An Outer Approximation Method for Scheduling Elective Surgeries with Sequence Dependent Setup Times to Multiple Operating Rooms
Abstract
:1. Introduction
2. Problem Description and Mathematical Formulation
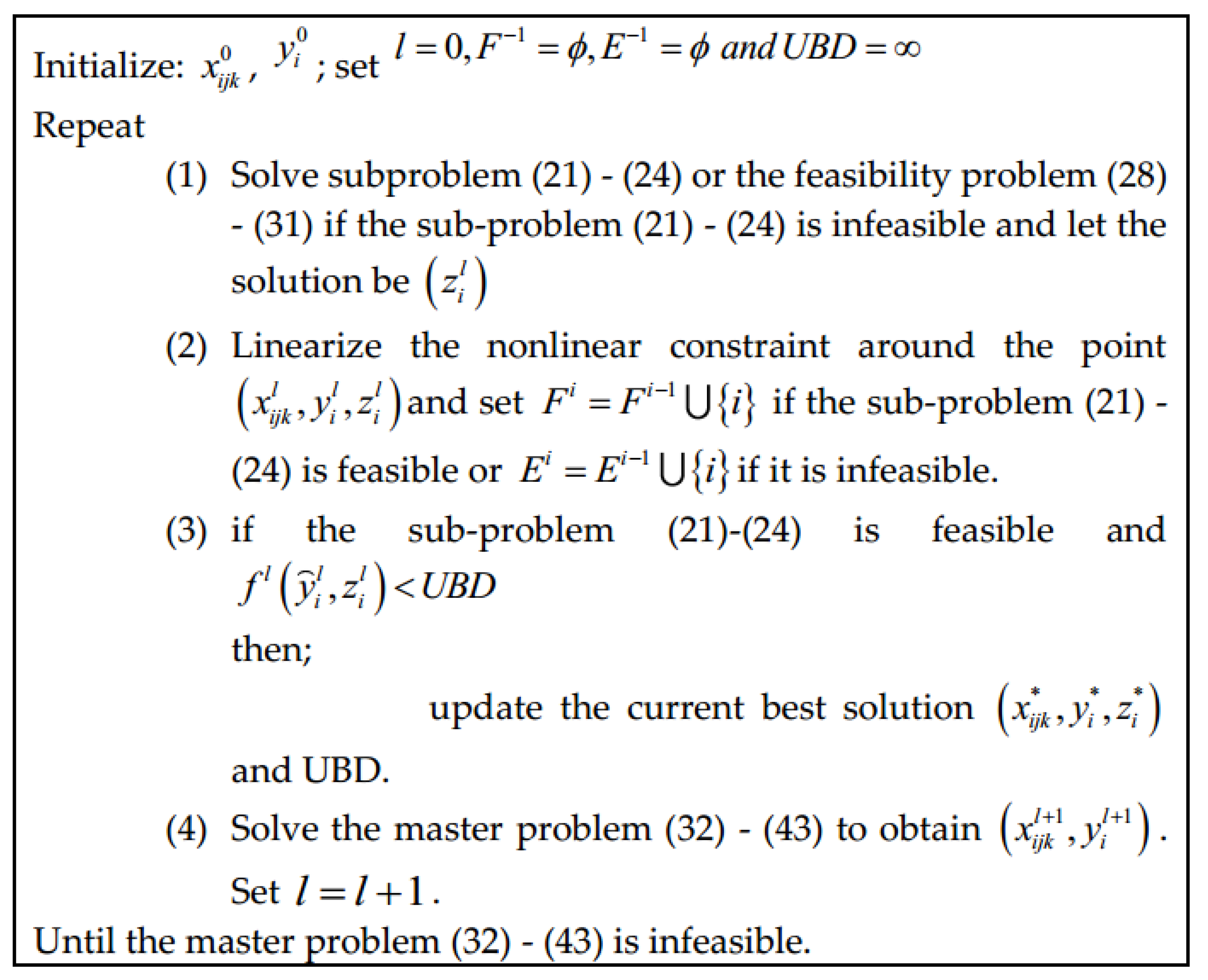
3. Solution Method
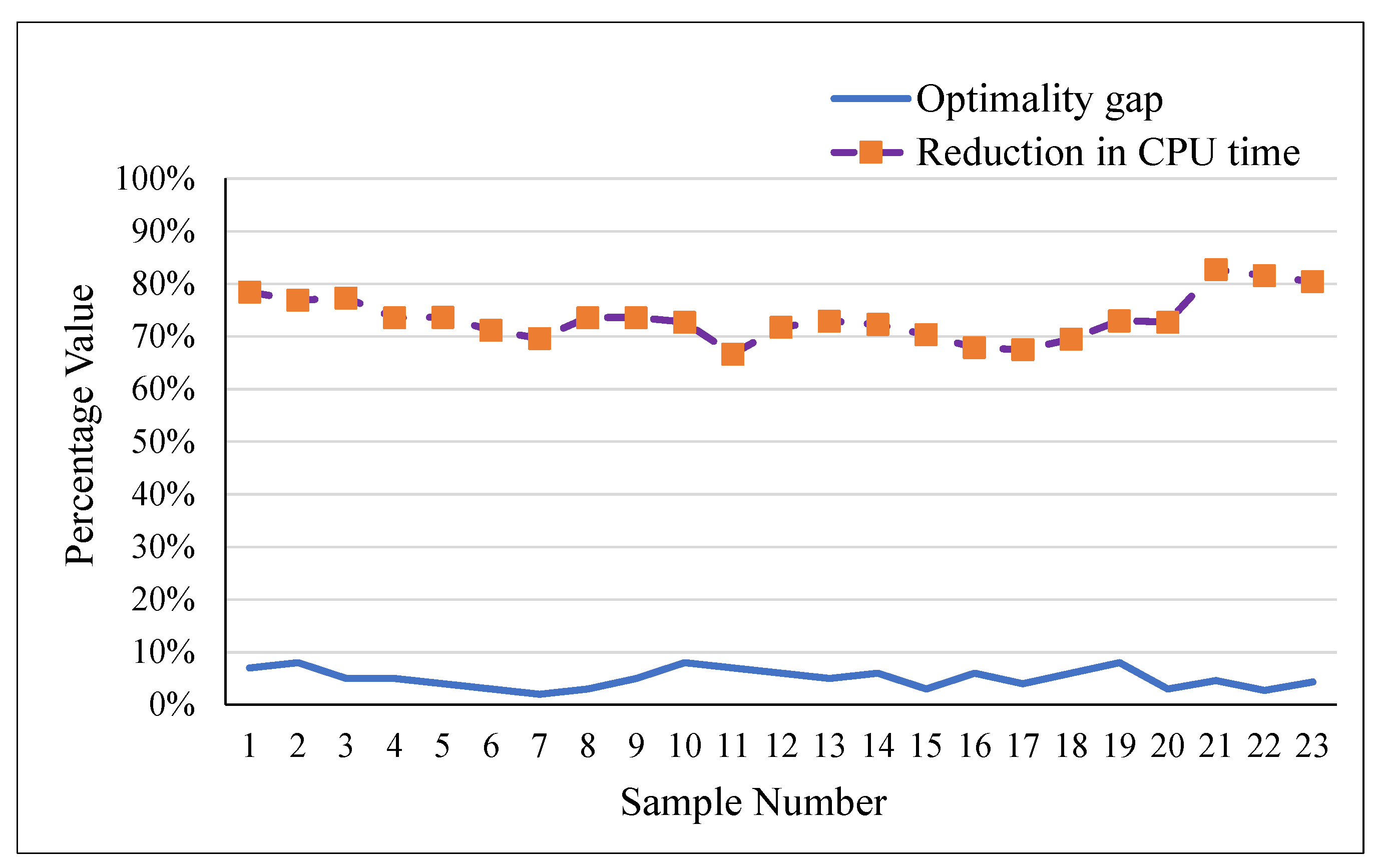
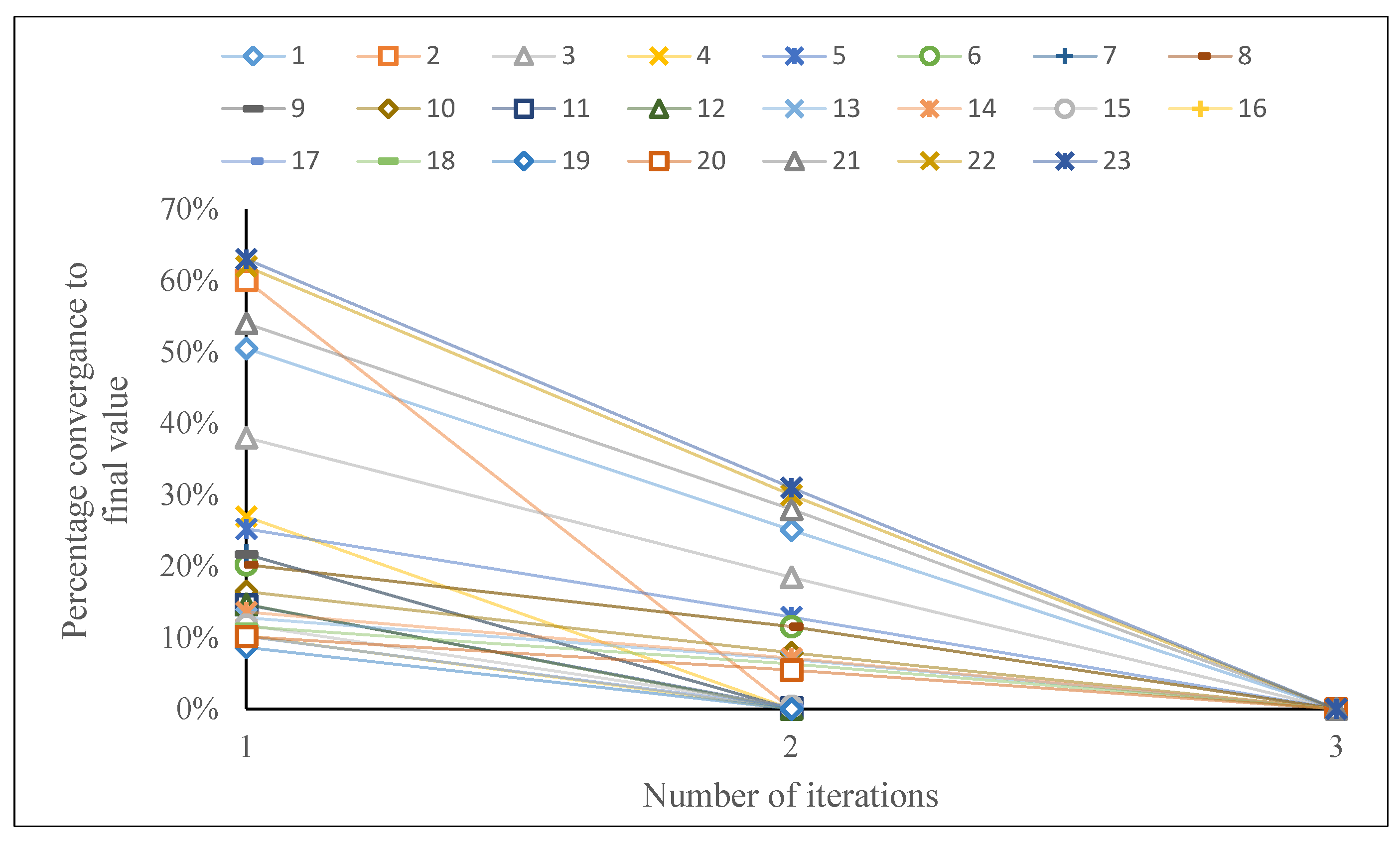
4. Computational Experiments and Results
Case Study
5. Conclusions and Suggestions for Future Research
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhao, Z.; Li, X. Scheduling elective surgeries with sequence-dependent setup times to multiple operating rooms using constraint programming. Oper. Res. Health Care 2014, 3, 160–167. [Google Scholar] [CrossRef]
- Denton, B.T.; Miller, A.J.; Balasubramanian, H.J.; Huschka, T.R. Optimal allocation of surgery blocks to operating rooms under uncertainty. Oper. Res. 2010, 58, 802–816. [Google Scholar] [CrossRef]
- Moosavi, A.; Ebrahimnejad, S. Scheduling of elective patients considering upstream and downstream units and emergency demand using robust optimization. Comput. Ind. Eng. 2018, 120, 216–233. [Google Scholar] [CrossRef]
- Moosavi, A.; Ebrahimnejad, S. Robust operating room planning considering upstream and downstream units: A new two-stage heuristic algorithm. Comput. Ind. Eng. 2020, 143, 106387. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Y.; Tang, J. A distributionally robust optimization approach for surgery block allocation. Eur. J. Oper. Res. 2019, 273, 740–753. [Google Scholar] [CrossRef]
- Bargetto, R.; Garaix, T.; Xie, X. A branch-and-price-and-cut algorithm for operating room scheduling under human resource constraints. Comput. Oper. Res. 2023, 152, 106136. [Google Scholar] [CrossRef]
- De Simone, B.; Agnoletti, V.; Rosato, C.; Kaafarani, H.; Stahel, P.F.; Collaborative, O.; Catena, R.; Catena, F. The “Operating Room Surgical Activity”(ORSA) study: A snap-shot international survey on the global management of the operating theatres for emergency surgery. When to persist is diabolical…. Res. Sq. 2023; preprint. [Google Scholar]
- Cardoen, B.; Demeulemeester, E.; Beliën, J. Operating room planning and scheduling: A literature review. Eur. J. Oper. Res. 2010, 201, 921–932. [Google Scholar] [CrossRef]
- Jebali, A.; Diabat, A. A stochastic model for operating room planning under capacity constraints. Int. J. Prod. Res. 2015, 53, 7252–7270. [Google Scholar] [CrossRef]
- Hof, S.; Fügener, A.; Schoenfelder, J.; Brunner, J.O. Case mix planning in hospitals: A review and future agenda. Health Care Manag. Sci. 2017, 20, 207–220. [Google Scholar] [CrossRef] [PubMed]
- Guerriero, F.; Guido, R. Operational research in the management of the operating theatre: A survey. Health Care Manag. Sci. 2011, 14, 89–114. [Google Scholar] [CrossRef] [PubMed]
- Batun, S.; Denton, B.T.; Huschka, T.R.; Schaefer, A.J. Operating room pooling and parallel surgery processing under uncertainty. INFORMS J. Comput. 2011, 23, 220–237. [Google Scholar] [CrossRef]
- Hashemi Doulabi, S.H.; Rousseau, L.-M.; Pesant, G. A constraint-programming-based branch-and-price-and-cut approach for operating room planning and scheduling. INFORMS J. Comput. 2016, 28, 432–448. [Google Scholar] [CrossRef]
- Fei, H.; Chu, C.; Meskens, N. Solving a tactical operating room planning problem by a column-generation-based heuristic procedure with four criteria. Ann. Oper. Res. 2009, 166, 91. [Google Scholar] [CrossRef]
- Marques, I.; Captivo, M.E.; Pato, M.V. An integer programming approach to elective surgery scheduling. OR Spectr. 2012, 34, 407–427. [Google Scholar] [CrossRef]
- Marques, I.; Captivo, M.E.; Pato, M.V. Scheduling elective surgeries in a Portuguese hospital using a genetic heuristic. Oper. Res. Health Care 2014, 3, 59–72. [Google Scholar] [CrossRef]
- Fei, H.; Meskens, N.; Chu, C. A planning and scheduling problem for an operating theatre using an open scheduling strategy. Comput. Ind. Eng. 2010, 58, 221–230. [Google Scholar] [CrossRef]
- Denton, B.; Viapiano, J.; Vogl, A. Optimization of surgery sequencing and scheduling decisions under uncertainty. Health Care Manag. Sci. 2007, 10, 13–24. [Google Scholar] [CrossRef]
- Pham, D.-N.; Klinkert, A. Surgical case scheduling as a generalized job shop scheduling problem. Eur. J. Oper. Res. 2008, 185, 1011–1025. [Google Scholar] [CrossRef]
- Oliveira, M.; Bélanger, V.; Marques, I.; Ruiz, A. Assessing the impact of patient prioritization on operating room schedules. Oper. Res. Health Care 2020, 24, 100232. [Google Scholar] [CrossRef]
- Younespour, M.; Atighehchian, A.; Kianfar, K.; Esfahani, E.T. Using mixed integer programming and constraint programming for operating rooms scheduling with modified block strategy. Oper. Res. Health Care 2019, 23, 100220. [Google Scholar] [CrossRef]
- Addis, B.; Carello, G.; Grosso, A.; Tànfani, E. Operating room scheduling and rescheduling: A rolling horizon approach. Flex. Serv. Manuf. J. 2016, 28, 206–232. [Google Scholar] [CrossRef]
- Landa, P.; Aringhieri, R.; Soriano, P.; Tànfani, E.; Testi, A. A hybrid optimization algorithm for surgeries scheduling. Oper. Res. Health Care 2016, 8, 103–114. [Google Scholar] [CrossRef]
- Neyshabouri, S.; Berg, B.P. Two-stage robust optimization approach to elective surgery and downstream capacity planning. Eur. J. Oper. Res. 2017, 260, 21–40. [Google Scholar] [CrossRef]
- Rachuba, S.; Werners, B. A fuzzy multi-criteria approach for robust operating room schedules. Ann. Oper. Res. 2017, 251, 325–350. [Google Scholar] [CrossRef]
- Bam, M.; Denton, B.T.; Van Oyen, M.P.; Cowen, M.E. Surgery scheduling with recovery resources. IISE Trans. 2017, 49, 942–955. [Google Scholar] [CrossRef]
- Kroer, L.R.; Foverskov, K.; Vilhelmsen, C.; Hansen, A.S.; Larsen, J. Planning and scheduling operating rooms for elective and emergency surgeries with uncertain duration. Oper. Res. Health Care 2018, 19, 107–119. [Google Scholar] [CrossRef]
- Marques, I.; Captivo, M.E.; Barros, N. Optimizing the master surgery schedule in a private hospital. Oper. Res. Health Care 2019, 20, 11–24. [Google Scholar] [CrossRef]
- Jebali, A.; Alouane, A.B.H.; Ladet, P. Operating rooms scheduling. Int. J. Prod. Econ. 2006, 99, 52–62. [Google Scholar] [CrossRef]
- Tayyab, A.; Ullah, S.; Mahmood, T.; Ghadi, Y.Y.; Latif, B.; Aljuaid, H. Modeling of Multi-Level Planning of Shifting Bottleneck Resources Integrated with Downstream Wards in a Hospital. Appl. Sci. 2023, 13, 3616. [Google Scholar] [CrossRef]
- Tayyab, A.; Saif, U. A Two-Stage Genetic Artificial Bee Colony Algorithm for Solving Integrated Operating Room Planning and Scheduling Problem With Capacity Constraints of Downstream Wards. IEEE Access 2022, 10, 131109–131127. [Google Scholar] [CrossRef]
- Kuo, P.C.; Schroeder, R.A.; Mahaffey, S.; Bollinger, R.R. Optimization of operating room allocation using linear programming techniques. J. Am. Coll. Surg. 2003, 197, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Mulholland, M.W.; Abrahamse, P.; Bahl, V. Linear programming to optimize performance in a department of surgery. J. Am. Coll. Surg. 2005, 200, 861–868. [Google Scholar] [CrossRef] [PubMed]
- Dexter, F.; Blake, J.T.; Penning, D.H.; Lubarsky, D.A. Calculating a potential increase in hospital margin for elective surgery by changing operating room time allocations or increasing nursing staffing to permit completion of more cases: A case study. Anesth. Analg. 2002, 94, 138–142. [Google Scholar] [CrossRef] [PubMed]
- Dexter, F.; Blake, J.T.; Penning, D.H.; Sloan, B.; Chung, P.; Lubarsky, D.A. Use of linear programming to estimate impact of changes in a hospital's operating room time allocation on perioperative variable costs. J. Am. Soc. Anesthesiol. 2002, 96, 718–724. [Google Scholar] [CrossRef]
- Cappanera, P.; Visintin, F.; Banditori, C. Addressing conflicting stakeholders’ priorities in surgical scheduling by goal programming. Flex. Serv. Manuf. J. 2018, 30, 252–271. [Google Scholar] [CrossRef]
- Blake, J.T.; Carter, M.W. A goal programming approach to strategic resource allocation in acute care hospitals. Eur. J. Oper. Res. 2002, 140, 541–561. [Google Scholar] [CrossRef]
- Adan, I.; Bekkers, J.; Dellaert, N.; Jeunet, J.; Vissers, J. Improving operational effectiveness of tactical master plans for emergency and elective patients under stochastic demand and capacitated resources. Eur. J. Oper. Res. 2011, 213, 290–308. [Google Scholar] [CrossRef]
- Testi, A.; Tànfani, E. Tactical and operational decisions for operating room planning: Efficiency and welfare implications. Health Care Manag. Sci. 2009, 12, 363–373. [Google Scholar] [CrossRef]
- Tànfani, E.; Testi, A. A pre-assignment heuristic algorithm for the Master Surgical Schedule Problem (MSSP). Ann. Oper. Res. 2010, 178, 105–119. [Google Scholar] [CrossRef]
- Ballestín, F.; Pérez, Á.; Quintanilla, S. Scheduling and rescheduling elective patients in operating rooms to minimise the percentage of tardy patients. J. Sched. 2019, 22, 107–118. [Google Scholar] [CrossRef]
- Vissers, J.M.; Adan, I.J.; Bekkers, J.A. Patient mix optimization in tactical cardiothoracic surgery planning: A case study. IMA J. Manag. Math. 2005, 16, 281–304. [Google Scholar] [CrossRef]
- Van Huele, C.; Vanhoucke, M. Operating theatre modelling: Integrating social measures. J. Simul. 2015, 9, 121–128. [Google Scholar] [CrossRef]
- Aringhieri, R.; Landa, P.; Soriano, P.; Tanfani, E.; Testi, A. A two level metaheuristic for the operating room scheduling and assignment problem. Comput. Oper. Res. 2015, 54, 21–34. [Google Scholar] [CrossRef]
- Beliën, J.; Demeulemeester, E. Building cyclic master surgery schedules with leveled resulting bed occupancy. Eur. J. Oper. Res. 2007, 176, 1185–1204. [Google Scholar] [CrossRef]
- Beliën, J.; Demeulemeester, E.; Cardoen, B. A decision support system for cyclic master surgery scheduling with multiple objectives. J. Sched. 2009, 12, 147–161. [Google Scholar] [CrossRef]
- Cappanera, P.; Visintin, F.; Banditori, C. Comparing resource balancing criteria in master surgical scheduling: A combined optimisation-simulation approach. Int. J. Prod. Econ. 2014, 158, 179–196. [Google Scholar] [CrossRef]
- Heider, S.; Schoenfelder, J.; McRae, S.; Koperna, T.; Brunner, J.O. Tactical scheduling of surgeries to level bed utilization in the intensive care unit. IISE Trans. Healthc. Syst. Eng. 2020, 10, 229–242. [Google Scholar] [CrossRef]
- Heydari, M.; Soudi, A. Predictive/reactive planning and scheduling of a surgical suite with emergency patient arrival. J. Med. Syst. 2016, 40, 30. [Google Scholar] [CrossRef]
- Akbarzadeh, B.; Moslehi, G.; Reisi-Nafchi, M.; Maenhout, B. The re-planning and scheduling of surgical cases in the operating room department after block release time with resource rescheduling. Eur. J. Oper. Res. 2019, 278, 596–614. [Google Scholar] [CrossRef]
- Kamran, M.A.; Karimi, B.; Dellaert, N. A column-generation-heuristic-based benders’ decomposition for solving adaptive allocation scheduling of patients in operating rooms. Comput. Ind. Eng. 2020, 148, 106698. [Google Scholar] [CrossRef]
- Wang, Y.; Tang, J.; Fung, R.Y. A column-generation-based heuristic algorithm for solving operating theater planning problem under stochastic demand and surgery cancellation risk. Int. J. Prod. Econ. 2014, 158, 28–36. [Google Scholar] [CrossRef]
- Zhang, J.; Dridi, M.; El Moudni, A. Column-generation-based heuristic approaches to stochastic surgery scheduling with downstream capacity constraints. Int. J. Prod. Econ. 2020, 229, 107764. [Google Scholar] [CrossRef]
- Beliën, J.; Demeulemeester, E. A branch-and-price approach for integrating nurse and surgery scheduling. Eur. J. Oper. Res. 2008, 189, 652–668. [Google Scholar] [CrossRef]
- Cardoen, B.; Demeulemeester, E.; Beliën, J. Sequencing surgical cases in a day-care environment: An exact branch-and-price approach. Comput. Oper. Res. 2009, 36, 2660–2669. [Google Scholar] [CrossRef]
- Luo, L.; Luo, Y.; Qin, C. Admission control policies for surgery patients. J. Med. Syst. 2017, 41, 131. [Google Scholar] [CrossRef]
- Barz, C.; Rajaram, K. Elective patient admission and scheduling under multiple resource constraints. Prod. Oper. Manag. 2015, 24, 1907–1930. [Google Scholar] [CrossRef]
- Zhang, J.; Dridi, M.; El Moudni, A. A two-level optimization model for elective surgery scheduling with downstream capacity constraints. Eur. J. Oper. Res. 2019, 276, 602–613. [Google Scholar] [CrossRef]
- Cardoen, B.; Demeulemeester, E.; Beliën, J. Optimizing a multiple objective surgical case sequencing problem. Int. J. Prod. Econ. 2009, 119, 354–366. [Google Scholar] [CrossRef]
- Berg, B.P.; Denton, B.T. Fast approximation methods for online scheduling of outpatient procedure centers. INFORMS J. Comput. 2017, 29, 631–644. [Google Scholar] [CrossRef]
- Stuart, K.; Kozan, E. Reactive scheduling model for the operating theatre. Flex. Serv. Manuf. J. 2012, 24, 400–421. [Google Scholar] [CrossRef]
- Fügener, A.; Hans, E.W.; Kolisch, R.; Kortbeek, N.; Vanberkel, P.T. Master surgery scheduling with consideration of multiple downstream units. Eur. J. Oper. Res. 2014, 239, 227–236. [Google Scholar] [CrossRef]
- Nemati, S.; Shylo, O.V.; Prokopyev, O.A.; Schaefer, A.J. The surgical patient routing problem: A central planner approach. INFORMS J. Comput. 2016, 28, 657–673. [Google Scholar] [CrossRef]
- Ma, G.; Demeulemeester, E. A multilevel integrative approach to hospital case mix and capacity planning. Comput. Oper. Res. 2013, 40, 2198–2207. [Google Scholar] [CrossRef]
- Zhang, Z.; Denton, B.T.; Xie, X. Branch and price for chance-constrained bin packing. INFORMS J. Comput. 2020, 32, 547–564. [Google Scholar] [CrossRef]
- Zhang, Z.; Xie, X.; Geng, N. Dynamic surgery assignment of multiple operating rooms with planned surgeon arrival times. IEEE Trans. Autom. Sci. Eng. 2013, 11, 680–691. [Google Scholar] [CrossRef]
- Deng, Y.; Shen, S.; Denton, B. Chance-constrained surgery planning under conditions of limited and ambiguous data. INFORMS J. Comput. 2019, 31, 559–575. [Google Scholar] [CrossRef]
- Marques, I.; Captivo, M.E.; Pato, M.V. A bicriteria heuristic for an elective surgery scheduling problem. Health Care Manag. Sci. 2015, 18, 251–266. [Google Scholar] [CrossRef]
- Vali-Siar, M.M.; Gholami, S.; Ramezanian, R. Multi-period and multi-resource operating room scheduling under uncertainty: A case study. Comput. Ind. Eng. 2018, 126, 549–568. [Google Scholar] [CrossRef]
- Hans, E.; Wullink, G.; Van Houdenhoven, M.; Kazemier, G. Robust surgery loading. Eur. J. Oper. Res. 2008, 185, 1038–1050. [Google Scholar] [CrossRef]
- Ewen, H.; Mönch, L. A simulation-based framework to schedule surgeries in an eye hospital. IIE Trans. Healthc. Syst. Eng. 2014, 4, 191–208. [Google Scholar] [CrossRef]
- Spratt, B.; Kozan, E. Waiting list management through master surgical schedules: A case study. Oper. Res. Health Care 2016, 10, 49–64. [Google Scholar] [CrossRef]
- Molina-Pariente, J.M.; Hans, E.W.; Framinan, J.M.; Gomez-Cia, T. New heuristics for planning operating rooms. Comput. Ind. Eng. 2015, 90, 429–443. [Google Scholar] [CrossRef]
- Roshanaei, V.; Booth, K.E.; Aleman, D.M.; Urbach, D.R.; Beck, J.C. Branch-and-check methods for multi-level operating room planning and scheduling. Int. J. Prod. Econ. 2020, 220, 107433. [Google Scholar] [CrossRef]
- Hamid, M.; Hamid, M.; Musavi, M.; Azadeh, A. Scheduling elective patients based on sequence-dependent setup times in an open-heart surgical department using an optimization and simulation approach. Simulation 2019, 95, 1141–1164. [Google Scholar] [CrossRef]
- Van Essen, J.T.; Hans, E.W.; Hurink, J.L.; Oversberg, A. Minimizing the waiting time for emergency surgery. Oper. Res. Health Care 2012, 1, 34–44. [Google Scholar] [CrossRef]
- Schneider, A.T.; van Essen, J.T.; Carlier, M.; Hans, E.W. Scheduling surgery groups considering multiple downstream resources. Eur. J. Oper. Res. 2020, 282, 741–752. [Google Scholar] [CrossRef]
- Van den Broek d’Obrenan, A.; Ridder, A.; Roubos, D.; Stougie, L. Minimizing bed occupancy variance by scheduling patients under uncertainty. Eur. J. Oper. Res. 2020, 286, 336–349. [Google Scholar] [CrossRef]
- Vancroonenburg, W.; De Causmaecker, P.; Berghe, G.V. Chance-constrained admission scheduling of elective surgical patients in a dynamic, uncertain setting. Oper. Res. Health Care 2019, 22, 100196. [Google Scholar] [CrossRef]
- Nazif, H. Operating room surgery scheduling with fuzzy surgery durations using a metaheuristic approach. Adv. Oper. Res. 2018, 2018, 8637598. [Google Scholar] [CrossRef]
- Xiang, W.; Yin, J.; Lim, G. An ant colony optimization approach for solving an operating room surgery scheduling problem. Comput. Ind. Eng. 2015, 85, 335–345. [Google Scholar] [CrossRef]
- Saremi, A.; Jula, P.; ElMekkawy, T.; Wang, G.G. Appointment scheduling of outpatient surgical services in a multistage operating room department. Int. J. Prod. Econ. 2013, 141, 646–658. [Google Scholar] [CrossRef]
- Duran, M.A.; Grossmann, I.E. An outer-approximation algorithm for a class of mixed-integer nonlinear programs. Math. Program. 1986, 36, 307–339. [Google Scholar] [CrossRef]
- Fletcher, R.; Leyffer, S. Solving mixed integer nonlinear programs by outer approximation. Math. Program. 1994, 66, 327–349. [Google Scholar] [CrossRef]
- Grossmann, I.E.; Kravanja, Z. Mixed-integer nonlinear programming techniques for process systems engineering. Comput. Chem. Eng. 1995, 19, 189–204. [Google Scholar] [CrossRef]
- Freeman, N.; Zhao, M.; Melouk, S. An iterative approach for case mix planning under uncertainty. Omega 2018, 76, 160–173. [Google Scholar] [CrossRef]
| Parameters | |
|---|---|
| The set of ORs | |
| The regular costs of OR per day | |
| The unit overtime costs of OR | |
| , including overtime | |
| The set of surgeries under consideration | |
| The operation time | |
| The set of specialities | |
| The index of specialities | |
| Decision variables | |
| is used, 0 otherwise | |
| , 0 otherwise | |
| Sample | No. of Patients | Specialties | ORs | Standard Model | Outer Approximation | ||||
|---|---|---|---|---|---|---|---|---|---|
| CPU (s) | Objective | CPU (s) | Objective | Optimality Gap | Reduction in CPU Time | ||||
| 1 | 15 | 3 | 2 | 51 | 11,960 | 11 | 12,795 | 7% | 78% |
| 2 | 20 | 3 | 2 | 52 | 11,120 | 12 | 12,053 | 8% | 77% |
| 3 | 25 | 3 | 3 | 53 | 16,040 | 12 | 16,867 | 5% | 77% |
| 4 | 30 | 4 | 3 | 53 | 21,240 | 14 | 22,342 | 5% | 74% |
| 5 | 35 | 4 | 4 | 57 | 25,320 | 15 | 26,315 | 4% | 74% |
| 6 | 40 | 4 | 4 | 59 | 28,940 | 17 | 29,691 | 3% | 71% |
| 7 | 45 | 4 | 4 | 56 | 29,100 | 17 | 29,791 | 2% | 70% |
| 8 | 50 | 4 | 5 | 72 | 35,720 | 19 | 36,644 | 3% | 74% |
| 9 | 55 | 5 | 5 | 72 | 36,020 | 19 | 37,800 | 5% | 74% |
| 10 | 60 | 5 | 6 | 77 | 38,440 | 21 | 41,600 | 8% | 73% |
| 11 | 70 | 5 | 6 | 75 | 42,700 | 25 | 45,500 | 7% | 67% |
| 12 | 75 | 5 | 6 | 78 | 43,840 | 22 | 46,600 | 6% | 72% |
| 13 | 80 | 5 | 7 | 85 | 49,480 | 23 | 51,960 | 5% | 73% |
| 14 | 85 | 5 | 7 | 83 | 48,300 | 23 | 51,120 | 6% | 72% |
| 15 | 90 | 5 | 7 | 81 | 51,140 | 24 | 52,728 | 3% | 70% |
| 16 | 95 | 5 | 8 | 81 | 56,800 | 26 | 60,060 | 6% | 68% |
| 17 | 100 | 6 | 8 | 80 | 58,100 | 26 | 60,332 | 4% | 68% |
| 18 | 105 | 6 | 8 | 82 | 57,460 | 25 | 60,810 | 6% | 70% |
| 19 | 110 | 6 | 9 | 100 | 64,920 | 27 | 70,240 | 8% | 73% |
| 20 | 115 | 6 | 9 | 99 | 66,340 | 27 | 68,164 | 3% | 73% |
| 21 | 200 | 6 | 10 | 272 | 71,210 | 47 | 74,650 | 5% | 83% |
| 22 | 250 | 6 | 11 | 315 | 75,250 | 58 | 77,380 | 3% | 82% |
| 23 | 300 | 6 | 12 | 358 | 77,440 | 70 | 80,960 | 4% | 80% |
| Day | Patients | Operating Rooms | CPU (s) | Objective | Average OR Overutilization | Average OR Overtime |
|---|---|---|---|---|---|---|
| 1 | 40 | 4 | 16 | 27,800 | 5% | 98 |
| 2 | 43 | 5 | 16 | 26,100 | 0% | 11 |
| 3 | 40 | 5 | 16 | 33,620 | 4% | 86 |
| 4 | 40 | 5 | 15 | 35,380 | 4% | 104 |
| 5 | 48 | 5 | 17 | 36,100 | 5% | 111 |
| 6 | 40 | 5 | 16 | 33,100 | 3% | 81 |
| 7 | 49 | 4 | 15 | 25,700 | 4% | 71 |
| 8 | 41 | 5 | 15 | 33,500 | 4% | 85 |
| 9 | 50 | 5 | 17 | 33,780 | 4% | 88 |
| 10 | 47 | 5 | 20 | 33,200 | 3% | 82 |
| 11 | 50 | 5 | 17 | 36,440 | 5% | 114 |
| 12 | 43 | 4 | 15 | 28,960 | 6% | 112 |
| 13 | 41 | 4 | 15 | 26,480 | 4% | 81 |
| 14 | 45 | 4 | 20 | 28,680 | 6% | 109 |
| 15 | 43 | 5 | 18 | 34,880 | 4% | 99 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tayyab, A.; Ullah, S.; Baki, M.F. An Outer Approximation Method for Scheduling Elective Surgeries with Sequence Dependent Setup Times to Multiple Operating Rooms. Mathematics 2023, 11, 2441. https://doi.org/10.3390/math11112441
Tayyab A, Ullah S, Baki MF. An Outer Approximation Method for Scheduling Elective Surgeries with Sequence Dependent Setup Times to Multiple Operating Rooms. Mathematics. 2023; 11(11):2441. https://doi.org/10.3390/math11112441
Chicago/Turabian StyleTayyab, Aisha, Saif Ullah, and Mohammed Fazle Baki. 2023. "An Outer Approximation Method for Scheduling Elective Surgeries with Sequence Dependent Setup Times to Multiple Operating Rooms" Mathematics 11, no. 11: 2441. https://doi.org/10.3390/math11112441
APA StyleTayyab, A., Ullah, S., & Baki, M. F. (2023). An Outer Approximation Method for Scheduling Elective Surgeries with Sequence Dependent Setup Times to Multiple Operating Rooms. Mathematics, 11(11), 2441. https://doi.org/10.3390/math11112441






