Abstract
This study explores the profound impacts of the COVID-19 pandemic on higher education, focusing on shifts in learning experiences and students’ intentions to utilize mental health services post-pandemic. Utilizing Andersen’s Behavioral Model of Health Services Use, this study assesses perceptions from a stratified random sample of college students on post-pandemic learning experiences and mental health service utilization intentions. Findings reveal a positive reception to university initiatives and a preference for ongoing virtual classes. There is an evident increase in, and varying intentions for, using mental health services, shaped by demographics, employment, and prior service utilization. Younger and female students showed an increased propensity to seek such services. This research underscores the urgent need for universities to bolster support for mental health and create awareness, alongside accommodating diverse learning preferences in transitioning back to traditional learning post-pandemic.
1. Introduction
The global COVID-19 pandemic has profoundly impacted society, including higher education institutions [1,2]. In response to the pandemic, colleges and universities worldwide were forced to adapt rapidly and implement measures to ensure the safety of their students, faculty, and staff [3,4]. Campus closures and the transition to remote learning became the new norm, significantly disrupting the traditional college experience. In addition, the pandemic has had a significant impact on college students’ mental health, necessitating the provision of adequate mental health services during campus reopening [5,6,7]. However, as the world recovers, there is relatively little research to understand the perspectives and experiences of students during this transitional phase and their utilization of mental health services to effectively support their well-being and ensure a successful return to campus life. This research examines the multifaceted aspects of students’ perspectives and experiences as they navigate the post-pandemic campus environment. The research seeks to explore college students’ perceptions on the impact of the pandemic on several topics such as mental health services utilization, online learning, virtual platforms, social connectedness, and teaching presence in fostering a sense of belonging.
1.1. Impact of COVID-19 in Higher Education and the Implications of the Transition to a New Normal
The onset of the COVID-19 pandemic mandated adaptations that disrupted education at all levels and uniquely shaped the academic experience of post-secondary students. Under the guidance of the CDC, colleges and universities across the country implemented several measures to manage the impact of COVID-19 on institutional operations and reduce disruptions to student learning including offering distance learning, adjusting the academic calendar, limiting student housing, modifying the operations of on-campus facilities and common areas, and enforcing mask-wearing policies [8]. The required adaptations and transitions drastically shaped the higher education experience for all students. Previous studies have indicated that the transition to remote learning had a profound negative impact on students academically. One study comparing students’ perceptions of in-person versus remote learning found that although 90% of students felt challenged by their in-person coursework and 92% were satisfied with it, less than half felt challenged by their remote coursework and only 28% reported satisfaction with it [9]. College students also associated the transition to remote learning with decreased levels of motivation and reduced engagement in their studies [10,11,12].
Apart from the impact of the transition to online instruction on academic performance, campus closures reduced social interactions between students and their peers, instructors, and mentors. Students reported that the remote classes left them feeling distant from their instructors who provided less feedback after the transition [11,13]. Many students expressed missing being able to connect with others socially and participate in on-campus events [11]. As a result of off-campus relocation due to school closures, students reported higher levels of COVID-19 related grief and worry, as well as an increase in symptoms of depression, anxiety, and PTSD [14]. Students faced unique challenges as they navigated the transition to remote learning, which had academic and personal implications. Given that campuses have reopened and have mostly resumed normal operations, future research may aim to determine if these disruptions to education have resulted in any long-term impact.
1.2. Mental Health Services Utilization among College Students following COVID-19
While the extant literature has established the profound mental health impact of COVID-19 on college and university students, fewer studies have examined the mental health service utilization patterns of this population within the context of the pandemic. Furthermore, the few studies that have examined mental health service utilization in this group were primarily conducted at the onset of the pandemic as opposed to during the reopening and post-pandemic era.
Studies carried out at the onset of the pandemic revealed a significant gap between need and mental health service utilization among college and university students [15,16]. For example, a study conducted among undergraduate students in Kentucky found that even among students demonstrating symptoms of moderate to severe levels of stress, depression, or anxiety, over 60% never used mental health services either on-campus or off-campus at the start of the pandemic [15]. Another study conducted among Texas university students in the summer of 2020 found similar results, with only 6.71% reporting using in-person mental health services and 18.02% reporting using virtual mental health services within the previous three-month period [16]. In the same study, almost 20% of respondents indicated that they avoided seeking mental health services as a result of the pandemic, and this was more likely among students who either believed school-sponsored mental health services were inadequate or were unaware of the availability of services [16].
Although mental health services were underutilized at the pandemic’s start, it is unclear whether these trends continued during campus reopening and the transition to the new normal. One study conducted among California nursing students a year into the pandemic indicated that about 85% of students with high levels of depression, anxiety, and traumatic stress used either on-campus or off-campus mental health services [17]. While these findings suggest an improvement in the mental health service utilization patterns of college students following the height of the pandemic, further research is needed to determine if these findings are upheld among students in other university settings.
1.3. Student Experiences and Perspectives during the Post-COVID Campus Re-Openings
Although many studies have explored the academic and psychological impact of school closures and the transition to distance learning on students, the student experience after resuming in-person classes is less understood. Some institutions resumed in-person instruction in the Fall of 2020, and studies conducted during that time demonstrated students’ concern about returning to campus. For example, a study conducted among students who were at least partially attending in-person classes at a midwestern US university demonstrated that the mental health impact of the pandemic persisted into the Fall 2020 semester, with almost 60% of students reporting moderate to severe symptoms of depression and over 40% of students reporting moderate to severe symptoms of either stress or anxiety [18]. Research has shown that students were concerned about the school’s ability to implement adequate protection measures, the risk of exposure to COVID-19, and a reduced quality of education upon returning to campus [18,19]. Seemingly, only one study has examined US college students’ mental health and academic experience beyond the first year of the pandemic [20]. In this study, researchers found that although students’ levels of fear had decreased since the onset of the pandemic, they had not returned to pre-pandemic levels [20]. Furthermore, students reported lower levels of happiness and severe impacts to their academic performance two years after the declaration of the pandemic [20]. The results of these studies highlight both the immediate and longer-term impacts of COVID-19 on the student experience.
1.4. Research Objectives
The purpose of this analysis is to explore college students’ learning experiences, both undergraduate and graduate, in the aftermath of COVID-19 and identify the factors influencing their intention to utilize mental health services as campuses reopen post-pandemic. Using data collected from a sample of college students, we applied Andersen’s Behavioral Model of Health Services Use as a conceptual framework to understand students ‘educational experiences and intentions regarding mental health service utilization in the post-pandemic era.
1.5. Theoretical Framework
Andersen’s Behavioral Model of Health Services Use (ABMHSU) was used as a conceptual framework to understand the intricacies of mental health services utilization among college students in the post-pandemic era. The ABMHSU, a socio-behavioral model, postulates that utilizing healthcare services hinges on three critical fundamental dynamics: predisposing factors, enabling factors, and need [21,22]. The predisposing factors represent characteristics of the individual that exist prior to the need for services. The enabling factors refer to resources, services, structural factors, or opportunities that facilitate or hinder the utilization of health services, and the need factors reflect the individual’s perceived need or professionally evaluated need for health services or experiences related to health service utilization. This framework allows for a nuanced analysis of how individual characteristics, systemic enablers, and perceived needs interact to influence students’ engagement with mental health services. By adopting the ABMHSU, the study aims to dissect and understand the complex dynamics of mental health service utilization among students in a post-pandemic learning environment.
2. Methods and Materials
2.1. Study Design and Data Collection
The study employed a cross-sectional research design, and data collection occurred over four weeks, spanning from January to February 2022. The primary data collection instrument was a 22-question survey. This survey covered demographic characteristics (e.g., age, gender, ethnicity, academic class standing), self-reported utilization of mental health services at specific time points, and a question matrix to assess students’ experiences and perceptions regarding campus reopening events and policies.
2.2. Study Participants and Procedure
The study, conducted at a large southeastern university in Virginia, was approved by the university’s Institutional Review Board (IRB) in accordance with federal regulations. Undergraduate and graduate students from the university were recruited through a representative sample provided by the university’s Office of Institutional Effectiveness and Assessment (IEA). To ensure a diverse and representative sample, a stratified random sampling method was used to reflect the university’s demographic composition. This method accounted for the gender distribution (43% male, 57% female) and academic composition (80% undergraduates, 20% graduate students) of the university’s student population. The IEA identified and invited 1025 eligible students, who were at least 18 years old and actively enrolled in either undergraduate or graduate programs. The sample size was chosen to achieve a maximum margin of error of ±3% at a 95% confidence level, based on the known total student population in Spring 2022. An anonymous survey link was generated through the QualtricsTM platform and disseminated to potential respondents via the Qualtrics Mailer system. Out of the initial pool of 1025 students, 257 actively responded to the survey invitation. However, 7 students chose not to consent to participate, while 250 provided their consent, resulting in a response rate of 24.4%. Within this group of participants, there were 14 instances where the survey was either left entirely blank or had more than 95% of the data missing. Thus, these responses were excluded from the analysis, yielding a final sample size of 236 students.
3. Measures
In line with ABMHSU, the study encompassed variables and measures to investigate the intricate relationship between diverse factors and mental health services (MHSs) utilization. Within this framework, we examined the following:
Predisposing Factors: These represent the individual characteristics that exist before the need for services. In this analysis, we explored the influence of age to assess how different age groups are associated with the intended utilization of MHSs following the COVID-19 pandemic. We also investigated the impact of gender, as well as the effect of race and ethnicity, on the intention to access MHSs in the post-pandemic context.
Enabling Factors: These factors encompass a range of elements, including resources, services, structural factors, and opportunities that can either facilitate or hinder the utilization of health services. Within this category, we specifically investigated how students’ enrollment status (full-time vs. part-time) influences their access to and utilization of MHSs. We also explored the role of living arrangements, such as living alone or with roommates, in enabling or hindering MHSs utilization. Furthermore, we examined how employment status (employed or not employed) shapes individuals’ ability to access and benefit from MHSs. Additionally, we considered the impact of academic class standing (undergraduate or graduate) and the availability of university support services and resources to determine whether they influence access to and initiation of MHSs. Finally, the influence of one’s academic discipline area, categorized as “hard” or “soft” based on Biglan’s taxonomy classification system, was considered to explore how it might facilitate or hinder the utilization of MHSs.
Need factors: These include the individual’s perceived need or professionally evaluated need for health services and their experiences related to health service utilization. We evaluated whether students’ regular use of MHSs before March 2020 and their use of MHSs during the pandemic are associated with their perceived need for initiating MHSs following the post-COVID-19. We also investigated whether students’ views on in-person instruction’s role in enhancing social connections and access to professors affect their perceived MHS need. Lastly, we explored if preferences for virtual classes during reopening relate to perceived MHS need. These factors collectively illuminate college students’ nuanced MHSs utilization, considering prior experiences and current perceptions in the evolving post-pandemic landscape.
Outcome Variable: Intention to use Mental Health Services (MHSs) post-pandemic (Yes/No). This variable gauges students’ contemplation of future engagement with mental health services. It serves as the focal outcome of interest, enabling us to investigate the influence of predisposing and enabling factors, in conjunction with the perceived need for mental health services, on students’ actual intention to seek MHSs in the aftermath of the COVID-19 pandemic.
Statistical Analysis
Descriptive and inferential statistics methods, tables, and graphs were used to summarize the data. All variables under consideration were categorical and are accordingly presented as frequencies and proportions. Initial bivariate analyses using chi-square and Fisher’s exact test were performed to assess associations between intention to use MHSs post-pandemic and various sociodemographic characteristics, along with other self-reported variables.
A block entry (hierarchical) logistic regression was used to investigate the association between predisposing, enabling, and need factors based on ABMHSU and the intention to use MHSs post-pandemic. The model was executed in three steps using the PROC LOGISTIC procedure in SAS, where each block of variables was entered sequentially to elucidate their contribution to the model. Model 1 was confined to predisposing factors like age, gender, race, and ethnicity. Subsequently, Model 2 was developed by sequentially adding enabling factors to Model 1 variables. Need factors were then incorporated into Model 2 to create Model 3.
The overall significance of each model was examined using the likelihood ratio test, and the individual contribution and significance of each variable was evaluated using Wald chi-square statistics. Additionally, the adequacy of the models and predictive accuracy and performance were rigorously evaluated using metrics like the -2 log-likelihood, Akaike information criterion (AIC), the Hosmer-Lemeshow goodness-of-fit test, and the area under the receiver operating characteristic (ROC) curve among other relevant performance metrics.
Finally, a comprehensive model integrating all significant variables from preliminary Models 1, 2, and 3 was created. This model subsequently underwent a stepwise selection procedure—encompassing both forward selection and backward elimination—to refine and determine the most relevant variables for predicting the intention to utilize MHSs post-pandemic. The Wald chi-square test and the odds ratio with a 95% confidence interval were computed for each predictor to evaluate the significance and the effect size, respectively.
To assess the robustness of our final logistic regression model, sensitivity analyses were conducted by modifying the predictor values to represent different plausible scenarios and studying the resultant variations in the outcome. All analyses were performed using SAS 9.3 and the statistical significance was set at p < 0.05.
4. Results
The overall sample data predominantly consists of younger individuals, with 54.66% falling within the 18–24 age group (Table 1). The gender demographics reveal a predominance of female representation at 69.07%, non-Hispanic (89.32%), and Caucasian (56.36%). The employment status data indicate that 70.76% of the students were employed.

Table 1.
Respondent demographics characteristics by intention to use MHSs Post-pandemic.
The perception of university support during the pandemic is generally positive, with 58.87% of students expressing satisfaction with the university’s initiatives. In focusing on the need factors in the overall sample, before the pandemic, only a tiny minority, 13.98% of students, regularly used mental health services. However, during the pandemic, there was a notable increase, with 22.46% of students utilizing mental health services (MHSs), emphasizing the heightened need and demand for mental health support in these unprecedented times. Regarding social connectedness—a pivotal aspect considering that in-person instruction can alleviate stress through increased interaction—the data exhibit diverse responses. A significant proportion neither agree nor disagree (32.88%), showcasing a neutral stance, potentially indicating varied experiences. However, 40.64% of students agree to varying extents that there is an improvement in social connectedness. The accessibility to professors reveals that a majority felt positive with 44.8% agreeing that in-person instruction does enhance accessibility. The data indicate diverse perspectives on preferences for virtual classes. A significant 58.37% agree with preference to attend virtual classes post-pandemic, signaling a discernible inclination toward this learning mode. However, 28.51% strongly or somewhat disagree with virtual learning, pointing to a preference for traditional learning environments.
The bivariate analysis (Table 1) revealed intuitive patterns and associations related to the intention to utilize MHSs post-pandemic. Notably, 39.32% (n = 92) of respondents anticipate a need for MHSs post-pandemic, while 60.68% (n = 142), do not foresee utilizing such services. Several key findings emerged when examining respondents’ demographic characteristics by intention to use MHSs post-pandemic. Predisposing factors revealed a significant relationship between age and intention to use MHSs post-pandemic (p = 0.0303), with a higher inclination observed in the 18–24 age group. Gender also displayed a distinct relationship with intention to use MHSs (p = 0.0029), with females showing a notably higher propensity (80.43%) compared to males (16.30%). However, race and ethnicity did not show any significant association with intention to use MHSs post-pandemic. Among enabling factors, employment status clearly connected to the intention to use MHSs (p = 0.0121), with employed respondents indicating a higher intention. Though not statistically significant, there was an observable trend suggesting that positive university support might influence the intention to use MHSs post-pandemic (p = 0.0787).
Regarding need factors, respondents who regularly used mental health services before the pandemic and those who utilized MHSs during the pandemic showed a pronounced likelihood to seek such services post-pandemic, with p-values of 0.0016 and <0.0001, respectively. Conversely, factors like academic class standing, living arrangement, social connectedness, accessibility to professors, and virtual class preferences did not reveal any clear associations with the intention to use MHSs post-pandemic. These findings underscore the crucial role of individual demographic characteristics, previous experiences with mental health services, and certain enabling factors in determining the likelihood of utilizing mental health services in the post-pandemic period.
The data in Figure 1 illustrate the varied opinions of students’ perspectives and experiences with online courses. We observed that the majority, or 57.26%, of students had not encountered online classes before the pandemic. Approximately 24.62% of students prefer online courses over traditional in-person ones. Conversely, a notable 20.42% of students identify no advantages to online courses, hinting at a potentially stronger inclination towards in-person instructional methodologies. Further, 27.63% of respondents perceived their learning outcomes are unaffected by the mode of delivery—whether it be online or in-person. Finally, 17.12% of the participants expressed a desire for an increased offering of online courses. For students who feel they learn a comparable amount in both environments, around 13.07% had experienced online classes compared to 14.89% without such experience. In the segment perceiving no advantages to online learning, 6.38% had previous experience, contrasting with 13.98% who did not. Finally, among those desiring more online courses, about 9.12% had pre-pandemic online class experience, while 7.90% did not.
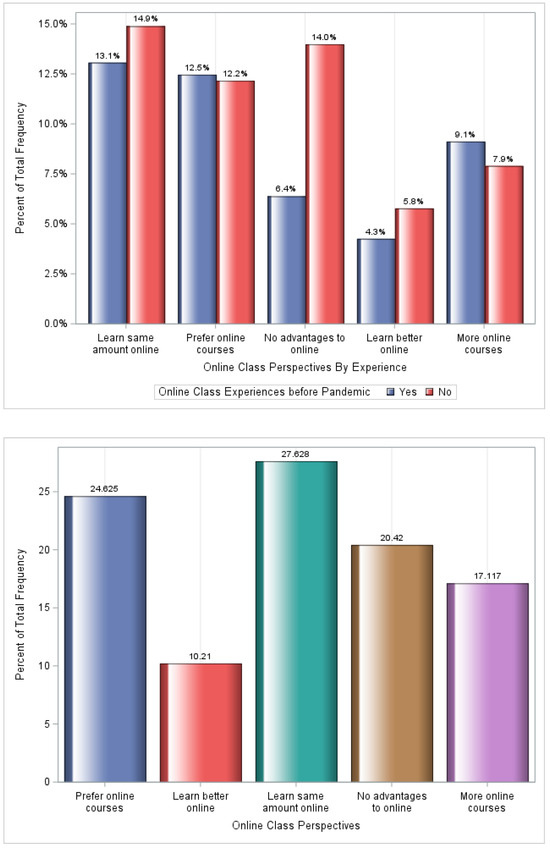
Figure 1.
Online class perspectives and experience.
In evaluating the association between predisposing, enabling, and need factors with the intention to use mental health services (MHSs) post-pandemic, in line with Andersen’s Behavioral Model, three logistic regression models were employed (Table 2). Predisposing factors like age demonstrated a significant association with the intention to use MHSs in Model 1 (p = 0.0263). However, the prominence of this association appears to diminish in Models 2 and 3. Gender maintained a significant association with the outcome across all three models, with Model 1 showing the strongest association (p = 0.0007). The introduction of enabling factors in Model 2, particularly living arrangement (p = 0.0489) and employment status (p = 0.0116), illustrated significant associations with the intention to use MHSs, refining the understanding achieved from predisposing factors alone. Furthermore, the integration of need factors in Model 3 emphasized the influence of utilizing MHSs during the pandemic (p = 0.0091) in determining post-pandemic intentions to use MHSs, offering a more comprehensive viewpoint. Notably, the progressive enhancement in model fit statistics from Model 1 to Model 3 accentuates the incremental explanatory power gained by incorporating enabling and need factors, yielding a nuanced understanding of the determinants of post-pandemic MHS utilization intentions.

Table 2.
Logistic regression analyses of predisposing, enabling, and need factors impacting intention to utilize MHSs post-pandemic.
The final model (Table 3), developed through the stepwise elimination procedure, retained employment status (p = 0.0250) and the use of MHSs during the pandemic (p <0.0001) as pivotal predictors for the intention to use MHSs post-pandemic. More specifically, the odds of intending to use MHSs are 2.12 times higher among employed students than unemployed, and they are about 5.29 times higher for those who utilized MHSs during the pandemic than those who did not. The gender variable showed a moderate association in the comprehensive model (p = 0.0434), but that weakened in the final model. Although theoretically essential, the remaining variables did not demonstrate statistically significant evidence of an association in the models, emphasizing the importance of empirical validation in model development.

Table 3.
Odds ratio and 95% confidence interval from the comprehensive and final models.
Sensitivity Analyses
The sensitivity analyses revealed that the associations identified in the primary analysis between employment status, intention to utilize mental health services post-pandemic, and the outcome remained robust. Specifically, the modified employment status exhibited a significant association with the outcome (Wald chi-square = 5.0234, p = 0.0250), with the odds of the outcome occurring being 2.11 times more for employed individuals compared to unemployed individuals (95% CI: 1.098, 4.056). Similarly, the modified intention to utilize MHSs post-pandemic remained highly significantly associated with the outcome (Wald chi-square = 22.5462, p < 0.0001), with the odds being 5.29 times more when the intention is “Yes” compared to “No” (95% CI: 2.658, 10.507). These results signify the robustness of the final model to plausible alterations in the predictor values, reinforcing the validity of the initial findings.
5. Discussion
The current study assessed college students’ learning experiences and examined factors associated with their intentions to use mental health services as they navigate the “new normal” after the height of the COVID-19 pandemic. In this study, most students endorsed positive perceptions of university initiatives during the pandemic. In addition, while online classes were a novel learning format for many students, most expressed interest in continuing virtual classes post-pandemic. With regard to the intention to utilize mental health services, study findings suggest that the utilization of mental health services increased after the onset of the COVID-19 pandemic; however, the intention to utilize MHSs in the post-pandemic era varied by demographic characteristics, employment status, and past use of mental health services.
The findings of this study show that intention to utilize MHSs post-pandemic differed by age and sex. Younger students, specifically those in the 18–24 age group, were more inclined to use MHSs post-pandemic. This trend could be reflective of the higher rates of mental health concerns and increased awareness [23] of mental health in younger generations. A recent study examined generational differences in mental health status at the start of the COVID-19 pandemic and found that in comparison to individuals in the Gen X or Baby Boomer generations, the prevalence of both major depressive disorder and generalized anxiety disorder was higher among Gen Z individuals and Millennials [24]. Additionally, female students showed a higher propensity to use MHSs post-COVID-19 than males, aligning with previous studies indicating that female college students often report higher professional mental health treatment access. In contrast, male students exhibit lesser mental health help-seeking behaviors [25,26]. Attitude in seeking help [27,28], lower mental health literacy, and more adverse perceptions of mental health among male students may contribute to this discrepancy [26].
Employment status, specifically employed students, is a pivotal factor affecting intention to seek MHSs post-pandemic. This finding may indicate that employment may impact students’mental health due to work-related stress or difficulties balancing work and academic responsibilities [29,30]. Also, this result could indicate that students who work have increased financial and social capital to seek MHSs [31,32].
The current study’s findings, showing a surge in MHSs utilization by college students during the COVID-19 pandemic, resonate with existing research depicting increased stress, depression, anxiety, and suicidal ideation in this demographic during this period [33,34,35,36], with additional evidence indicating an overall increase in mental health treatment sought by students in this timeframe [17,37]. Importantly, those who accessed MHSs during the pandemic are particularly more likely to seek such services post-pandemic, underscoring the escalating global need for mental health support [38].
Interestingly, our final model conflicts with previous research among the predisposing factors of race and ethnicity and intention to seek MHSs. Previous research states that racial and ethnic minorities have greater underutilization MHS rates when compared to non-Hispanic Whites [37,39,40]. Research indicates that the differences in intention to utilize MHSs is due to cultural mistrust created by fear, racism, and discrimination [41]. These findings suggest that perhaps the current on-campus MHSs are diverse and actively work towards training non-discriminatory providers.
Though not statistically significant, a visible trend suggests the importance of university support in influencing students’ intentions to use MHSs post-pandemic, aligning with a 2016 study, conducted across 39 college campuses in California, showing higher rates of MHS utilization on campuses perceived as supportive of mental health concerns [42]. This emphasizes the need for universities to foster awareness and provide robust mental health resources, addressing findings of substantial unawareness and lack of information among students [43,44].
Finally, the present study reveals divergent student perspectives on post-pandemic online learning, supporting prior research that outlines challenges like reduced interaction, increased burnout, and decreased retention of material [45,46], while highlighting benefits like greater flexibility and enriched learning experiences through technology [45,47,48]. These findings highlight the need to accommodate diverse learning preferences as institutions transition back to in-person learning.
Limitations and Strengths
Although our study contributed novel findings to the existing literature on student experiences during and after the COVID-19 pandemic, a few limitations and strengths should be considered. First, there is an overrepresentation of female participants in the study, with 69% being female compared to the university’s female population of 57%. This could potentially introduce bias, limiting the generalizability of the findings to the broader student population. The overrepresentation of females within the sample may be due to males’ unwillingness to disclose seeking MHSs due to stigma and social norms associated with the behavior, as help-seeking is generally considered a feminine behavior [49,50]. Furthermore, studies have shown that females are more likely than males to participate in surveys [51,52]. However, using a stratified random sample is a significant strength, promoting a more representative depiction of the enrolled students, enhancing the reliability of the findings. Second, using a cross-sectional design limits the ability to infer causation and analyze longitudinal effects over time. However, our study focused on the transition to the new normal and was conducted later in the pandemic, a unique timepoint compared to the many studies conducted at the pandemic’s onset. Additionally, the response rate and sample size were adequate and comparable to other studies examining the mental health impact of the pandemic on the experiences of US college and university students [33,34,53]. Third, the lack of a validated mental health status assessment tool, is a notable limitation, restricting a deeper understanding of the actual mental health conditions of the participants. Despite this, the robustness of the statistical methods, including sensitivity analyses, and the study’s structured and comprehensive application of ABMHSU serve as a foundational strength, allowing for an organized exploration of the variables in play, which augments the weight of the study’s conclusions. The study’s methodological integration supports its contributions to understanding post-pandemic student experiences and mental health needs.
6. Conclusions
This study has provided critical awareness of college students’ learning experiences and their intentions to utilize mental health services in the evolving post-pandemic environment. This study emphasizes the necessity for higher education institutions to be agile and responsive to students’ diverse needs and preferences in the post-pandemic landscape. The findings emphasize the need for a sustained and adaptive approach to online learning, acknowledging its challenges and benefits, and necessitate creating a flexible and inclusive learning environment that caters to varied learning preferences and needs. Institutions should bolster their support for mental health, recognizing the increased inclination, especially among younger and female students, to utilize mental health services post-pandemic. Proactive efforts should be made to mitigate the barriers to mental health help-seeking, particularly among male students, through initiatives aimed at enhancing mental health literacy and altering perceptions about mental health. The role of employment status in influencing mental health service utilization should be considered, and appropriate support should be extended to employed students grappling with work-related stress and academic responsibilities.
Further, universities should harness the visibility and impact of their support to foster a conducive environment that encourages mental health help-seeking, addresses information gaps, and raises awareness about available mental health resources. The highlighted trends and varied intentions to use mental health services post-pandemic reflect the pressing need for a holistic approach to mental health support, underscored by a supportive and informed university environment. These recommendations aim to facilitate a smooth and enriched transition back to in-person learning, ensuring students’ well-being and academic success in the evolving educational landscape.
Author Contributions
Conceptualization, H.G.; methodology, H.G.; software, H.G. and C.T.; validation, H.G., A.D. and C.T.; formal analysis, H.G.; investigation, H.G.; data curation, H.G.; writing—original draft preparation, H.G.; writing—review and editing, H.G., A.D. and C.T.; visualization, H.G.; supervision, H.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Human Subjects Review Committee of the Old Dominion University (protocol code [1726110-2] and approved on 6 January 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available from the corresponding author upon reasonable request.
Acknowledgments
We express our sincere gratitude to the students, Hira Nadeem, Priyanka Patel, and Brenda Berumen-Flucker, who generously contributed their unique perspectives in designing the survey questions. Their invaluable input was instrumental in enhancing the relevance and comprehensiveness of our research instrument, ensuring it accurately captured the diverse experiences and views of our study participants.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Schleicher, A. The Impact of COVID-19 on Education: Insights from “Education at a Glance 2020”; OECD Publishing: Paris, France, 2020. [Google Scholar]
- Aristovnik, A.; Keržič, D.; Ravšelj, D.; Tomaževič, N.; Umek, L. Impacts of the COVID-19 pandemic on life of higher education students: A global perspective. Sustainability 2020, 12, 8438. [Google Scholar] [CrossRef]
- Turnbull, D.; Chugh, R.; Luck, J. Transitioning to E-Learning during the COVID-19 pandemic: How have Higher Education Institutions responded to the challenge? Educ. Inf. Technol. 2021, 26, 6401–6419. [Google Scholar] [CrossRef] [PubMed]
- Sharaievska, I.; McAnirlin, O.; Browning, M.H.; Larson, L.R.; Mullenbach, L.; Rigolon, A.; D’Antonio, A.; Cloutier, S.; Thomsen, J.; Metcalf, E.C.; et al. “Messy transitions”: Students’ perspectives on the impacts of the COVID-19 pandemic on higher education. High. Educ. 2022; ahead of print. [Google Scholar]
- Roche, A.I.; Holdefer, P.J.; Thomas, E.B.K. College student mental health: Understanding changes in psychological symptoms in the context of the COVID-19 pandemic in the United States. Curr. Psychol. 2022; ahead of print. [Google Scholar]
- Wood, C.I.; Yu, Z.; Sealy, D.-A.; Moss, I.; Zigbuo-Wenzler, E.; McFadden, C.; Landi, D.; Brace, A.M. Mental health impacts of the COVID-19 pandemic on college students. J. Am. Coll. Health, 2022; ahead of print. [Google Scholar]
- Stamatis, C.A.; Broos, H.C.; Hudiburgh, S.E.; Dale, S.K.; Timpano, K.R. A longitudinal investigation of COVID-19 pandemic experiences and mental health among university students. Br. J. Clin. Psychol. 2022, 61, 385–404. [Google Scholar] [CrossRef] [PubMed]
- Moreland, S.; Zviedrite, N.; Ahmed, F.; Uzicanin, A. COVID-19 prevention at institutions of higher education, United States, 2020–2021: Implementation of nonpharmaceutical interventions. BMC Public Health 2023, 23, 164. [Google Scholar] [CrossRef]
- Parker, S.W.; Hansen, M.A.; Bernadowski, C. COVID-19 campus closures in the United States: American student perceptions of forced transition to remote learning. Soc. Sci. 2021, 10, 62. [Google Scholar] [CrossRef]
- Ives, B. University students experience the COVID-19 induced shift to remote instruction. Int. J. Educ. Technol. High. Educ. 2021, 18, 59. [Google Scholar] [CrossRef] [PubMed]
- Mucci-Ferris, M.; Grabsch, D.K.; Bobo, A. Positives, negatives, and opportunities arising in the undergraduate experience during the COVID-19 pandemic. J. Coll. Stud. Dev. 2021, 62, 203–218. [Google Scholar] [CrossRef]
- Prokes, C.; Housel, J. Community college student perceptions of remote learning shifts due to COVID-19. TechTrends 2021, 65, 576–588. [Google Scholar] [CrossRef]
- Means, B.; Neisler, J. Teaching and learning in the time of COVID: The student perspective. Online Learn. 2021, 25, 8–27. [Google Scholar] [CrossRef]
- Conrad, R.C.; Koire, A.; Pinder-Amaker, S.; Liu, C.H. College student mental health risks during the COVID-19 pandemic: Implications of campus relocation. J. Psychiatr. Res. 2021, 136, 117–126. [Google Scholar] [CrossRef]
- Lee, J.; Jeong, H.J.; Kim, S. Stress, anxiety, and depression among undergraduate students during the COVID-19 pandemic and their use of mental health services. Innov. High. Educ. 2021, 46, 519–538. [Google Scholar] [CrossRef]
- Villatoro, A.P.; Errisuriz, V.L.; DuPont-Reyes, M.J. Mental Health Needs and Services Utilization among Undergraduate and Graduate Students in Texas during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 6066. [Google Scholar] [CrossRef] [PubMed]
- Jardon, C.; Choi, K.R. COVID-19 experiences and mental health among graduate and undergraduate nursing students in Los Angeles. J. Am. Psychiatr. Nurses Assoc. 2022, 30, 86–942. [Google Scholar] [CrossRef]
- Ding, Q.; Ward, M.D.; Edwards, N.; Wu, E.A.; Kersey, S.; Funk, M. A mixed-methods approach to understand university students’ perceived impact of returning to class during COVID-19 on their mental and general health. PLoS ONE 2023, 18, e0279813. [Google Scholar] [CrossRef]
- Pandit, N.; Monda, S.; Campbell, K. Anticipatory worry and returning to campus during the COVID-19 pandemic. J. Am. Coll. Health, 2022; ahead of print. [Google Scholar]
- Hu, K.; Godfrey, K.; Ren, Q.; Wang, S.; Yang, X.; Li, Q. The impact of the COVID-19 pandemic on college students in USA: Two years later. Psychiatry Res. 2022, 315, 114685. [Google Scholar] [CrossRef]
- Andersen, R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995, 36, 1–10. [Google Scholar] [CrossRef]
- Babitsch, B.; Gohl, D.; Von Lengerke, T. Re-revisiting Andersen’s Behavioral Model of Health Services Use: A systematic review of studies from 1998–2011. GMS Psycho Soc. Med. 2012, 9, 9. [Google Scholar]
- Sampogna, G.; Bakolis, I.; Evans-Lacko, S.; Robinson, E.; Thornicroft, G.; Henderson, C. The impact of social marketing campaigns on reducing mental health stigma: Results from the 2009–2014 Time to Change programme. Eur. Psychiatry 2017, 40, 116–122. [Google Scholar] [CrossRef]
- Grelle, K.; Shrestha, N.; Ximenes, M.; Perrotte, J.; Cordaro, M.; Deason, R.G.; Howard, K. The Generation Gap Revisited: Generational Differences in Mental Health, Maladaptive Coping Behaviors, and Pandemic-Related Concerns During the Initial COVID-19 Pandemic. J. Adult Dev. 2023, 30, 381–392. [Google Scholar] [CrossRef] [PubMed]
- Eisenberg, D.; Hunt, J.; Speer, N.; Zivin, K. Mental health service utilization among college students in the United States. J. Nerv. Ment. Dis. 2011, 199, 301–308. [Google Scholar] [CrossRef]
- Rafal, G.; Gatto, A.; DeBate, R. Mental health literacy, stigma, and help-seeking behaviors among male college students. J. Am. Coll. Health 2018, 66, 284–291. [Google Scholar] [CrossRef]
- Mackenzie, C.S.; Gekoski, W.L.; Knox, V.J. Age, gender, and the underutilization of mental health services: The influence of help-seeking attitudes. Aging Ment. Health 2006, 10, 574–582. [Google Scholar] [CrossRef]
- Nam, S.K.; Chu, H.J.; Lee, M.K.; Lee, J.H.; Kim, N.; Lee, S.M. A meta-analysis of gender differences in attitudes toward seeking professional psychological help. J. Am. Coll. Health 2010, 59, 110–116. [Google Scholar] [CrossRef]
- Sprung, J.M.; Rogers, A. Work-life balance as a predictor of college student anxiety and depression. J. Am. Coll. Health 2021, 69, 775–782. [Google Scholar] [CrossRef] [PubMed]
- Logan, J.; Hughes, T.; Logan, B. Overworked? An observation of the relationship between student employment and academic performance. J. Coll. Stud. Retent. Res. Theory Pr. 2016, 18, 250–262. [Google Scholar] [CrossRef]
- Flores, E.C.; Fuhr, D.C.; Bayer, A.M.; Lescano, A.G.; Thorogood, N.; Simms, V. Mental health impact of social capital interventions: A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 107–119. [Google Scholar] [CrossRef] [PubMed]
- Coombs, N.C.; Meriwether, W.E.; Caringi, J.; Newcomer, S.R. Barriers to healthcare access among US adults with mental health challenges: A population-based study. SSM-Popul. Health 2021, 15, 100847. [Google Scholar] [CrossRef] [PubMed]
- Kecojevic, A.; Basch, C.H.; Sullivan, M.; Davi, N.K. The impact of the COVID-19 epidemic on mental health of undergraduate students in New Jersey, cross-sectional study. PLoS ONE 2020, 15, e0239696. [Google Scholar] [CrossRef] [PubMed]
- Son, C.; Hegde, S.; Smith, A.; Wang, X.; Sasangohar, F. Effects of COVID-19 on college students’ mental health in the United States: Interview survey study. J. Med. Internet Res. 2020, 22, e21279. [Google Scholar] [CrossRef]
- Wang, X.; Hegde, S.; Son, C.; Keller, B.; Smith, A.; Sasangohar, F. Investigating mental health of US college students during the COVID-19 pandemic: Cross-sectional survey study. J. Med. Internet Res. 2020, 22, e22817. [Google Scholar] [CrossRef] [PubMed]
- Wilson, O.W.; Holland, K.E.; Elliott, L.D.; Duffey, M.; Bopp, M. The impact of the COVID-19 pandemic on US college students’ physical activity and mental health. J. Phys. Act. Health 2021, 18, 272–278. [Google Scholar] [CrossRef]
- Lipson, S.K.; Zhou, S.; Abelson, S.; Heinze, J.; Jirsa, M.; Morigney, J.; Patterson, A.; Singh, M.; Eisenberg, D. Trends in college student mental health and help-seeking by race/ethnicity: Findings from the national healthy minds study, 2013–2021. J. Affect. Disord. 2022, 306, 138–147. [Google Scholar] [CrossRef]
- Pfefferbaum, B.; North, C.S. Mental health and the COVID-19 pandemic. N. Engl. J. Med. 2020, 383, 510–512. [Google Scholar] [CrossRef]
- Liu, C.H.; Stevens, C.; Wong, S.H.; Yasui, M.; Chen, J.A. The prevalence and predictors of mental health diagnoses and suicide among US college students: Implications for addressing disparities in service use. Depress. Anxiety 2019, 36, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Kodish, T.; Lau, A.S.; Gong-Guy, E.; Congdon, E.; Arnaudova, I.; Schmidt, M.; Shoemaker, L.; Craske, M.G. Enhancing racial/ethnic equity in college student mental health through innovative screening and treatment. Adm. Policy Ment. Health Ment. Health Serv. Res. 2021, 49, 267–282. [Google Scholar] [CrossRef]
- McGuire, T.G.; Miranda, J. New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Aff. 2008, 27, 393–403. [Google Scholar] [CrossRef]
- Sontag-Padilla, L.; Woodbridge, M.W.; Mendelsohn, J.; D’Amico, E.J.; Osilla, K.C.; Jaycox, L.H.; Eberhart, N.K.; Burnam, A.M.; Stein, B.D. Factors affecting mental health service utilization among California public college and university students. Psychiatr. Serv. 2016, 67, 890–897. [Google Scholar] [CrossRef] [PubMed]
- Yorgason, J.B.; Linville, D.; Zitzman, B. Mental health among college students: Do those who need services know about and use them? J. Am. Coll. Health 2008, 57, 173–182. [Google Scholar] [CrossRef]
- Harris, B.R.; Maher, B.M.; Wentworth, L. Optimizing efforts to promote mental health on college and university campuses: Recommendations to facilitate usage of services, resources, and supports. J. Behav. Health Serv. Res. 2022, 49, 252–258. [Google Scholar] [CrossRef]
- Al-Mawee, W.; Kwayu, K.M.; Gharaibeh, T. Student’s perspective on distance learning during COVID-19 pandemic: A case study of Western Michigan University, United States. Int. J. Educ. Res. Open 2021, 2, 100080. [Google Scholar] [CrossRef]
- Chen, E.; Kaczmarek, K.; Ohyama, H. Student perceptions of distance learning strategies during COVID-19. J. Dent. Educ. 2020, 85 (Suppl. S1), 1190. [Google Scholar] [CrossRef] [PubMed]
- Garris, C.P.; Fleck, B. Student evaluations of transitioned-online courses during the COVID-19 pandemic. Sch. Teach. Learn. Psychol. 2022, 8, 119. [Google Scholar] [CrossRef]
- Ironsi, C.S. Navigating learners towards technology-enhanced learning during post COVID-19 semesters. Trends Neurosci. Educ. 2022, 29, 100189. [Google Scholar] [CrossRef] [PubMed]
- Pattyn, E.; Verhaeghe, M.; Bracke, P. The gender gap in mental health service use. Soc. Psychiatry Psychiatr. Epidemiol. 2015, 50, 1089–1095. [Google Scholar] [CrossRef]
- McKenzie, S.K.; Collings, S.; Jenkin, G.; River, J. Masculinity, social connectedness, and mental health: Men’s diverse patterns of practice. Am. J. Men’s Health 2018, 12, 1247–1261. [Google Scholar] [CrossRef] [PubMed]
- Curtin, R.; Presser, S.; Singer, E. The effects of response rate changes on the index of consumer sentiment. Public Opin. Q. 2000, 64, 413–428. [Google Scholar] [CrossRef] [PubMed]
- Moore, D.L.; Tarnai, J. Evaluating nonresponse error in mail surveys. In Survey. Nonresponse; Groves, R.M., Dillman, D.A., Eltinge, J.L., Little, R.J.A., Eds.; Wiley: Hoboken, NJ, USA, 2002; pp. 197–211. ISBN 978-0-471-39627-7. [Google Scholar]
- Roberts, M.E.; Bell, E.A.; Meyer, J.L. Mental health and academic experiences among US college students during the COVID-19 pandemic. Front. Psychol. 2023, 14, 1166960. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).