Computational Analysis of Coronary Blood Flow: The Role of Asynchronous Pacing and Arrhythmias
Abstract
:1. Introduction
2. Materials and Methods
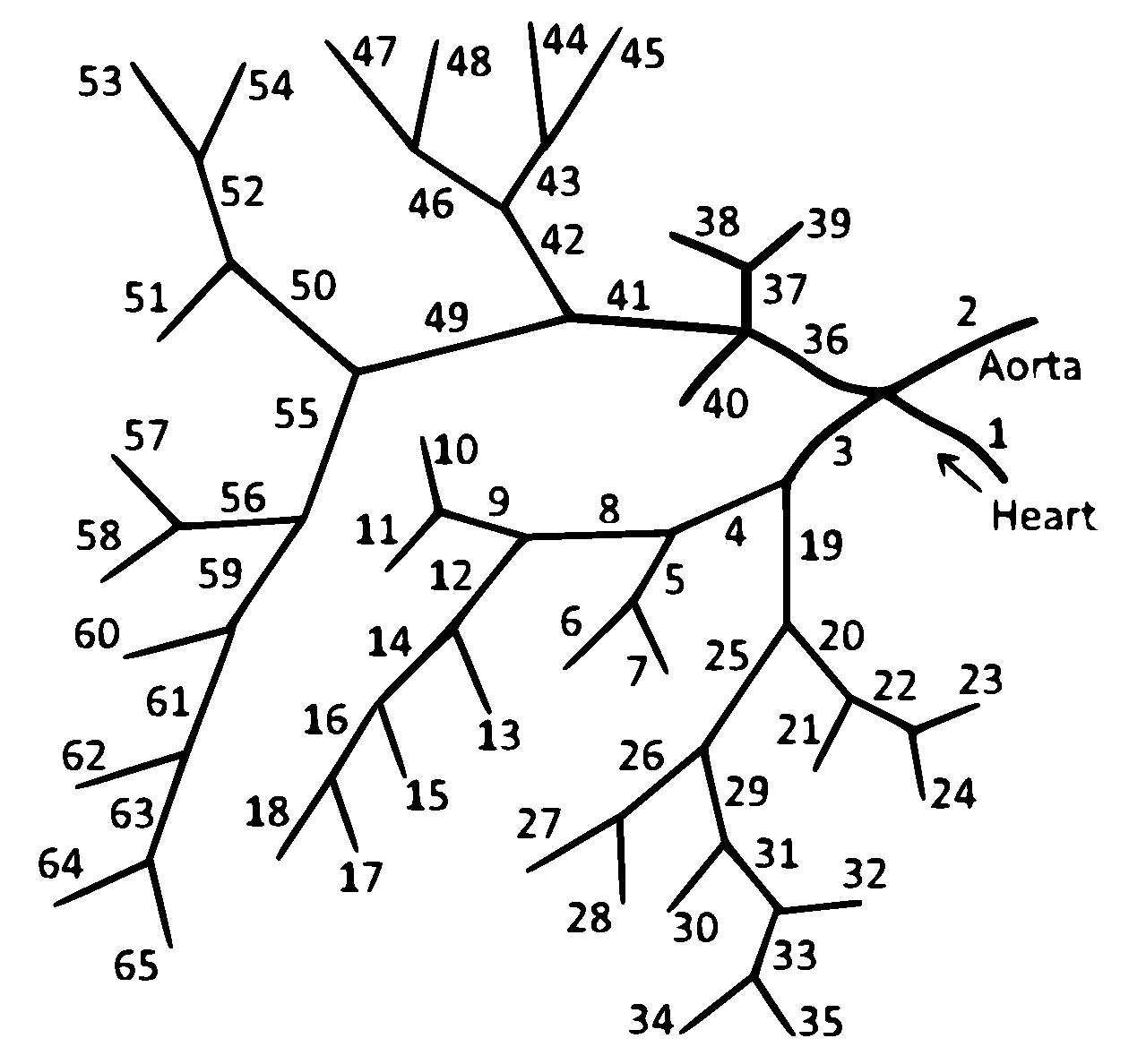
2.1. 1D Mathematical Model of Blood Flow in the Coronary Vascular Network
2.2. Effects of the Heart Rhythm on the Coronary Circulation
3. Results
3.1. Interventricular Dyssynchrony Due to Asynchronous Cardiac Pacing
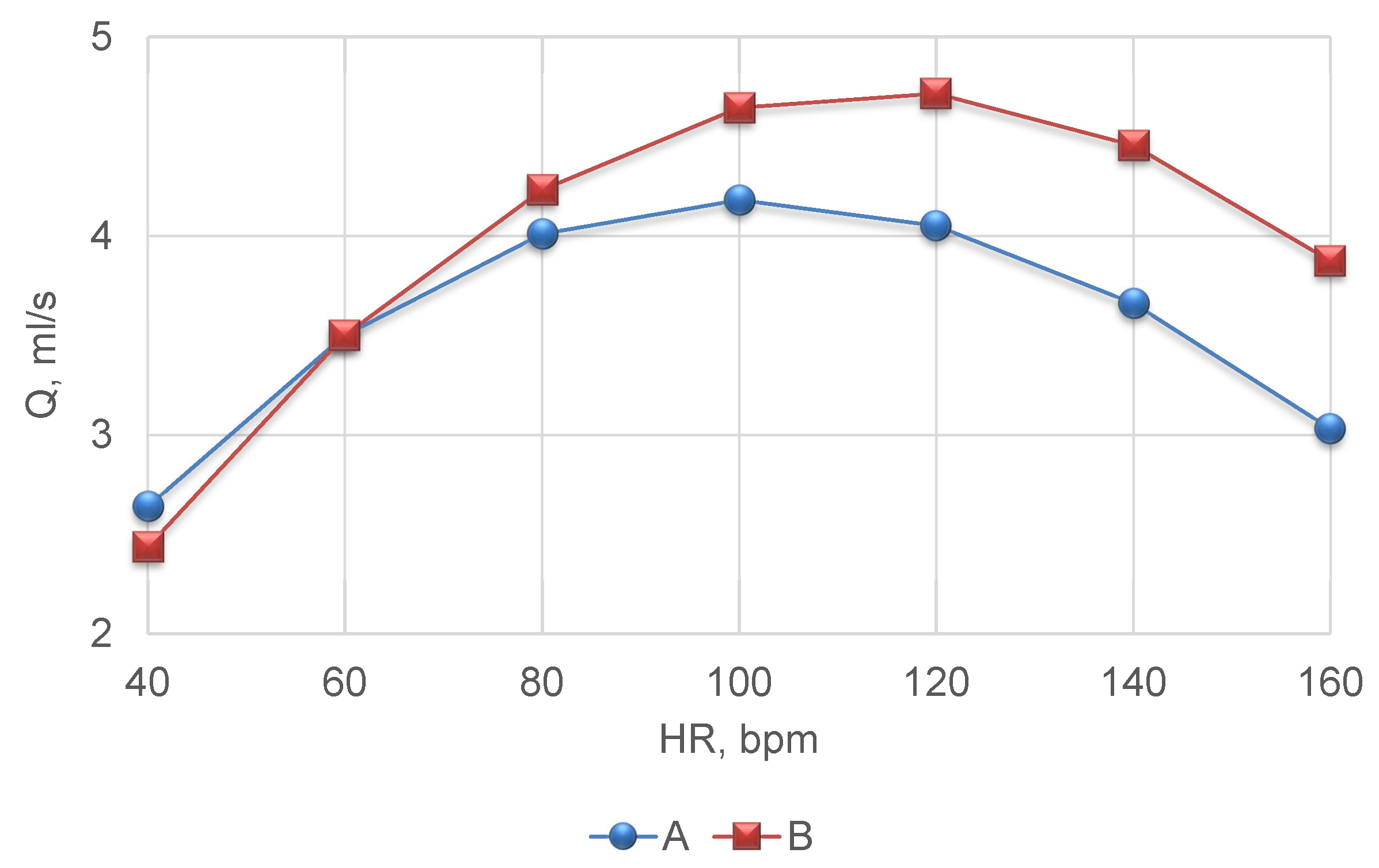
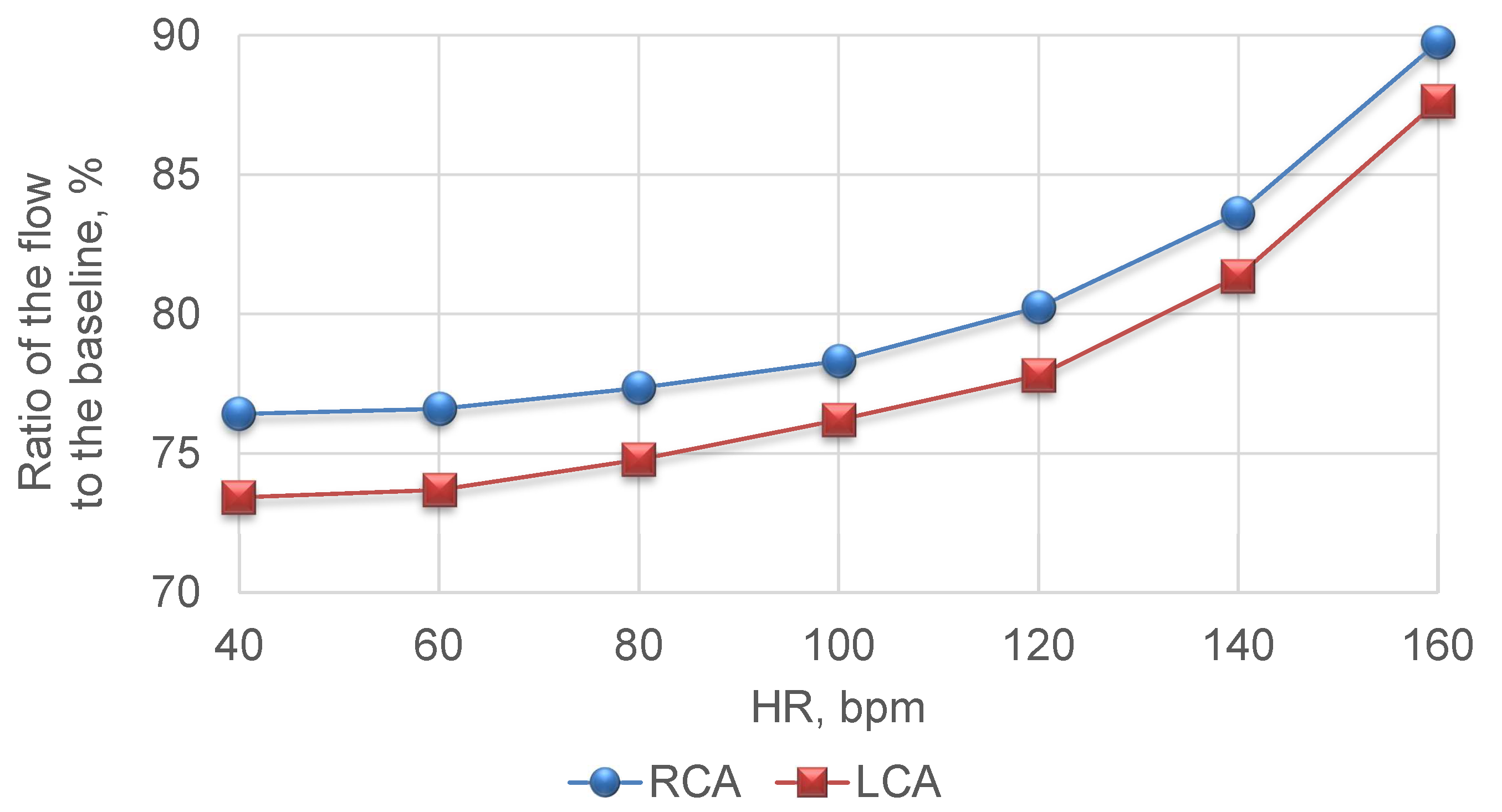
3.2. Tachycardia and Bradycardia
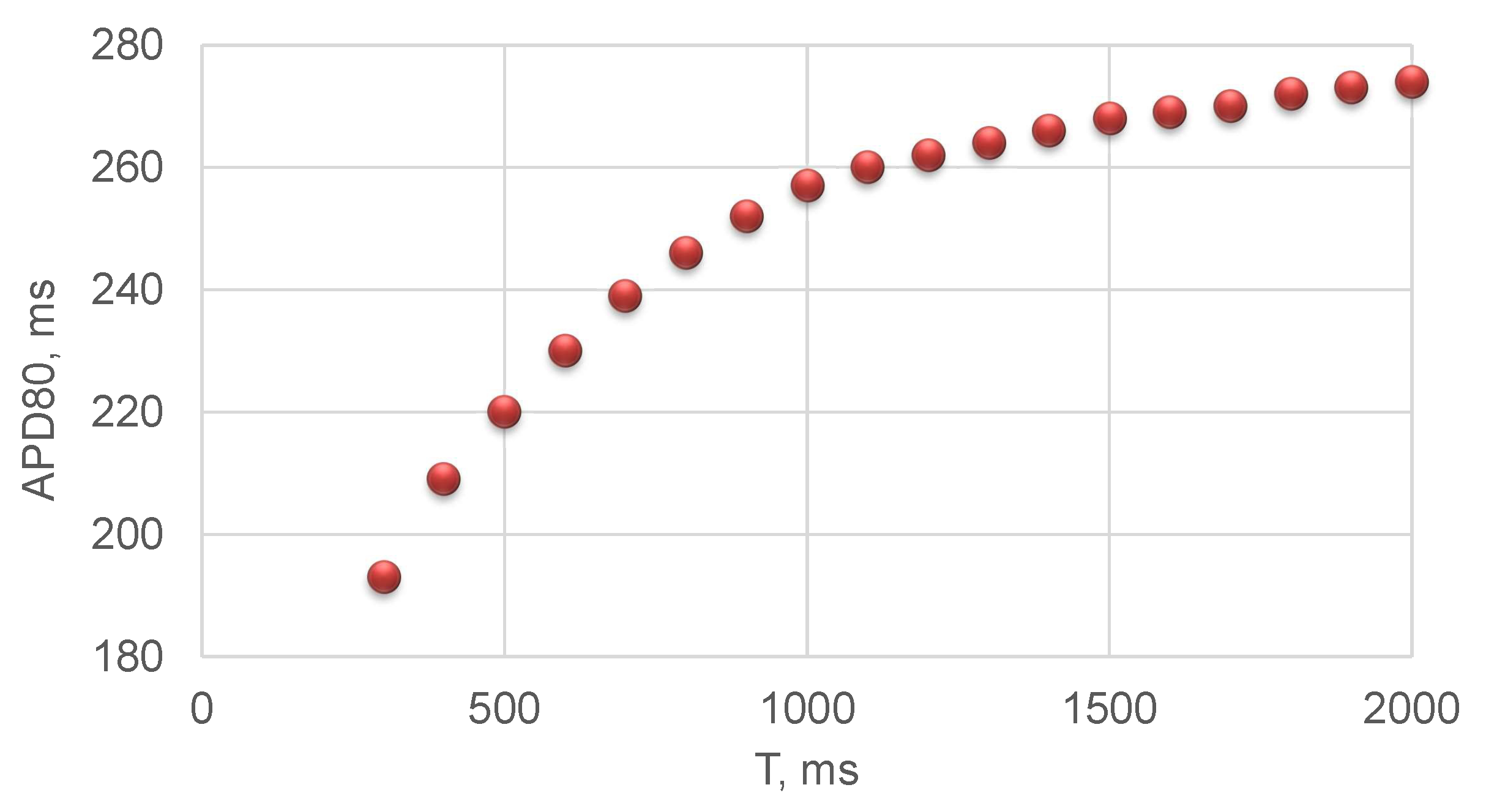
3.3. Long QT Syndrome
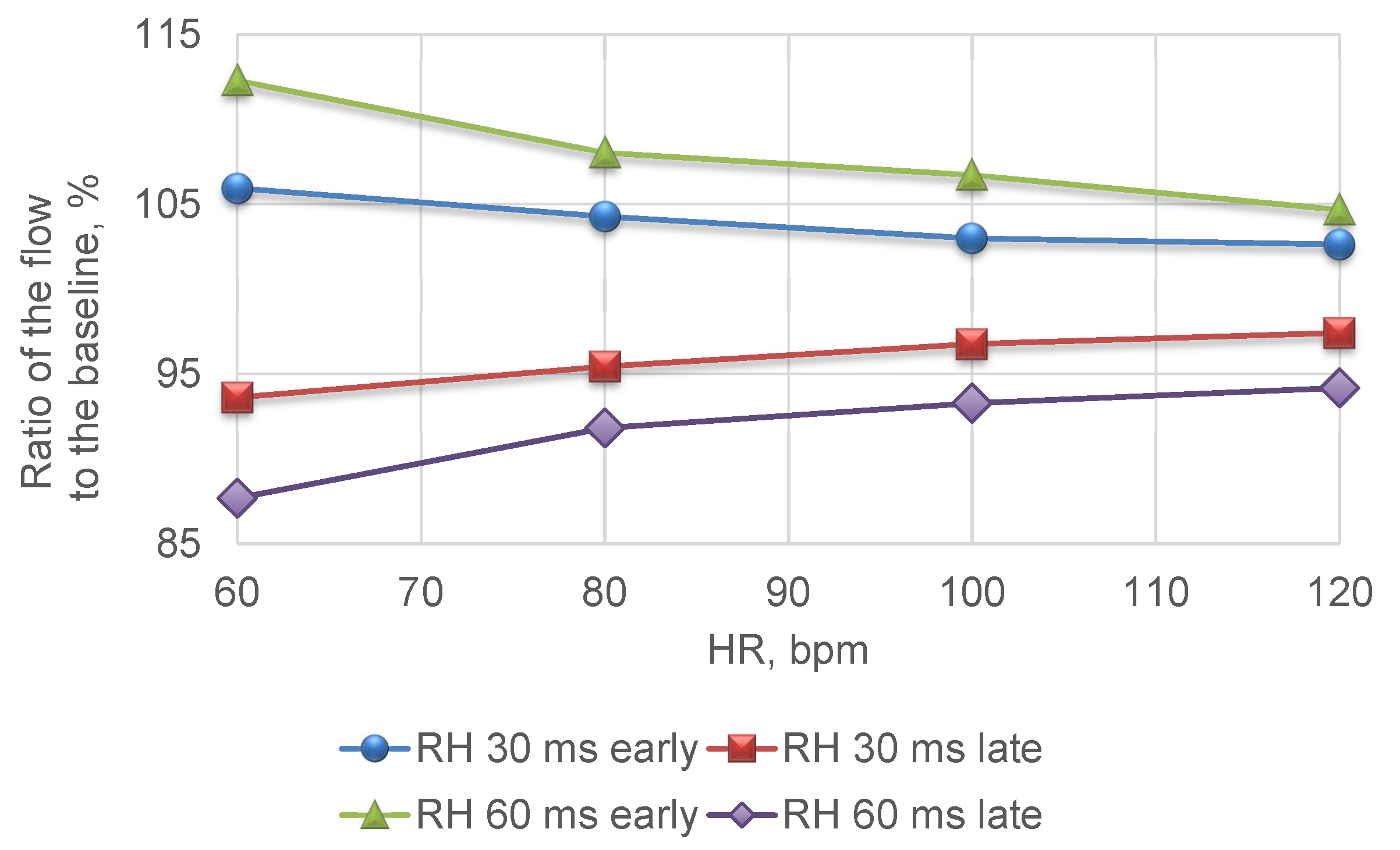
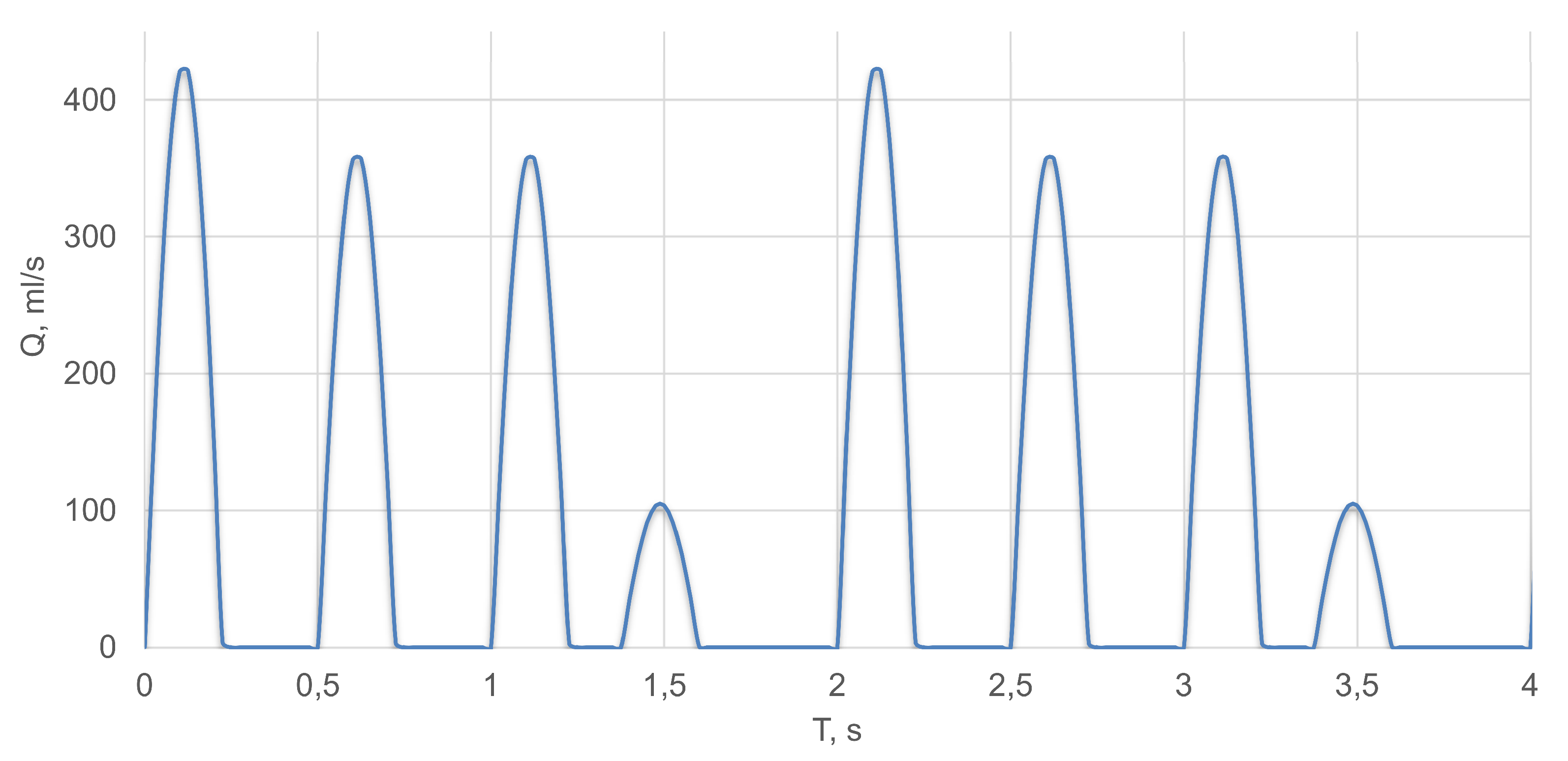
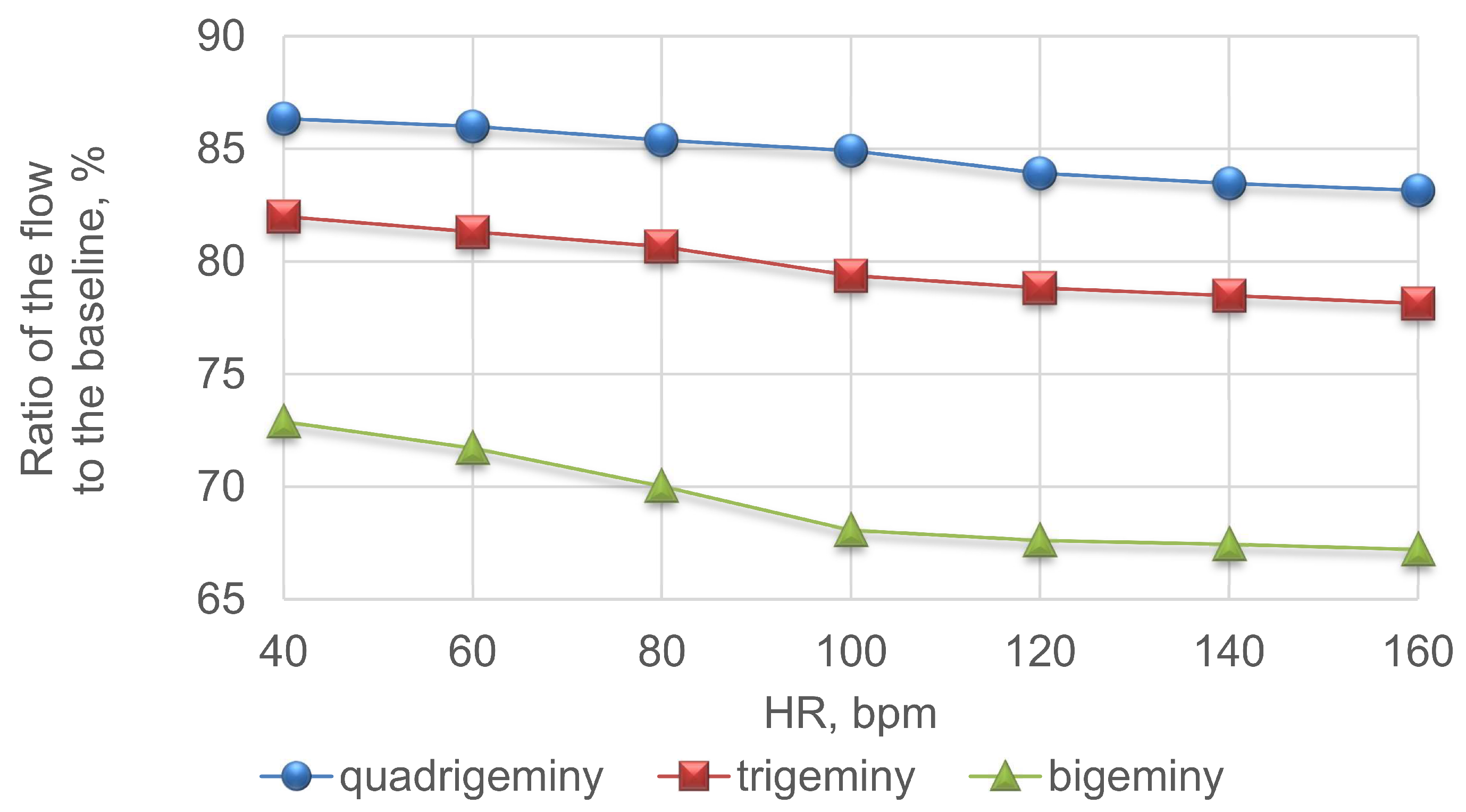
3.4. Premature Ventricular Contraction
4. Discussion
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| APD80 | Action potential duration at 80% repolarisation |
| AF | Atrial fibrillation |
| bpm | Beats per minute |
| CA | Coronary arteries |
| CBF | Coronary blood flow |
| CO | Cardiac output |
| ECG | Electrocardiogram |
| HR | Heart rate |
| LV | Left ventricle |
| LCA | Left coronary artery |
| OAC | Oral anticoagulant |
| PVC | Premature ventricular contraction |
| RCA | Right coronary artery |
| RV | Right ventricle |
| SAN | Sinoatrial node |
| SV | Stroke volume |
Appendix A

| k | k | ||||||
|---|---|---|---|---|---|---|---|
| 1 | 5.2 | 21.7 | 700 | 34 | 1.23 | 0.9 | 1200 |
| 2 | 20 | 25 | 1094 | 35 | 0.71 | 1.87 | 1200 |
| 3 | 2.61 | 4.96 | 1200 | 36 | 1.74 | 3.46 | 1300 |
| 4 | 1.83 | 4.14 | 1200 | 37 | 2.35 | 1.84 | 1300 |
| 5 | 2.45 | 1.78 | 1200 | 38 | 0.38 | 0.9 | 1300 |
| 6 | 0.65 | 0.9 | 1200 | 39 | 0.27 | 0.88 | 1300 |
| 7 | 1.58 | 0.9 | 1200 | 40 | 2.05 | 1.95 | 1300 |
| 8 | 2.04 | 3.04 | 1200 | 41 | 2.42 | 3.26 | 1300 |
| 9 | 2.76 | 1.96 | 1200 | 42 | 0.81 | 2.53 | 1300 |
| 10 | 3.3 | 0.89 | 1200 | 43 | 1.86 | 1.56 | 1300 |
| 11 | 1.98 | 0.96 | 1200 | 44 | 0.75 | 0.9 | 1300 |
| 12 | 1.32 | 2.31 | 1200 | 45 | 0.62 | 0.88 | 1300 |
| 13 | 2.66 | 1.11 | 1200 | 46 | 2.95 | 1.59 | 1300 |
| 14 | 3.67 | 1.78 | 1200 | 47 | 0.47 | 0.92 | 1300 |
| 15 | 2.26 | 0.98 | 1200 | 48 | 0.76 | 0.93 | 1300 |
| 16 | 1.94 | 1.05 | 1200 | 49 | 4.53 | 2.57 | 1300 |
| 17 | 0.97 | 0.9 | 1200 | 50 | 1.84 | 1.97 | 1300 |
| 18 | 1.84 | 0.9 | 1200 | 51 | 1.34 | 1.07 | 1300 |
| 19 | 3.13 | 3.92 | 1200 | 52 | 2.34 | 1.52 | 1300 |
| 20 | 4.97 | 2.91 | 1200 | 53 | 3.17 | 0.72 | 1300 |
| 21 | 2.16 | 1.3 | 1200 | 54 | 1.05 | 0.54 | 1300 |
| 22 | 4.05 | 1.84 | 1200 | 55 | 4.6 | 1.85 | 1300 |
| 23 | 2.49 | 0.9 | 1200 | 56 | 3.37 | 1.41 | 1300 |
| 24 | 1.97 | 0.88 | 1200 | 57 | 2.34 | 0.6 | 1300 |
| 25 | 2.47 | 3.02 | 1200 | 58 | 1.88 | 0.67 | 1300 |
| 26 | 2.45 | 1.78 | 1200 | 59 | 2.42 | 1.5 | 1300 |
| 27 | 1.5 | 1.06 | 1200 | 60 | 3.14 | 0.88 | 1300 |
| 28 | 1.11 | 1.03 | 1200 | 61 | 0.66 | 1.34 | 1300 |
| 29 | 2.58 | 2.39 | 1200 | 62 | 1.47 | 0.9 | 1300 |
| 30 | 1.34 | 1.07 | 1200 | 63 | 0.87 | 1.15 | 1300 |
| 31 | 0.71 | 1.87 | 1200 | 64 | 2.75 | 0.6 | 1300 |
| 32 | 2.1 | 1.02 | 1200 | 65 | 1.23 | 0.42 | 1300 |
| 33 | 2.22 | 1.44 | 1200 |
References
- Abdi, M.; Karimi, A.; Navidbakhsh, M.; Pirzad, G.; Hassani, J.K. A lumped parameter mathematical model to analyze the effects of tachycardia and bradycardia on the cardiovascular system. Int. J. Numer. Model. Electron. Netw. Devices Fields 2015, 3, 346–357. [Google Scholar] [CrossRef]
- Arthurs, C.J.; Lau, K.D.; Asrress, K.N.; Redwood, S.R.; Figueroa, C.A. A mathematical model of coronary blood flow control: Simulation of patient-specific three-dimensional hemodynamics during exercise. Am. J. Physiol. Heart Circ. Physiol. 2016, 310, H1242–H1258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bashore, T.M.; Stine, R.A.; Shaffer, P.B.; Bush, C.A.; Leier, C.V.; Schaal, S.F. The noninvasive localization of ventricular pacing sites by radionuclide phase imaging. Circulation 1984, 70, 681–694. [Google Scholar] [CrossRef] [Green Version]
- Prinzen, F.W.; Augustijn, C.H.; Arts, T.; Allessie, M.A.; Reneman, R.S. Redistribution of myocardial fiber strain and blood flow by asynchronous activation. Am. J. Physiol. Heart Circ. Physiol. 1990, 259, H300–H308. [Google Scholar] [CrossRef] [PubMed]
- Delhaas, T.; Arts, T.; Prinzen, F.W.; Reneman, R.S. Regional fibre stress–Fibre strain area as an estimate of regional blood flow and oxygen demand in the canine heart. J. Physiol. 1994, 477, 481–496. [Google Scholar] [CrossRef] [PubMed]
- Tarumi, T.; Takebayashi, S.; Fujita, M.; Nakano, T.; Ito, M.; Yamakado, T. Pacing tachycardia exaggerates left ventricular diastolic dysfunction but not systolic function and regional asynergy or asynchrony in patients with hypertrophic cardiomyopathy. EP Eur. 2010, 12, 1308–1315. [Google Scholar] [CrossRef] [PubMed]
- Numan, M.T.; Maposa, D.; Kantharia, B. Supraventricular tachycardia significantly reduces stroke volume and causes minimal reduction of cardiac output: Study of pediatric patients. Heart Rhythm 2011, 8, 1826. [Google Scholar] [CrossRef]
- Khan, I.A. Long QT syndrome: Diagnosis and management. Am. Heart J. 2002, 143, 7–14. [Google Scholar] [CrossRef]
- Patel, P.J.; Borovskiy, Y.; Killian, A.; Verdino, R.J.; Epstein, A.E.; Callans, D.J.; Marchlinski, F.E.; Deo, R. Optimal QT interval correction formula in sinus tachycardia for identifying cardiovascular and mortality risk: Findings from the Penn Atrial Fibrillation Free study. Heart Rhythm 2016, 13, 527–535. [Google Scholar] [CrossRef] [Green Version]
- Gerstenfeld, E.P.; De Marco, T. Premature Ventricular Contractions. Circulation 2019, 140, 624–626. [Google Scholar] [CrossRef]
- Cohn, K.; Kryda, W. The influence of ectopic beats and tachyarrhythmias on stroke volume and cardiac output. J. Electrocardiol. 1981, 14, 207–218. [Google Scholar] [CrossRef]
- Van de Vosse, F.N. Mathematical modelling of the cardiovascular system. J. Eng. Math. 2003, 47, 175–183. [Google Scholar] [CrossRef]
- Bessonov, N.; Sequeira, A.; Simakov, S.; Vassilevski, Y.; Volpert, V. Methods of blood flow modelling. Math. Model. Nat. Phenom. 2016, 11, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Jackowska-Zduniak, B.; Fory’s, U. Mathematical model of the atrioventricular nodal double response tachycardia and double-fire pathology. Math. Biosci. Eng. 2016, 13, 1143–1158. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ge, X.; Liu, Y.; Yin, Z.; Tu, S.; Fan, Y.; Vassilevski, Y.; Simakov, S.; Liang, F. Comparison of instantaneous wave-free ratio (iFR) and fractional flow reserve (FFR) with respect to their sensitivities to cardiovascular factors: A computational model-based study. J. Interv. Cardiol. 2020, 2020, 4094121. [Google Scholar] [CrossRef] [PubMed]
- Ge, X.; Liu, Y.; Tu, S.; Simakov, S.; Vassilevski, Y.; Liang, F. Model-based analysis of the sensitivities and diagnostic implications of FFR and CFR under various pathological conditions. Int. J. Numer. Methods Biomed. Eng. 2019. [Google Scholar] [CrossRef]
- Boileau, E.; Pant, S.; Roobottom, C.; Sazonov, I.; Deng, J.; Xie, X.; Nithiarasu, P. Estimating the accuracy of a reduced-order model for the calculation of fractional flow reserve (FFR). Int. J. Numer. Methods Biomed. Eng. 2017, 34, e2908. [Google Scholar] [CrossRef] [Green Version]
- Bezerra, C.; Lemos, P.A.; Pinton, F.A.; Müller, L.; Bulant, C.; Talou, G.M.; Feijóo, R.A.; Esteves, A.E.F.; Blanco, P. Tct-619 comparison of one-dimensional (1d) and three-dimensional (3d) models for the estimation of coronary fractional flow reserve through cardiovascular imaging. J. Am. Coll. Cardiol. 2018, 72 (Suppl. 13), B248. [Google Scholar] [CrossRef]
- Sinclair, M.D.; Lee, J.; Cookson, A.N.; Rivolo, S.; Hyde, E.R.; Smith, N.P. Measurement and modeling of coronary blood flow. Wiley Interdiscip. Rev. Syst. Biol. Med. 2015, 7, 335–356. [Google Scholar] [CrossRef]
- Gamilov, T.M.; Liang, F.Y.; Simakov, S.S. Mathematical modeling of the coronary circulation during cardiac pacing and tachycardia. Lobachevskii J. Math. 2019, 40, 448–458. [Google Scholar] [CrossRef]
- Plasticboy Pictures CC. 2009. Available online: http://www.plasticboy.co.uk/store/ (accessed on 20 June 2020).
- Vassilevski, Y.; Olshanskii, M.; Simakov, S.; Kolobov, A.; Danilov, A. Personalized Computational Hemodynamics: Models, Methods, and Applications for Vascular Surgery and Antitumor Therapy; Academic Press: Cambridge, MA, USA, 2020. [Google Scholar]
- Danilov, A.; Ivanov, Y.; Pryamonosov, R.; Vassilevski, Y. Methods of graph network reconstruction in personalized medicine. Int. J. Numer. Methods Biomed. Eng. 2016, 32, e02754. [Google Scholar] [CrossRef] [PubMed]
- Gamilov, T.; Alastruey, J.; Simakov, S. Linear optimization algorithm for 1D hemodynamics parameter estimation. In Proceedings of the 6th European Conference on Computational Mechanics: Solids, Structures and Coupled Problems, ECCM 2018 and 7th European Conference on Computational Fluid Dynamics, ECFD 2018; Owen, R., de Borst, R., Reese, J., Pearce, C., Eds.; CIMNE: Barcelona, Spain, 2020; pp. 1845–1850. [Google Scholar]
- Van de Vosse, F.N.; Stergiopulos, N. Pulse wave propagation in the arterial tree. Annu. Rev. Fluid Mech. 2011, 43, 467–499. [Google Scholar] [CrossRef] [Green Version]
- Gamilov, T.; Simakov, S. Blood flow under mechanical stimulations. Adv. Intell. Syst. Comput. 2020, 1028, 143–150. [Google Scholar]
- Gamilov, T.; Kopylov, P.; Simakov, S. Computational simulations of fractional flow reserve variability. Lect. Notes Comput. Sci. Eng. 2016, 112, 499–507. [Google Scholar]
- Vassilevski, Y.V.; Salamatova, V.Y.; Simakov, S.S. On the elasticity of blood vessels in one-dimensional problems of hemodynamics. Comput. Math. Math. Phys. 2015, 55, 1567–1578. [Google Scholar] [CrossRef]
- Magomedov, K.M.; Kholodov, A.S. Grid-Characteristic Numerical Methods; Urite: Moscow, Russia, 2018. [Google Scholar]
- O’Hara, T.; Virág, L.; Varró, A.; Rudy, Y. Simulation of the undiseased human cardiac ventricular action potential: Model formulation and experimental validation. PLoS Comput. Biol. 2011, 7, e1002061. [Google Scholar] [CrossRef] [Green Version]
- Rush, S.; Larsen, H. A practical algorithm for solving dynamic membrane equations. IEEE Trans. Biomed. Eng. 1978, 25, 389–392. [Google Scholar] [CrossRef]
- Smirnov, D.; Pikunov, A.; Syunyaev, R.; Deviatiiarov, R.; Gusev, O.; Aras, K.; Gams, A.; Koppel, A.; Efimov, I.R. Genetic algorithm-based personalized models of human cardiac action potential. PLoS ONE 2020, 15, e0231695. [Google Scholar] [CrossRef]
- Linhart, J.W. Myocardial function in coronary artery disease determined by atrial pacing. Circulation 1972, 44, 203–212. [Google Scholar] [CrossRef] [Green Version]
- Geddes, L.A.; Wessale, J.L. Cardiac output, stroke Volume, and pacing rate: A review of the literature and a proposed technique for selection of the optimum pacing rate for an Exercise responsive pacemaker. J. Cardiovasc. Electrophysiol. 1991, 2, 408–415. [Google Scholar] [CrossRef]
- Noble, M.I.M.; Trenchord, D.; Guz, A. Effect of changing heart rate on cardiovascular function in the conscious dog. Circ. Res. 1966, 19, 206–213. [Google Scholar] [CrossRef] [Green Version]
- Kenny, J.; Plappert, T.; Doubilet, P.; Salzman, D.; Sutton, M.G. Effects of heart rate on ventricular size, stroke volume, and output in the normal human fetus: A prospective Doppler echocardiographic study. Circulation 1987, 76, 52–58. [Google Scholar] [CrossRef] [Green Version]
- Roeth, N.A.; Ball, T.R.; Culp, W.C.; Bohannon, W.T.; Atkins, M.D.; Johnston, W.E. Effect of increasing heart rate and tidal volume on stroke volume variability in vascular surgery patients. J. Cardiothorac. Vasc. Anesth. 2014, 28, 1516–1520. [Google Scholar] [CrossRef]
- Kumada, M.; Azuma, T.; Matsuda, K. The cardiac output-heart rate relationship under different conditions. Jpn. J. Physiol. 1967, 17, 538–555. [Google Scholar] [CrossRef]
- Gamilov, T.M.; Kopylov, P.Y.; Pryamonosov, R.A.; Simakov, S.S. Virtual fractional flow reserve assessment in patient-specific coronary networks by 1d hemodynamic model. Russ. J. Numer. Anal. Math. Model. 2015, 30, 269–276. [Google Scholar] [CrossRef]
- Vassilevski, Y.V.; Danilov, A.A.; Gamilov, T.M.; Simakov, S.S.; Ivanov, Y.A.; Pryamonosov, R.A. Patient-specific anatomical models in human physiology. Russian J. Numer. Anal. Math. Model. 2015, 30, 185–201. [Google Scholar] [CrossRef]
- Carson, J.M.; Pant, S.; Roobottom, C.; Alcock, R.; Blanco, P.J.; Carlos Bulant, C.A.; Vassilevski, Y.; Simakov, S.; Gamilov, T.; Pryamonosov, R.; et al. Non-invasive coronary CT angiography-derived fractional flow reserve: A benchmark study comparing the diagnostic performance of four different computational methodologies. Int. J. Numer. Methods Biomed. Eng. 2019, 35, e3235. [Google Scholar] [CrossRef] [Green Version]
- Barret, K.; Brooks, H.; Boitano, S.; Barman, S. Ganong’s Review of Medical Physiology, 23th ed.; The McGraw-Hill: New York, NY, USA, 2010. [Google Scholar]
- Ghio, S.; Constantin, C.; Klersy, C.; Serio, A.; Fontana, A.; Campana, C.; Tavazzi, L. Interventricular and intraventricular dyssynchrony are common in heart failure patients, regardless of QRS duration. Eur. Heart J. 2004, 25, 571–578. [Google Scholar] [CrossRef]
- Heusch, G. Heart rate in the pathophysiology of coronary blood flow and myocardial ischaemia: Benefit from selective bradycardic agents. Br. J. Pharmacol. 2008, 153, 1589–1601. [Google Scholar] [CrossRef]
- Simakov, S.; Gamilov, T.; Soe, Y.N. Computational study of blood flow in lower extremities under intense physical load. Russ. J. Numer. Anal. Math. Model. 2013, 28, 485–503. [Google Scholar] [CrossRef]
- Kovács, S.J. The duration of the QT interval as a function of heart rate: A derivation based on physical principles and a comparison to measured values. Am. Heart J. 1985, 110, 872–878. [Google Scholar] [CrossRef]
- Lou, Q.; Fedorov, V.V.; Glukhov, A.V.; Moazami, N.; Fast, V.G.; Efimov, I.R. Transmural heterogeneity and remodeling of ventricular excitation-contraction coupling in human heart failure. Circulation 2011, 123, 1881–1890. [Google Scholar] [CrossRef] [PubMed]
- Kassiri, Z.; Myers, R.; Kaprielian, R.; Banijamali, H.S.; Backx, P.H. Rate-dependent changes of twitch force duration in rat cardiac trabeculae: A property of the contractile system. J. Physiol. 2000, 524 Pt 1, 221–231. [Google Scholar] [CrossRef]
- Lang, D.; Holzem, K.; Kang, C.; Xiao, M.; Hwang, H.J.; Ewald, G.A.; Yamada, K.A.; Efimov, I.R. Arrhythmogenic remodeling of β2 versus β1 adrenergic signaling in the human failing heart. Circ. Arrhythmia Electrophysiol. 2015, 8, 409–419. [Google Scholar] [CrossRef] [Green Version]
- Manav, S. Contemporary management of stroke prevention in atrial fibrillation following the European Society of Cardiology guidelines. Eur. Cardiol. 2017, 12, 38–39. [Google Scholar]
- January, C.T.; Wann, L.S.; Alpert, J.S.; Calkins, H.; Cigarroa, J.E.; Clevel, J.C., Jr.; Conti, J.B.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: A report of the American College of Cardiology/American Heart Association task force on practice guidelines and the heart rhythm society. J. Am. Coll. Cardiol. 2014, 64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- DiMatteo, M.R. Variations in Patients’ Adherence to Medical Recommendations. Med. Care 2004, 42, 200–209. [Google Scholar] [CrossRef] [PubMed]
- Lowres, N.; Giskes, K.; Hespe, C.; Freedman, B. Reducing stroke risk in atrial fibrillation: Adherence to guidelines has improved, but patient persistence with anticoagulant therapy remains suboptimal. Korean Circ. J. 2019, 49, 883–907. [Google Scholar] [CrossRef] [PubMed]
- Banerjee, A.; Benedetto, V.; Gichuru, P.; Burnell, J.; Antoniou, S.; Schilling, R.J.; Strain, W.D.; Ryan, R.; Watkins, C.; Marshall, T.; et al. Adherence and persistence to direct oral anticoagulants in atrial fibrillation: A population–Based study. Heart 2020, 106, 119–126. [Google Scholar] [CrossRef] [Green Version]
- Guala, A.; Leone, D.; Milan, A.; Ridolfi, L. In silico analysis of the anti-hypertensive drugs impact on myocardial oxygen balance. Biomech. Model. Mechanobiol. 2017, 16, 1035–1047. [Google Scholar] [CrossRef]


© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gamilov, T.; Kopylov, P.; Serova, M.; Syunyaev, R.; Pikunov, A.; Belova, S.; Liang, F.; Alastruey, J.; Simakov, S. Computational Analysis of Coronary Blood Flow: The Role of Asynchronous Pacing and Arrhythmias. Mathematics 2020, 8, 1205. https://doi.org/10.3390/math8081205
Gamilov T, Kopylov P, Serova M, Syunyaev R, Pikunov A, Belova S, Liang F, Alastruey J, Simakov S. Computational Analysis of Coronary Blood Flow: The Role of Asynchronous Pacing and Arrhythmias. Mathematics. 2020; 8(8):1205. https://doi.org/10.3390/math8081205
Chicago/Turabian StyleGamilov, Timur, Philipp Kopylov, Maria Serova, Roman Syunyaev, Andrey Pikunov, Sofya Belova, Fuyou Liang, Jordi Alastruey, and Sergey Simakov. 2020. "Computational Analysis of Coronary Blood Flow: The Role of Asynchronous Pacing and Arrhythmias" Mathematics 8, no. 8: 1205. https://doi.org/10.3390/math8081205
APA StyleGamilov, T., Kopylov, P., Serova, M., Syunyaev, R., Pikunov, A., Belova, S., Liang, F., Alastruey, J., & Simakov, S. (2020). Computational Analysis of Coronary Blood Flow: The Role of Asynchronous Pacing and Arrhythmias. Mathematics, 8(8), 1205. https://doi.org/10.3390/math8081205






