das Gesundh. 2018, 80, 754–766. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Health Literacy: The Solid Facts; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2013; ISBN 978-92-890-00154. Available online: https://apps.who.int/iris/handle/10665/326432 (accessed on 20 November 2021).
- Sørensen, K.; Pelikan, J.M.; Röthlin, F.; Ganahl, K.; Slonska, Z.; Doyle, G.; Fullam, J.; Kondilis, B.; Agrafiotis, D.; Uiters, E.; et al. Health literacy in Europe: Comparative results of the European health literacy survey (HLS-EU). Eur. J. Public Health 2015, 25, 1053–1058. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schaeffer, D.; Berens, E.-M.; Vogt, D. Gesundheitskompetenz der Bevölkerung in Deutschland. Dtsch. Ärztebl. 2017, 114, 53–60. [Google Scholar]
- Schaeffer, D.; Berens, E.-M.; Gille, S.; Griese, L.; Klinger, J.; de Sombre, S.; Vogt, D.; Hurrelmann, K. Gesundheitskompetenz der Bevölkerung in Deutschland vor und während der Corona Pandemie: Ergebnisse des HLS-GER 2; Universität Bielefeld: Bielefeld, Germany, 2021. [Google Scholar]
- Adam, Y.; Carol, S. Gesundheitskompetenz von Menschen mit Migrationshintergrund: Perspektive und Erfahrungen von Türkisch-und Russischsprachigen Frauen; Universität Bielefeld: Bielefeld, Germany, 2020. [Google Scholar]
- Protheroe, J.; Whittle, R.; Bartlam, B.; Estacio, E.V.; Clark, L.; Kurth, J. Health literacy, associated lifestyle and demographic factors in adult population of an English city: A cross-sectional survey. Health Expect. 2017, 20, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Wernly, B.; Wernly, S.; Magnano, A.; Paul, E. Cardiovascular health care and health literacy among immigrants in Europe: A review of challenges and opportunities during the COVID-19 pandemic. Z. Gesundh. Wiss 2020, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Berens, E.-M.; Vogt, D.; Messer, M.; Hurrelmann, K.; Schaeffer, D. Health literacy among different age groups in Germany: Results of a cross-sectional survey. BMC Public Health 2016, 16, 1151. [Google Scholar] [CrossRef] [Green Version]
- Berkman, N.D.; Sheridan, S.L.; Donahue, K.E.; Halpern, D.J.; Crotty, K. Low health literacy and health outcomes: An updated systematic review. Ann. Intern. Med. 2011, 155, 97–107. [Google Scholar] [CrossRef]
- Bjørnsen, H.N.; Espnes, G.A.; Eilertsen, M.-E.B.; Ringdal, R.; Moksnes, U.K. The relationship between positive mental health literacy and mental well-being among adolescents: Implications for school health services. J. Sch. Nurs. 2019, 35, 107–116. [Google Scholar] [CrossRef] [Green Version]
- Boren, S.A. A review of health literacy and diabetes: Opportunities for technology. J. Diabetes Sci. Technol. 2009, 3, 202–209. [Google Scholar] [CrossRef] [Green Version]
- Sanders, L.M.; Federico, S.; Klass, P.; Abrams, M.A.; Dreyer, B. Literacy and child health: A systematic review. Arch. Pediatr. Adolesc. Med. 2009, 163, 131–140. [Google Scholar] [CrossRef] [Green Version]
- Stormacq, C.; Wosinski, J.; Boillat, E.; Van den Broucke, S. Effects of health literacy interventions on health-related outcomes in socioeconomically disadvantaged adults living in the community: A systematic review. JBI Evid Synth. 2020, 18, 1389–1469. [Google Scholar] [CrossRef]
- Zhang, F.; Or, P.P.L.; Chung, J.W.Y. How different health literacy dimensions influences health and well-being among men and women: The mediating role of health behaviours. Health Expect 2021, 24, 617–627. [Google Scholar] [CrossRef]
- Fleary, S.A.; Joseph, P.; Pappagianopoulos, J.E. Adolescent health literacy and health behaviors: A systematic review. J. Adolesc. 2018, 62, 116–127. [Google Scholar] [CrossRef]
- Mayberry, L.S.; Schildcrout, J.S.; Wallston, K.A.; Goggins, K.; Mixon, A.S.; Rothman, R.L.; Kripalani, S.; Bachmann, J.; Bell, S.P.; Donato, K.M.; et al. Health literacy and 1-year mortality: Mechanisms of association in adults hospitalized for cardiovascular disease. In Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2018. [Google Scholar]
- Sansom-Daly, U.M.; Lin, M.; Robertson, E.; Wakefield, C.E.; McGill, B.C.; Girgis, A.; Cohn, R. Health Literacy in Adolescents and Young Adults: An Updated Review. J. Adolesc. Young Adult Oncol. 2016, 5, 106–118. [Google Scholar] [CrossRef]
- Walters, R.; Leslie, S.J.; Polson, R.; Cusack, T.; Gorely, T. Establishing the efficacy of interventions to improve health literacy and health behaviours: A systematic review. BMC Public Health 2020, 20, 1–17. [Google Scholar] [CrossRef]
- Federal Institute for Vocational Education and Training (Publisher). Datenreport zum Berufsbildungsbericht 2019. Informationen und Analysen zur Entwicklung der beruflichen Bildung, 1st ed.; Bundesinstitut für Berufsbildung: Bonn, Germany, 2019; ISBN 978-3-96208-128-7. Available online: https://www.bibb.de/dokumente/pdf/bibb_datenreport_2019.pdf (accessed on 20 November 2021).
- Pinquart, M.; Silbereisen, R. Gesundheitsverhalten im Kindes-und Jugendalter. Bundesgesundheitsbl.-Gesundh.-Gesundh. 2002, 45, 873–878. [Google Scholar] [CrossRef]
- Kaminski, A.; Nauerth, A.; Pfefferle, P.I. Gesundheitszustand und Gesundheitsverhalten von Auszubildenden im ersten Lehrjahr—Erste Ergebnisse einer Befragung in Bielefelder Berufskollegs. Gesundheitswesen 2008, 70, 38–46. [Google Scholar] [CrossRef]
- Badura, B.; Ducki, A.; Schröder, H.; Klose, J.; Meyer, M. Fehlzeiten—Report 2015: Neue Wege für mehr Gesundheit-Qualitätsstandards für ein Zielgruppenspezifisches Gesundheitsmanagement; Springer: Berlin/Heidelberg, Germany, 2015. [Google Scholar]
- Reick, S.; Hering, T. Gesundheitskompetenz Studierender—Ergebnisse einer Online-Befragung an der Hochschule für Gesundheit Bochum. Int. J. Health Prof. 2018, 5, 44–52. [Google Scholar]
- Steinke, S.; Koch, P.; Lietz, J.; Schillmöller, Z.; Nienhaus, A. Health Literacy, Health Behavior and States of Health among Trainee Personnel in Northern Germany. Healthcare 2021, 9, 757. [Google Scholar] [CrossRef]
- Röthlin, F.; Pelikan, J.; Ganahl, K. Die Gesundheitskompetenz der 15-Jährigen Jugendlichen in Österreich; Ludwig Boltzmann Institut Health Promotion Research (LBIHPR): Wien, Austria, 2013; Available online: https://oepgk.at/wp-content/uploads/2020/02/bericht_die_gesundheitskompetenz_von_15-jaehrigen_jugendlich.pdf (accessed on 20 November 2021).
- Hasselhorn, H.-M.; Freude, G. Der Work-ability-Index: Ein Leitfaden; Bundesanstalt für Arbeitsschutz und Arbeitsmedizin; Wirtschaftsverlag NW: Bremerhaven, Germany, 2007; ISBN 978-3-86509-702-6. [Google Scholar]
- Brähler, E.; Mühlan, H.; Albani, C.; Schmidt, S. Teststatistische prüfung und normierung der deutschen versionen des EUROHIS-QOL lebensqualität-Index und des WHO-5 wohlbefindens-index. Diagnostica 2007, 53, 83–96. [Google Scholar] [CrossRef]
- Krug, S.; Jordan, S.; Mensink, G.B.; Müters, S.; Finger, J.; Lampert, T. Körperliche Aktivität. Bundesgesundheitsbl.-Gesundh.-Gesundh. 2013, 56, 765–771. [Google Scholar] [CrossRef]
- Bush, K.; Kivlahan, D.R.; McDonell, M.B.; Fihn, S.D.; Bradley, K.A.; Project, A.C.Q.I. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Arch. Intern. Med. 1998, 158, 1789–1795. [Google Scholar] [CrossRef] [Green Version]
- Lampert, T.; Von Der Lippe, E.; Müters, S. Verbreitung des Rauchens in der Erwachsenenbevölkerung in Deutschland. Bundesgesundheitsbl.-Gesundh.-Gesundh. 2013, 56, 802–808. [Google Scholar] [CrossRef] [Green Version]
- Winkler, G.; Döring, A. Validation of a short qualitative food frequency list used in several German large scale surveys. Z. Für Ernährungswiss. 1998, 37, 234–241. [Google Scholar] [CrossRef]
- Schultes, K. Gesundheitskompetenz, subjektive Gesundheit und Gesundheitsverhalten bei Studierenden. Public Health Forum 2017, 25, 84–86. [Google Scholar] [CrossRef]
- Sukys, S.; Cesnaitiene, V.J.; Ossowsky, Z.M. Is health education at university associated with students’ health literacy? Evidence from cross-sectional study applying HLS-EU-Q. BioMed Res. Int. 2017, 2017, 8516843. [Google Scholar] [CrossRef]
- Klinker, C.D.; Aaby, A.; Ringgaard, L.W.; Hjort, A.V.; Hawkins, M.; Maindal, H.T. Health literacy is associated with health behaviors in students from vocational education and training schools: A Danish population-based survey. Int. J. Environ. Res. Public Health 2020, 17, 671. [Google Scholar] [CrossRef] [Green Version]
- Amoah, P.A. Social participation, health literacy, and health and well-being: A cross-sectional study in Ghana. SSM Popul. Health 2018, 4, 263–270. [Google Scholar] [CrossRef]
- Fiedler, S.; Pfaff, H.; Soellner, R.; Pförtner, T.K. Exploring the Association Between Health Literacy and Psychological Well-Being Among Industry Managers in Germany. J. Occup. Environ. Med. 2018, 60, 743–753. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.C. Health literacy, self-reported status and health promoting behaviours for adolescents in Taiwan. J. Clin. Nurs. 2011, 20, 190–196. [Google Scholar] [CrossRef] [PubMed]
- Quenzel, G.; Schaeffer, D.; Messer, M.; Vogt, D. Gesundheitskompetenz bildungsferner Jugendlicher. Bundesgesundheitsbl.-Gesundh.-Gesundh. 2015, 58, 951–957. [Google Scholar] [CrossRef] [PubMed]
- Domanska, O.; Firnges, C.; Jordan, S. Verstehen Jugendliche die Items des „Europäischen Health Literacy Survey Questionnaire“ (HLS-EU-Q47)? Ergebnisse kognitiver Interviews im Rahmen des Projektes „Messung der Gesundheitskompetenz bei Jugendlichen“ (MOHLAA). Das Gesundh. 2016, 78, A200. [Google Scholar] [CrossRef]
- Okan, O. Gesundheitskompetenz im Kindes- und Jugendalter: Bestandsaufnahme und Analyse der Konzeptionellen und Methodischen Erforschung. 2019. Unviversity of Bielefeld, Germany. Available online: https://pub.uni-bielefeld.de/record/2941647 (accessed on 20 November 2021).
- Hart, L.M.; Mason, R.J.; Kelly, C.M.; Cvetkovski, S.; Jorm, A.F. ‘teen Mental Health First Aid’: A description of the program and an initial evaluation. Int. J. Ment. Health Syst. 2016, 10, 3. [Google Scholar] [CrossRef] [Green Version]
- Perry, Y.; Petrie, K.; Buckley, H.; Cavanagh, L.; Clarke, D.; Winslade, M.; Hadzi-Pavlovic, D.; Manicavasagar, V.; Christensen, H. Effects of a classroom-based educational resource on adolescent mental health literacy: A cluster randomised controlled trial. J. Adolesc. 2014, 37, 1143–1151. [Google Scholar] [CrossRef]
| Female 309 (79%) | Male 82 (21%) | Total 391 (100%) | p | |
|---|---|---|---|---|
| Age in years (baseline) | ||||
| (SD) | 21.2 (5.4) | 21.0 (3.8) | 21.2 (5.1) | 0.328 1 |
| Range | 16–53 | 13–36 | 16–53 | |
| Nationality | ||||
| German | 290 (79%) | 76 (21%) | 366 (95%) | 0.934 2 |
| Other | 16 (80%) | 4 (20%) | 20 (5%) | |
| n missing | 3 | 2 | 5 | |
| School leaving exam | ||||
| Lower secondary school (Hauptschule) | 13 (62%) | 8 (38%) | 21 (5%) | 0.069 2 |
| Higher secondary school (Realschule) | 150 (82%) | 32 (18%) | 182 (47%) | |
| Vocational training college (Fachhochschule) | 62 (83%) | 13 (17%) | 75 (19%) | |
| A-Levels (Abitur) | 84 (74%) | 29 (26%) | 113 (29%) | |
| Branch | ||||
| Office | 76 (63%) | 45 (37%) | 121 (31%) | <0.001 2 |
| Retail | 21 (70%) | 9 (30%) | 30 (8%) | |
| Education | 43 (92%) | 4 (8%) | 47 (12%) | |
| Nursing/Medical assistants | 158 (95%) | 9 (5%) | 167 (42%) | |
| Engineering | 0 (0%) | 14 (100%) | 14 (4%) | |
| Hairdressers | 11 (95%) | 1 (8%) | 12 (3%) | |
| Federal State/Vocational training college | ||||
| Lower Saxony | 238 (80%) | 59 (20%) | 297 (76%) | 0.275 2 |
| Mecklenburg-Western Pomerania | 14 (87%) | 2 (13%) | 16 (4%) | |
| Schleswig-Holstein | 57 (73%) | 21 (27%) | 78 (20%) | |
| Bremen | 0 (0%) | 0 (0%) | 0 (0%) | |
| Demographic Variables | Category (n) | p * | |
|---|---|---|---|
| Gender | female (309) | 11.9 (3.0) | 0.865 |
| male (82) | 11.9 (3.0) | ||
| Age group (years) | 16–18 (102) | 12.4 (2.9) | 0.093 |
| 19–20 (145) | 12.0 (2.9) | ||
| 21–25 (98) | 11.5 (3.1) | ||
| ≥26 (44) | 11.4 (3.1) | ||
| Nationality | German (366) | 11.9 (3.0) | 0.790 |
| Other (20) | 12.1 (3.4) | ||
| School Leaving Exam | Lower secondary school (Hauptschule) (21) | 10.9 (3.6) | 0.304 |
| Higher secondary school exam (Realschule) (182) | 11.9 (3.0) | ||
| Vocational training college leaving exam (Fachhochschule) (75) | 11.8 (3.1) | ||
| A-Levels (Abitur) (113) | 12.2 (2.7) |
| Variable | Group | Baseline (SD) n (%) | Follow-Up (SD) n (%) | p | Trend | |
|---|---|---|---|---|---|---|
| Health literacy (Score 0–16) | Total | 11.9 (2.9) | 12,2 (2.9) | 0.070 2 | ||
| Nursing/ MFA | 12.1 (2.8) | 12.5 (2.9) | 0.019 2 | ↑ | ||
| Unfavourable nutrition | Total | 188 (49%) | 184 (48%) | 0.696 1 | ||
| Fast food | Total | 60 (15%) | 56 (14%) | 0.708 1 | ||
| Smoking | Total | 117 (30%) | 116 (30%) | 0.885 1 | ||
| Lack of exercise (<2 h exercise/week) | Total | 249 (64%) | 240 (62%) | 0.542 1 | ||
| Risky alcohol consumption | Total | 175 (46%) | 156 (41%) | 0.073 1 | ||
| Women | 133 (44%) | 113 (37%) | 0.024 1 | ↓ | ||
| BMI | Total | 23.9 (5.1) | 24,3 (4.9) | 0.033 1 | ↑ | |
| Hairdressers | 24.4 (5.8) | 25.9 (7.0) | 0.014 1 | ↑ | ||
| Office | 23.5 (4.5) | 24.0 (4.9) | 0.020 1 | ↑ | ||
| Subjective health status (poor/less good) | Total | 59 (15%) | 56 (14%) | 0.804 1 | ||
| Medically diagnosed diseases | Musculoskeletal disease (MSD) | Total | 79 (21%) | 69 (18%) | 1.000 1 | |
| Skin | Total | 84 (22%) | 54 (14%) | 0.002 1 | ↓ | |
| Office | 30 (25%) | 12 (10%) | 0.002 1 | ↓ | ||
| Women | 69 (26%) | 46 (15%) | 0.011 1 | ↓ | ||
| Respiratory tract | Total | 83 (21%) | 74 (19%) | 0.306 1 | ||
| Psyche | Total | 40 (10%) | 34 (9%) | 0.361 1 | ||
| Neurological | Total | 60 (16%) | 55 (14%) | 0.519 1 | ||
| Digestive system | Total | 32 (8%) | 41 (11%) | 0.203 1 | ||
| Hormonal | Total | 38 (10%) | 54 (14%) | 0.008 1 | ↑ | |
| Nursing/ Medical Assistant | 15 (9%) | 30 (18%) | 0.001 1 | ↑ | ||
| Women | 35 (11%) | 48 (16%) | 0.021 1 | ↑ | ||
| Cardiovascular | Total | 18 (5%) | 22 (6%) | 0.523 1 | ||
| Psychological well-being (Score 0–25) | Total | 13.4 (4.6) | 13.7 (4.5) | 0.263 3 | ||
| Branch | HL T0 (SD) | HL T1 (SD) | Δ HL T1–T0 |
|---|---|---|---|
| Office | 11.9 (3.2) | 11.9 (3.1) | 0.06 |
| Retail | 10.9 (3.4) | 10.9 (3.3) | 0.04 |
| Education | 12.0 (2.8) | 12.3 (2.4) | 0.30 |
| Nursing/Medical assistant | 12.1 (2.8) | 12.5 (2.9) | 0.47 * |
| Engineering | 12.4 (2.8) | 12.4 (3.2) | 0.01 |
| Hairdressing | 11.8 (3.8) | 12.6 (3.3) | 0.75 |
| Outcome: Psychological Well-Being (n = 365) | ||
|---|---|---|
| Outcome: Lower Psychological Well-Being (Score < 37%) | ||
| Missing Data: 6%, r2: 8%, Hosmer-Lemeshow Goodness-of-Fit Test: p = 0.771 | ||
| OR * (95% CI) | p | |
| HL adequate | 1 | - |
| HL problematic | 2.1 (1.30–3.38) | 0.002 |
| HL inadequate | 3.3 (1.70–6.32) | <0.001 |
| Gender: female vs. male | 1.9 (1.06–3.35) | 0.032 |
| Outcome: Subjective Health Status (n = 362) | ||
|---|---|---|
| Outcome: Poor/Less Good (15%) | ||
| Missing Data: 7%, r2: 9%, Hosmer-Lemeshow-Goodness-of-Fit Test: p = 0.923 | ||
| OR * (95% CI) | p | |
| HL adequate | 1 | - |
| HL problematic | 1.6 (0.84–3.22) | 0.147 |
| HL inadequate | 2.8 (1.23–6.33) | 0.014 |
| Health behaviour good | 1 | - |
| Health behaviour moderate | 2.2 (1.11–4.44) | 0.023 |
| Health behaviour poor | 4.0 (1.51–10.48) | 0.005 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koch, P.; Schillmöller, Z.; Nienhaus, A. How Does Health Literacy Modify Indicators of Health Behaviour and of Health? A Longitudinal Study with Trainees in North Germany. Healthcare 2022, 10, 2. https://doi.org/10.3390/healthcare10010002
Koch P, Schillmöller Z, Nienhaus A. How Does Health Literacy Modify Indicators of Health Behaviour and of Health? A Longitudinal Study with Trainees in North Germany. Healthcare. 2022; 10(1):2. https://doi.org/10.3390/healthcare10010002
Chicago/Turabian StyleKoch, Peter, Zita Schillmöller, and Albert Nienhaus. 2022. "How Does Health Literacy Modify Indicators of Health Behaviour and of Health? A Longitudinal Study with Trainees in North Germany" Healthcare 10, no. 1: 2. https://doi.org/10.3390/healthcare10010002
APA StyleKoch, P., Schillmöller, Z., & Nienhaus, A. (2022). How Does Health Literacy Modify Indicators of Health Behaviour and of Health? A Longitudinal Study with Trainees in North Germany. Healthcare, 10(1), 2. https://doi.org/10.3390/healthcare10010002







