The Caregiver Support Ratio in Europe: Estimating the Future of Potentially (Un)Available Caregivers
Abstract
:1. Introduction
2. Materials and Methods
Sample and Procedures
3. Results
4. Discussion
5. Conclusions and Future Direction
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- OECD. Health at a Glance 2019: OECD Indicators; OECD Publishing: Paris, France, 2019. [Google Scholar] [CrossRef]
- Mitnick, S.; Leffler, C.; Hood, V.L. Family caregivers, patients, and physicians: Ethical guidance to optimize relationships. J. Gen. Intern. Med. 2010, 25, 255–260. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Redfoot, D.; Feinberg, L.; Houser, A. AARP Public Policy Institute: Insight on the Issues 85. 2013. Available online: https://www.aarp.org/home-family/caregiving/info-08-2013/the-aging-of-the-baby-boom-and-the-growing-care-gap-AARP-ppiltc.html (accessed on 19 December 2021).
- Colombo, F.; Llena-Nozal, A.; Mercier, J.; Tjadens, F. Help Wanted? Providing and Paying for Long-Term Care, OECD Health Policy Studies; OECD Publishing: Paris, France, 2011; Available online: http://dx.doi.org/10.1787/9789264097759-en (accessed on 19 December 2021).
- European Union. Eurostat Regional Yearbook; Publications Office of the European Union: Luxembourg, 2021. [Google Scholar]
- European Union. Ageing Europe. Looking at the Lives of Older People in the EU; Publications Office of the European Union: Luxembourg, 2020. [Google Scholar]
- Zigante, V. Informal Care in Europe: Exploring Formalisation, Availability, and Quality; European Commission: Brussels, Belgium, 2018. [Google Scholar]
- Ribeiro, O.; Teixeira, L.; Araújo, L.; Paúl, C. Caregiver Support Ratio in Europe. Innov. Ageing 2019, 3, 138. [Google Scholar] [CrossRef]
- Reinhard, S.C.; Feinberg, L.F.; Houser, A.; Choula, R.; Evans, M. AARP Public Policy Institute. Insights on the Issues. Valuing the Invaluable: 2019 Update. Charting a Path Forward. 2019. Available online: https://www.aarp.org/content/dam/aarp/ppi/2019/11/valuing-the-invaluable-2019-update-charting-a-path-forward.doi.10.26419-2Fppi.00082.001.pdf (accessed on 19 December 2021).
- CENSUS HUB. Available online: https://ec.europa.eu/CensusHub2/query.do?step=selectHyperCube&qhc=false (accessed on 4 February 2021).
- UN Data. Available online: http://data.un.org/ (accessed on 4 February 2021).
- Pickard, L.; King, D. Informal Care Supply and Demand in Europe. ENEPRI Report; Geerts, J., Willemé, P., Mots, E., Eds.; ANCIEN: Brussels, Belgium, 2012; ISBN 9789461382023. [Google Scholar]
- Esping-Andersen, G. The Three Worlds of Welfare Capitalism; Policy Press: Cambridge, UK, 1990. [Google Scholar]
- EUROCARERS. Family Care in Europe. 2009. Available online: http://www.eurocarers.org/FactsheetEurocarers.pdf (accessed on 28 October 2021).
- Ferrera, M. Welfare State Reform in Southern Europe: Fighting Poverty and Social Exclusion in Italy, Spain, Portugal, and Greece; Routledge: London, UK, 2005. [Google Scholar]
- Barczyk, D.; Kredler, M. Long-term care across Europe and the United States: The role of informal and formal care. Fisc. Stud. 2019, 40, 329–373. [Google Scholar] [CrossRef]
- Rau, R.; Muszyńska, M.; Vaupel, J. Europe, the Oldest-Old Continent. In The Demography of Europe; Neyer, G., Andersson, G., Kulu, H., Bernardi, L., Bühler, C., Eds.; Springer: Berlin/Heidelberg, Germany, 2013; pp. 119–137. [Google Scholar]
- Gonyea, J.G. Changing family demographics, multigenerational bonds, and care for the oldest old. Public Policy Aging Rep. 2013, 23, 11–15. [Google Scholar] [CrossRef]
- World Health Organization. World Report on Ageing and Health; World Health Organization: Geneva, Switzerland, 2015. Available online: https://apps.who.int/iris/handle/10665/186463 (accessed on 19 December 2021).
- Herrmann, F.; Michel, J.-P.; Robine, J.-M. Worldwide decline in the oldest old support ratio. Eur. Geriatr. Med. 2010, 1, 3–8. [Google Scholar] [CrossRef]
- Teixeira, L.; Araújo, L.; Jopp, D.; Ribeiro, O. Centenarians in Europe. Maturitas 2017, 104, 90–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jopp, D.S.; Boerner, K.; Ribeiro, O.; Rott, C. Life at Age 100: An International Research Agenda for Centenarian Studies. J. Aging Soc. Policy 2016, 28, 133–147. [Google Scholar] [CrossRef] [PubMed]
- Macedo, T.; Sousa, L.; Ribeiro, O. Aged 70 and still a child: Complexities, strains and gains of older children caring for their (near) centenarian mothers. Age Ageing 2021. [Google Scholar] [CrossRef] [PubMed]
- ILC-UK. The Emotional Well-Being of Older Carers; University College London: London, UK, 2015; Available online: https://ilcuk.org.uk/wp-content/uploads/2018/10/The-emotional-wellbeing-of-older-carers.pdf (accessed on 25 October 2021).
- Tur-Sinai, A.; Teti, A.; Rommel, A.; Hlebec, V.; Lamura, G. How many older informal caregivers are there in Europe? Comparison of estimates of their prevalence from three European surveys. Int. J. Environ. Res. Public Health 2020, 17, 9531. [Google Scholar] [CrossRef] [PubMed]
- Greenwood, N.; Smith, R. The oldest carers: A narrative review and synthesis of the experiences of carers aged 75 years. Maturitas 2016, 94, 161–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- OECD. Who Cares? Attracting and Retaining Care Workers for the Elderly, OECD Health Policy Studies; OECD Publishing: Paris, France, 2020. [Google Scholar] [CrossRef]
- Aburto, J.M.; Schöley, J.; Kashnitsky, I.; Zhang, L.; Rahal, C.; Missov, T.I.; Mills, M.C.; Dowd, J.B.; Kashyap, R. Quantifying impacts of the COVID-19 pandemic through life-expectancy losses: A population-level study of 29 countries. Int. J. Epidemiol. 2021. [Google Scholar] [CrossRef]
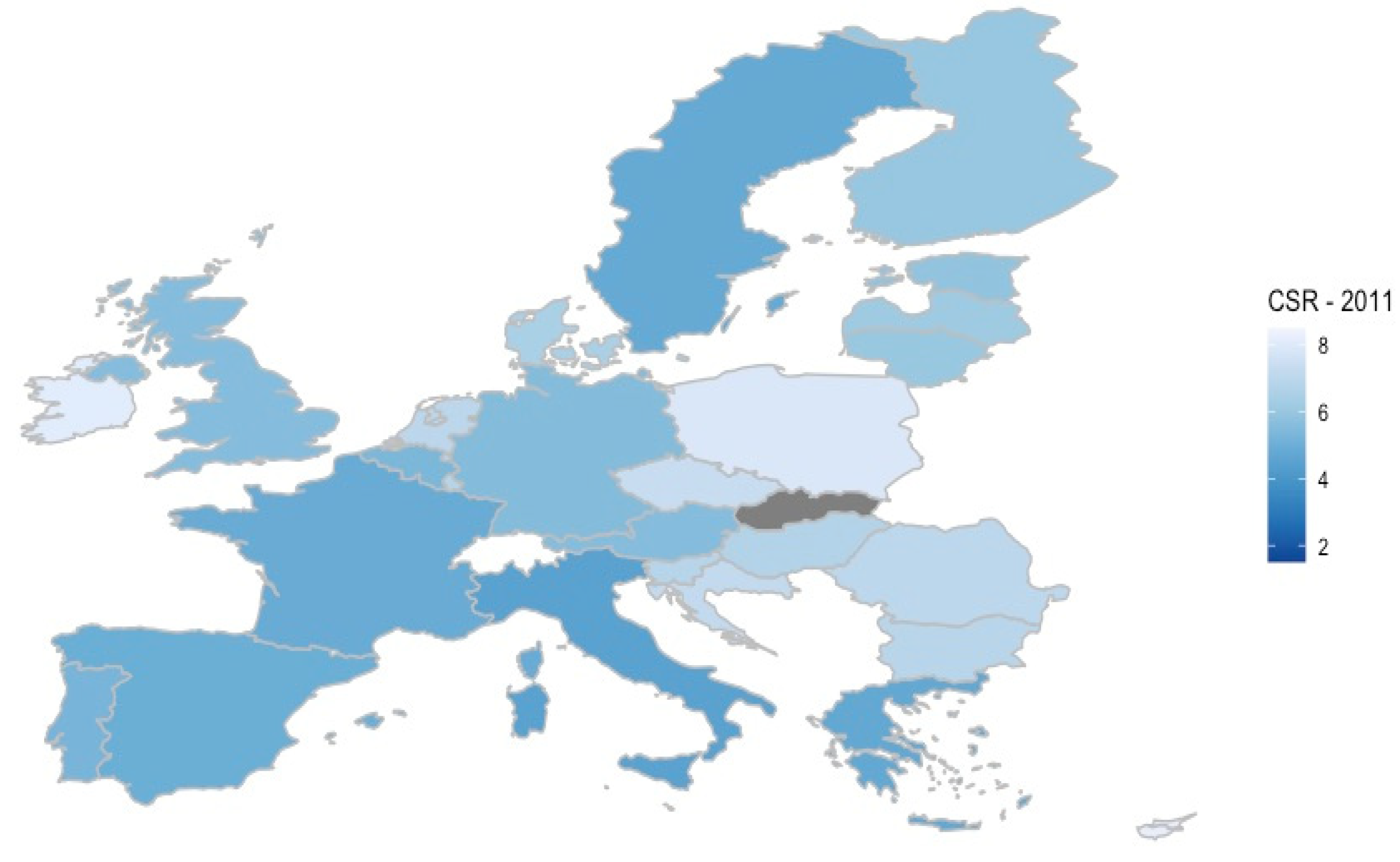
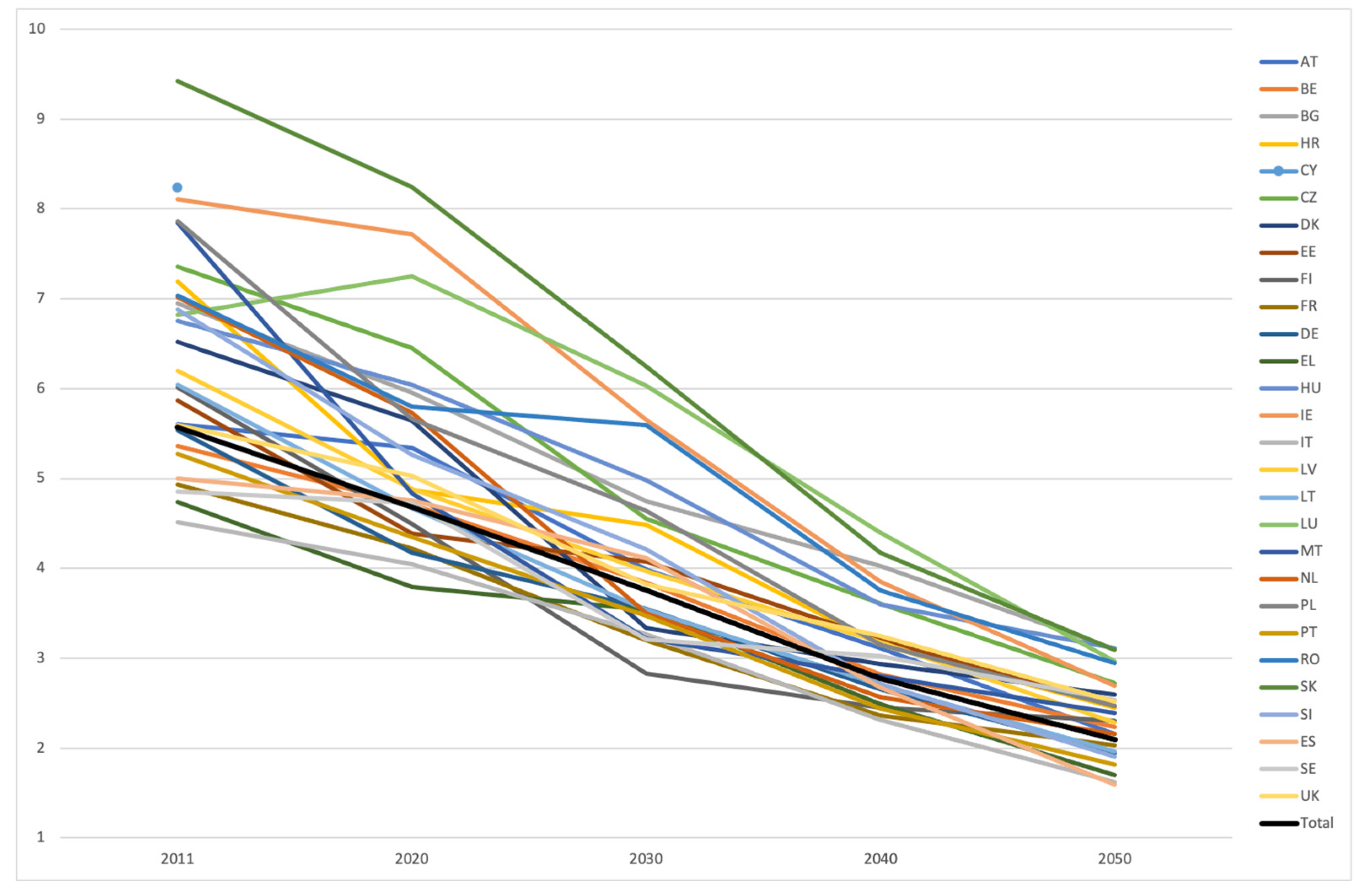
| Country | Caregiver Support Ratio, by Year | ||||
|---|---|---|---|---|---|
| 2011 | 2020 | 2030 | 2040 | 2050 | |
| Austria | 5.60 | 5.34 | 3.99 | 3.11 | 2.16 |
| Belgium | 5.36 | 4.71 | 3.84 | 2.82 | 2.24 |
| Bulgaria | 6.95 | 5.95 | 4.75 | 4.03 | 3.10 |
| Croatia | 7.19 | 4.87 | 4.48 | 3.15 | 2.45 |
| Cyprus | 8.24 | - | - | - | - |
| Czech Republic | 7.36 | 6.45 | 4.55 | 3.61 | 2.72 |
| Denmark | 6.52 | 5.64 | 3.34 | 2.94 | 2.60 |
| Estonia | 5.87 | 4.39 | 4.08 | 3.21 | 2.47 |
| Finland | 6.01 | 4.49 | 2.83 | 2.45 | 2.30 |
| France | 4.93 | 4.22 | 3.20 | 2.36 | 2.03 |
| Germany | 5.54 | 4.17 | 3.55 | 2.65 | 1.94 |
| Greece | 4.74 | 3.79 | 3.54 | 2.49 | 1.70 |
| Hungary | 6.75 | 6.04 | 4.98 | 3.60 | 3.11 |
| Ireland | 8.11 | 7.72 | 5.65 | 3.85 | 2.69 |
| Italy | 4.51 | 4.05 | 3.27 | 2.31 | 1.62 |
| Latvia | 6.20 | 4.88 | 3.97 | 3.18 | 2.28 |
| Lithuania | 6.04 | 4.67 | 3.54 | 2.70 | 1.96 |
| Luxembourg | 6.82 | 7.25 | 6.03 | 4.40 | 2.97 |
| Malta | 7.84 | 4.83 | 3.22 | 2.80 | 2.39 |
| Netherlands | 7.02 | 5.73 | 3.50 | 2.57 | 2.16 |
| Poland | 7.86 | 5.66 | 4.64 | 3.15 | 2.47 |
| Portugal | 5.27 | 4.35 | 3.47 | 2.44 | 1.82 |
| Romania | 7.03 | 5.80 | 5.59 | 3.75 | 2.95 |
| Slovakia | 9.42 | 8.24 | 6.25 | 4.17 | 3.09 |
| Slovenia | 6.88 | 5.26 | 4.21 | 2.71 | 1.90 |
| Spain | 5.00 | 4.76 | 4.11 | 2.67 | 1.59 |
| Sweden | 4.85 | 4.73 | 3.21 | 3.02 | 2.54 |
| United Kingdom | 5.59 | 5.03 | 3.82 | 3.25 | 2.52 |
| Total | 5.57 | 4.68 | 3.76 | 2.78 | 2.09 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ribeiro, O.; Araújo, L.; Figueiredo, D.; Paúl, C.; Teixeira, L. The Caregiver Support Ratio in Europe: Estimating the Future of Potentially (Un)Available Caregivers. Healthcare 2022, 10, 11. https://doi.org/10.3390/healthcare10010011
Ribeiro O, Araújo L, Figueiredo D, Paúl C, Teixeira L. The Caregiver Support Ratio in Europe: Estimating the Future of Potentially (Un)Available Caregivers. Healthcare. 2022; 10(1):11. https://doi.org/10.3390/healthcare10010011
Chicago/Turabian StyleRibeiro, Oscar, Lia Araújo, Daniela Figueiredo, Constança Paúl, and Laetitia Teixeira. 2022. "The Caregiver Support Ratio in Europe: Estimating the Future of Potentially (Un)Available Caregivers" Healthcare 10, no. 1: 11. https://doi.org/10.3390/healthcare10010011
APA StyleRibeiro, O., Araújo, L., Figueiredo, D., Paúl, C., & Teixeira, L. (2022). The Caregiver Support Ratio in Europe: Estimating the Future of Potentially (Un)Available Caregivers. Healthcare, 10(1), 11. https://doi.org/10.3390/healthcare10010011







