Group Physical Activity and Behavioral Practices in Adolescents with Autism: A Case Series on Integrated Educational Interventions
Abstract
1. Introduction
1.1. Physical Activity Interventions Increasing Motor and Cognitive Skills
1.2. Physical Activity Interventions Targeting Challenging Behaviors
1.3. The Present Study
2. Materials and Methods
2.1. Participants and Setting
2.2. Research Design
2.3. Instruments
2.4. Procedure and Intervention Protocol
2.5. Data Analysis
3. Results
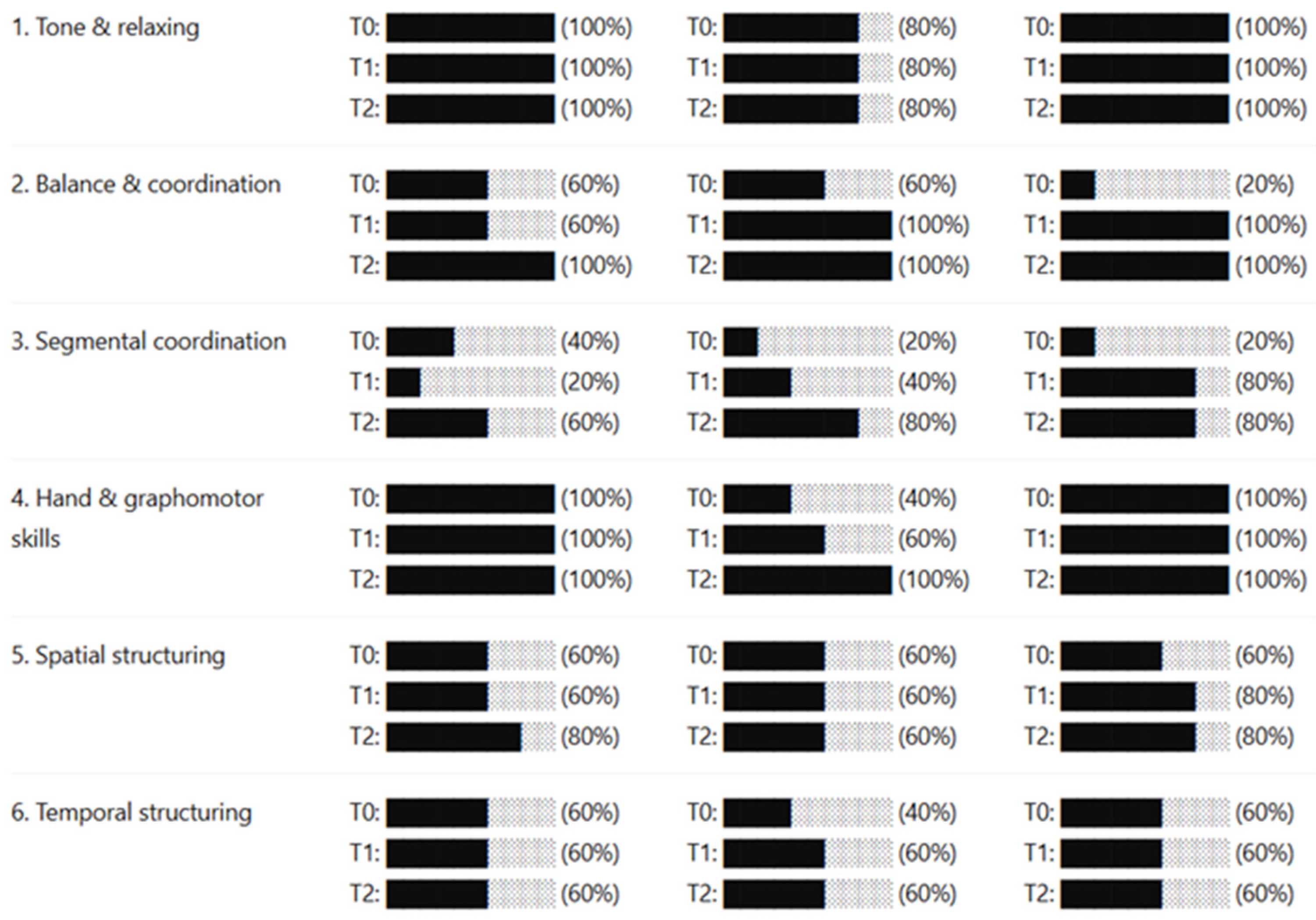
3.1. Capacity-Level Outcomes
3.2. Sub-Capacity Outcomes
3.3. Individual Trajectories
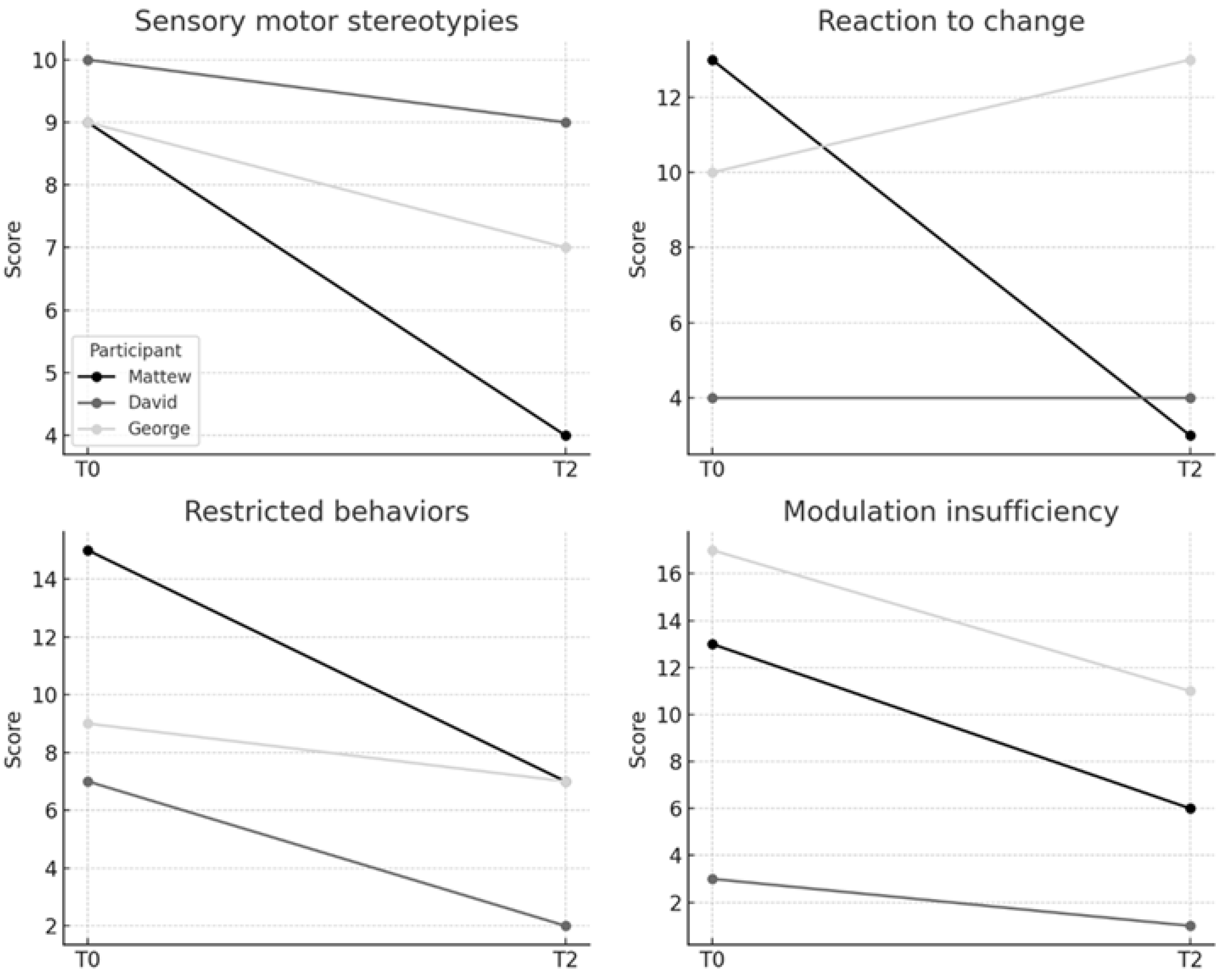
3.4. Changes in Repetitive Behaviors from Baseline to Post-Intervention
3.5. Exploratory Analysis of Baseline Characteristics as Potential Moderator
3.6. Parental Feedback
4. Discussion
4.1. Limitations
4.2. Strengths and Implications of the Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Domain/Capacity | Sub-Capacity | Training Task | Manuel | Dean | Gene |
|---|---|---|---|---|---|
| 1. Tone and Relaxing | Shift from activity to inactivity | Alternate arm circles, changing direction on the teacher’s command | ✓ | ||
| Arm circles (one arm forward–backward) on verbal command | ✓ | ||||
| Arm circles forward and backward | ✓ | ✓ | |||
| Arm circles, changing direction on verbal command. | ✓ | ✓ | |||
| 2. Balance and General Dynamic Coordination | Balance on one foot | Balance on dominant foot, hands on hips, eyes closed, 5″ | ✓ | ||
| Balance on left foot 18″ | ✓ | ✓ | ✓ | ||
| Balance on non-dominant foot, hands on hips, eyes closed, 5″ | ✓ | ||||
| Ball throw while balancing on one foot. | ✓ | ✓ | ✓ | ||
| Maintain balance on the dominant foot, hands on the hips, eyes closed, 5″ | ✓ | ✓ | |||
| Maintain balance on the dominant foot, hands on the hips, eyes open, 8″ | ✓ | ||||
| Maintain balance on non-dominant foot, hands on hips, eyes closed, 5″ | ✓ | ✓ | |||
| 2. Balance and General Dynamic Coordination | Balance on tiptoes | Balance on tiptoes for 10″, eyes open, while catching and throwing a ball (2 m) | ✓ | ||
| Balance on tiptoes, eyes open, catching and throwing a ball from 2 m | ✓ | ||||
| Maintain balance on tiptoes, eyes open, while catching and throwing a ball from 2 m, 10″ | ✓ | ||||
| Stand on tiptoes, hands on hips, 10″ | ✓ | ✓ | ✓ | ||
| 2. Balance and General Dynamic Coordination | Jumps with balance | Jumps on dominant leg 8 m, curved path, inside 40 cm lane | ✓ | ||
| Jumps on dominant leg 8 m, straight path, inside 40 cm lane | ✓ | ||||
| Jumps on dominant leg for 8 m, curved path, inside 40 cm lane | ✓ | ||||
| Jumps on non-dominant leg 8 m, straight path, inside 40 cm lane | ✓ | ||||
| Jumps on non-dominant leg for 8 m, straight path, inside 40 cm lane | ✓ | ||||
| Jumps on right foot (path 8 m) | ✓ | ||||
| 2. Balance and General Dynamic Coordination | Running with balance | Run 20 m on a curved path with low obstacles (10–20 cm), inside a 20 cm lane. | ✓ | ||
| Run 20 m on a curved path, inside a 20 cm lane. | ✓ | ||||
| Run about 20 m on a curved path with low obstacles (10–20 cm), inside a 20 cm lane. | ✓ | ||||
| Run about 20 m on a curved path with low obstacles (10–20 cm), inside a 30 cm lane. | ✓ | ||||
| Run approximately 20 m on a curved path, inside a 20 cm lane. | ✓ | ||||
| 2. Balance and General Dynamic Coordination | Running/jumping with balance | Jumps on right foot (path 8 m) | ✓ | ||
| Jumps on the spot, bringing knees to chest, 15″ | ✓ | ||||
| Jumps on the spot, dominant leg 15″ | ✓ | ||||
| Jumps on the spot, non-dominant leg 15″ | ✓ | ||||
| Skipping 20″ | ✓ | ||||
| 2. Balance and General Dynamic Coordination | Runs, hops, jumps on the spot | Jumps bringing knees to chest, 15″ | ✓ | ✓ | |
| Jumps on the spot, dominant leg, 15″ | ✓ | ✓ | |||
| Jumps on the spot, non-dominant leg, 15″ | ✓ | ✓ | |||
| Skipping 20″ | ✓ | ✓ | |||
| 3. Segmental Coordination | Asymmetrical arm–leg movements | Alternate arm swings (forward–backward) | ✓ | ||
| Alternate swings of arms with knee bends and head rotation | ✓ | ||||
| Leg swing with same-side hand touch | ✓ | ||||
| Leg swings forward, then outward | ✓ | ||||
| Move one arm forward and the other backward alternately. | ✓ | ✓ | |||
| Small jumps forward–backward (alternate legs) | ✓ | ||||
| Standing, arms extended forward, open one arm then the other, and rotate your head to follow. | ✓ | ||||
| Standing, arms forward, open one arm, then the other, rotating head to follow | ✓ | ||||
| Swing the leg outward, touch with the same-side hand, and rotate the head to the same side. | ✓ | ||||
| Swing one leg forward, touch with the same side, then the opposite hand. | ✓ | ✓ | |||
| 3. Segmental Coordination | Head–arm coordination | Arm–head coordination task | ✓ | ✓ | ✓ |
| Flex one leg backward, touch heel with same-side hand, rotate head to same side. | ✓ | ||||
| Standing, arms forward, alternate arm swings on the sagittal plane, and rotate the head to follow the backward arm. | ✓ | ||||
| Standing, arms forward, alternate arm swings on the sagittal plane, rotating the head to follow the backward arm | ✓ | ||||
| Swing the leg outward, touch with the same-side hand, and rotate the head to that side. | ✓ | ||||
| Touch heel with the same-side hand. | ✓ | ✓ | |||
| 3. Segmental Coordination | Symmetrical arm movements | Arm swings (forward–backward) + knee bends | ✓ | ||
| Jumps forward–backward with alternating arm swings on the sagittal plane | ✓ | ||||
| Side jumps (open–close legs) with arm swings upward on the frontal plane. | ✓ | ||||
| Standing, arm swings on the frontal plane (outward), raising the head to look at the hands | ✓ | ||||
| Standing, arm swings on the sagittal plane (forward), following with the head | ✓ | ||||
| Standing, swing arms on the frontal plane (outward), raising head to look at hands. | ✓ | ||||
| Standing, swing arms on the sagittal plane (forward), following with the head. | ✓ | ||||
| Standing, swing arms on the sagittal plane, following with the head. | ✓ | ||||
| 3. Segmental Coordination | Symmetrical arm–leg movements | Jumps forward–backward with alternating arm swings on the sagittal plane | ✓ | ||
| Side jumps (open–close legs) + arm swings upward from front to above, following with head. | ✓ | ||||
| Side jumps (open–close legs) + arm swings upward on the frontal plane, followed by the head. | ✓ | ||||
| Side jumps (open–close legs) with arm swings upward on the frontal plane. | ✓ | ||||
| Simultaneous arm swings (forward–backward) + knee bends | ✓ | ||||
| Small jumps forward–backward (alternate legs) | ✓ | ||||
| 4. Intersegmental Coordination | Arm–leg combined movements | Bicycle exercise | ✓ | ✓ | ✓ |
| Side jumps (open–close legs) + arm swings upward from front to above, following with head. | ✓ | ||||
| Small jumps forward–backward (alternate legs) | ✓ | ||||
| 5. Spatial Orientation | Movement in relation to peers | Run and pass peers (opposite facing direction) | ✓ | ✓ | ✓ |
| Run and pass peers (same facing direction) | ✓ | ✓ | ✓ | ||
| Run right and left, change direction on verbal request. | ✓ | ✓ | |||
| Run right and left, changing direction on verbal request. | ✓ | ||||
| 5. Spatial Orientation | Right–left on others | Identify the peer’s right/left hand, foot, eye, and ear on verbal request | ✓ | ||
| Indicate the peer’s right/left hand, foot, eye, ear (facing forward) | ✓ | ||||
| Indicate the peer’s right/left hand, foot, eye, ear (opposite facing direction) | ✓ | ||||
| Indicate the peer’s right/left hand, foot, eye, ear (same facing direction) | ✓ | ||||
| 5. Spatial Orientation | Right–left on self | Perform eight movements: touch the right/left eyes and ears with the corresponding hands. | ✓ | ||
| Perform eight movements: touch the right/left eyes and ears with the corresponding hands. | ✓ | ||||
| 5. Spatial Orientation | Spatial localization of objects | Hit the target 30 cm in diameter at 5 m (10 throws with a small ball + 10 throws with a big ball) | ✓ | ✓ | ✓ |
| Hit the target 60 cm in diameter at 5 m (10 throws with a small ball + 10 throws with a big ball) | ✓ | ✓ | ✓ | ||
| Hit teacher moving on the short side of the gym from 5 m (10 throws) | ✓ | ✓ | |||
| Hit the teacher walking along the short side of the gym from 5 m (10 throws) | ✓ | ||||
| 5. Spatial Orientation | Spatial memory | Perform obstacle course (as demonstrated), reproduce on paper | ✓ | ✓ | |
| Perform the obstacle course and reproduce it on paper. | ✓ | ||||
| Play a short volleyball/ball passing game, then reproduce positions on paper. | ✓ | ||||
| Run and stop when estimating a 20 m distance. | ✓ | ✓ | |||
| Run freely 20″ in a 9 × 9 m without colliding with 12–15 peers. | ✓ | ✓ | |||
| Run freely 20″ in a 9 × 9 m without colliding with peers and avoiding nine sticks. | ✓ | ✓ | |||
| Run in line, maintain a 2 m distance, and stop at the signal. | ✓ | ✓ | ✓ | ||
| Throw a 3 kg weight and estimate the distance it travels. | ✓ | ||||
| Throw a 3 kg weight and estimate the distance it travels. | ✓ | ✓ | |||
| Walk in line, maintain a 2 m distance, and stop at the signal. | ✓ | ✓ | ✓ | ||
| Walk an unfamiliar city path (100 m, two right + 2 left turns), reproduce on paper. | ✓ | ✓ | |||
| Walk an unfamiliar city path (100 m, consisting of two right turns and two left turns), then return to the start. | ✓ |
Appendix B
| Session | Observation Date | Score Obtained | Max Possible Score | Fidelity % | Brief Notes |
|---|---|---|---|---|---|
| 2 | 15 June 2021 | 14.5 | 15 | 96.7% | Excellent adherence. |
| 5 | 6 July 2021 | 13.0 | 15 | 86.7% | The session was slightly rushed, with a shorter duration. |
| 8 | 27 July 2021 | 13.0 | 13 | 100% | No challenging behaviors observed (D1, D2 = N/A). |
| 11 | 17 August 2021 | 12.5 | 15 | 83.3% | The token economy was not systematically applied. |
| 14 | 7 September 2021 | 14.0 | 15 | 93.3% | Excellent adherence. |
| 18 | 5 October 2021 | 15.0 | 15 | 100% | Session implemented perfectly. |
| 21 | 26 October 2021 | 13.5 | 15 | 90.0% | Feedback was sometimes delayed. |
| 25 | 23 November 2021 | 12.0 | 15 | 80.0% | Minimum adherence; follow-up supervision recommended. |
| 28 | 14 December 2021 | 14.0 | 14 | 100% | Use of time-out not required (D2 = N/A). |
| Average | 92.2% | Overall Fidelity: HIGH |
| Component | Item | Response | Score | Notes/Details |
|---|---|---|---|---|
| A. Structural | ||||
| Session held in a public gym? | Yes | 1 | |
| Duration was ~2 h? | Yes | 1 | |
| Trainer + tech present? | Yes | 1 | |
| BCBA supervision conducted? | N/A | Not a supervision day. | |
| B. Procedural | ||||
| Preference assessment conducted? | Partially | 0.5 | Conducted informally. |
| Clear instructions provided? | Yes | 1 | |
| Exercise demonstrated? | Yes | 1 | |
| C. Behavioral | ||||
| Social praise used? | Yes | 1 | |
| Immediate feedback provided? | Yes | 1 | |
| Token economy implemented? | Yes | 1 | |
| D. Behavior Management | ||||
| Rules re-explained for minor issues? | Yes | 1 | |
| Time-out reserved for severe behavior? | Yes | 1 | |
| E. Data Collection | ||||
| Activities logged in the matrix? | Yes | 1 | |
| Parameters recorded? | Yes | 1 | |
References
- Almutairi, A. F., Gardner, G. E., & McCarthy, A. (2014). Practical guidance for the use of a pattern-matching technique in case-study research: A case presentation. Nursing & Health Sciences, 16(2), 239–244. [Google Scholar] [CrossRef]
- Bassette, L., Kulwicki, J., Dieringer, S. T., Zoder-Martell, K. A., & Heneisen, R. (2018). The use of a multicomponent behavioral intervention to promote physical activity in adolescents with autism spectrum disorders across inclusive community settings. Behavior Analysis in Practice, 11(4), 358–369. [Google Scholar] [CrossRef]
- Bourreau, Y., Roux, S., Gomot, M., Bonnet-Brilhault, F., & Barthélémy, C. (2009). Validation of the repetitive and restricted behaviour scale in autism spectrum disorders. European Child & Adolescent Psychiatry, 18(11), 675–682. [Google Scholar] [CrossRef]
- Bölte, S., Poustka, F., & Constantino, J. N. (2008). Assessing autistic traits: Cross-cultural validation of the social responsiveness scale (SRS). Autism Research, 1(6), 354–363. [Google Scholar] [CrossRef]
- Chan, A. S., Han, Y. M. Y., Sze, S. L., & Lau, E. M. C. (2015). Neuroenhancement of memory for children with autism by a mind–body exercise. Frontiers in Psychology, 6, 1893. [Google Scholar] [CrossRef]
- Ferris, E. L., Howard, A. R., Baker, E., Craig, A. R., Roane, H. S., & Sullivan, W. E. (2025). Chaining differential reinforcement of compliance and functional communication training to treat challenging behavior maintained by negative reinforcement. Behavioral Sciences, 15(7), 891. [Google Scholar] [CrossRef]
- Foti, F., Mazzone, L., Menghini, D., De Peppo, L., Federico, F., Postorino, V., & Vicari, S. (2014). Learning by observation in children with autism spectrum disorder. Psychological Medicine, 44(11), 2437–2447. [Google Scholar] [CrossRef]
- Hagopian, L. P., Long, E. S., & Rush, K. S. (2004). Preference assessment procedures for individuals with developmental disabilities. Behavior Modification, 28(5), 668–677. [Google Scholar] [CrossRef] [PubMed]
- Healy, S., Nacario, A., Braithwaite, R. E., & Hopper, C. (2018). The effect of physical activity interventions on youth with autism spectrum disorder: A meta-analysis. Autism Research, 11(6), 818–833. [Google Scholar] [CrossRef]
- Huang, J., Du, C., Liu, J., & Tan, G. (2020). Meta-analysis on intervention effects of physical activities on children and adolescents with autism. International Journal of Environmental Research and Public Health, 17(6), 1950. [Google Scholar] [CrossRef] [PubMed]
- Kazdin, A. E. (2021). Single-case experimental designs: Characteristics, changes, and challenges. Journal of the Experimental Analysis of Behavior, 115(1), 56–85. [Google Scholar] [CrossRef] [PubMed]
- Kou, R., Li, Z., Li, M., Zhou, R., Zhu, F., Ruan, W., & Zhang, J. (2024). Comparative effectiveness of physical exercise interventions on sociability and communication in children and adolescents with autism: A systematic review and network meta-analysis. BMC Psychology, 12, 712. [Google Scholar] [CrossRef] [PubMed]
- Lang, R., Koegel, L. K., Ashbaugh, K., Regester, A., Ence, W., & Smith, W. (2010). Physical exercise and individuals with autism spectrum disorders: A systematic review. Research in Autism Spectrum Disorders, 4(4), 565–576. [Google Scholar] [CrossRef]
- Ledford, J. R., & Wolery, M. (2013). Procedural fidelity: An analysis of measurement and reporting practices. Journal of Early Intervention, 35(2), 173–193. [Google Scholar] [CrossRef]
- Leif, E. S., Roscoe, E. M., Ahearn, W. H., Rogalski, J. P., & Morrison, H. (2020). Increasing item engagement and decreasing automatically reinforced problem behavior within a modified competing stimulus assessment. Journal of Applied Behavior Analysis, 53(3), 1638–1659. [Google Scholar] [CrossRef] [PubMed]
- Levinson, L. J., & Reid, G. (1993). The effects of exercise intensity on the stereotypic behaviors of individuals with autism. Adapted Physical Activity Quarterly, 10(3), 255–268. [Google Scholar] [CrossRef]
- Livingston, C. P., Schneider, D. E., Melanson, I. J., Martinez, S. E., Anderson, H., & Bryan, S. J. (2025). Variables influencing physical activity for children with autism: Environmental and behavioral factors. Behavioural Interventions, 40, e2067. [Google Scholar] [CrossRef]
- Mayes, S. D. (2018). Brief report: Checklist for autism spectrum disorder: Most discriminating items for diagnosing autism. Journal of Autism and Developmental Disorders, 48(3), 935–939. [Google Scholar] [CrossRef]
- Muharib, R., & Walker, V. L. (2024). Differential reinforcement in applied settings for individuals with autism: A systematic literature review. Advances in Neurodevelopmental Disorders, 8(3), 255–270. [Google Scholar] [CrossRef]
- Nabors, L., Overstreet, A., Carnahan, C., & Ayers, K. (2021). Evaluation of a pilot healthy eating and exercise program for young adults with autism spectrum disorder and intellectual disabilities. Advances in Neurodevelopmental Disorders, 5(4), 413–430. [Google Scholar] [CrossRef]
- Neely, L., Rispoli, M., Gerow, S., & Ninci, J. (2015). Effects of antecedent exercise on academic engagement and stereotypy during instruction. Behavior Modification, 39(1), 98–116. [Google Scholar] [CrossRef]
- Palumbo, C., Minghelli, V., & Pallonetto, L. (2021). The psychomotor practice at the kindergarten: The MOVIT tests as a tool of observation and design. Journal of Sports Science, 9, 1–8. [Google Scholar] [CrossRef]
- Pan, C. Y., Tsai, C. L., Chen, F. C., Chow, B. C., Chen, C. C., & Chu, C. H. (2021). Physical and sedentary activity patterns in youths with autism spectrum disorder. International Journal of Environmental Research and Public Health, 18(4), 1739. [Google Scholar] [CrossRef] [PubMed]
- Paolizzi, E., Perzolli, S., & Bentenuto, A. (2025). Mothers and fathers’ perception of social-responsive behaviors of autistic individuals. Research in Developmental Disabilities, 163, 105045. [Google Scholar] [CrossRef] [PubMed]
- Parker, R. I., Vannest, K. J., & Davis, J. L. (2011). Effect size in single-case research: A review of nine nonoverlap techniques. Behavior Modification, 35(4), 303–322. [Google Scholar] [CrossRef] [PubMed]
- Prupas, A., & Reid, G. (2001). Effects of exercise frequency on stereotypic behaviors of children with developmental disabilities. Education and Training in Mental Retardation and Developmental Disabilities, 36(2), 196–206. [Google Scholar]
- Reinders, N. J., Branco, A., Wright, K., Fletcher, P. C., & Bryden, P. J. (2019). Scoping review: Physical activity and social functioning in young people with autism spectrum disorder. Frontiers in Psychology, 10, 120. [Google Scholar] [CrossRef]
- Rivera, R. A., Robertson, M. C., & McCleery, J. P. (2025). Exercise interventions for autistic people: An integrative review of clinical trials. Current Psychiatry Reports, 27, 286–306. [Google Scholar] [CrossRef]
- Rosenthal-Malek, A., & Mitchell, S. (1997). Brief report: The effects of exercise on the self-stimulatory behaviors and positive responding of adolescents with autism. Journal of Autism and Developmental Disorders, 27(2), 193–202. [Google Scholar] [CrossRef]
- Salar, S., Jorgić, B. M., Olanescu, M., & Popa, I. D. (2024). Barriers to physical activity participation in children and adolescents with autism spectrum disorder. Healthcare, 12(23), 2420. [Google Scholar] [CrossRef]
- Schultheis, S. F., Boswell, B. B., & Decker, J. (2000). Successful physical activity programming for students with autism. Focus on Autism and Other Developmental Disabilities, 15(3), 159–162. [Google Scholar] [CrossRef]
- Sorensen, C., & Zarrett, N. (2014). Benefits of physical activity for adolescents with autism spectrum disorders: A comprehensive review. Review Journal of Autism and Developmental Disorders, 1(4), 344–353. [Google Scholar] [CrossRef]
- Sowa, M., & Meulenbroek, R. (2012). Effects of physical exercise on autism spectrum disorders: A meta-analysis. Research in Autism Spectrum Disorders, 6(1), 46–57. [Google Scholar] [CrossRef]
- Srinivasan, S. M., Pescatello, L. S., & Bhat, A. N. (2014). Current perspectives on physical activity and exercise recommendations for children and adolescents with autism spectrum disorders. Physical Therapy, 94(6), 875–889. [Google Scholar] [CrossRef]
- Suárez-Manzano, S., Ruiz-Ariza, A., de Loureiro, N. E. M., & Martínez-López, E. J. (2024). Effects of physical activity on cognition, behavior, and motor skills in youth with autism spectrum disorder: A systematic review of intervention studies. Behavioral Sciences, 14(4), 330. [Google Scholar] [CrossRef]
- Tierney, C. D., Mayes, S. D., Lohsandt, J. R., & Black, A. (2015). How valid is the checklist for autism spectrum disorder when a child has apraxia of speech? Journal of Developmental & Behavioral Pediatrics, 36(8), 569–574. [Google Scholar] [CrossRef]
- Toscano, C. V. A., Ferreira, J. P., Quinaud, R. T., Silva, K., Carvalho, H. M., & Gaspar, J. M. (2022). Exercise improves the social and behavioral skills of children and adolescents with autism spectrum disorders. Frontiers in Psychiatry, 13, 1027799. [Google Scholar] [CrossRef]
- Travers, B. G., Mason, A. H., Mrotek, L. A., Ellertson, A., Dean, D. C., Engel, C., & McLaughlin, K. (2018). Biofeedback-based videogame balance training in autism. Journal of Autism and Developmental Disorders, 48(1), 163–175. [Google Scholar] [CrossRef]
- Tse, C., Pang, C. L., & Lee, P. H. (2018). Choosing an appropriate physical exercise to reduce stereotypic behavior in children with autism spectrum disorders: A non-randomized crossover study. Journal of Autism and Developmental Disorders, 48(5), 1666–1672. [Google Scholar] [CrossRef] [PubMed]
- Valenti, M., Pino, M. C., Le Donne, I., Vagnetti, R., Tiberti, S., Attanasio, M., & Mazza, M. (2022). Adaptive response of Italian young adults with autism to the COVID-19 pandemic: A longitudinal study. Research in Developmental Disabilities, 131, 104333. [Google Scholar] [CrossRef]
- Wang, S., Chen, D., Yoon, I., Klich, S., & Chen, A. (2022). Bibliometric analysis of research trends of physical activity intervention for autism spectrum disorders. Frontiers in Human Neuroscience, 16, 926346. [Google Scholar] [CrossRef]
- Watters, R. G., & Watters, W. E. (1980). Decreasing self-stimulatory behavior with physical exercise in a group of autistic boys. Journal of Autism and Developmental Disorders, 10(4), 379–387. [Google Scholar] [CrossRef]
- Wong, T., Falcomata, T. S., & Barnett, M. (2023). The collateral effects of antecedent exercise on stereotypy and other nonstereotypic behaviors exhibited by individuals with autism spectrum disorder: A systematic review. Behavior Analysis in Practice, 16(2), 407–420. [Google Scholar] [CrossRef] [PubMed]
- Wood, C. L., Kisinger, K. W., Brosh, C. R., Fisher, L. B., & Muharib, R. (2018). Stopping behavior before it starts: Antecedent interventions for challenging behavior. Teaching Exceptional Children, 50(6), 356–363. [Google Scholar] [CrossRef]
- Xing, Y., Huang, S., Zhao, Y., & Wu, X. (2025). Effects of group sports activities on physical activity and social interaction abilities of children with autism spectrum disorders. Frontiers in Psychology, 15, 1496660. [Google Scholar] [CrossRef] [PubMed]
- Xing, Y., & Wu, X. (2025). Effects of motor skills and physical activity interventions on motor development in children with autism spectrum disorder: A systematic review. Healthcare, 13(5), 489. [Google Scholar] [CrossRef] [PubMed]
| Age | CASD | Social Responsiveness Scales | Vineland | Repetitive and Restricted Behavior | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subjects | Year | Severity | Awareness | Cognition | Communication | Motivation | Communication | Daily Living | Socialization | Sensory Motor | Reaction to Change | Restricted Behaviors | Modulation Insufficiency |
| Manuel | 18 | 15 | 74 | 73 | 79 | 35 | 13 * | 15 * | 12 * | 9 | 13 | 15 | 13 |
| Dean | 17 | 20 | 77 | 72 | 90 | 68 | 11 * | 10 * | 6 * | 10 | 4 | 7 | 3 |
| Gene | 17 | 18 | 65 | 71 | 79 | 64 | 12 * | 15 * | 16 * | 9 | 10 | 9 | 17 |
| RRBS (T0) | SRS-2 (T0) | VABS (T0) | Mean Motor Improvement | Variability of Improvement | |
|---|---|---|---|---|---|
| Participant | Reaction to Change | Social Motivation (T0) | Socialization (T0) | (Mean Δ%) | (SD of Δ%) |
| Manuel | 13 (High) | 35 (Typical) | 12 | 36.5% | 19.1% (High) |
| Dean | 4 (Low) | 68 (Impaired) | 6 (Low) | 48.0% | 7.1% (Low) |
| Gene | 10 (Moderate) | 64 (Impaired) | 16 (High) | 31.5% | 16.3% (High) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Esposito, M.; Caputi, M.; Fadda, R.; Ricciardi, O.; Pagano, E.; Bove, D.; Mazza, M.; Valenti, M. Group Physical Activity and Behavioral Practices in Adolescents with Autism: A Case Series on Integrated Educational Interventions. Educ. Sci. 2025, 15, 1491. https://doi.org/10.3390/educsci15111491
Esposito M, Caputi M, Fadda R, Ricciardi O, Pagano E, Bove D, Mazza M, Valenti M. Group Physical Activity and Behavioral Practices in Adolescents with Autism: A Case Series on Integrated Educational Interventions. Education Sciences. 2025; 15(11):1491. https://doi.org/10.3390/educsci15111491
Chicago/Turabian StyleEsposito, Marco, Marcella Caputi, Roberta Fadda, Orlando Ricciardi, Elisa Pagano, Domenico Bove, Monica Mazza, and Marco Valenti. 2025. "Group Physical Activity and Behavioral Practices in Adolescents with Autism: A Case Series on Integrated Educational Interventions" Education Sciences 15, no. 11: 1491. https://doi.org/10.3390/educsci15111491
APA StyleEsposito, M., Caputi, M., Fadda, R., Ricciardi, O., Pagano, E., Bove, D., Mazza, M., & Valenti, M. (2025). Group Physical Activity and Behavioral Practices in Adolescents with Autism: A Case Series on Integrated Educational Interventions. Education Sciences, 15(11), 1491. https://doi.org/10.3390/educsci15111491






