Abstract
Health care organisations have broadened their commitment to corporate social responsibility, since, as well as providing health care to patients, their activities negatively affect world pollution. This is a result of the products and technologies they use, the resources they consume, the waste they produce, and the buildings they occupy and operate. This, in turn, affects the health of the community. For this reason, a growing number of health care organisations have become involved in improvements to environmental sustainability, in order to promote public health. These improvements need to be controlled by a system whose effects can be assessed within a process of continuous improvement. This research, therefore, sets out a model constructed by extension to a fuzzy environment of the technique for order preference by similarity to ideal situation (TOPSIS), to assess the environmental responsibility of health care organizations. The weights were obtained from judgements given by both an expert in environmental matters, and a group of patients, and the judgements of both types of stakeholder were combined. The model has been applied in a Spanish public hospital over a period of five years. The closeness coefficients obtained with the judgements from the patient group are on average 6.59% higher than those obtained from the expert, and so it can be said that patients are less demanding on environmental matters. The similarity of the models was assessed, by comparing the model that combines both sets of judgements with the model constructed from the judgements of the expert and the model built from the judgements of the patient groups. The similarity is seen to be high, but it is greater in the case of the ranking obtained from the patient judgements. The results in all cases suggest a low risk of a serious environmental problem in the hospital. Nonetheless, it also implies that there are opportunities for continuous improvement. The use of a model with judgements from a patient group was intended to take into account the increasingly important need to include the judgements and opinions of different stakeholders in decision and assessment processes in the hospital environment.
1. Introduction
Health care organisations have broadened their commitment to corporate social responsibility, since, as well as patient care, improvements in environmental sustainability affect the health of a community, as the combined effects of climate change, chemical pollution, and unsustainable use of resources lead to higher rates of disease around the world. However, health care activity itself has negative effects on pollution around the world due to the products and technologies it uses, the resources it consumes, the waste it produces, and the buildings it builds and operates, the consequences of which it must also deal with [1]. Health care organisations must, therefore, offer care services in a sustainable manner, to safeguard not only health, but also the environment and society [2]. An increasing number of health care organisations have made commitments to improving environmental sustainability in order to promote public health.
Despite its great significance, there are serious deficiencies in the literature regarding sustainability in hospitals, as shown in Section 2.1. For example, the literature does not take into account the various stakeholders in environmental assessment systems. Including the opinions of stakeholders, such as patients and experts, helps to have a fuller view of the level of environmental sustainability valued by the community. Furthermore, comparisons of the sustainability of hospitals between countries is practically impossible due to differences in economic income, legislation, services, waste management systems, etc. [3]. There is also the fact that public hospitals are not prepared to compare their sustainability initiatives. All of this makes it difficult to apply benchmarking and to obtain the benefits offered by this tool [4]. It is, therefore, essential to have objective tools to facilitate monitoring of environmental sustainability in health care organisations, in order to take informed decisions. Most important, however, is to minimise the negative environmental impacts that might have health implications [5]. The assessment of sustainability is recognised as an effective analytical methodology for improving performance in sustainability [6], with a process of continuous improvement.
This research, therefore, sets out a multicriteria assessment model designed with the fuzzy technique for order preference by similarity to ideal situation (TOPSIS), to assess the environmental sustainability of health care organisations. Working in a fuzzy environment can improve the research, since it includes the hesitancy, vagueness, ambiguity, uncertainty, and doubt typical of real-life decision processes. However, it can also lead to significant difficulties in implementation, and a considerable increase in the complexity of the MCDA model. Although there are several options for addressing uncertainty, it is important to choose an MCDA methodology that is simple and comprehensible to decision makers [7]. This is especially important if they are unfamiliar with uncertainty analysis, as is the case, in our study, of hospital patients. A full description of the reasons for the choice of fuzzy TOPSIS is given in Section 3.
The main contribution of this environmental assessment system is to provide health care organisations with a model that is easy to use, with criteria specific to health care, and that allows the level of environmental sustainability to be monitored over time and compared with other Health care organisations, in order to assess the goodness of applying specific actions. This assessment was carried out using the weights obtained from an expert in environmental matters, independently from a group of hospital patients, and also using a combination of the judgements of the expert and the patients. Following the methodology used in Carnero [8], the criteria were assessed as a function of the number of services provided annually at the hospital. This allows the results to be compared from year to year or between health care organisations, allowing for internal and competitive benchmarking. The model was applied in a public hospital over a period of five years, and the results obtained from the weights of the expert, the patient group, and combining all the judgements were compared.
The main contributions of this research are:
- Presenting a multicriteria model for internal and competitive assessment (benchmarking) of the environmental sustainability of health care organisations, so that a quick and objective comparison of environmental improvement actions undertaken by each hospital can be carried out. This was done by applying the model to a public hospital over five consecutive years, using internal benchmarking to detect actions that lead to significant improvement or decline in environmental sustainability.
- Including the ambiguities, uncertainties, and doubts inherent in real-world decision processes in the model, by designing a multicriteria model in a fuzzy environment.
- Comparing the results obtained with the model by using, independently, judgements from an expert and from a patient group, in order to see the aspects that each decision maker considers more important and how they affect the results.
- Combining the judgements of the environmental expert and the patient group into one model. Comparing the results obtained by combining the judgements of the environmental expert and the group of patients with the results of the models that use the judgements of each stakeholder independently.
The layout of this paper is as follows. Firstly, there is a literature review on environmental sustainability, including the background of the problem, and multicriteria contributions applied to this field. The fuzzy multicriteria TOPSIS technique is then described, followed by the model for assessment of environmental responsibility for health care organisations. Next come the results of applying the model for five consecutive years in a hospital, considering the judgements given by an environmental expert, a group of patients, and from combining the judgements of the expert and the patient group. The conclusions are then shown, including future lines of research. Appendix A shows the sensitivity analysis, and finally the references are given.
2. Literature Review
2.1. Background of the Problem
Environmental sustainability in health care organisations is increasingly being recognised and explored [9]. In fact, as described in Lenzen et al. [5], there is a growing need to understand the health impact and the environmental footprint of health care. This is because, as the amount of health care activity provided increases around the world, there is ever more potential for damaging health through pollution and climate change. Climate change due to increased greenhouse gas emissions causes a rise in diseases such as dengue fever [10], and in events that cause injury, such as heat waves, cyclones, floods, and droughts. These in turn lead to increases in demand for health care, costs, and greenhouse gas emissions [5]. Health care organisations may also set standards for other entities in their commitment to environmental protection and make a significant contribution to economic sustainability in health care [11].
Health care organisations are unique in that they produce all existing types of waste, from non-hazardous or general health care waste to potentially infectious waste, which may be carcinogenic, mutagenic, teratogenic, or radioactive. However, although only 15% of health care waste is considered to be hazardous [12], the improper sorting of waste mixes the two types, leading to a much larger quantity of dangerous waste [13]. This increases the risk of infections, toxic effects, and injuries to care and non-care staff, waste handlers, patients and visitors, and the wider community. To this should be added the risk of environmental pollution from the dangerous combustion gases produced by incineration of this waste or its build-up in rubbish tips, and the difficulty of designing strategies for recovery and recycling of non-hazardous waste [14]. Furthermore, waste management should satisfy the principles of the circular economy, producing items that are highly reusable, and recycling materials that do not contain dangerous compounds, or from which they can be removed. However, infectious material contains blood or other bodily substances which do not currently have circular-specified techniques to create value, or they require excessive energy consumption. Traditional linear solutions, using the sequence extract-produce-consume-dispose, cannot, therefore, be completely discarded [15].
A successful environmental sustainability programme has a number of advantages for the organisation:
- Performance of the organisation is improved in terms of efficiency and effectiveness. These improvements are linked to improved outcomes in clinical results, the experience of staff and patients, system reliability, and company culture.
- Risk is reduced, given the regulatory control of energy consumption and waste disposal.
- Costs are reduced, due to lower resource consumption and waste production.
All this also leads to improvements in the positive perception of the organisation by society, due to the conservation of scarce natural resources and the promotion of the health of patients and staff [16].
This problem can be seen at a global level, as although in middle and low-income countries, health care waste generation is usually lower than in high-income countries [17], it is also true that, in the former, hazardous clinical waste is not generally sorted from non-hazardous waste, and the quantity of hazardous waste is in fact much greater. There is also a growing trend of increased access to health care services [3], and in some cases no rigorous estimate of medical waste generation based on scientific studies is carried out [18]. In developed countries on the other hand, ageing populations lead to greater hospital use. This all leads to an overall increase in production of clinical waste. Furthermore, comparison between countries is practically impossible due to differences in legislation, services, waste management systems, etc. [3]. Although Patwary et al. [18] suggest that it would be more reliable to compare the most economically developed countries, in practice, such a comparison is even seen to be difficult between hospitals in the same country. This is because, for example, each hospital sets its own procedures for data collection, the variables to be controlled, environmental performance reports, etc., and so it is almost impossible to apply benchmarking.
In Spain, specifically, up to a decade ago, state-run hospitals put no effort into sustainable initiatives. However, although there is now a positive trend in this regard, there is also a clear lack of guidelines and homogeneity in sustainability planning, as well as there being no assessment stage as to the outcomes of the sustainability initiatives put into practice. Public hospitals, moreover, are not willing to compare their sustainability initiatives with those of other hospitals. This means that there is no opportunity to use benchmarking [4]. This is also true in other countries [19].
It is thus essential to have objective tools to monitor environmental sustainability in health care organisations in order to make informed decisions about health care practices, and strategical activities or processes [20] and costs, but primarily to prevent or at least minimise negative environmental impact, in turn reducing the impact they may have on health [5]. Sustainability assessment is increasingly recognised as an effective analytic methodology and management tool for improving sustainability performance [6], within a process of continuous improvement.
There are still important gaps in the literature regarding sustainability in hospitals, although we are starting to see assessments of environmental impact and the use of natural resources, both in individual hospitals and over an entire health system [21]. However, there is no case in the literature of an environmental assessment system for health care organisations which takes into account the various stakeholders. The interests of stakeholders coincide in many areas, but in others there are in conflict, and so taking into account the opinions of various stakeholders, such as patients and experts, provides a fuller vision of the level of environmental sustainability valued by the community.
2.2. MCDA Methods in Environmental Sustainability
Contributions on sustainability performance in private and public health care organisations are very scarce [4], despite the importance of sustainability in this sector.
The problems in quantifying sustainability stem from using only qualitative aspects, and because different stakeholders, such as policy makers, social scientists, economists, engineers, patients, etc., tend to identify different sustainability criteria or indicators depending on the particular class of application [22].
Multicriteria decision analysis (MCDA) techniques help decision makers simplify a complex problem by breaking it down into three elements [23]:
- Alternatives to be assessed (options, strategies or action plans).
- Objectives or aims and criteria by which the alternatives will be assessed.
- Criteria weights which bring together the judgements, knowledge, information, etc., of the decision makers.
A MCDA model can include both quantitative and qualitative information, as well as different stakeholders, scenarios, goals and a variety of aspects to be assessed. The complexity inherent in the decision-making process is further complicated by the often incomplete or vague nature of the information available [24]. MCDA addresses this problem by including uncertainty methodologies such as sensitivity analysis, validation, probability models, fuzzy set theory and grey systems theory [25]. In any case, it is an indispensable condition that the decision-making process be simple and compressible to decision makers. It is these characteristics that make MCDA techniques very useful in environmental assessment [26,27], since multiple technical, social, political, economic, and environmental matters are usually involved, which may frequently conflict [28,29]. It can also be useful to include a number of decision makers with different responsibilities in the Health Care System. Although there are many MCDA techniques, and no technique is universally preferable to the rest, there do exist techniques that are more appropriate to a given problem and the features it involves [30].
MCDA techniques allow objective models to be designed, as they are built with mathematical techniques, and so they can help to ensure public acceptance of the results [31]. This question is very important to a health care organisation since in most cases, in Spain at least, they are publicly owned. This means that the use of these techniques increases the consistency, transparency, and legitimacy of decisions [32].
There is an extensive literature, which successfully uses different MCDA methods to assess environmental sustainability and/or environmental impact [7,31,33]. Sustainability assessments based on MCDA are generally seen to cover the three dimensions of sustainable development, economic, social, and environmental, although they mainly focus on environmental impacts [34]. However, environmental aspects are not always analysed from the life cycle perspective. Also, the models designed do not provide a wholly quantitative assessment of the economic and social questions [35]. It was found that nearly all the MCDA methods available have been used, although the analytic hierarchy process (AHP) is the leading technique.
Among the contributions that use one or more multicriteria techniques in a crisp environment are the following. Stefanović et al. [36] compared the results obtained with AHP and the analysis and synthesis of parameters under information deficiency (ASPID) method to assess sustainability of waste management scenarios. The best sustainable waste management scenario is found to be similar with both methods, and is related to composting of organic waste and recycling of inorganic waste. Büyüközkan and Karabulut [37] integrated AHP, for determining the weights of the evaluation criteria, and VIKOR for ranking energy project alternatives, to assess and rank the sustainability performance of one thermal power and three renewable energy projects. Loikkanen et al. [38] applied stochastic multicriteria acceptability analysis (SMAA) to the assessment of sustainable energy solutions such as different configurations of solar power, ground source heat, and roof constructions, along with district heating for a building. Talukder and Hipel [39] used the Preference Ranking Organization Method for Enrichment Evaluation (PROMETHEE) method to assess sustainability, using the productivity, stability, efficiency, durability, compatibility, and equity of agricultural systems in coastal Bangladesh. Melkonyan et al. [40] analysed sustainability in last-mile logistics and distribution strategies, also estimating the impact of dynamic changes on the design, using the PROMETHEE. Ziemba [41] looked at strong sustainability from the perspective of a limited capacity to replace certain natural capital with other kinds of capital. This was done using PROMETHEE for sustainability assessment (PROSA), a method that is more flexible in its choice of criteria and groups, and that offers the decision maker more analytical possibilities, allowing the expected strength of the sustainability to be defined. Deshpande et al. [35] assessed the environmental, social and economic impacts of landfilling, incinerating, and recycling of waste fishing gear through two scenarios, i.e., recycling inland and exporting, using multi-attribute value theory (MAVT). Khan [42] used a simple multi-attribute rating technique (SMART) to assess sustainability in the power generation sector in Bangladesh in a model built with 19 sustainability indicators, of which 10 concern social factors, four environmental, and five economic. The result was to show that the sustainability of the power generation sector will deteriorate in the future.
Research on environmental sustainability in the fuzzy environment is very scarce, but the following studies should be noted. Hu et al. [43] created a framework based on the Global Reporting Initiative Guidelines, a kind of scorecard for assessing the quality and the content of sustainability reports from 16 companies operating in Taiwan. A fuzzy Delphi method with expert questionnaires was used to choose 44 indicators structured into 18 criteria. Subsequently, the fuzzy AHP was used to calculate the weights of the criteria and give a score to each sustainability report. Ezbakhe and Pérez-Foguet [7] used a modified elimination and choice translating reality (ELECTRE) III model to incorporate the uncertainty in the decision process, and so determine discrimination thresholds for planning renewable energy in Turkey. The model was compared with other research which used three different MCDA techniques with the same goal, namely fuzzy set theory combined with AHP, used by Kahraman and Kaya [44], fuzzy AHP and fuzzy technique for order preference by similarity to ideal solution (TOPSIS) by Erdogan and Kaya [45], and modified ELECTRE in a hesitant fuzzy sets environment by Mousavi et al. [46]. In all these studies, considering a veto-to-preference ratio of eight in Ezbakhe and Pérez-Foguet [7], the findings are that wind energy is in first place, followed by solar, geothermal, biomass, and hydropower.
A further review of the literature on environmental questions analysed via MCDA techniques can be seen in Huang et al. [31], Büyüközkan and Karabulut [34], Kiker et al. [47], Herva and Roca [48], and Neste and Karjalainen [49].
An increasing number of contributions combine geographic information systems (GIS) and MCDA techniques, as they can potentially support the solution of a wide variety of environmental decision and assessment problems, according to multiple criteria and decision makers’ preferences. Among them is Boggia et al. [50] which described a model for sustainability assessment integrating TOPSIS with GIS to obtain a traceable and transparent system using a set of indicators structured in the economic, social and environmental sectors, to attempt balance between the three dimensions of sustainability. Jelokhani-Niaraki et al. [51] focused on the semantic interoperability of GIS and MCDA, using an ontological framework to assist in environmental assessment and decision making.
However, in the area of health care organisations, environmental assessment is only beginning to be carried out, both for individual hospitals and for the health system in general [21]. The literature includes some contributions analysing the assessment of environmental issues in health care organisations, for example, with respect to guidelines, ESC [52] provided practical advice to help health care facilities improve their environmental management systems and performance. CMPBS [53] provided a guide for a self-certifying metric toolkit of best practice that designers, owners, and operators can use to assess their evolution towards high-performance environments. The World Health Organization identified the elements of a climate-friendly hospital [54]: energy efficiency, green building design, alternative energy generation, transportation, food, waste and water. Smith [55] analysed the concept of sustainable health care. Intraruangsri [56] broke down the idea of a green hospital to analyse the evolution of the concept, and the guidelines for applying it successfully.
McGain and Naylor [21] identified the following essential areas of environmental sustainability in hospitals: hospital design, direct energy consumption, water, procurement, waste, travel and psychology and behaviour. Pinzone et al. [57] analysed the role of green human resource management practices on the environment. Castro et al. [58] set out a method for assessing the sustainability of health care buildings by means of a list of indicators and considering the perspectives of the main health care stakeholders. Ref. [59] continued with that aim, but introduces the concept of sustainable-effective design, adapted to the Portuguese building sector. Kleber [60] described the potential role of nurses in waste reduction in hospitals, by unifying and involving staff in shared governance models. Carino et al. [9] identified the environmental and associated economic impacts of hospital food services and the results from different strategies that can improve the environmental sustainability of food services. Factors to bear in mind include the importance of commitment and communication between the hospital and local stakeholders in achieving environmentally sustainable food services, and also control processes to minimise the production of food waste, and bring about the long-term sustainable sourcing of some of the ingredients. Nutritionists should also analyse the environmental sustainability of the food services in hospitals.
In a more quantitative and practical way, Nascimento et al. [16] assessed the level of sustainable practices with an environmental dimension in Brazilian hospitals. Areas such as operational performance, where ISO 14,001 certification, the publication of sustainability reports, and the existence of an area dedicated to corporate sustainability are looked at, together with the maturity of hospitals in relation to sustainability practices. 58% of the hospitals surveyed returned the rating very high or high, but additional sustainable actions are recommended, such as establishing dialogue with stakeholders. Also looking at Brazilian hospitals, Blass et al. [19] developed a practical framework to measure environmental performance. The framework includes three phases, eight steps and fourteen worksheets, and has been applied to six hospitals, helping them to comply with current legislation and quality standards. Tomson [11] describes a set of actions to minimise greenhouse gas emission in hospitals, with the categories reduction in pharmaceutical use, more efficient use of buildings, waste reduction, reduction of energy use, sustainable procurement, health care activity for hospital staff and the community (reducing obesity and smoking), separation of emergency and elective care, telemedicine, improvements in monitoring of chronic illnesses by patients (activated patients), improvements in end-of-life care and reform of the payment system. The study of Thiel et al. [61] was along similar lines, but it focused on laparoscopic surgery, and showed that the greatest savings in carbon footprint were in the choice of specific anaesthetic gases, and minimising the materials used in surgery (reusing cotton towels, switching to reusable gowns and drapes, etc.). In addition, optimising energy use, specifically heating, ventilation, and air-conditioning systems can contribute to a reduction of 10% in the carbon footprint, and recycling surgical waste, 5%. Lenzen et al. [5] assessed the contribution of health care organisations to environmental damage, and found an environmental impact of between 1% and 5%, depending on the indicator used, and over 5% in some countries. For example, in emissions of greenhouse gases and air pollutants, health care organisations have a high footprint: 4.4% of greenhouse gases, 2.8% of particulate matter, 3.4% of NOx, and 3.6% of SO2. These are mainly caused by transporting patients and heating buildings and water.
There is research that includes MCDA techniques in these assessments in the health care organizations, although it is very limited. It includes the following contributions in the crisp environment. Romero and Carnero [62] built a model with the AHP, with the aim of facilitating recognition of Standard ISO 14,001 or Regulation EMAS. The model uses a total of 54 indicators classified into three categories: environmental behaviour, environmental management and environmental condition. This classification follows the recommendations of the Commission of the European Communities for the application of Regulation (CE) nº 761/2001 [63]. Five alternatives are used to classify a hospital, according to the level of satisfaction of the indicators: excellent, very good, good, deficient and very deficient, as well as the alternatives maximum and minimum which characterise a hospital with the highest and lowest level respectively in all the indicators. Zamparas et al. [64] built an AHP model to assess procedures, techniques and methods of handling infectious waste in the health care unit of a general hospital in Greece. Staff/patient environmental sensitivity was included in the criteria, patient judgements were not considered, as three experts in health care organisations were used. The resulting values are very good in environmental management, due to good behaviour in environmental policy standards and waste management procedures. However, staff sensitisation programmes, and other actions on green procurement, should be developed.
In the fuzzy environment, the following stand out: [65] built a model using fuzzy AHP with utility functions to evaluate the quantitative criteria. This model was applied to a public (state-run) hospital, and gave a valuation of 0.764 out of 1, showing that this type of model can play a positive role in the process for certification to Standard ISO 14001. However, as the hospital performs a different number of care services each year, comparing results between years, or between organisations, is complex. Carnero [8] described a model combining fuzzy AHP and utility theory to evaluate environmental sustainability in health care organisations. The model assesses the quantitative criteria, looking at the number of services provided annually by the organisation, meaning that the results are comparable over time, and between different health care organisations. The model has been applied to a hospital and to a walk-in centre which only treats out-patients, and it shows when given actions carried out in a given year have made a greater contribution to environmental sustainability.
It should be underlined that the inclusion of a variety of stakeholders in decision models, as a success factor in performance assessment models, is increasingly common [66]. However, this is not true of environmental performance in health care organisations. Nonetheless, there is a need to include in the model the people directly involved in the production and handling of health care waste, such as care and non-care staff of the health care organisation or policy makers. In addition, environmental bodies, environmental health practitioners, voluntary groups, advisers, researchers and students should also be considered [67], and the general population, due to broader environmental awareness, and the need to reduce public spending and the introduction of stronger environmental regulations. Also, the public is aware of real problems in this area, as they suffer environmental problems daily [30]. Thus, ensuring that the results obtained are easily intelligible to non-experts, and that the assessment is traceable and transparent [50], is key in the production of assessment models.
2.3. Conclusions from the Literature Review
In conclusion, in the literature review, there are a number of missing features to do with sustainability focused on the environment that need to be addressed, and to which it is hoped this research will contribute:
- The application of internal and competitive benchmarking within and between health care organisations over time.
- The inclusion of a variety of stakeholders in the decision process.
- The choice of a MCDA technique to assist in building a model involving various stakeholders.
- The inclusion of uncertainty due to incomplete, imprecise or vague information, which at the moment is still a challenge [7].
- Assessment of sustainability in health care organisations exclusively uses AHP and fuzzy AHP. Application of other techniques would make for an interesting point of comparison in the literature.
3. Fuzzy TOPSIS
Fuzzy TOPSIS was chosen over other techniques, principally fuzzy AHP, which is the technique mainly used in the fuzzy environment, for the following reasons. Fuzzy TOPSIS imposes no constraints on the number of criteria and alternatives [68]. AHP and fuzzy AHP, however, are limited to the use of nine criteria and alternatives, so as not to compromise human judgment and its consistency. Although in this paper the model was applied over five consecutive years, and so it considers five alternatives, the goal is to apply it over time, and so it is necessary that many alternatives can be assessed or applied over many years. Fuzzy TOPSIS does not have the problem of rank reversal which exists in other techniques such as fuzzy AHP. With time, the model could require the addition or elimination of criteria. According to the study of Lima et al. [69], when a criterion is added or removed in fuzzy TOPSIS, there is no change in the order of importance of the remaining criteria. With regard to the number of judgements required, if is the number of alternatives and the number of criteria, fuzzy TOPSIS requires judgements. This number is much smaller than in other techniques. As the number of criteria and alternatives increases, for example, in the model with nine alternatives and nine criteria, fuzzy TOPSIS requires four times fewer judgements than fuzzy AHP. It can therefore be said that fuzzy TOPSIS works better than fuzzy AHP with respect to interaction with decision makers for data gathering. In this sense, fuzzy TOPSIS gives greater agility to the decision process than fuzzy AHP. Looking at computational complexity, fuzzy TOPSIS requires a total of operations, while for example fuzzy AHP, including the consistency tests, needs operations. Thus, fuzzy TOPSIS behaves slightly better than fuzzy AHP as the number of alternatives increases. Although there are many methods that allow aggregation of judgements from more than one decision maker, aggregation of criteria weights and ratings of alternatives given by k decision makers is explicitly considered in the application procedure of fuzzy TOPSIS. Also, the participation of a large number of decision makers, as required by the model studied here, through the contribution of the group of patients, increases the time complexity less than other techniques like fuzzy AHP. Fuzzy TOPSIS is recognised as a suitable technique for solving group decision-making problems in a fuzzy environment [70]. Furthermore, fuzzy TOPSIS is simple and yields an unarguable preference order, although each attribute should only have an increasing or decreasing utility [71]. Furthermore, it is the second most-used fuzzy MCDA technique in the literature, after fuzzy AHP, and the likelihood that this will continue to be true is also recognised [72]. It has been successfully applied to many real-world problems, as noted in the literature review of Salih at al. [73]. For all of these reasons, fuzzy TOPSIS was chosen rather than other fuzzy MCDA methods.
The fuzzy environment allows judgements to be given using fuzzy numbers rather than crisp numbers, making the job of the decision maker easier. Uncertainties, ambiguous information, or vagueness in the judgements of the decision makers can be included [74]. Decision makers are also likely to feel more confident giving interval judgements than crisp judgements [75].
There are many examples of the successful application of fuzzy TOPSIS to different areas and problem types. For example, for choosing a suitable security mechanism for e-business processes [76], in personnel assessment [77], selecting the most suitable IT outsourcing strategy in the banking environment [78], assessing banking strategies to minimise the effects of financial crisis [79], selecting enterprise resource planning (ERP) systems [80], choosing the most sustainable disposal alternative for the construction and demolition waste [81], assessing suppliers [82], selection of a mobile health application [83], evaluation of sustainability of electric vehicle development [68], etc.
A triangular fuzzy number (TFN) , is denoted by is defined by a membership function as shown in Equation (1) [84].
with , where the lowest possible value, the modal value or the most promising value, and the largest possible value of the fuzzy number [85].
The algebraic operations of two triangular fuzzy numbers and are [86]:
In a decision problem with criteria and alternatives , the best alternative in fuzzy TOPSIS is the one that has the shortest distance to a fuzzy positive ideal solution (FPIS) and the farthest distance from a fuzzy negative ideal solution (FNIS). The FPIS is an alternative that maximises the benefit-type criteria, and minimises the cost-type criteria, while the FNIS works the other way around [87].
In fuzzy TOPSIS, the criteria should satisfy one of these conditions, to ensure they are monotonic:
- (a)
- As the value of the variable increases, so do the values of the other variables.
- (b)
- As the value of the variable increases, the values of other variables decrease.
The weights of the criteria are assigned directly by the decision makers through linguistic variables, that is, variables whose values are words or sentences defined in a natural or artificial language. These linguistic variables are very useful for handling situations that are too complex or are not correctly defined and so cannot be reasonably described by conventional quantitative expressions [88]. The linguistic terms of each linguistic variable are translated into TFNs on the interval [0, 1] [87]. The linguistic scale used to calculate the weights of the criteria can be seen in Table 1.

Table 1.
Linguistic scale for the weights.
A fuzzy multicriteria decision-making problem can be expressed by a fuzzy matrix as shown in Equation (8) [88].
where is the performance ratio of alternative with respect to the criterion evaluated by the kth decision maker and .
The aggregate fuzzy weights of each criterion given by k decision makers are calculated using Equation (10).
The ratings of alternatives with respect to the criteria are evaluated using the linguistic scale in Table 2 [88]. Different linguistic scales for the criteria weights and ratings are used by different authors (see for example [85,89,90]), however, this study uses the original definitive scale from Chen [88], and used, for example, by Kutlu and Ekmekçioğlu [91].

Table 2.
Linguistic scale for the ratings.
To avoid the complicated normalisation formula used in TOPSIS, the linear scale transformation is used to transform the scales of the different criteria into a comparable scale. This gives the normalised fuzzy decision matrix denoted by and guarantees that the ranks of the normalised fuzzy numbers are in [0, 1] [91].
with
in benefit-type criteria
in cost-type criteria
It is now necessary to bear in mind the importance of each criterion, and so the fuzzy weighted normalised decision matrix is calculated from Equation (12) by multiplying the weights of the criteria , by the elements of the normalised fuzzy decision matrix.
The positive ideal solution allows the benefit-type criteria to be maximised, and the cost-type criteria minimized, whereas the negative ideal solution minimises the benefit-type criteria and maximises the cost-type criteria. The FPIS and PNIS are determined from Equations (13) and (14), respectively [90].
The Euclidean distances and of each weighted alternative from the FPIS and FNIS are calculated using the following equations, by the vertex method described in Chen [88].
The closeness coefficient must then be calculated, , for each alternative i using Equation (19) [90].
The classification of alternatives is obtained in descending order of value. The best alternative is the closest to the FPIS and the furthest from the FNIS [91]. However, there are cases, such as when assessing risk, that the alternative with the lowest is chosen.
4. Fuzzy TOPSIS Model for Assessment of Environmental Sustainability
The model has been applied in a public hospital that has been operating for over 35 years. It offers 30 specialities, 397 beds, 15 operating theatre and 1744 staff, providing health care to 313,000 inhabitants. The hospital has taken part in the European project towards zero-carbon hospitals with renewable energy systems (RES), and expects, in the medium term, to get over 50% of its energy production from renewables. In 2005 it introduced an environmental management system and is certified to Standard ISO 140,001 and European Regulation 1221/2009 (EMAS III). It also has its carbon footprint certified, and has GRI certification in corporate social responsibility, with a++ rating. In 2010 it started the ‘Green Hospital’ project, and won an award for its environmental work.
4.1. Structuring
The choice of criteria and subcriteria takes account of environmental declarations from different health care organisations, since the model is limited to obtaining data from public environmental declarations. The model uses the criteria defined by the Galdakao-Usansolo Hospital [8,65,92] which allows for an assessment to be made of most health care organisations. The criteria and subcriteria considered by the model are as follows:
- Annual water consumption (AWC). The annual consumption of water provides a measure of the suitability of the actions taken by the hospital to reduce it. These include the introduction of thermostatic taps and timers, low consumption systems in showers and baths, insulating conduits and storage tanks, using controlled service pressures, etc.
- Annual energy consumption. Two subcriteria are considered:
- ○
- Annual energy consumption (MW/h) of electricity, refrigerating energy, thermal energy and natural gas (AEC). Evaluating this criterion allows analysis of the impact of actions such as installing insulation and changing windows, installing energy-saving devices in lighting and replacing bulbs with low-consumption versions, reprogramming air-conditioning timers, zoning, recovering energy from extracted air, carrying out an effective preventive maintenance programme, installing an energy management system, etc.
- ○
- Annual renewable energy consumption of (ARE). This assesses the quantity of energy consumed from renewable sources, mainly by installing solar panels, biomass, and geothermal energy, for heating and refrigeration systems, or heating the water in the therapy pool.
- Environmental accidents and incidents (EAI): Environmental accidents that occur in a health care Organisation can affect the infrastructure, equipment and the people in the hospital, and/or the surrounding community. In the former case the seriousness of leaving the population without health care until the situation is under control must be considered. In both cases the peak in demand which might occur as a result also needs to be considered. As does the damage to the image of the hospital due to the inability to serve the community and as a source of risk. Competitive advantage is also reduced when compared to other health care organisations. Environmental incidents, although not as serious as environmental accidents, should be analysed and their causes eliminated as soon as possible, and may lead to internal non-compliance with Standard ISO 14001, requiring analysis of the cause, and corrective action. This criterion, therefore, evaluates the existence in the hospital of internal and external emergency plans, with action procedures ready for previously analysed risks, as well as plans to prevent or reduce risks, and recovery plans for affected areas. The number and seriousness of accidents and incidents that occur annually are evaluated, for example, unsuitable storage of waste or chemicals, fires, leaks, or escapes of dangerous chemicals, etc.
- Biodiversity (BIO): There is a further assessment of the impact of the hospital on the environment, and actions taken to make continuous improvements to this impact. Adaptation to the rural and forest environment is looked at, as well as care of protected or endangered species within the categories of the International Union for Conservation of Nature (IUCN) or on national lists, living in the area around the hospital.
- Activities to promote and disseminate environmental issues (APD). There is an assessment of activities, mainly practical, undertaken annually, which encourage cycling and walking, as well as the use of electric or hybrid vehicles, public transport in the community for trips to the hospital, etc. Also, other actions may be contemplated, such as seminars on the environment, mobility, ecological menus, photography competitions, participation in congresses, exhibitions, making of posters and triptychs, etc. The possibility should also be considered of producing an annual environmental audit, available to the community, a declaration of greenhouse gas emissions, and spreading messages of awareness and sensitivity among staff, patients, and visitors.
- Training and evaluations on environmental matters (TAE). Training programmes in environment matters, especially in sorting of waste, applied both to care and non-care staff, are assessed. The existence of dedicated groups to analyse and solve environmental problems, and encouragement of the co-operation of the whole organisation in this area. Programmes for collecting suggestions, complaints, opinions and surveys about environmental questions and their efficient management are analysed. Certification of the organisation to standards such as ISO 14001, Regulation (EC) No 1221/2009 of the European Parliament and of the Council of 25 November 2009 on the voluntary participation by organisations in a Community eco-management and audit scheme (EMAS), ISO 14,064 (on reporting of greenhouse gas emissions), etc. is assessed, as is participation in hospital networks or national or international environmental projects, such as the Global Green and Healthy Hospitals Initiative (see https://www.greenhospitals.net/) which monitor different environmental issues.
- Noise pollution: Noise pollution has important health effects (both physiological and psychological, see [93]), and can affect the effectiveness of patient treatments, and their improvement and rest, as well as the health of all the workers in the organisation. This criterion comprises the following subcriteria:
- ○
- Noise inside the hospital (NIH). This should not exceed 30 dBA, and optimum noise is between 15 and 25 dBA.
- ○
- Noise outside the hospital (NOH). This should not exceed 55 dBA, and optimum noise is between 35 and 45 dBA.
- Waste production: Assess annual waste production. This is divided into the subcriteria:
- ○
- Group I waste (GIW). This is general waste, with no risk, such as edible oils, plastics, paper and cardboard, clothes, glass, etc.
- ○
- Group II waste (GII). Sanitary waste that may be treated as urban waste.
- ○
- Group III waste (GIII). Dangerous waste products, including industrial oil, batteries, non-halogenated solvents, chemical waste, radiology liquid, out-of-date or retired medicines, anatomical remains with formaldehyde, cytostatic waste, etc.
Other waste, in other groups, including radioactive waste, is subject to special legislation which must be complied with, and so is not included in the assessment system.
- Green purchasing (GPU): Including ideas of circular economy in procurement (optimising purchasing of food, pharmaceuticals and other materials, to minimise waste, purchase recyclable items or that contain recyclable materials, reuse of equipment, etc.). Also considered is the choice of local suppliers from km 0, purchasing items with lower environmental impact, that minimise energy consumption (energy labels or energy stars), including conditions in the contracts to guarantee respectful treatment of the environment at all stages of production and packaging, or using suppliers and outsourcers that are certified in environmental standards.
The criteria and subcriteria will be assessed with respect to annual number of consultations, hospital stays and emergency services offered by the health care organisation. Although it would have been possible to include the hospital workforce, made up of both care and non-care staff, who use resources on a daily basis, it has not in fact been included in the calculation of services provided, as it remains largely stable over time. This allows the results to be compared over time in a hospital, and between different hospitals [8].
Although it would have been possible to include further criteria, such as consumption of specific materials, it should be borne in mind that the model needs to be stable over time, and some of the materials analysed in health care organisations are being replaced by other materials, or are ceasing to be used. This is, for example, the case of glutaraldehyde, which has been replaced with peracetic aid, or x-rays, which have for some years been exclusively digital. There was also an intention to keep the model as simple as possible, so that patients can give judgements, including very specific materials, about which they have no information, which would make these judgements too uncertain, and in many cases, patients would not answer.
4.2. Weighting
Firstly, an expert in environmental issues, using the fuzzy scale set out in Table 1, gave the judgements necessary to obtain weights for the criteria and subcriteria. A group of patients was also asked to assess the importance of similar criteria, using a similar fuzzy scale. The patient group was chosen randomly from among the people who wished to co-operate with the study. The judgements were given individually by each patient by filling out a questionnaire. Fuzzy weights of each criterion given by K patients were aggregated using Equation (18). Some criteria were not assessed by all patients and were left blank, so Equation (20) was particularised by the number of judgements given for each criterion.
Additional weights were obtained by combining the judgements of the expert and the patient group, the latter considered as one single decision maker. The judgements of the expert and of the patient group were given similar importance.
The initial values of the fuzzy multicriteria decision-making matrix corresponding to the evaluation of each alternative (year) in each criterion/subcriterion using the expert judgements are shown in Table 3. This assessment is made using the linguistic scale for ratings shown in Table 2. The patient group did not take part in the assessment of alternatives, as they did not have sufficient data and information to give reliable assessments of the hospital.

Table 3.
Initial values of the fuzzy multicriteria decision-making matrix corresponding to the assessment of each alternative (year) in each criterion/subcriterion by the expert.
The resulting fuzzy weights obtained from the expert, from the patient group and by combining the judgements of the expert and the patient group, are shown in Table 4. It can be seen that in general the fuzzy weights given by the patient group are less extreme than those of the expert, that is, the values are closer together in all the criteria. There is also agreement between the two decision makers in giving greater importance to criteria such as environmental accidents and incidents and Group III waste, and a similar importance to the criteria of training and cooperation on environmental matters and green purchasing. However, in the criterion of activities to promote and disseminate environmental issues, the patient group gave a much higher weighting.

Table 4.
Fuzzy weights.
These subjective weights are determined only by the preferences of the decision makers. This study, however, also considers the objective weights. These are found by solving mathematical models without any consideration of the decision maker’s preferences, for example, via the entropy method, multiple objective programming, etc. The objective weights are particularly suitable for situations in which reliable subjective weights cannot be obtained [94]. The most cited entropic measure of uncertainty is Shannon entropy [95].
Shannon and Weaver [96] proposed the concept of entropy, which is a measure of uncertainty in information expressed in terms of probability theory. Entropy is suitable for measuring the relative contrast intensities of criteria, in order to represent the average intrinsic information transmitted to the decision maker [97]. That is, the parameter can be used to measure the amount of useful information given by the data. The higher the entropy value in a criterion, the smaller the differences in the ratings of the alternatives with respect to this criterion. This implies that the criterion gives less information, and so has a smaller weight. The criterion is thus less important in the decision-making process [98].
Shannon set out three conditions for measuring the information in a communication stream. His entropy measure H satisfies the following conditions for all within the estimated joint probability distribution P [99]:
- H is a continuous positive function.
- If all are equal, , then H should be a monotonic increasing function of n.
- For all
Shannon showed that the only function that satisfies these conditions is:
where K is a positive constant that amounts to a choice of a unit of measurement, and is a discrete random variable with values ( on a finite set, which occur with probability .
In a decision-making problem comprising alternatives and criteria, the fuzzy decision matrix, , can be expressed as shown in Equation (22):
where the rating of the ith alternative con respect to the jth criterion.
The objective criteria weights can be found in the following way [100]:
- Construct the normalized fuzzy decision matrix using Equation (23).
- Calculate the Shannon entropy vector via:where or or are defined as 0 if , or are 0 respectively.
- Calculate the divergence vector with:The greater , the more important is criterion .
- Calculate the fuzzy weight vector for the criterion from Equation (25).
- Normalise the fuzzy criteria weights.
The weights derived by the Shannon entropy method are shown in Table 4. In the criteria Biodiversity and Noise inside the hospital, the weights are (0, 0, 0), as the hospital has the same results in all the five years assessed. Since it is the level of environmental sustainability in hospitals that is being assessed, rather than different solutions to a problem, the valuations in these criteria with null weights could change in future years, and so would it not be appropriate to exclude them from the study.
The data in Table 3 are normalised by means of Equation (11), and the results combined with the weights in Table 4, by means of Equation (12), to get the fuzzy weighted normalised decision matrices shown in Table 5, Table 6 and Table 7.

Table 5.
The fuzzy weighted normalised decision matrix obtained from the expert’s judgements.

Table 6.
The fuzzy weighted normalised decision matrix obtained from the patient group judgements.

Table 7.
The fuzzy weighted normalised decision matrix obtained from combining the judgements of the expert and patient group.
5. Results and Discussion
The distances and of each weighted alternative from the FPIS and FNIS are calculated using Equations (15) and (16), giving the results shown in Table 8. It is seen that the distances with respect to FPIS are greater when applying the weights of the expert than of the patient group, and so the distances with respect to the FNIS are greater in the case of the patient group weights. In the case of the combined environmental expert and patient group judgements, the distances of the first two years with respect to the FNIS are greater, while in the last three years, the behaviour is reversed, and the distances to the FPIS are greater.

Table 8.
Distances obtained from the expert, patient group judgements and combining the judgements of the expert and patient group.
The CC of each alternative for the expert and patient group weights separately are set out in Table 9, and the combined expert and patient group judgements in Table 10, using subjective and objective weights. The classification obtained using the weights from decision makers is the same in the top two positions, and in the fourth, as that obtained using Shannon’s entropy. From CC the rankings of the five years studied using the expert weights and the patient group weights separately, and when the judgements of both are combined, it can be seen that in all cases Year 2 has the highest score. In the case of the patient group and the combined judgements of the expert and the patient group, the first three years have a similar classification, with the first year in the second position and the third year in third. For Years 4 and 5, the classification from the results given by the expert, and the combined judgements from the expert and the patient group. Comparing Years 4 and 5 with the classification from the patient group, they switch between the 4th and 5th positions. The better behaviour in the first three years in all the models may be because in the early years the improvements introduced led to important reductions in water and energy use. However, continuing to achieve similar improvements becomes increasingly more complex the longer the continuous improvement plan is implemented, and a greater effort is necessary to obtain results that are usually lower, that is, the process is subject to the law of diminishing returns. Thus, the hospital must introduce additional projects that allow consumption to be further lowered. However, this is in agreement with the environmental management model, which is subject to continuous improvement thanks to the cycle plan-do-check-act (PDCA). Also, the worse behaviour of Years 4 and 5 is due to environmental accidents. In Year 4, the dangerous storage of chemicals was detected, and there was a leak in the gasoil tank in the cogeneration plant, and in Year 5, there was a coolant leak from a cooler. In Year 4, there were also complaints about high levels of noise coming from the air-conditioning units on the roof of the hospital. This problem was solved in Year 5 by installing silencers in the outlets of the air-conditioning units, limiting the exterior noise to 40 dBA. To this should be added that Years 4 and 5 saw lower consumption of renewable energy, which had already begun in Year 3. Furthermore, in Year 4, there was an unexplained increase in water consumption, which continued into Year 5, when a leak was found in the hot water circuit, and a loss of efficiency in the valves of the compressor cooling circuit, and so it was changed, from which time there has been a considerable reduction in water consumption.

Table 9.
Closeness coefficient with the environmental expert and patient group judgements from each year studied.

Table 10.
Closeness coefficient of environmental expert integrated with patient group in each year studied.
One of the environmental goals set by health care organisations is reducing different types of waste, which was assessed positively in the first three years. However, in Years 4 and 5 there is a reduction in the Group I waste, and a significant increase in Group II and III waste. Although this would be valued negatively by the model, a correction was required, as this effect is an indication that sorting processes are improving. For example, in Year 4, glass containers for medication are disposed of from this year as dangerous waste. This aspect was thus valued positively by the model.
It can be seen that the CC is slightly higher in all the alternatives when using the weights obtained from the patient group than using the results from the expert. However, the percentage of variation is below 10% in all the alternatives when comparing results obtained with different weights, with a mean variation of 6.59%. It would thus seem that the patients are slightly less demanding in environmental matters, despite the risk to them, those who accompany them and the community in general from bad environment management in hospitals, as they are one of the few organisations to produce all of the groups of environmental waste, and the negative effects on the health and comfort of patients and visitors, for example, from high levels of noise.
The patient group gives more balanced judgements in all the criteria, with minimal values of 0.575 for the central values of the fuzzy number judgement (in the criterion Green purchasing) and the highest central value is 0.875 (in the criterion Group III waste). Whereas for the environmental expert, water consumption, energy, and the production of Group III waste are the criteria with the greatest weight, and this is true in all three cases, for the patient group, the most important, in decreasing order of weighting (looking at mean value) are Group III waste (GIII), environmental accidents and incidents (EAI) and noise inside the hospital (NIH). Thus, in both cases the importance of Group III waste is acknowledged, but they do not agree on the other criteria. The criteria assigned least importance by the environmental expert are noise outside the hospital (NOH), activities to promote and disseminate environmental issues (APD) and Group I waste (GIW) or general waste. Meanwhile, for the patient group, they are, in decreasing order, training and assessment on environmental matters (TAE), biodiversity (BIO), and green purchasing (GPU). So, they do not agree on the least important criteria in the model.
Comparing the CC obtained by combining the judgements of the environmental expert with those of the patient group to those obtained only from the environmental expert, shows that the results are slightly better in every year in the first case, following the trend seen in the patient group. The variations are below 5% in all the alternatives, with a mean variation of 2.47%. Therefore, comparing the model combining the judgements from the two sources with those just from the patient group shows that all the results are lower, with variations below −5.05% in all the alternatives and a mean variation of −3.56%. Thus, the final model captures behaviour from the models built on the judgements of the expert and of the patient group independently. The similarity of the rankings with the weights with the combined expert and patient judgements was assessed using the value of similarity () coefficient [101]. This coefficient is strongly correlated with the difference between two rankings at particular positions, and the top of the ranking has a more significant influence on similarity than the bottom. Equation (26) is used to compute the coefficient.
where N is a ranking length, and are defined as the place in the ranking for the ith element in ranking x and ranking y, respectively. If the coefficient is less than 0.234, then the similarity is low, and if it is higher than 0.808, then the similarity is high [101]. In the similarity assessment performed in the case of the ranking obtained from the judgements of the expert and in the ranking produced from the patient judgements. Therefore, in both cases, the similarity is high, but it is higher for the ranking obtained from the patient judgements. If the weights calculated using Shannon’s entropy are used, .
Assessment results for the alternatives can be defined absolutely according to their CC. The interval of CC is divided into five subintervals and linguistic variables are set for each subinterval. The assessment status and value interval of CC are defined in Chen et al. [102] applied to the assessment of suppliers. A similar concept was used in our study, but associating subintervals with excellence levels in hospital environmental performance, as shown in Table 11. All the alternatives proposed are in the interval , which implies a low risk of a serious environmental problem in the hospital. Nonetheless, it also implies that there are important opportunities for continuous improvement.

Table 11.
Excellence status.
The sensitivity analysis carried out on the models can be seen in Appendix A. The results obtained show that the models constructed are robust.
6. Conclusions
Health care organisations have broadened their involvement with corporate social responsibility, as the number of services provided in countries around the world has also increased. As well as health care to people, improvements in environmental sustainability improve the health of the community, as the combined effects of climate change, chemical pollution, and the use of unsustainable resources worsen the incidence of illness around the world. However, health care activity itself has negative effects on world pollution via the products and technology it uses, the resources it consumes, the waste it produces and the buildings it constructs and operates.
Despite the importance of this type of organisation to the environment, studies performing environmental assessment are only just beginning, and those that use objective tools like fuzzy MCDA techniques are very scarce.
This research presents a fuzzy multicriteria model for assessing environmental sustainability in health care organizations. The intention is to build a consistent, transparent objective model, which shows the legitimacy of decisions, ensuring public acceptance of the results obtained.
The model was tested in a public health care organisation over five consecutive years, showing how the improvement actions undertaken increase the overall utility of the result, and how, as important improvements are achieved, the model demands new actions on a similar scale due to the law of diminishing returns. The weights obtained from the environmental expert and from the patient group were applied independently in the model. The ranking of alternatives is the same in first place, and there are switches between the second and third, and between the fourth and fifth positions. The closeness coefficients obtained with the weights of the patient group are on average 6.59% higher than the closeness coefficients obtained from the expert. This higher value in the results obtained from the patients is observed in all the years studied. In general, the weights from the patient group are more balanced, while those of the environmental expert are more extreme. Additionally, the model is applied with a combination of the judgements from the expert and from the patient group. The ranking in this case is similar, in the top three positions, to that obtained with the judgements of the patient group, and a similar ranking in the fourth and fifth positions to the results obtained from the judgements of the expert.
In any case, the values of the closeness coefficient are on the interval , and so according to the defined excellence or assessment status, they have a low risk of a serious environmental problem in the hospital.
The use of the judgements from the patient group is intended to take into account the ever greater need to include judgements and opinions of the different stakeholders in decision and assessment processes in the hospital environment, since, for example, patients may be affected by environmental problems when they visit the hospital.
Fuzzy AHP and fuzzy TOPSIS are the most commonly-used fuzzy MCDA techniques in the literature [72] and have been successfully applied in many real-world problems [73]. However, this study uses fuzzy TOPSIS because it places no constraints on the number of criteria and alternatives included in the model [68]. It does not suffer from the problem of rank reversal. If the model requires an update, by including or removing some criterion, there is no change in the order of importance of the remaining criteria [69]. Fuzzy TOPSIS works better than fuzzy AHP with regard to the level of interaction with the decision makers in the data gathering. It has an explicit aggregation procedure for the judgements of different decision makers. For these reasons, fuzzy TOPSIS is recognised as a suitable technique for solving group decision-making problems in a fuzzy environment [70]. However, as future lines of research, it would be interesting to combine fuzzy TOPSIS with the measuring attractiveness by a categorical based evaluation technique (MACBETH), and compare the results obtained by the two methodologies. MACBETH has a series of advantages that affect the precision of the results, such as the creation of reference levels in the scales associated with each descriptor defined for each criterion.
In addition to the similarity coefficient , used to analyse the similarity of the rankings with the weights from integrating judgements of the expert and of patients compared with the weights from the expert and patient group, the similarity confirmation method described by Zhuang et al. [103] can be applied to determine whether two score vectors are from an identical population and/or have an identical distribution, in order to confirm the similarity of the final rankings, which is directly observable.
New technologies, which are being developed under the concept Industry 4.0, could have important effects on energy efficiency, pollution and waste reduction, such as, for example, intelligent climate management, optimisation of lighting supplies (combining the level of natural lighting of the building with pre-set schedules and presence detectors), tools for traceability of industrial waste, remote detection of leaks in water supply infrastructure, use of sensors and artificial intelligence in monitoring of air, noise and electromagnetic radiation, to improve the environmental quality, or the use of technology in waste collection to optimise collection routes, allow user recognition to know who places what in each container, among other possibilities. It is also possible to include moving structures on the facade, in order to block direct sunlight which, at certain times of year, heats the inside of the building. All these systems have their own switches and sensors which must be operated by their own controls, integrated into the building management system (BMS). That is, there must be a multiplatform to gather data and, through big data, integrate all the information from the building, in order that the hospital as a whole can be managed in the most efficient environmental manner possible. Monitoring of the different model criteria will therefore serve as a quantifier for the environmental sustainability of the improvement actions taken with respect to Industry 4.0. This could serve to spur other hospitals to introduce new technologies. Moreover, advances in telemedicine will reduce visits to hospitals, saving resources, reducing noise and waste in hospitals. This all contributes to giving hospitals a lower carbon footprint, reduced environmental impact and improvements in the wellbeing of patients, visitors, and staff of the health care organisation. The influence on the environment of these important changes in the health context could also be monitored with the system described here.
This model should be periodically updated with the introduction of new criteria, or by changing the definitions of the criteria defined in the model. For example, clinical, psychological or social factors that influence how health care professionals use resources, travel to/from hospital, and interact with the buildings and technologies available, are questions that could be addressed in future research.
Additional judgements from experts, patients or other stakeholder groups, such as, for example, the directors or managers of hospitals, and heads of care and non-care areas (such as those in charge of maintenance, logistics, environmental issues, etc.) should be included in the research to obtain more accurate weights.
The United Nations (UN) Environment Programme [104] declares that, during the current outbreak of COVID-19, there has been an increase in the volume of hazardous healthcare waste produced. It is estimated that each coronavirus patient produces 3.4 kilos daily of waste considered hazardous in Asian cities, and from 2.0 to 2.2 kilos per patient per day in Mexico, for example. Among the risks and challenges associated with waste management during the COVID-19 pandemic, according to the UN, are: increased infectious waste generation, interruptions to healthcare waste management services, improper healthcare waste management treatment in situ, suspension of recycling activities, and insufficient capacity for waste treatment and disposal. It should be considered that the available guidelines on healthcare waste management were produced assuming a society operating under normal conditions, rather than in the middle of a pandemic. It is therefore necessary to introduce new policies and guidance for handling healthcare waste during the COVID-19 pandemic, considering that additional capacity and resources are required to maintain compliance with proper waste management. Incorrect handling of this increasing quantity of hazardous healthcare waste may give rise to a rebound effect, both for human health and for the environment, hence the vital importance of safe handling and disposal as part of an efficient emergency response. It would be interesting, therefore, to perform an environmental analysis of the years in which the hospital was treating patients with COVID-19, as a large increase in dangerous waste has been observed, due to the treatment of far more patients with infectious diseases than in previous years.
Funding
This research was funded by the University of Castilla-La Mancha and the European Union through the European Regional Development Fund to the Predictive Analysis Laboratory (PREDILAB) group (2020-GRIN-28770).
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
To test the robustness of the proposed model, a sensitivity analysis was carried out. In this way, the influence of the criteria weights on changes to the ranking of alternatives can be analysed. In order to assess the influence of the criteria weights on the ranking, the aggregated fuzzy weights given by the patient group were modified, increasing and decreasing the weights of each criterion by 10% and 20%. A similar modification was applied to each of the expert’s criteria weights, and the weights obtained by combining the judgements of the experts and the patient group. The rankings of the alternatives were assessed for each of these cases and the influence of changes in criteria weights on the alternatives assessed. Figure A1 shows the results obtained in the case of modifying the expert’s weights, Figure A2 the patient group’s weights and Figure A3 the combination of expert and patient group weights. The specific values obtained in this latter case are shown in Table A1.
From the sensitivity analysis, we can see that no modification in the ranking of alternatives is produced by the increase and decrease of the weights of the criteria when using the combination of the expert and patient group judgements. Therefore, the model is robust. In the case of the weights given by the expert, there are only two switches in the classification, between Years 1 and 3, when the weights of the criteria AEC and TAE are reduced by 20%. However, this decrease is considered too high in both cases, and thus not feasible. In the case of the weights provided by the patients, there was only one switch, in the classification of Years 4 and 5 with a decrease of 10% in the weighting of the criterion noise outside of hospital (NOH). Although this decrease would lead to a change in the classification, the environmental performance measured would undergo very small variations, on the order of 0.03, and so it would not affect the environmental performance significantly in any given year.
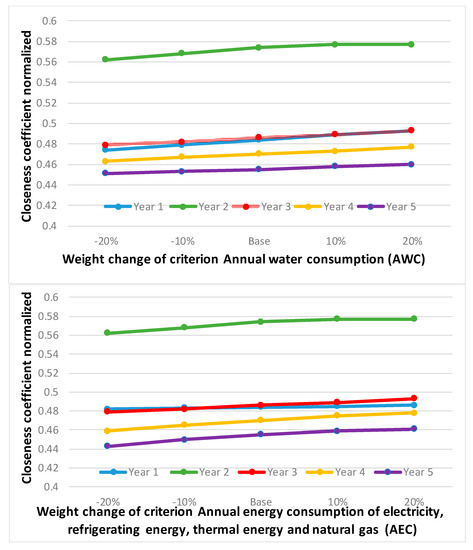
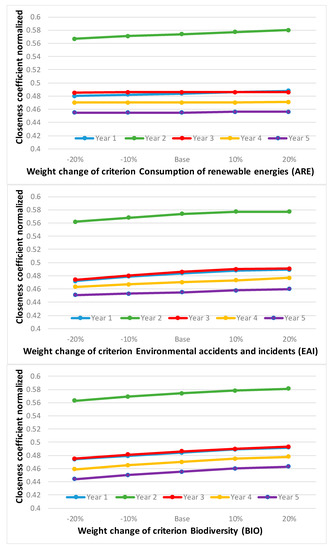
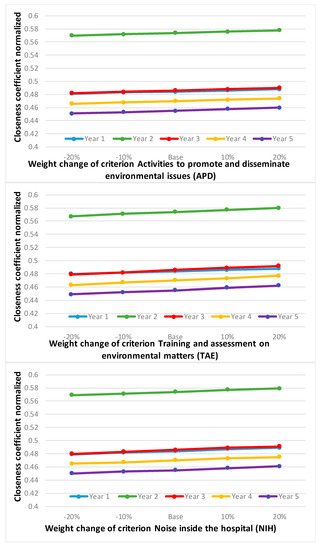
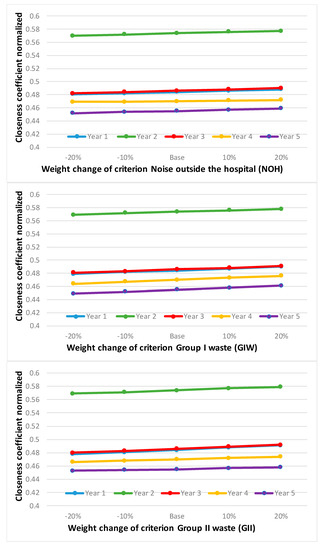
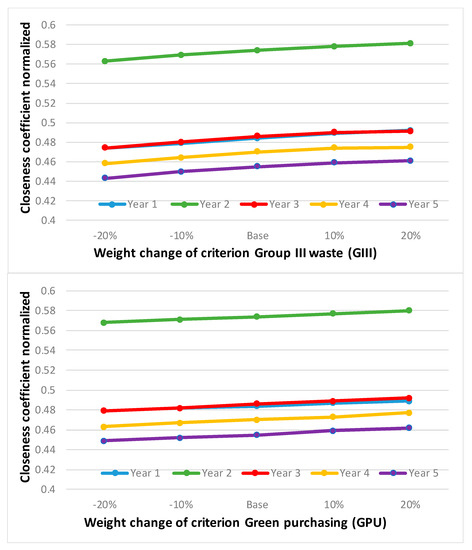
Figure A1.
Sensitivity analysis results modifying the expert’s weights.
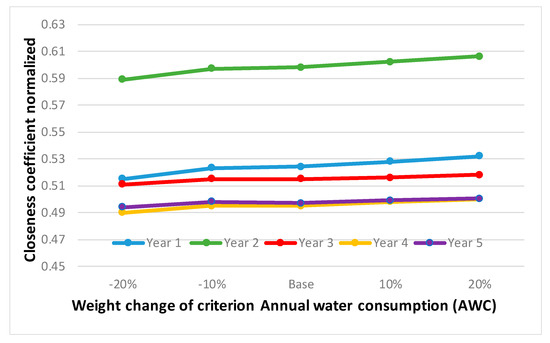
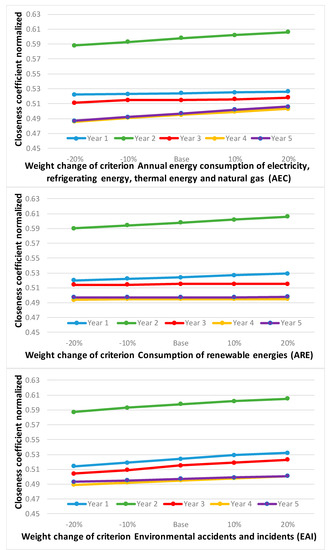
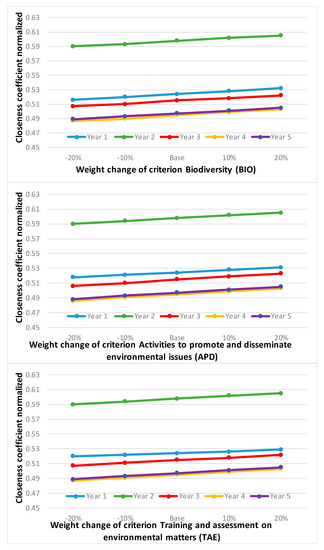
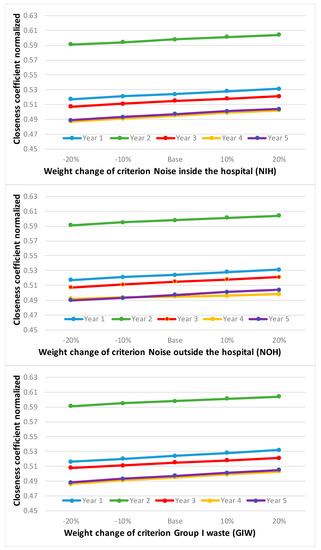
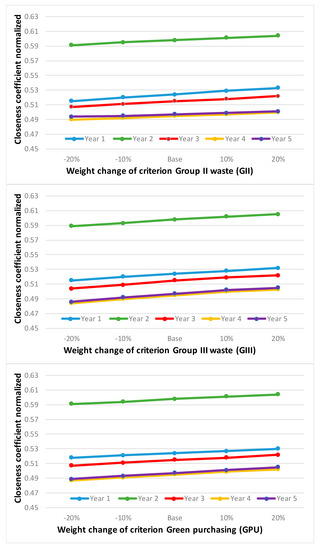
Figure A2.
Sensitivity analysis results modifying the patient group weights.
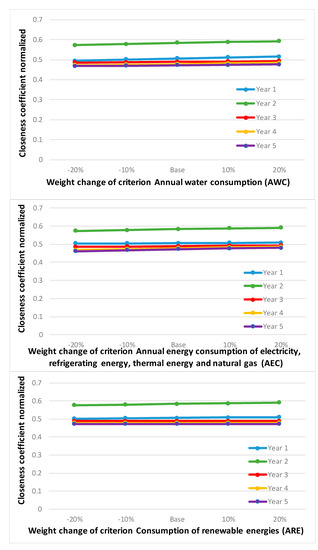
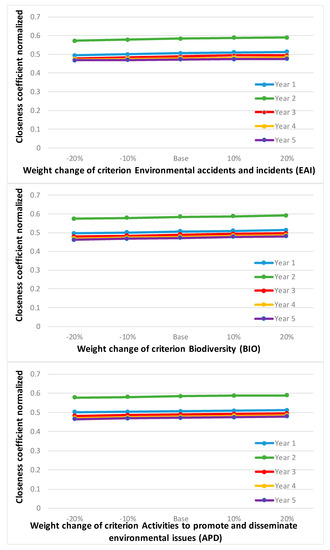
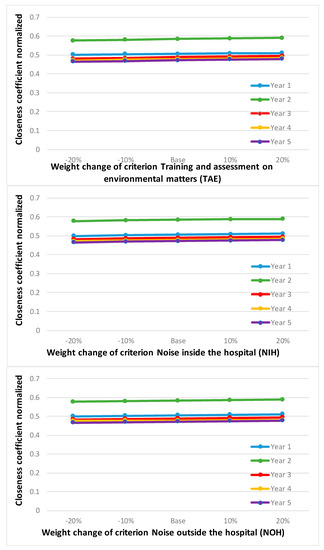
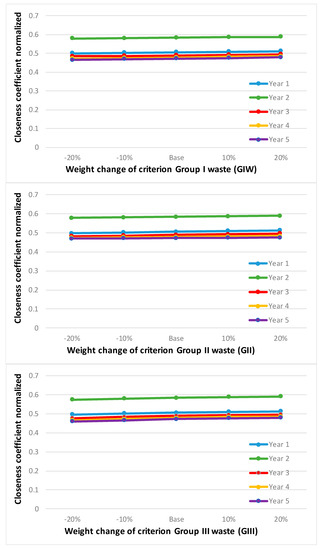
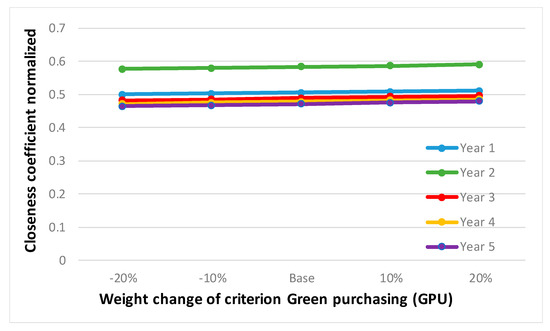
Figure A3.
Sensitivity analysis combining judgements from the expert and the patient group.

Table A1.
Sensitivity analysis results modifying expert and patient group combined weights.
Table A1.
Sensitivity analysis results modifying expert and patient group combined weights.
| Alternative | −20% | −10% | Base | 10% | 20% |
|---|---|---|---|---|---|
| Annual Water Consumption (AWC) | |||||
| Year 1 | 0.495 | 0.501 | 0.506 | 0.511 | 0.515 |
| Year 2 | 0.573 | 0.578 | 0.584 | 0.588 | 0.592 |
| Year 3 | 0.485 | 0.487 | 0.489 | 0.491 | 0.493 |
| Year 4 | 0.472 | 0.475 | 0.478 | 0.481 | 0.484 |
| Year 5 | 0.468 | 0.47 | 0.472 | 0.474 | 0.476 |
| Annual Consumption (MW/H) by the Hospital of Electricity, Refrigerating Energy, Thermal Energy and Natural Gas (AEC) | |||||
| Year 1 | 0.504 | 0.505 | 0.506 | 0.507 | 0.508 |
| Year 2 | 0.573 | 0.578 | 0.584 | 0.588 | 0.591 |
| Year 3 | 0.485 | 0.487 | 0.489 | 0.491 | 0.493 |
| Year 4 | 0.468 | 0.473 | 0.478 | 0.482 | 0.486 |
| Year 5 | 0.461 | 0.467 | 0.472 | 0.477 | 0.48 |
| Consumption of Renewable Energies (ARE) | |||||
| Year 1 | 0.501 | 0.504 | 0.506 | 0.508 | 0.51 |
| Year 2 | 0.576 | 0.58 | 0.584 | 0.587 | 0.591 |
| Year 3 | 0.488 | 0.489 | 0.489 | 0.489 | 0.489 |
| Year 4 | 0.478 | 0.478 | 0.478 | 0.478 | 0.479 |
| Year 5 | 0.472 | 0.472 | 0.472 | 0.472 | 0.473 |
| Environmental Accidents and Incidents (EAI) | |||||
| Year 1 | 0.494 | 0.5 | 0.506 | 0.51 | 0.513 |
| Year 2 | 0.572 | 0.578 | 0.584 | 0.588 | 0.59 |
| Year 3 | 0.477 | 0.483 | 0.489 | 0.494 | 0.496 |
| Year 4 | 0.472 | 0.475 | 0.478 | 0.481 | 0.484 |
| Year 5 | 0.468 | 0.47 | 0.472 | 0.474 | 0.476 |
| Biodiversity (BIO) | |||||
| Year 1 | 0.496 | 0.501 | 0.506 | 0.51 | 0.514 |
| Year 2 | 0.574 | 0.579 | 0.584 | 0.588 | 0.592 |
| Year 3 | 0.479 | 0.484 | 0.489 | 0.493 | 0.497 |
| Year 4 | 0.469 | 0.474 | 0.478 | 0.483 | 0.487 |
| Year 5 | 0.462 | 0.467 | 0.472 | 0.477 | 0.481 |
| Activities to Promote and Disseminate Environmental Issues (APD) | |||||
| Year 1 | 0.501 | 0.503 | 0.506 | 0.508 | 0.511 |
| Year 2 | 0.578 | 0.581 | 0.584 | 0.587 | 0.589 |
| Year 3 | 0.482 | 0.486 | 0.489 | 0.492 | 0.495 |
| Year 4 | 0.471 | 0.475 | 0.478 | 0.482 | 0.485 |
| Year 5 | 0.465 | 0.469 | 0.472 | 0.475 | 0.479 |
| Training and Evaluations on Environmental Matters (TAE) | |||||
| Year 1 | 0.502 | 0.504 | 0.506 | 0.508 | 0.51 |
| Year 2 | 0.576 | 0.58 | 0.584 | 0.587 | 0.59 |
| Year 3 | 0.482 | 0.485 | 0.489 | 0.493 | 0.596 |
| Year 4 | 0.471 | 0.475 | 0.478 | 0.482 | 0.485 |
| Year 5 | 0.465 | 0.468 | 0.472 | 0.476 | 0.479 |
| Noise Inside the Hospital (NIH) | |||||
| Year 1 | 0.499 | 0.503 | 0.506 | 0.509 | 0.512 |
| Year 2 | 0.577 | 0.581 | 0.584 | 0.587 | 0.589 |
| Year 3 | 0.482 | 0.486 | 0.489 | 0.492 | 0.495 |
| Year 4 | 0.472 | 0.475 | 0.478 | 0.481 | 0.484 |
| Year 5 | 0.465 | 0.469 | 0.472 | 0.475 | 0.478 |
| Noise Outside the Hospital (NOH) | |||||
| Year 1 | 0.5 | 0.503 | 0.506 | 0.509 | 0.511 |
| Year 2 | 0.578 | 0.581 | 0.584 | 0.586 | 0.589 |
| Year 3 | 0.483 | 0.486 | 0.489 | 0.492 | 0.494 |
| Year 4 | 0.476 | 0.477 | 0.478 | 0.479 | 0.48 |
| Year 5 | 0.466 | 0.469 | 0.472 | 0.475 | 0.478 |
| Group I Waste (GIW) | |||||
| Year 1 | 0.5 | 0.503 | 0.506 | 0.509 | 0.512 |
| Year 2 | 0.579 | 0.581 | 0.584 | 0.586 | 0.588 |
| Year 3 | 0.484 | 0.486 | 0.489 | 0.491 | 0.494 |
| Year 4 | 0.472 | 0.475 | 0.478 | 0.482 | 0.485 |
| Year 5 | 0.465 | 0.469 | 0.472 | 0.475 | 0.479 |
| Group II Waste (GII) | |||||
| Year 1 | 0.498 | 0.502 | 0.506 | 0.51 | 0.513 |
| Year 2 | 0.578 | 0.581 | 0.584 | 0.586 | 0.589 |
| Year 3 | 0.482 | 0.485 | 0.489 | 0.492 | 0.496 |
| Year 4 | 0.474 | 0.476 | 0.478 | 0.481 | 0.483 |
| Year 5 | 0.469 | 0.471 | 0.472 | 0.474 | 0.475 |
| Group III Waste (GIII) | |||||
| Year 1 | 0.496 | 0.501 | 0.506 | 0.51 | 0.513 |
| Year 2 | 0.574 | 0.579 | 0.584 | 0.588 | 0.591 |
| Year 3 | 0.477 | 0.483 | 0.489 | 0.493 | 0.496 |
| Year 4 | 0.466 | 0.473 | 0.478 | 0.483 | 0.485 |
| Year 5 | 0.46 | 0.466 | 0.472 | 0.477 | 0.479 |
| Green Purchasing (GPU) | |||||
| Year 1 | 0.5 | 0.503 | 0.506 | 0.509 | 0.511 |
| Year 2 | 0.577 | 0.58 | 0.584 | 0.587 | 0.59 |
| Year 3 | 0.482 | 0.485 | 0.489 | 0.493 | 0.496 |
| Year 4 | 0.471 | 0.475 | 0.478 | 0.482 | 0.485 |
| Year 5 | 0.465 | 0.468 | 0.472 | 0.476 | 0.479 |
References
- Hospitecnia. Agenda Global Para Hospitales Verdes y Saludables. Available online: https://hospitecnia.com/arquitectura/sostenibilidad/agenda-global-hospitales-verdes-saludables/ (accessed on 19 July 2020).
- Ostrom, A.L.; Bitner, M.J.; Brown, S.W.; Burkhard, K.A.; Goul, M.; Smith-Daniels, V.; Rabinowich, E. Moving forward and making a difference: Research priorities for the science of service. J. Serv. Res. 2010, 13, 4–36. [Google Scholar] [CrossRef]
- Minoglou, M.; Gerassimidou, S.; Komilis, D. Healthcare Waste Generation Worldwide and Its Dependence on Socio-Economic and Environmental Factors. Sustainability 2017, 9, 220. [Google Scholar] [CrossRef]
- Rodriguez, R.; Svensson, G.; Wood, G. Sustainability trends in public hospitals: Efforts and priorities. Eval. Program Plan. 2020, 78, 101742. [Google Scholar] [CrossRef]
- Lenzen, M.; Malik, A.; Li, M.; Fry, J.; Weisz, H.; Pichler, P.-P.; Pencheon, D.; Suveges, L.; Chaves, M.; Capon, A.; et al. The environmental footprint of health care: A global assessment. Lancet 2020, 4, e271–e279. [Google Scholar] [CrossRef]
- Cai, W.; Lai, K.H. Sustainability assessment of mechanical manufacturing systems in the industrial sector. Renew. Sustain. Energy Rev. 2021, 135, 110169. [Google Scholar] [CrossRef]
- Ezbakhe, F.; Pérez-Foguet, A. Decision analysis for sustainable development: The case of renewable energy planning under uncertainty. Eur. J. Oper. Res. 2020, in press. [Google Scholar] [CrossRef]
- Carnero, M.C. Assessment of Environmental Sustainability in Health Care Organizations. Sustainability 2015, 7, 8270–8291. [Google Scholar] [CrossRef]
- Carino, S.; Porter, J.; Malekpour, S.; Collins, J. Environmental Sustainability of Hospital Foodservices across the Food Supply Chain: A Systematic Review. J. Acad. Nutr. Diet. 2020, 120, 825–873. [Google Scholar] [CrossRef]
- Hales, S.; de Wet, N.; Maindonald, J.; Woodward, A. Potential effect of population and climate changes on global distribution of dengue fever: An empirical model. Lancet 2002, 360, 830–834. [Google Scholar] [CrossRef]
- Tomson, C. Reducing the carbon footprint of hospital-based care. Future Hosp. J. 2015, 2, 57–62. [Google Scholar] [CrossRef]
- World Health Organization. Safe Management of Wastes from Health-Care Activities a Summary; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- Kanbar, A.; Abdessater, M.; Dabal, C.; El Khoury, J.; Akl, H.; El Hachem, C.; Halabi, R.; Elias, S.; Boustany, J.; El Khoury, R. Health-care waste segregation among surgical team groups: A new assessment method. Perioper. Care Oper. Room Manag. 2020, 20, 100103. [Google Scholar] [CrossRef]
- Carnero, M.C. Waste Segregation FMEA Model Integrating Intuitionistic Fuzzy Set and the PAPRIKA Method. Mathematics 2020, 8, 1375. [Google Scholar] [CrossRef]
- Voudrias, E.A. Healthcare waste management from the point of view of circular economy. Waste Manag. 2018, 75, 1–2. [Google Scholar] [CrossRef]
- Nascimento, G.; Araujo, C.A.S.; Alves, L.A. Corporate sustainability practices in accredited Brazilian hospitals: A degree-of-maturity assessment of the environmental dimension. Rev. Adm. 2017, 52, 26–35. [Google Scholar] [CrossRef][Green Version]
- Pruss, A.; Giroult, E.; Rushbrook, P. Safe Management of Wastes from Health-Care Activities; World Health Organization: Geneva, Switzerland, 1999. [Google Scholar]
- Patwary, M.A.; O’Hare, W.T.; Street, G.; Elahi, K.M.; Hossain, S.S.; Sarker, M.H. Quantitative assessment of medical waste generation in the capital city of Bangladesh. Waste Manag. 2009, 29, 2392–2397. [Google Scholar] [CrossRef]
- Blass, A.; Gouvêada, S.E.; Pinheiro de Lima, E.; Borges, L.A. Measuring environmental performance in hospitals: A practical approach. J. Clean. Prod. 2017, 142, 279–289. [Google Scholar] [CrossRef]
- Salvado, M.F.; Azevedo, S.G.; Matias, J.C.O.; Ferreira, L.M. Proposal of a Sustainability Index for the Automotive Industry. Sustainability 2015, 7, 2113–2144. [Google Scholar] [CrossRef]
- McGain, F.; Naylor, C. Environmental sustainability in hospitals–a systematic review and research agenda. J. Health Serv. Res. Policy 2014, 19, 245–252. [Google Scholar] [CrossRef]
- Frangopoulos, C.A.; Keramioti, D.E. Multi-criteria evaluation of energy systems with sustainability considerations. Entropy 2010, 12, 1006–1020. [Google Scholar] [CrossRef]
- Belton, V.; Stewart, T. Multiple Criteria Decision Analysis: An Integrated Approach; Springer: New York, NY, USA, 2002. [Google Scholar]
- Hokkanen, J.; Lahdelma, R.; Salminen, P. Multicriteria decision support in a technology competition for cleaning polluted soil in Helsinki. J. Environ. Manag. 2000, 60, 339–348. [Google Scholar] [CrossRef]
- Broekhuizen, H.; Groothuis-Oudshoorn, C.G.; van Til, J.A.; Hummel, J.M.; IJzerman, M.J. A review and classification of approaches for dealing with uncertainty in multi-criteria decision analysis for healthcare decisions. Pharmacoeconomics 2015, 33, 445–455. [Google Scholar] [CrossRef]
- Bond, A.; Morrison-Saunders, A.; Pope, J. Sustainability assessment: The state of the art. Impact Assess. Proj. Apprais. 2012, 30, 53–62. [Google Scholar] [CrossRef]
- Santoyo-Castelazo, E.; Azapagic, A. Sustainability assessment of energy systems: Integrating environmental, economic and social aspects. J. Clean. Prod. 2014, 80, 1–20. [Google Scholar] [CrossRef]
- Lahdelma, R.; Salminen, P.; Hokkanen, J. Locating a waste treatment facility by using stochastic multicriteria acceptability analysis with ordinal criteria. Eur. J. Oper. Res. 2002, 142, 345–356. [Google Scholar] [CrossRef]
- Munda, G. Measuring sustainability: A multi-criterion framework. Environ. Dev. Sustain. 2005, 2, 117–134. [Google Scholar] [CrossRef]
- Achillas, C.; Vlachokostas, C.; Moussiopoulos, N.; Banias, G. Prioritize strategies to confront environmental deterioration in urban areas: Multicriteria assessment of public opinion and experts’ views. Cities 2011, 28, 414–423. [Google Scholar] [CrossRef]
- Huang, I.B.; Keisler, J.; Linkov, I. Multi-criteria decision analysis in environmental sciences: Ten years of applications and trends. Sci. Total Environ. 2011, 409, 3578–3594. [Google Scholar] [CrossRef]
- Thokala, P.; Devlin, N.; Marsh, K.; Baltussen, R.; Boysen, M.; Kalo, Z.; Longrenn, T.; Mussen, F.; Peacock, S.; Pharm, J.W.; et al. Multiple Criteria Decision Analysis for Health Care Decision Making—An Introduction: Report 1 of the ISPOR MCDA Emerging Good Practices Task Force. Value Health 2016, 19, 1–13. [Google Scholar] [CrossRef]
- Martín-Gamboa, M.; Iribarren, D.; García-Gusano, D.; Dufour, J. A review of life-cycle approaches coupled with data envelopment analysis within multi-criteria decision analysis for sustainability assessment of energy systems. J. Clean. Prod. 2017, 150, 164–174. [Google Scholar] [CrossRef]
- Büyüközkan, G.; Karabulut, Y. Sustainability performance evaluation: Literature review and future directions. J. Environ. Manag. 2018, 217, 253–267. [Google Scholar] [CrossRef]
- Deshpande, P.C.; Skaar, C.; Brattebø, H.; Fet, A.M. Multi-criteria decision analysis (MCDA) method for assessing the sustainability of end-of-life alternatives for waste plastics: A case study of Norway. Sci. Total Environ. 2020, 719, 137353. [Google Scholar] [CrossRef]
- Stefanović, G.; Milutinović, B.; Vučićević, B.; Denčić-Mihajlov, K.; Turanjanin, V. A comparison of the Analytic Hierarchy Process and the Analysis and Synthesis of Parameters under Information Deficiency method for assessing the sustainability of waste management scenarios. J. Clean. Prod. 2016, 130, 155–165. [Google Scholar] [CrossRef]
- Büyüközkan, G.; Karabulut, Y. Energy project performance evaluation with sustainability perspective. Energy 2017, 119, 549–560. [Google Scholar] [CrossRef]
- Loikkanen, O.; Lahdelma, R.; Salminen, P. Multicriteria evaluation of sustainable energy solutions for Colosseum. Sustain. Cities Soc. 2017, 35, 289–297. [Google Scholar] [CrossRef]
- Talukder, B.; Hipel, K.W. The PROMETHEE Framework for Comparing the Sustainability of Agricultural Systems. Resources 2018, 7, 74. [Google Scholar] [CrossRef]
- Melkonyan, A.; Gruchmann, T.; Lohmar, F.; Kamath, V.; Spinler, S. Sustainability assessment of last-mile logistics and distribution strategies: The case of local food networks. Int. J. Prod. Econ. 2020, 228, 107746. [Google Scholar] [CrossRef]
- Ziemba, P. Towards Strong Sustainability Management—A Generalized PROSA Method. Sustainability 2019, 11, 1555. [Google Scholar] [CrossRef]
- Khan, I. Power generation expansion plan and sustainability in a developing country: A multi-criteria decision analysis. J. Clean. Prod. 2019, 220, 707–720. [Google Scholar] [CrossRef]
- Hu, A.H.; Chen, L.T.; Hsu, C.W.; Ao, J.G. An evaluation framework for scoring corporate sustainability reports in Taiwan. Environ. Eng. Sci. 2011, 28, 843–858. [Google Scholar] [CrossRef]
- Kahraman, C.; Kaya, İ. A fuzzy multicriteria methodology for selection among energy alternatives. Expert Syst. Appl. 2010, 37, 6270–6281. [Google Scholar] [CrossRef]
- Erdogan, M.; Kaya, I. An integrated multi-criteria decision-making methodology based on type-2 fuzzy sets for selection among energy alternatives in Turkey. Iran. J. Fuzzy Syst. 2015, 12, 1–25. [Google Scholar]
- Mousavi, M.; Gitinavard, H.; Mousavi, S. A soft computing based-modified ELECTRE model for renewable energy policy selection with unknown information. Renew. Sustain. Energy Rev. 2017, 68, 774–787. [Google Scholar] [CrossRef]
- Kiker, G.; Bridges, T.; Varghese, A.; Seager, T.; Linkov, I. Application of multicriteria decision analysis in environmental decision making. Integr. Enviro Assess. Manag. 2005, 1. [Google Scholar] [CrossRef]
- Herva, M.; Roca, E. Review of combined approaches and multi-criteria analysis for corporate environmental evaluation. J. Clean. Prod. 2013, 39, 355–371. [Google Scholar] [CrossRef]
- Neste, J.; Karjalainen, T.P. A literature review–The use of multi-criteria decision analysis in Environmental Impact Assessment. Available online: https://jyx.jyu.fi/bitstream/handle/123456789/49480/Annex7.2.5ReportontheuseofMCDAinEIAandSEA.pdf?isAllowed=y&sequence=1 (accessed on 25 April 2013).
- Boggia, A.; Massei, G.; Pace, E.; Rocchi, L.; Paolotti, L.; Attard, M. Spatial multicriteria analysis for sustainability assessment: A new model for decision making. Land Use Policy 2018, 71, 281–292. [Google Scholar] [CrossRef]
- Jelokhani-Niaraki, M.; Sadeghi-Niaraki, A.; Choi, S.M. Semantic interoperability of GIS and MCDA tools for environmental assessment and decision making. Environ. Model. Softw. 2018, 100, 104–122. [Google Scholar] [CrossRef]
- Environment Science Center (ESC). Greener Hospital: Improving Environmental Performance; Environmental Science Center, University of Augsburg: Augsburg, Germany, 2007. [Google Scholar]
- Center for Maximum Potential Building Systems and Practice Greenhealth (CMPBS). The Green Guide for Health Care. 2008. Available online: https://www.gghc.org/documents/Version2.2/GGHC-v2-2-Ops-08Rev.pdf (accessed on 21 May 2020).
- World Health Organisation. World Health Organisation Healthy Hospitals, Healthy Planet, Healthy People: Addressing Climate Change in Healthcare Settings. Available online: www.who.int/globalchange/publications/climatefootprint_report.pdf (accessed on 25 August 2020).
- Smith, M.E.F. Sustainable Healthcare. A Path to Sustainability. Master’s Thesis, Lund University, Lund, Sweden, 2012. [Google Scholar]
- Intraruangsri, J. The Evolution of Green Hospital Concept for Thailand’s Hospital. Master’s Thesis, Thammasat University, Phra Nakhon, Thailand, 2018. [Google Scholar]
- Pinzone, M.; Guerci, M.; Lettieri, E.; Redman, T. Progressing in the change journey towards sustainability in healthcare: The role of ‘Green’ HRM. J. Clean. Prod. 2016, 122, 201–211. [Google Scholar] [CrossRef]
- Castro, M.D.; Mateus, R.; Braganca, L. Development of a healthcare building sustainability assessment method-proposed structure and system of weights for the Portuguese context. J. Clean. Prod. 2017, 148, 555–570. [Google Scholar] [CrossRef]
- Castro, M.D.; Mateus, R.; Braganca, L. Healthcare Building Sustainability Assessment tool-Sustainable Effective Design criteria in the Portuguese context. Environ. Impact Assess. Rev. 2017, 67, 49–60. [Google Scholar] [CrossRef]
- Kleber, J. Environmental Stewardship: The Nurse’s Role in Sustainability. Clin. J. Oncol. Nurs. 2018, 22, 354–356. [Google Scholar] [CrossRef]
- Thiel, C.L.; Woods, N.C.; Bilec, M.M. Strategies to Reduce Greenhouse Gas Emissions from Laparoscopic Surgery. Am J Public Health 2018, 108, 158–164. [Google Scholar] [CrossRef]
- Romero, I.; Carnero, M.C. Environmental Assessment in Health Care Organizations. Environ. Sci. Pollut. Res. 2017. [Google Scholar] [CrossRef]
- European Union. Reglamento (CE) no 1221/2009 del Parlamento Europeo y del Consejo de 25 de noviembre de 2009 relativo a la participación voluntaria de organizaciones en un sistema comunitario de gestión y auditoría medioambientales (EMAS), y por el que se derogan el Regl. In Boletín Oficial del Estado (DOUE-L-2009-82515); Diario Oficial: Madrid, Spain, 2009. [Google Scholar]
- Zamparas, M.; Kapsalis, V.C.; Kyriakopoulos, G.L.; Aravossis, K.G.; Kanteraki, A.E.; Vantarakis, A.; Kalavrouziotis, I.K. Medical waste management and environmental assessment in the Rio University Hospital, Western Greece. Sustain. Chem. Pharm. 2019, 13, 100163. [Google Scholar] [CrossRef]
- Carnero, M.C. Model for Sustainability in Health Care Organizations. In Encyclopedia of Business Analytics and Optimization; Wang, J., Ed.; IGI Global: Hershey, PA, USA, 2014; Volume III, Chapter 141; pp. 437–456. [Google Scholar]
- Tawfik-Shukor, A.R.; Klazinga, N.S.; Arah, O.A. Comparing health system performance assessment and management approaches in the Netherlands and Ontario, Canada. BMC Health Serv. Res. 2007, 7, 25. [Google Scholar] [CrossRef]
- Chartier, Y.; Emmanuel, J.; Pieper, U.; Prüss, A.; Rushbrook, P.; Stringer, R.; Townend, W.; Wilburn, S.; Zghondi, R. Safe Management of Wastes from Health-Care Activities, 2nd ed.; World Health Organization: Geneva, Switzerland, 2014. [Google Scholar]
- Samaie, F.; Meyar-Naimi, H.; Javadi, S.; Feshki-Farahani, H. Comparison of sustainability models in development of electric vehicles in Tehran using fuzzy TOPSIS method. Sustain. Cities Soc. 2020, 53, 101912. [Google Scholar] [CrossRef]
- Lima, F.R.; Osiro, L.; Carpinetti, L.C.R. A comparison between Fuzzy AHP and Fuzzy TOPSIS methods to supplier selection. Appl. Soft Comput. 2014, 21, 194–209. [Google Scholar] [CrossRef]
- Basahel, A.; Taylan, O. Using fuzzy AHP and fuzzy TOPSIS approaches for assessing safety conditions at worksites in construction industry. Int. J. Saf. Secur. Eng. 2016, 6, 728–745. [Google Scholar] [CrossRef]
- Feng, C.M.; Wang, R.T. Performance evaluation for airlines including the consideration of financial ratios. J. Air Transp. Manag. 2000, 6, 133–142. [Google Scholar] [CrossRef]
- Sarraf, R.; McGuire, M.P. Integration and comparison of multi-criteria decision making methods in safe route planner. Expert Syst. Appl. 2020, 154. [Google Scholar] [CrossRef]
- Salih, M.M.; Zaidan, B.B.; Zaidan, A.A.; Ahmed, M.A. Survey on fuzzy TOPSIS state-of-the-art between 2007 and 2017. Comput. Oper. Res. 2019, 104, 207–227. [Google Scholar] [CrossRef]
- SeongKon, L.; Gento, M.; SangKon, L.; JongWook, K. Prioritizing the weights of hydrogen energy technologies in the sector of the hydrogen economy by using a fuzzy AHP approach. Int. J. Hydrogen Energy 2011, 36, 1897–1902. [Google Scholar]
- Isaai, M.T.; Kanani, A.; Tootoonchi, M.; Afzali, H.R. Intelligent timetable evaluation using fuzzy AHP. Expert Syst. Appl. 2011, 38, 3718–3723. [Google Scholar] [CrossRef]
- Mohammadi, S.; Golara, S.; Mousavi, N. Selecting Adequate Security Mechanisms in E-Business Processes Using Fuzzy TOPSIS. Int. J. Fuzzy Syst. Appl. 2012, 2, 35–53. [Google Scholar] [CrossRef][Green Version]
- Alguliyev, R.M.; Aliguliyev, R.M.; Mahmudova, R.S. A Fuzzy TOPSIS+Worst-Case Model for Personnel Evaluation Using Information Culture Criteria. Int. J. Oper. Res. Inf. Syst. 2016, 7, 38–66. [Google Scholar] [CrossRef]
- Ravasan, A.Z.; Hanafizadeh, P.; Olfat, L.; Taghavifard, M.T. A Fuzzy TOPSIS Method for Selecting an E-banking Outsourcing Strategy. Int. J. Enterp. Inf. Syst. 2017, 13. [Google Scholar] [CrossRef]
- Dinçer, H.; Hacıoğlu, Ü.; Yüksel, S. A Strategic Approach to Global Financial Crisis in Banking Sector: A Critical Appraisal of Banking Strategies Using Fuzzy ANP and Fuzzy Topsis Methods. Int. J. Sustain. Econ. Manag. 2017, 6, 1–21. [Google Scholar] [CrossRef][Green Version]
- Gupta, R.; Naqvi, S.K. A Framework for Applying CSFs to ERP Software Selection: An Extension of Fuzzy TOPSIS Approach. Int. J. Intell. Inf. Technol. 2017, 13, 41–62. [Google Scholar] [CrossRef]
- Marzouk, M.; El-Razek, M.A. Selecting Demolition Waste Materials Disposal Alternatives Using Fuzzy TOPSIS Technique. Int. J. Nat. Comput. Res. 2017, 6, 38–57. [Google Scholar] [CrossRef][Green Version]
- Rahpeyma, B.; Zarei, M. An Integrated QFD-TOPSIS Approach for Supplier Selection under Fuzzy Environment: A Case of Detergent Manufacturing Industry. Int. J. Serv. Sci. Manag. Eng. Technol. 2018, 9, 62–81. [Google Scholar] [CrossRef]
- Rajak, M.; Shaw, K. Evaluation and selection of mobile health (mHealth) applications using AHP and fuzzy TOPSIS. Technol. Soc. 2019, 59, 101186. [Google Scholar] [CrossRef]
- Chang, D.Y. Applications of the extent analysis method on fuzzy AHP. Eur. J. Oper. Res. 1996, 95, 649–655. [Google Scholar] [CrossRef]
- Rostamzadeh, R.; Sofian, S. Prioritizing effective 7Ms to improve production systems performance using fuzzy AHP and fuzzy TOPSIS (case study). Expert Syst. Appl. 2011, 38, 5166–5177. [Google Scholar] [CrossRef]
- Kaufmann, A.; Gupta, M.M. Fuzzy Mathematical Models in Engineering and Management Science; North Holland: Amsterdam, The Netherland, 1988. [Google Scholar]
- Priyadarshini, M.; Nayak, I.; Rana, J.; Tripathy, P.P. Multi-objective optimization of turning process using fuzzy-TOPSIS analysis. Mater. Today Proc. 2020. [Google Scholar] [CrossRef]
- Chen, C.T. Extension of the TOPSIS for group decision—Making under fuzzy environment. Fuzzy Sets Syst. 2000, 114, 1–9. [Google Scholar] [CrossRef]
- Rashidi, K.; Cullinane, K. A comparison of fuzzy DEA and fuzzy TOPSIS in sustainable supplier selection: Implications for sourcing strategy. Expert Syst. Appl. 2019, 121, 266–281. [Google Scholar] [CrossRef]
- Javad, M.O.M.; Darvishi, M.; Javad, A.O.M. Green supplier selection for the steel industry using BWM and fuzzy TOPSIS: A case study of Khouzestan steel company. Sustain. Futures 2020, 2, 100012. [Google Scholar] [CrossRef]
- Kutlu, A.C.; Ekmekçioğlu, M. Fuzzy failure modes and effects analysis by using fuzzy TOPSIS-based fuzzy AHP. Expert Syst. Appl. 2012, 39, 61–67. [Google Scholar] [CrossRef]
- Galdakao-Usansolo Hospital. Declaración Ambiental. Ejercicio 2012. Available online: http://www.hospitalgaldakao-usansolo.com (accessed on 15 January 2020).
- World Health Organization. Night Noise Guidelines for Europe; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- Deng, H.; Yeh, C.H.; Willis, R.J. Inter-company comparison using modified TOPSIS with objective weights. Comput. Oper. Res. 2000, 27, 963–973. [Google Scholar] [CrossRef]
- Ahmad, K.; Khan, M.A.; Khan, S.; Ali, A.; Chu, Y.M. New estimates for generalized Shannon and Zipf-Mandelbrot entropies via convexity results. Results Phys. 2020, 18. [Google Scholar] [CrossRef]
- Shannon, C.E.; Weaver, W. The Mathematical Theory of Communication; The University of Illinois Press: Urbana, IL, USA, 1947. [Google Scholar]
- Zeleny, M. Multiple Criteria Decision Making; Springer: New York, NY, USA, 1996. [Google Scholar]
- Wu, J.; Sun, J.; Liang, L.; Zha, Y. Determination of weights for ultimate cross efficiency using Shannon entropy. Expert Syst. Appl. 2011, 38, 5162–5165. [Google Scholar] [CrossRef]
- Wang, T.C.; Lee, H.D. Developing a fuzzy TOPSIS approach based on subjective weights and objective weights. Expert Syst. Appl. 2009, 36, 8980–8985. [Google Scholar] [CrossRef]
- Kacprzak, D. Objective Weights Based on Ordered Fuzzy Numbers for Fuzzy Multiple Criteria Decision-Making Methods. Entropy 2017, 19, 373. [Google Scholar] [CrossRef]
- Sałabun, W.; Urbaniak, K. A New Coefficient of Rankings Similarity in Decision-Making Problems. In Computational Science–ICCS 2020; ICCS 2020. Lecture Notes in Computer Science; Springer: Cham, Switzerland, 2020; Volume 12138. [Google Scholar] [CrossRef]
- Chen, C.T.; Lin, C.T.; Huang, S.F. A fuzzy approach for supplier evaluation and selection in supply chain management. Int. J. Prod. Econ. 2006, 102, 289–301. [Google Scholar] [CrossRef]
- Zhuang, Z.Y.; Su, C.R.; Chang, S.C. The effectiveness of IF-MADM (intuitionistic-fuzzy multi-attribute decision-making) for group decisions: Methods and an empirical assessment for the selection of a senior centre. Technol. Econ. Dev. Econ. 2019, 25, 322–364. [Google Scholar] [CrossRef]
- Tsukiji, M.; Gamaralalage, P.J.D.; Pratomo, I.S.Y.; Onogawa, K.; Alverson, K.; Honda, S.; Ternald, D.; Dilley, M.; Fujioka, J.; Condrorini, D. Waste Management during de COVID-19 Pandemic. United Nations Environment Programme, 2020. Available online: https://wedocs.unep.org/bitstream/handle/20.500.11822/33416/WMC-19.pdf?sequence=1&isAllowed=y (accessed on 8 October 2020).
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).