A Fuzzy Collaborative Approach for Evaluating the Suitability of a Smart Health Practice
Abstract
1. Introduction
2. Previous Work
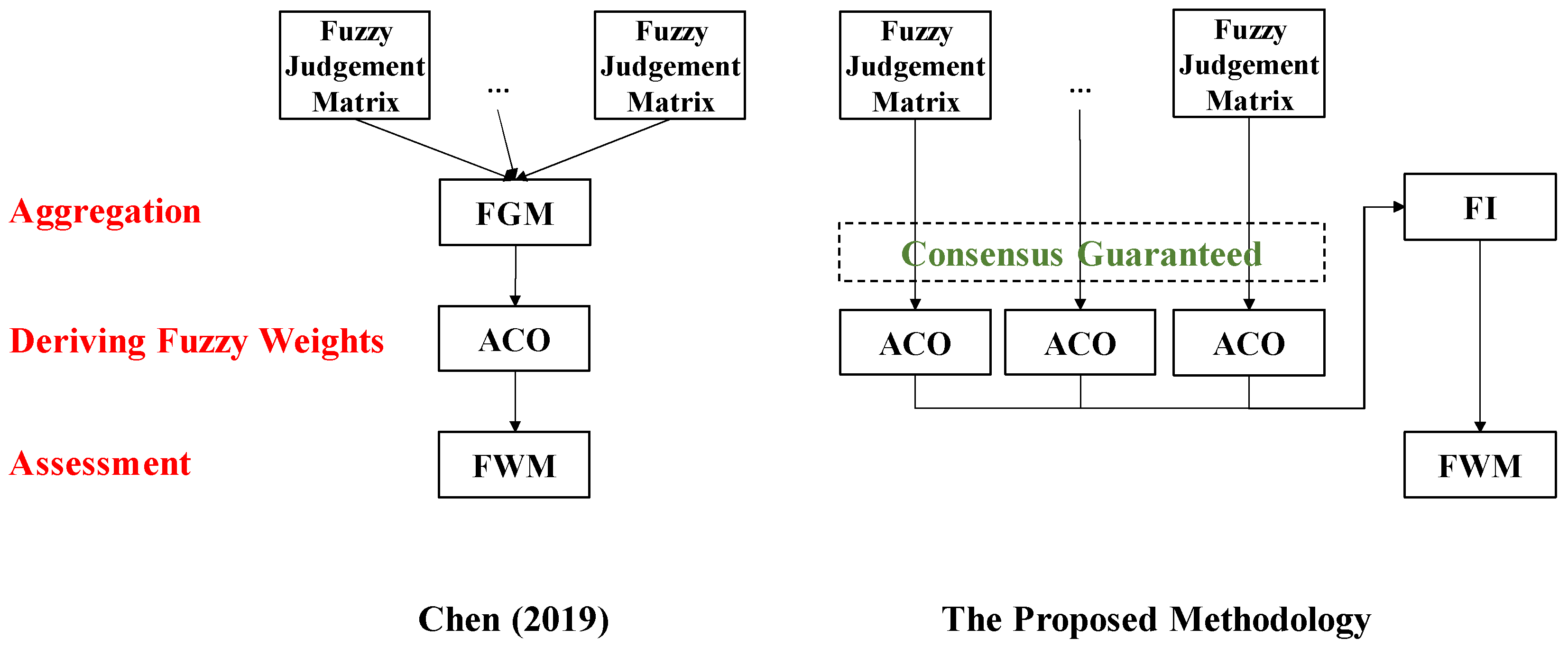
3. Methodology
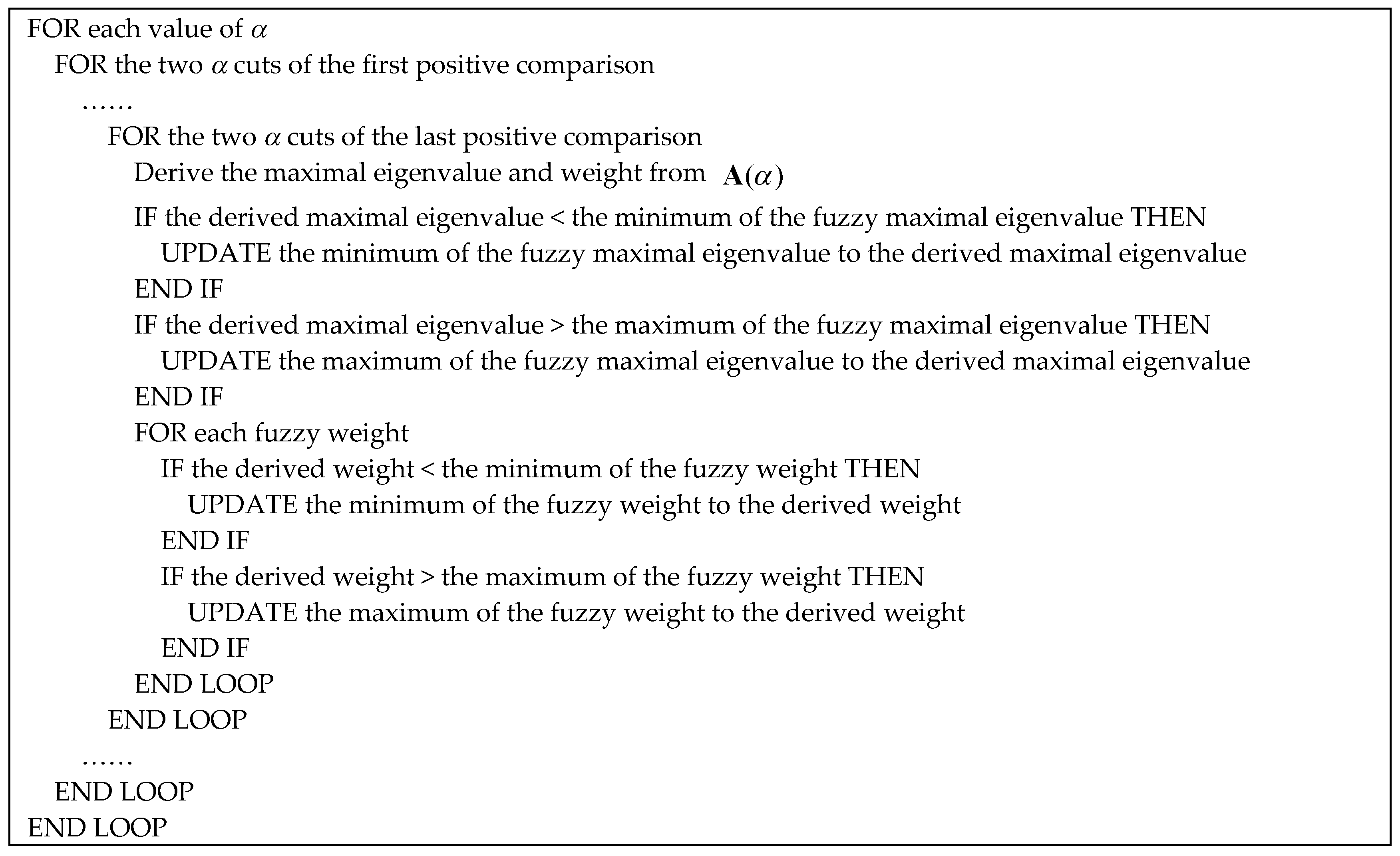
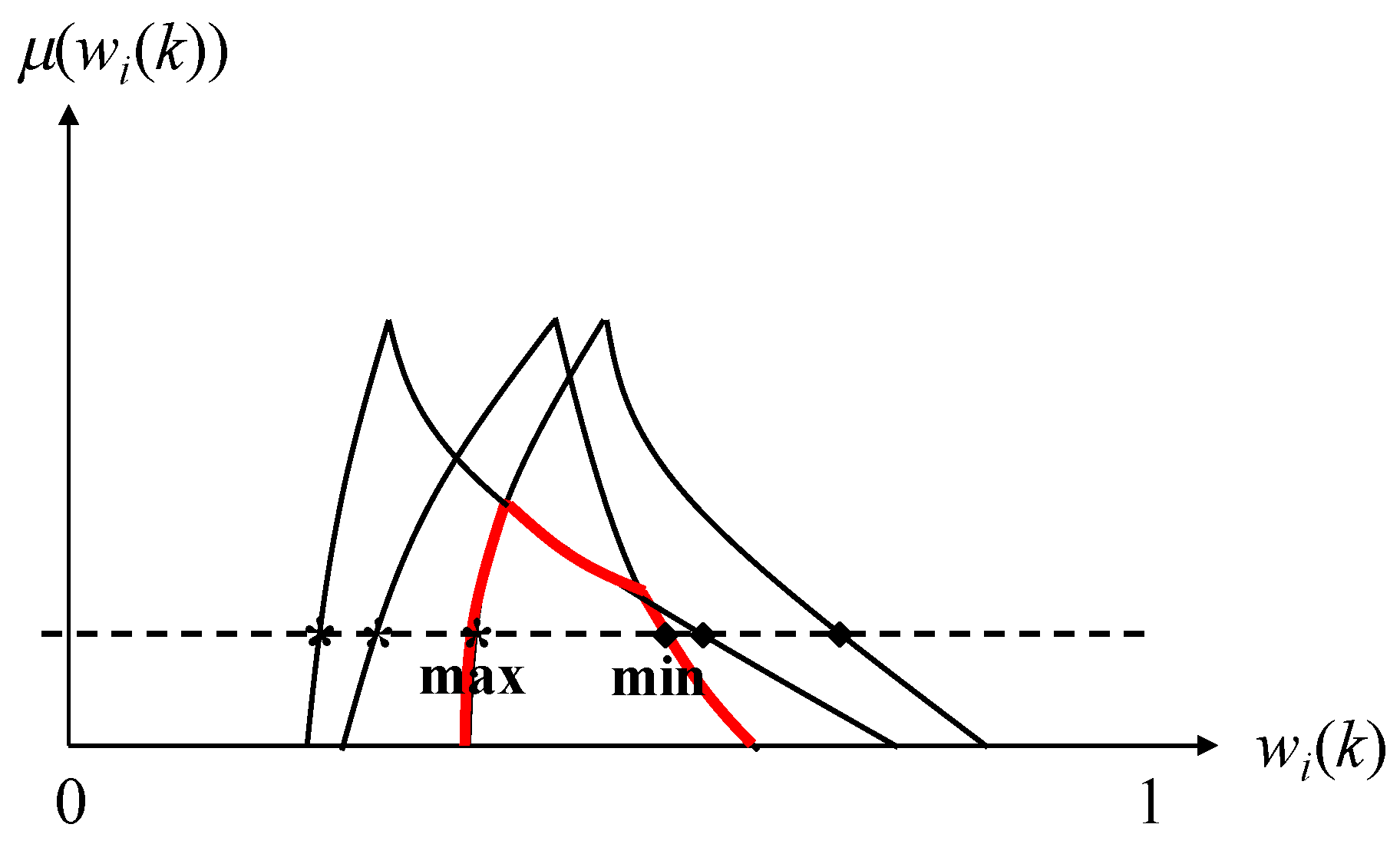
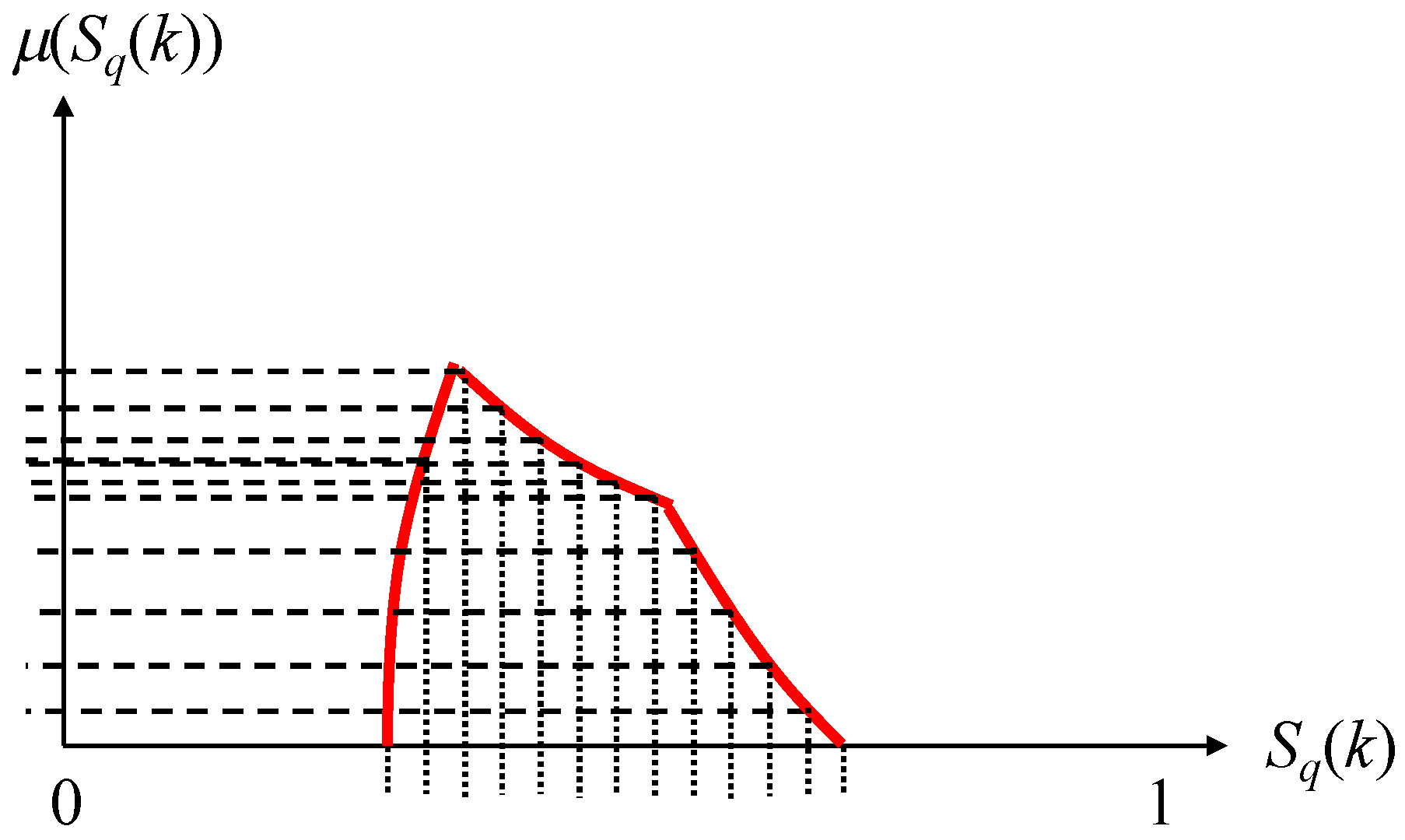
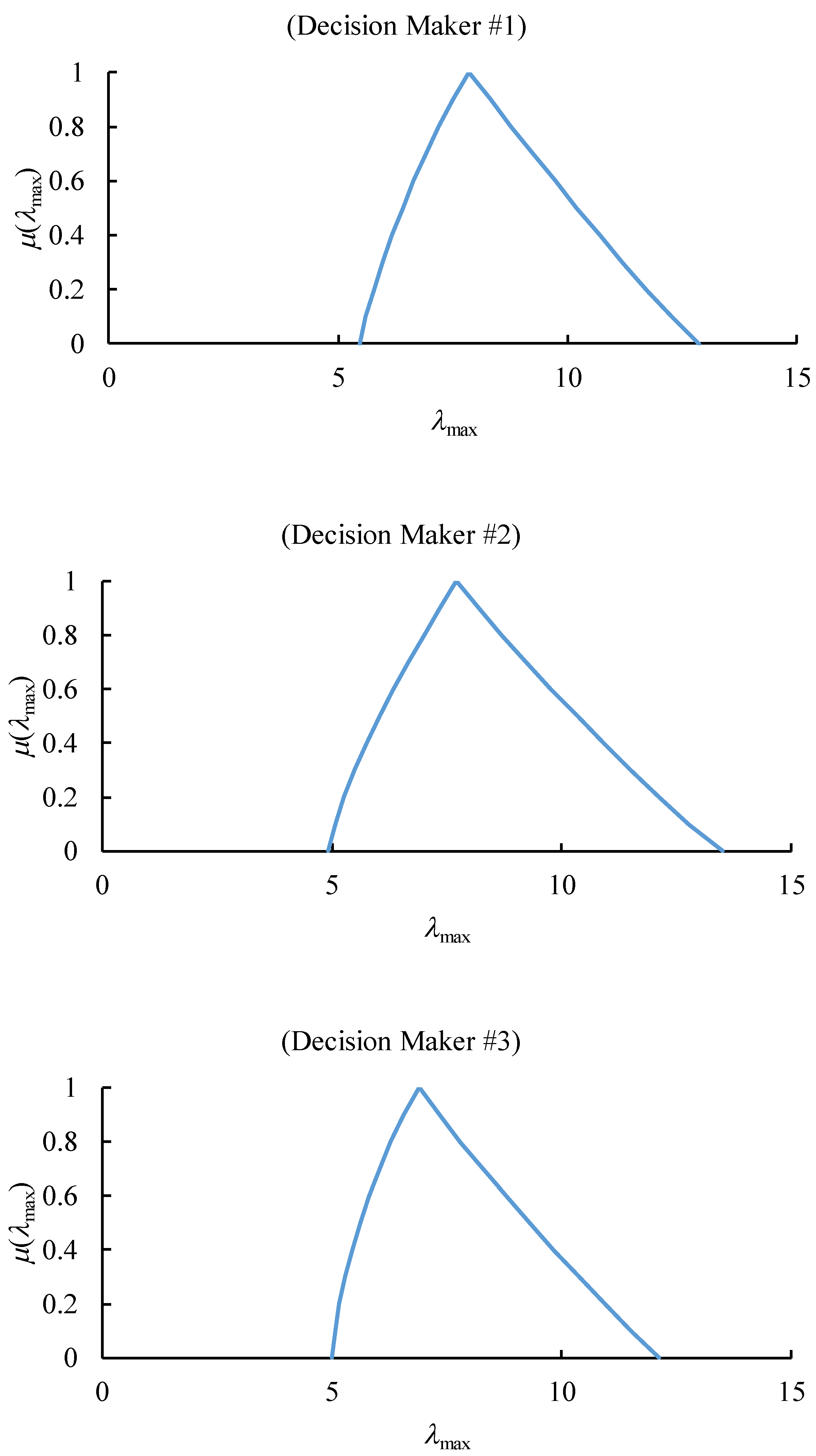
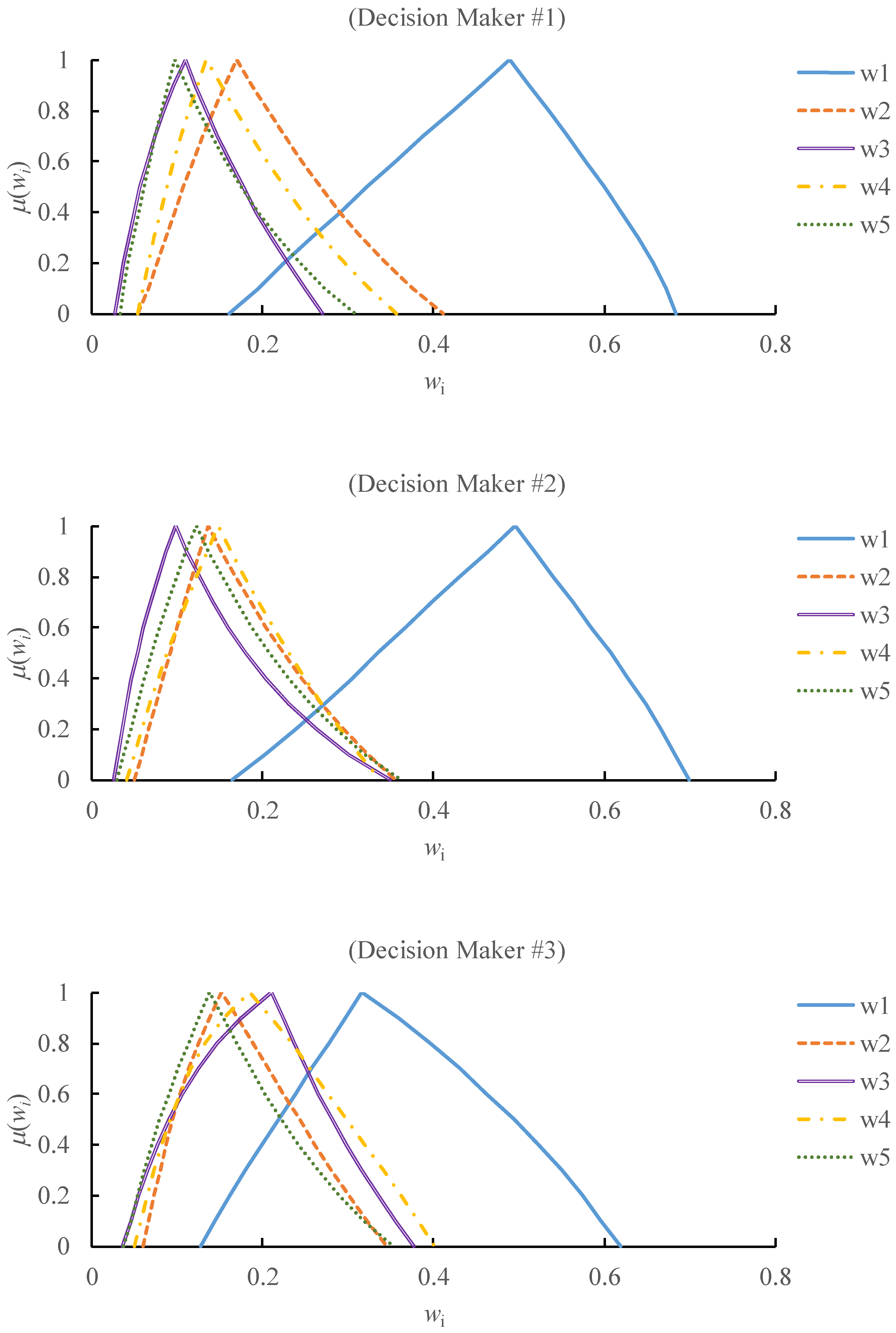
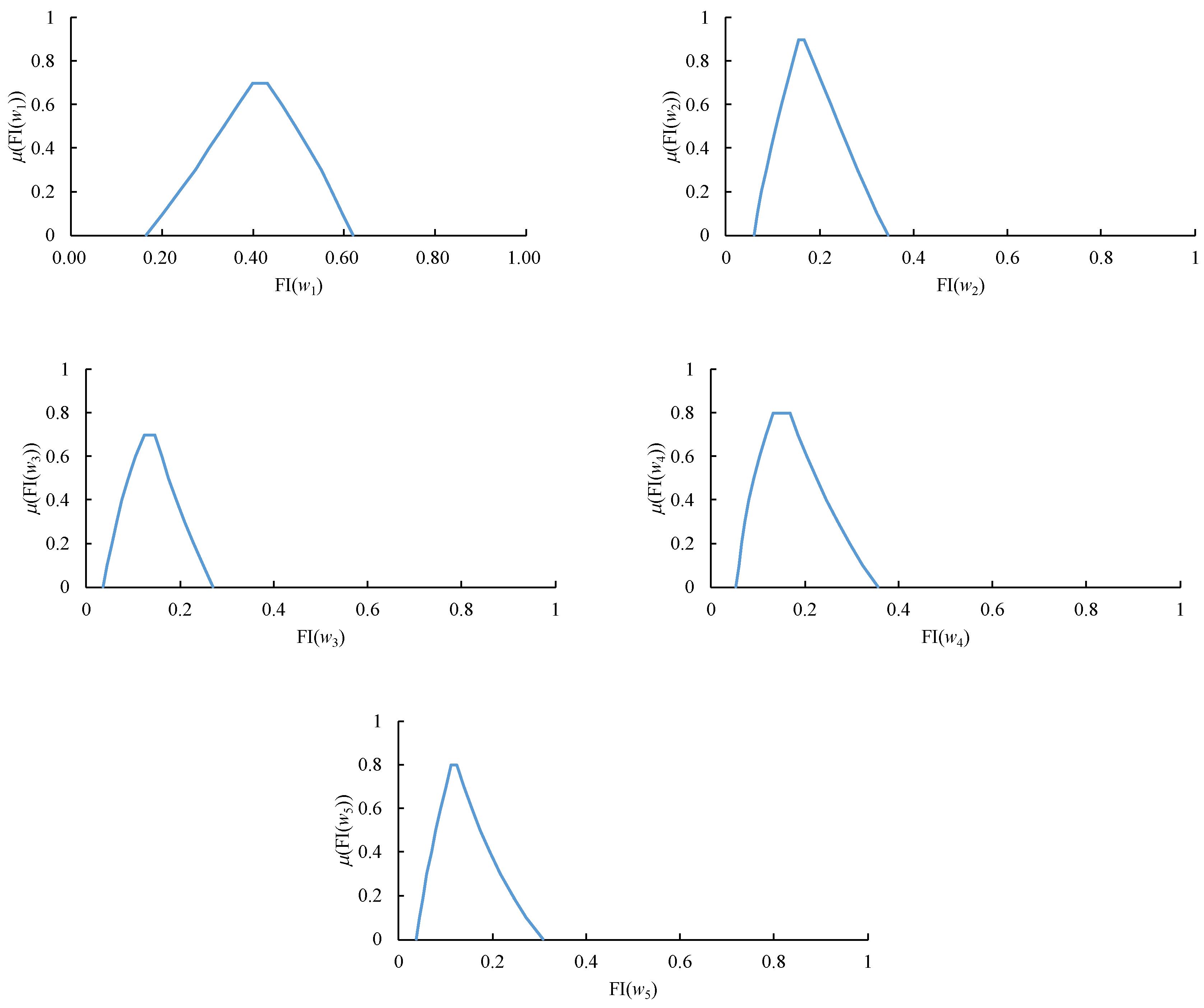
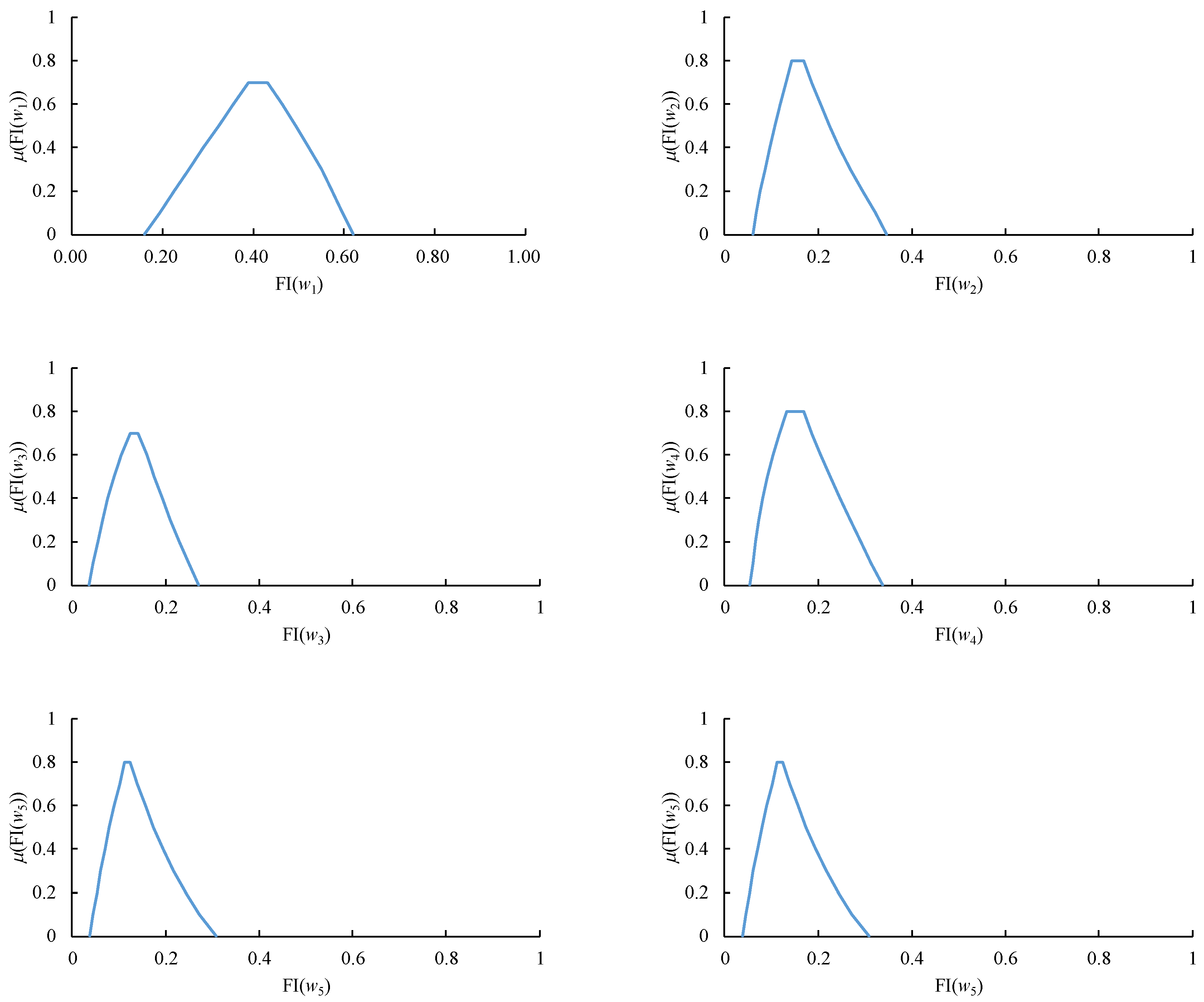
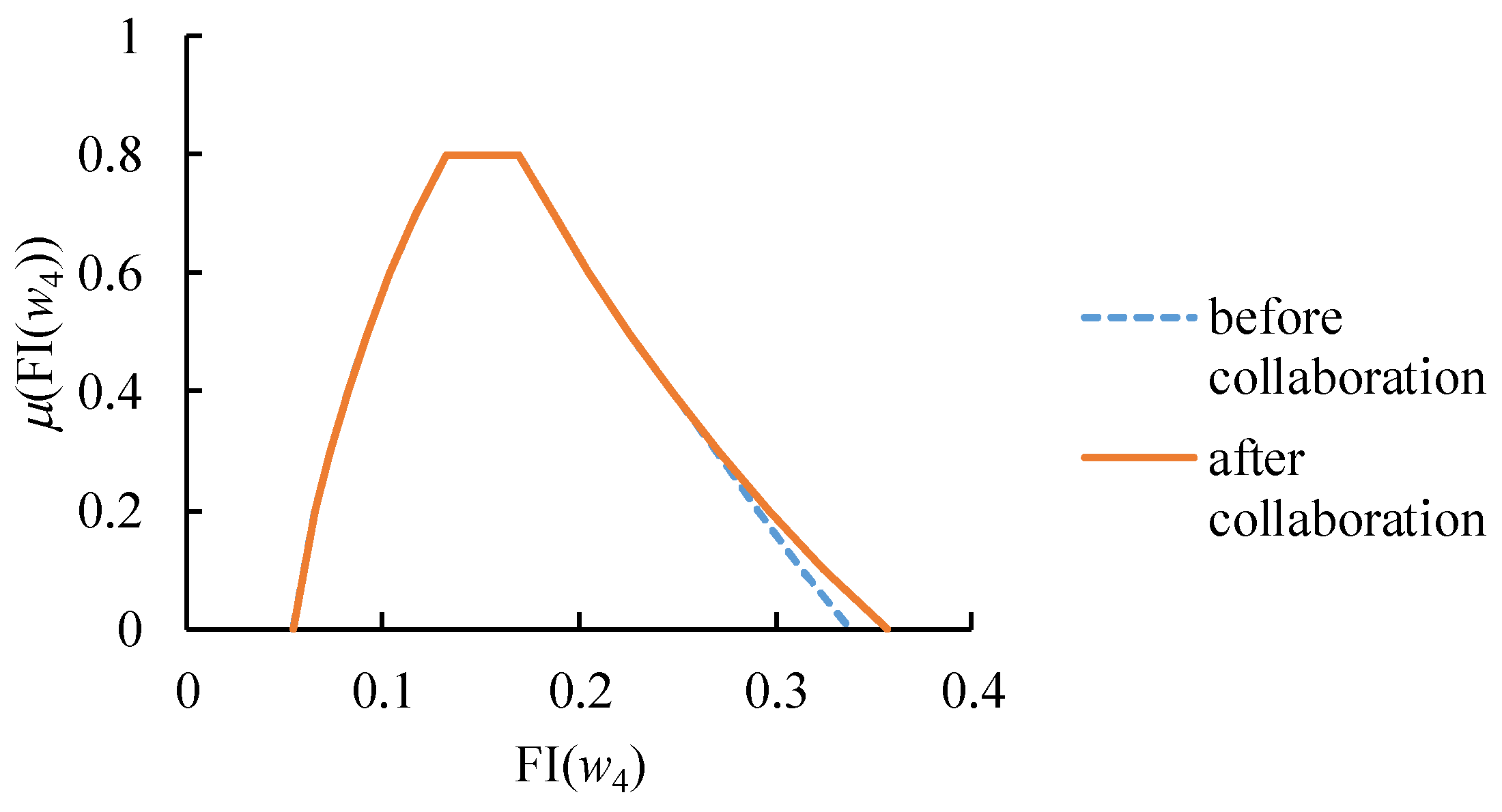
3.1. Deriving Fuzzy Weights for Each Decision Maker Using ACO
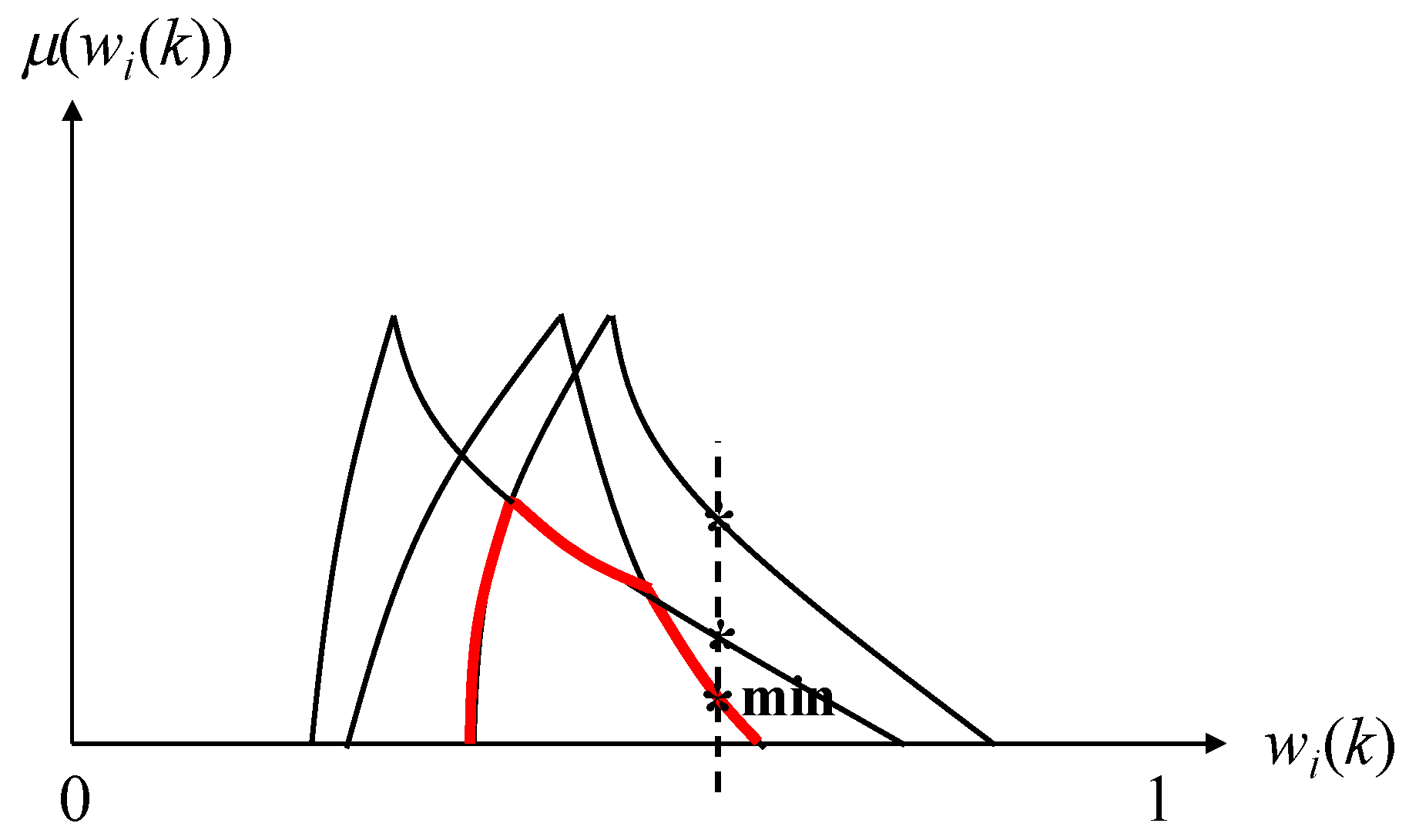
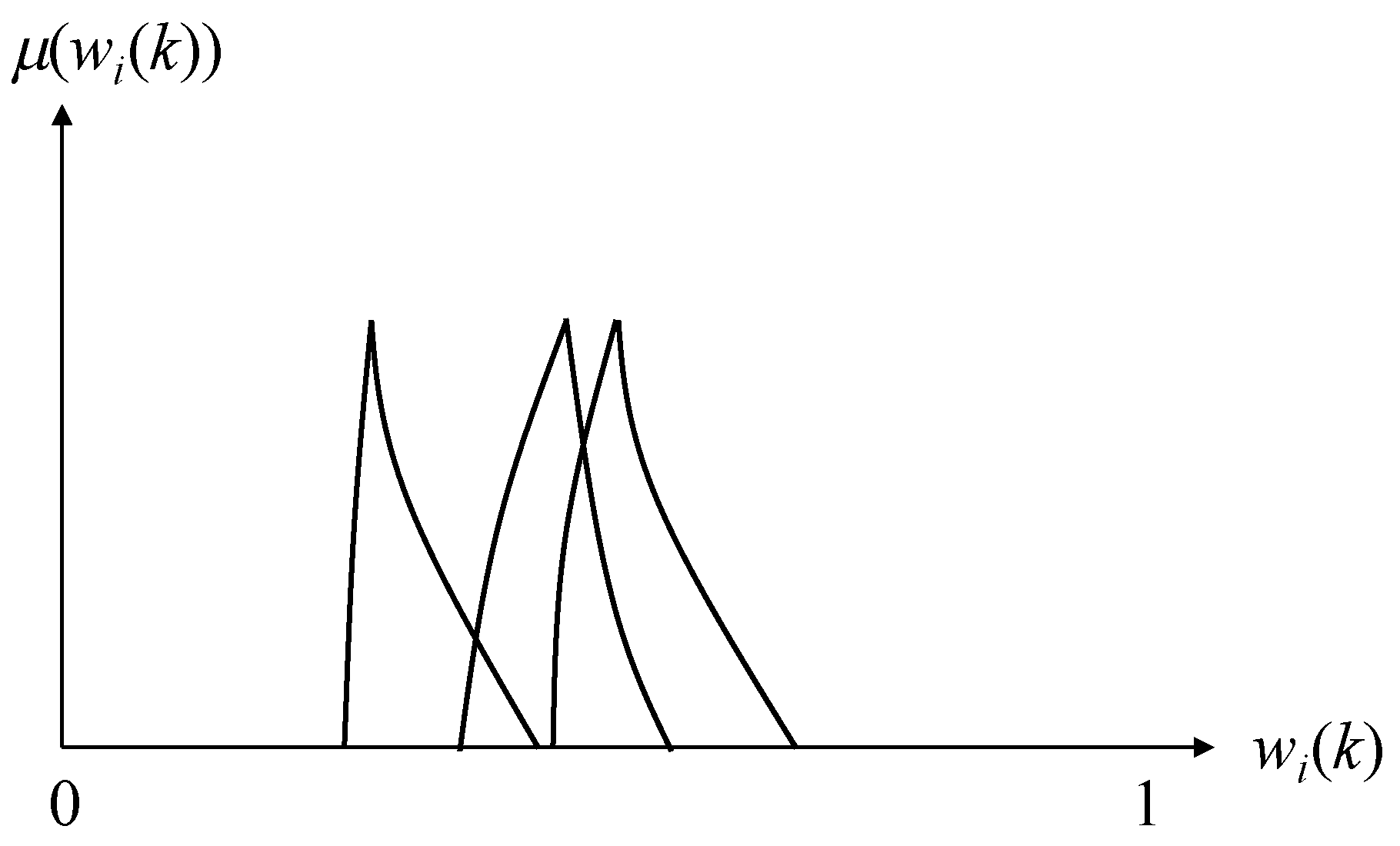
3.2. Aggregating the Fuzzy Weights by All Decision Makers Using FI
- (i)
- iffor some g: If a decision maker is absolutely important, then the value ofis determined solely by the decision maker.
- (ii)
- if∀ k: If all decision makers are equally important, then the value ofis determined by the consensus among the decision makers.
- (iii)
- if∀: If decision makeris more important than decision maker, then the value ofis closer to the value derived by decision makerthan to that by decision maker.
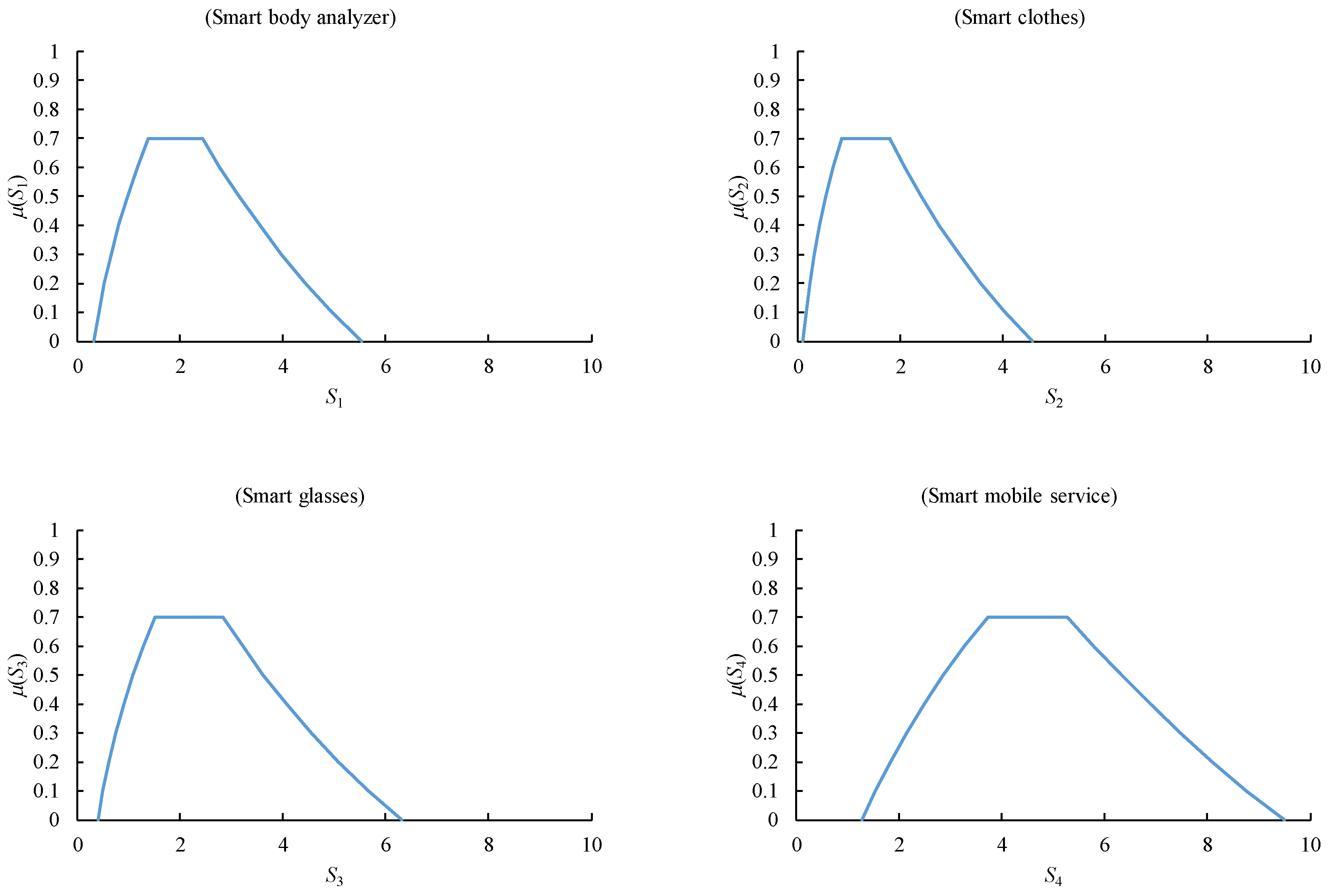
3.3. Assessing the Suitability of a Smart Health Practice Using FWM
4. Application
- (1)
- C1: unobtrusiveness,
- (2)
- C2: supporting online social networking,
- (3)
- C3: cost effectiveness,
- (4)
- C4: availability of mobile health care facilities, and
- (5)
- C5: correct, reliable, and robust identification of a user’s need and situation.
- Very poor: (0, 0, 1),
- Poor: (0, 1, 2),
- Moderate: (1.5, 2.5, 3.5),
- Good: (3, 4, 5), and
- Very good: (4, 5, 5).
- (1)
- Smart mobile services were the most suitable smart health practice, while smart clothes were still the least suitable smart health practice, owing to their obtrusiveness.
- (2)
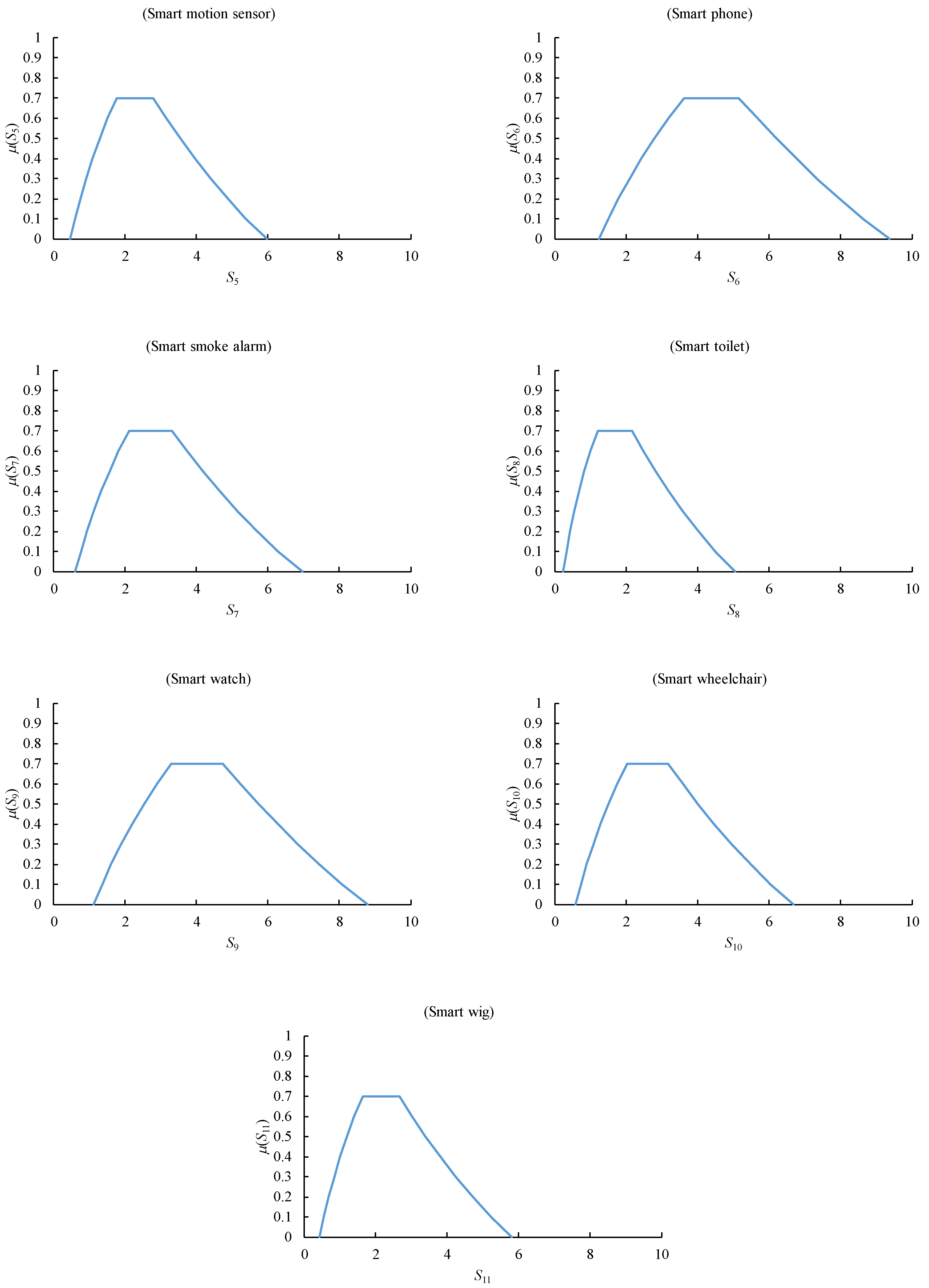
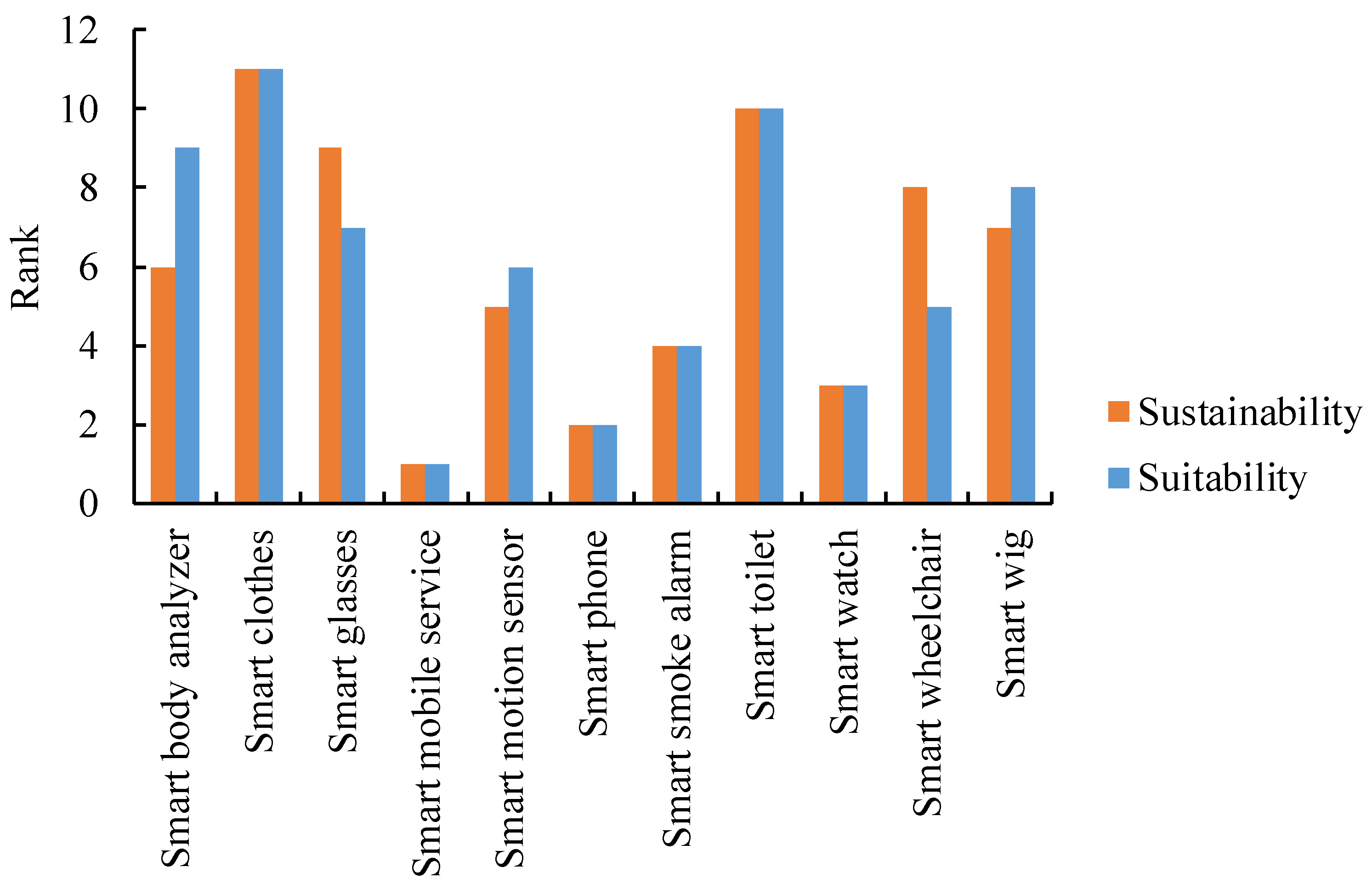
- The suitabilities of the eleven smart health practices were ranked. The results are shown in Figure 15. The ranking results of the sustainabilities of these smart health practices, retrieved from Chen [6], are also presented in this figure for comparison. Obviously, there are some differences between the two results. For example, the suitability of smart body analyzers was low, but its suitability was high, showing the great potential of smart body analyzers in the future.
- (3)
- In the experiment, decision makers modified their fuzzy judgment results just once to achieve a higher consensus, yet this was not always the case since modifications were subjectively made. It was possible for decision makers to undergo many rounds of collaboration before achieving a higher consensus. To tackle this problem, a mechanism for facilitating the collaboration process among decision makers should be designed.
- (4)
- The efficiency of ACO was a problem to the application of the fuzzy collaborative approach, and needed to be enhanced somehow, e.g., by applying a genetic algorithm. In previous studies, there were two major ways of combining genetic algorithms with fuzzy analytic hierarchy analysis. The first way obtains the weights of criteria by using fuzzy analytic hierarchy analysis, which designs the fitness function of the genetic algorithm to compare various alternatives. The second way solves a multi-objective optimization problem with a genetic algorithm to obtain multiple Pareto-optimal solutions, and then performs a fuzzy analytic hierarchy analysis to set the weights of the objective functions to further compare these Pareto-optimal solutions. The motive for applying a genetic algorithm in this study is different from those in previous studies.
- (5)
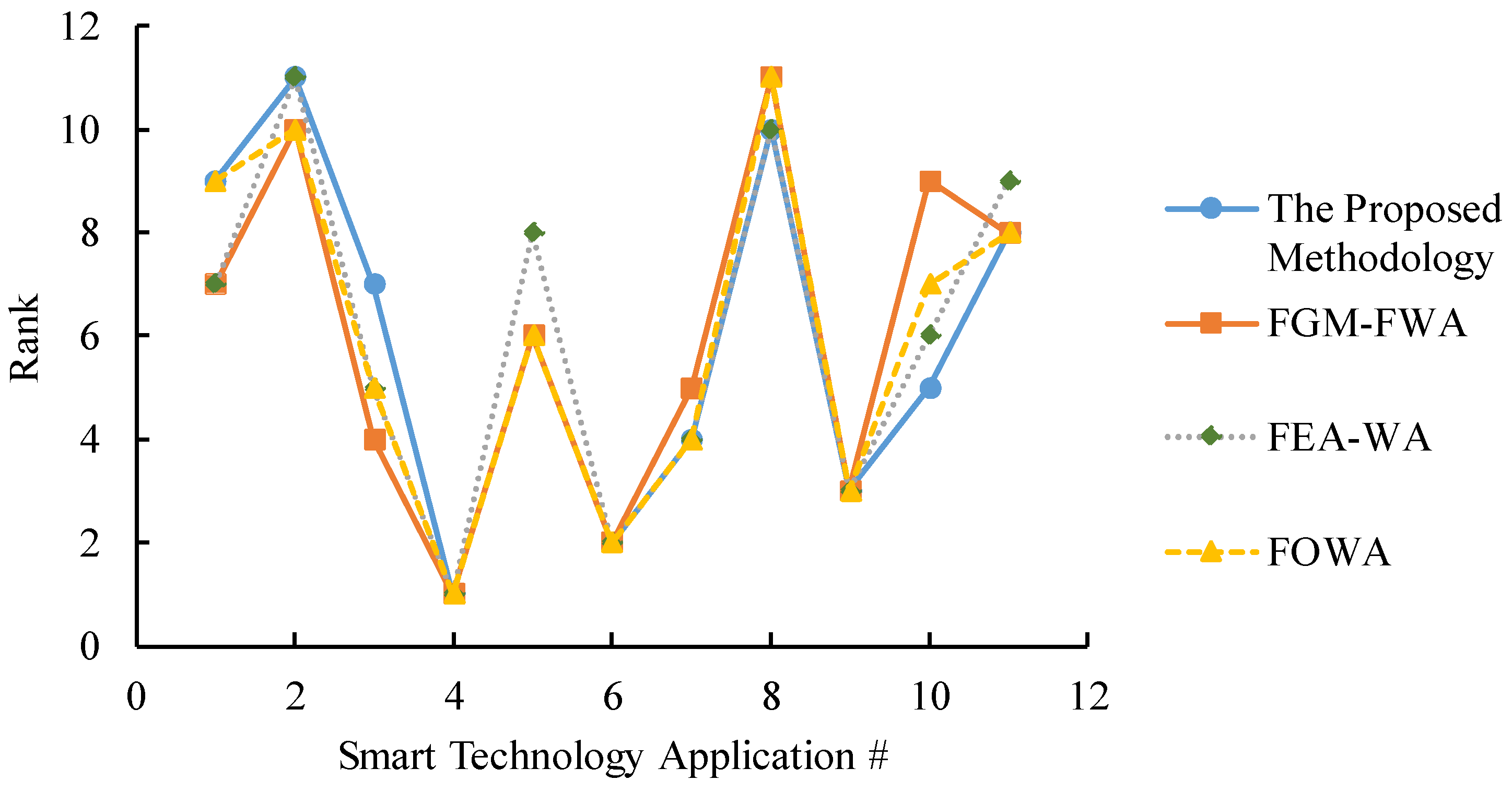
- Three existing methods, fuzzy ordered weighted average (FOWA), fuzzy geometric mean (FGM)-FWM, and the fuzzy extent analysis (FEA)-weighted average (WA) method proposed by Chang [29], were also applied to assess the suitability of each smart health practice for comparison. In FOWA, the moderately optimistic strategy was adopted. In FGM-FWM, fuzzy weights were approximated using FGM and expressed in terms of TFNs. In FEA-WA, since the weights estimated using FEA were crisp, WA, rather than FWM, was applied to assess the suitability of each smart health practice. Finally, the suitabilities of all smart health practices were ranked. The ranking results using various methods are compared in Figure 16. In sum, these methods came to the same conclusions about the suitabilities of smart mobile services and smart phones. In contrast, the suitabilities of other smart health practices assessed using different methods were not the same.
5. Conclusions
- (1)
- Smart mobile services and smart clothes were evaluated as the most suitable and the least suitable smart health practices, respectively.
- (2)
- The suitabilities of smart mobile services and smart phones evaluated using various methods were identical. In contrast, the suitabilities of other smart health practices, assessed using various methods, differed.
- (3)
- Among the compared methods, only the fuzzy collaborative approach could guarantee the existence of a consensus among decision makers. In other words, only the results assessed using the fuzzy collaborative approach were acceptable to all decision makers.
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Jordan, M. What Is ‘Smart’ Technology? Available online: http://knowit.co.nz/2011/08/what-is-smart-technology (accessed on 12 October 2019).
- Silva, B.M.; Rodrigues, J.J.; de la Torre Díez, I.; López-Coronado, M.; Saleem, K. Mobile-health: A review of current state in 2015. J. Biomed. Inform. 2015, 56, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Chen, T.; Chiu, M.-C. Smart technologies for assisting the life quality of persons in a mobile environment: A review. J. Ambient. Intell. Humaniz. Comput. 2018, 9, 319327. [Google Scholar] [CrossRef]
- Haymes, L.K.; Storey, K.; Maldonado, A.; Post, M.; Montgomery, J. Using applied behavior analysis and smart technology for meeting the health needs of individuals with intellectual disabilities. Dev. Neurorehabilit. 2015, 18, 407–419. [Google Scholar] [CrossRef]
- Chiu, M.-C.; Chen, T.-C.T. Assessing sustainable effectiveness of the adjustment mechanism of a ubiquitous clinic recommendation system. Health Care Manag. Sci. 2019, 1–10. [Google Scholar] [CrossRef]
- Chen, T.-C.T. Evaluating the sustainability of a smart technology application to mobile health care: The FGM–ACO–FWA approach. Complex Intell. Syst. 2019, 1–13. [Google Scholar] [CrossRef]
- Chen, T.-C.T. Guaranteed-consensus posterior-aggregation fuzzy analytic hierarchy process method. Neural Comput. Appl. 2019, 1–12. [Google Scholar] [CrossRef]
- Liu, F.; Mendel, J.M. Aggregation using the fuzzy weighted average as computed by the Karnik–Mendel algorithms. IEEE Trans. Fuzzy Syst. 2008, 16, 1–12. [Google Scholar]
- Steele, R. Social media, mobile devices and sensors: Categorizing new techniques for health communication. In Proceedings of the 2011 Fifth International Conference on Sensing Technology, Palmerston North, New Zealand, 28 November–1 December 2011; pp. 187–192. [Google Scholar]
- Hswen, Y.; Murti, V.; Vormawor, A.A.; Bhattacharjee, R.; Naslund, J.A. Virtual avatars, gaming, and social media: Designing a mobile health app to help children choose healthier food options. J. Mob. Technol. Med. 2013, 2, 8. [Google Scholar] [CrossRef] [PubMed]
- Petersen, C.; DeMuro, P. Legal and regulatory considerations associated with use of patient-generated health data from social media and mobile health (mHealth) devices. Appl. Clin. Inform. 2015, 6, 16–26. [Google Scholar] [PubMed]
- Cook, D.J.; Duncan, G.; Sprint, G.; Fritz, R.L. Using smart city technology to make healthcare smarter. Proc. IEEE 2018, 106, 708–722. [Google Scholar] [CrossRef]
- Reeder, B.; David, A. Health at hand: A systematic review of smart watch uses for health and wellness. J. Biomed. Inform. 2016, 63, 269–276. [Google Scholar] [CrossRef] [PubMed]
- Mandel, J.C.; Kreda, D.A.; Mandl, K.D.; Kohane, I.S.; Ramoni, R.B. SMART on FHIR: A standards-based, interoperable apps platform for electronic health records. J. Am. Med Inform. Assoc. 2016, 23, 899–908. [Google Scholar] [CrossRef] [PubMed]
- Hamidi, H. An approach to develop the smart health using Internet of Things and authentication based on biometric technology. Future Gener. Comput. Syst. 2019, 91, 434–449. [Google Scholar] [CrossRef]
- Rathod, R. Sensors Used in Smartphone. Available online: http://myphonefactor.in/2012/04/sensors-used-in-a-smartphone/ (accessed on 10 October 2019).
- Eklund, J.; Forsman, M. Smart work clothes give better health-Through improved work technique, work organization and production technology. In Congress of the International Ergonomics Association; Springer: Berlin/Heidelberg, Germany, 2018; pp. 515–519. [Google Scholar]
- Liu, L.; Stroulia, E.; Nikolaidis, I.; Miguel-Cruz, A.; Rincon, A.R. Smart homes and home health monitoring technologies for older adults: A systematic review. Int. J. Med Inform. 2016, 91, 44–59. [Google Scholar] [CrossRef] [PubMed]
- Eskofier, B.M.; Lee, S.I.; Baron, M.; Simon, A.; Martindale, C.F.; Gaßner, H.; Klucken, J. An overview of smart shoes in the internet of health things: Gait and mobility assessment in health promotion and disease monitoring. Appl. Sci. 2017, 7, 986. [Google Scholar] [CrossRef]
- Chen, M.; Ma, Y.; Song, J.; Lai, C.F.; Hu, B. Smart clothing: Connecting human with clouds and big data for sustainable health monitoring. Mob. Netw. Appl. 2016, 21, 825–845. [Google Scholar] [CrossRef]
- Duman, G.M.; El-Sayed, A.; Kongar, E.; Gupta, S.M. An intelligent multiattribute group decision-making approach with preference elicitation for performance evaluation. IEEE Trans. Eng. Manag. 2019, 1–17. [Google Scholar] [CrossRef]
- Kubler, S.; Robert, J.; Derigent, W.; Voisin, A.; Le Traon, Y. A state-of the-art survey & testbed of fuzzy AHP (FAHP) applications. Expert Syst. Appl. 2016, 65, 398–422. [Google Scholar]
- Saaty, T.L. Decision making—the analytic hierarchy and network processes (AHP/ANP). J. Syst. Sci. Syst. Eng. 2004, 13, 1–35. [Google Scholar] [CrossRef]
- Zheng, G.; Zhu, N.; Tian, Z.; Chen, Y.; Sun, B. Application of a trapezoidal fuzzy AHP method for work safety evaluation and early warning rating of hot and humid environments. Saf. Sci. 2012, 50, 228–239. [Google Scholar] [CrossRef]
- Michael, H. Applied Fuzzy Arithmetic an Introduction with Engineering Applications; Springer: Berlin/Heidelberg, Germany, 2005. [Google Scholar]
- Golub, G.H.; Van Loan, C.F. Matrix Computations; Johns Hopkins: Baltimore, MD, USA, 1996; p. 694. [Google Scholar]
- Saaty, T.L. The Analytic Hierarchy Process; McGraw-Hill: New York, NY, USA, 1980; p. 324. [Google Scholar]
- Wang, Y.-C.; Chen, T.; Yeh, Y.-L. Advanced 3D printing technologies for the aircraft industry: A fuzzy systematic approach for assessing the critical factors. Int. J. Adv. Manuf. Technol. 2018, 1–11. [Google Scholar] [CrossRef]
- Chang, D.-Y. Applications of the extent analysis method on fuzzy AHP. Eur. J. Oper. Res. 1996, 95, 649–655. [Google Scholar] [CrossRef]
- Wang, Y.C.; Chen, T. A fuzzy collaborative forecasting approach for forecasting the productivity of a factory. Adv. Mech. Eng. 2013, 5, 234571. [Google Scholar] [CrossRef]
- Al-Refaie, A.; Aldwairi, R.; Chen, T. Optimizing performance of rigid polyurethane foam using FGP models. J. Ambient Intell. Humaniz. Comput. 2018, 9, 351–366. [Google Scholar] [CrossRef]
- Csutora, R.; Buckley, J.J. Fuzzy hierarchical analysis: The Lambda-Max method. Fuzzy Sets Syst. 2001, 120, 181–195. [Google Scholar] [CrossRef]
- Chen, T. An effective fuzzy collaborative forecasting approach for predicting the job cycle time in wafer fabrication. Comput. Ind. Eng. 2013, 66, 834–848. [Google Scholar] [CrossRef]
- Yolcu, O.C.; Yolcu, U.; Egrioglu, E.; Aladag, C.H. High order fuzzy time series forecasting method based on an intersection operation. Appl. Math. Model. 2016, 40, 8750–8765. [Google Scholar] [CrossRef]
- Chen, T. A heterogeneous fuzzy collaborative intelligence approach for forecasting the product yield. Appl. Soft Comput. 2017, 57, 210–224. [Google Scholar] [CrossRef]
- Wang, Y.-C.; Chen, T.-C.T. A direct-solution fuzzy collaborative intelligence approach for yield forecasting in semiconductor manufacturing. Procedia Manuf. 2018, 17, 110–117. [Google Scholar] [CrossRef]
- Wang, Y.C.; Chen, T.C.T. A partial-consensus posterior-aggregation FAHP method—supplier selection problem as an example. Mathematics 2019, 7, 179. [Google Scholar] [CrossRef]
- Chen, T.-C.T.; Honda, K. Fuzzy Collaborative Forecasting and Clustering: Methodology, System Architecture, and Applications; Springer: Cham, Switzerland, 2019; p. 89. [Google Scholar]
- Van Broekhoven, E.; De Baets, B. Fast and accurate center of gravity defuzzification of fuzzy system outputs defined on trapezoidal fuzzy partitions. Fuzzy Sets Syst. 2006, 157, 904–918. [Google Scholar] [CrossRef]
- Ventola, C.L. Mobile devices and apps for health care professionals: Uses and benefits. Pharm. Ther. 2014, 39, 356. [Google Scholar]
- Demiris, G.; Hensel, B.K.; Skubic, M.; Rantz, M. Senior residents’ perceived need of and preferences for “smart home” sensor technologies. Int. J. Technol. Assess. Health Care 2008, 24, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Vodopivec-Jamsek, V.; de Jongh, T.; Gurol-Urganci, I.; Atun, R.; Car, J. Mobile phone messaging for preventive health care. Cochrane Database Syst. Rev. 2012, 12, CD007457. [Google Scholar] [CrossRef] [PubMed]
- Sarasohn-Kahn, J. How Smartphones are Changing Health Care for Consumers and Providers. Available online: https://www.chcf.org/wp-content/uploads/2017/12/PDF-HowSmartphonesChangingHealthCare.pdf (accessed on 3 July 2019).
- Bieber, G.; Kirste, T.; Urban, B. Ambient interaction by smart watches. In Proceedings of the 5th International Conference on PErvasive Technologies Related to Assistive Environments, Heraklion, Crete, Greece, 6–8 June 2012. article no. 39. [Google Scholar]
- Free, C.; Phillips, G.; Galli, L.; Watson, L.; Felix, L.; Edwards, P.; Haines, A. The effectiveness of mobile-health technology-based health behaviour change or disease management interventions for health care consumers: A systematic review. PLoS Med. 2013, 10, e1001362. [Google Scholar] [CrossRef]
- Porzi, L.; Messelodi, S.; Modena, C.M.; Ricci, E. A smart watch-based gesture recognition system for assisting people with visual impairments. In Proceedings of the 3rd ACM International Workshop on Interactive Multimedia on Mobile Portable Devices, Barcelona, Spain, 22 October 2013; pp. 19–24. [Google Scholar]
- Hamel, M.B.; Cortez, N.G.; Cohen, I.G.; Kesselheim, A.S. FDA regulation of mobile health technologies. New Engl. J. Med. 2014, 371, 372. [Google Scholar]
- Shcherbina, A.; Mattsson, C.M.; Waggott, D.; Salisbury, H.; Christle, J.W.; Hastie, T.; Ashley, E.A. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J. Pers. Med. 2017, 7, 3. [Google Scholar] [CrossRef]
- Solanas, A.; Patsakis, C.; Conti, M.; Vlachos, I.S.; Ramos, V.; Falcone, F.; Postolache, O.; Perez-martinez, P.A.; Pietro, R.D.; Perrea, D.N.; et al. Smart health: A context-aware health paradigm within smart cities. IEEE Commun. Mag. 2014, 52, 74–81. [Google Scholar] [CrossRef]
- Baig, M.M.; Gholamhosseini, H. Smart health monitoring systems: An overview of design and modeling. J. Med Syst. 2013, 37, 9898. [Google Scholar] [CrossRef]


| Method | Smart Technology | Assessment Method | Group Decision Making | Consensus | Aggregation |
|---|---|---|---|---|---|
| Chen and Chiu [3] | All | Literature review | No | - | - |
| Haymes et al. [4] | Not specified | Behavior analysis | No | - | - |
| Chiu and Chen [5] | Smart mobile services | Learning curve analysis | No | - | - |
| Chen [6] | All | FGM-ACO-FWM | Yes | Not guaranteed | Anterior-aggregation |
| Chen [7] | All | FGM-FI-FWM | Yes | Guaranteed | Posterior-aggregation |
| Our proposed methodology | All | ACO-FI-FWM | Yes | Guaranteed | Posterior-aggregation |
| C1 | C2 | C3 | C4 | C5 | |
|---|---|---|---|---|---|
| C1 | 1 | (1, 5, 9), (3, 7, 9), (3, 7, 9) | (1, 1, 5), (1, 5, 9), (1, 1, 5) | (3, 7, 9), (5, 9, 9), (1, 1, 5) | (1, 5, 9), (1, 5, 9), (1, 3, 7) |
| C2 | - | 1 | (1, 1, 5), (1, 4, 8), (1, 3, 7) | (3, 7, 9), (1, 3, 7), (1, 1, 5) | - |
| C3 | - | - | 1 | - | (1, 5, 9), (1, 4, 8), (1, 5, 9) |
| C4 | - | - | (1, 1, 5), (1, 3, 7), (1, 1, 5) | 1 | (3, 7, 9), (1, 5, 9), (1, 3, 7) |
| C5 | - | (1, 3, 7), (1, 5, 9), (1, 4, 8) | - | - | 1 |
| C1 | C2 | C3 | C4 | C5 | |
|---|---|---|---|---|---|
| C1 | 1 | (1, 5, 9), (3, 7, 9), (3, 7, 9) | (1, 1, 5), (1, 3, 7), (1, 1, 5) | (3, 7, 9), (1, 5, 9), (1, 1, 5) | (1, 5, 9), (1, 5, 9), (1, 3, 7) |
| C2 | - | 1 | (1, 1, 5), (1, 1, 5), (1, 3, 7) | (3, 7, 9), (1, 5, 9), (1, 1, 5) | - |
| C3 | - | - | 1 | - | (1, 5, 9), (1, 4, 8), (1, 5, 9) |
| C4 | - | - | (1, 1, 5), (1, 3, 7), (1, 1, 5) | 1 | (3, 7, 9), (1, 4, 8), (1, 3, 7) |
| C5 | - | (1, 3, 7), (1, 5, 9), (1, 4, 8) | - | - | 1 |
| Smart Health Practice | C1 (Unobtrusiveness) | C2 (Online Social Networking) | C3 (Cost Effectiveness) | C4 (Availability of Mobile Health Care Facilities) | C5 (Correct, Reliable, and Robust Identification) |
|---|---|---|---|---|---|
| Smart body analyzers | (1.00, 2.00, 3.00) | (1.00, 2.00, 3.00) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (2.50, 3.50, 4.50) |
| Smart clothes | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (2.50, 3.50, 4.50) |
| Smart glasses | (0.00, 1.00, 2.00) | (3.33, 4.33, 5.00) | (0.00, 1.00, 2.00) | (2.00, 3.00, 4.00) | (2.50, 3.50, 4.50) |
| Smart mobile services | (3.67, 4.67, 5.00) | (3.67, 4.67, 5.00) | (3.67, 4.67, 5.00) | (3.67, 4.67, 5.00) | (3.33, 4.33, 5.00) |
| Smart motion sensors | (2.00, 3.00, 4.00) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (3.67, 4.67, 5.00) |
| Smart phones | (3.67, 4.67, 5.00) | (3.67, 4.67, 5.00) | (2.50, 3.50, 4.50) | (3.67, 4.67, 5.00) | (3.67, 4.67, 5.00) |
| Smart smoke alarms | (2.00, 3.00, 4.00) | (0.00, 1.00, 2.00) | (1.00, 2.00, 3.00) | (2.00, 3.00, 4.00) | (3.67, 4.67, 5.00) |
| Smart toilets | (1.00, 2.00, 3.00) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (2.00, 3.00, 4.00) |
| Smart watches | (3.67, 4.67, 5.00) | (2.50, 3.50, 4.50) | (1.00, 2.00, 3.00) | (3.67, 4.67, 5.00) | (3.67, 4.67, 5.00) |
| Smart wheelchairs | (2.50, 3.50, 4.50) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (2.00, 3.00, 4.00) | (2.00, 3.00, 4.00) |
| Smart wigs | (2.00, 3.00, 4.00) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (0.00, 1.00, 2.00) | (2.50, 3.50, 4.50) |
| Smart Health Practice | Defuzzified Suitability |
|---|---|
| Smart body analyzers | 2.10 |
| Smart clothes | 1.52 |
| Smart glasses | 2.40 |
| Smart mobile services | 4.64 |
| Smart motion sensors | 2.45 |
| Smart phones | 4.54 |
| Smart smoke alarms | 2.91 |
| Smart toilets | 1.86 |
| Smart watches | 4.17 |
| Smart wheelchairs | 2.79 |
| Smart wigs | 2.33 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, T.-C.T.; Wang, Y.-C.; Lin, Y.-C.; Wu, H.-C.; Lin, H.-F. A Fuzzy Collaborative Approach for Evaluating the Suitability of a Smart Health Practice. Mathematics 2019, 7, 1180. https://doi.org/10.3390/math7121180
Chen T-CT, Wang Y-C, Lin Y-C, Wu H-C, Lin H-F. A Fuzzy Collaborative Approach for Evaluating the Suitability of a Smart Health Practice. Mathematics. 2019; 7(12):1180. https://doi.org/10.3390/math7121180
Chicago/Turabian StyleChen, Tin-Chih Toly, Yu-Cheng Wang, Yu-Cheng Lin, Hsin-Chieh Wu, and Hai-Fen Lin. 2019. "A Fuzzy Collaborative Approach for Evaluating the Suitability of a Smart Health Practice" Mathematics 7, no. 12: 1180. https://doi.org/10.3390/math7121180
APA StyleChen, T.-C. T., Wang, Y.-C., Lin, Y.-C., Wu, H.-C., & Lin, H.-F. (2019). A Fuzzy Collaborative Approach for Evaluating the Suitability of a Smart Health Practice. Mathematics, 7(12), 1180. https://doi.org/10.3390/math7121180








