Examination of the Transdiagnostic Role of Impulsivity in the Development of ADHD and ODD Symptoms in Primary and Secondary School Students
Abstract
1. Introduction
Attention Deficit/Hyperactivity Disorder and Oppositional Defiant Disorder: Comorbidity and the Transdiagnostic Approach
2. Materials and Methods
2.1. Participants
2.2. Measures
2.3. Procedure
3. Results
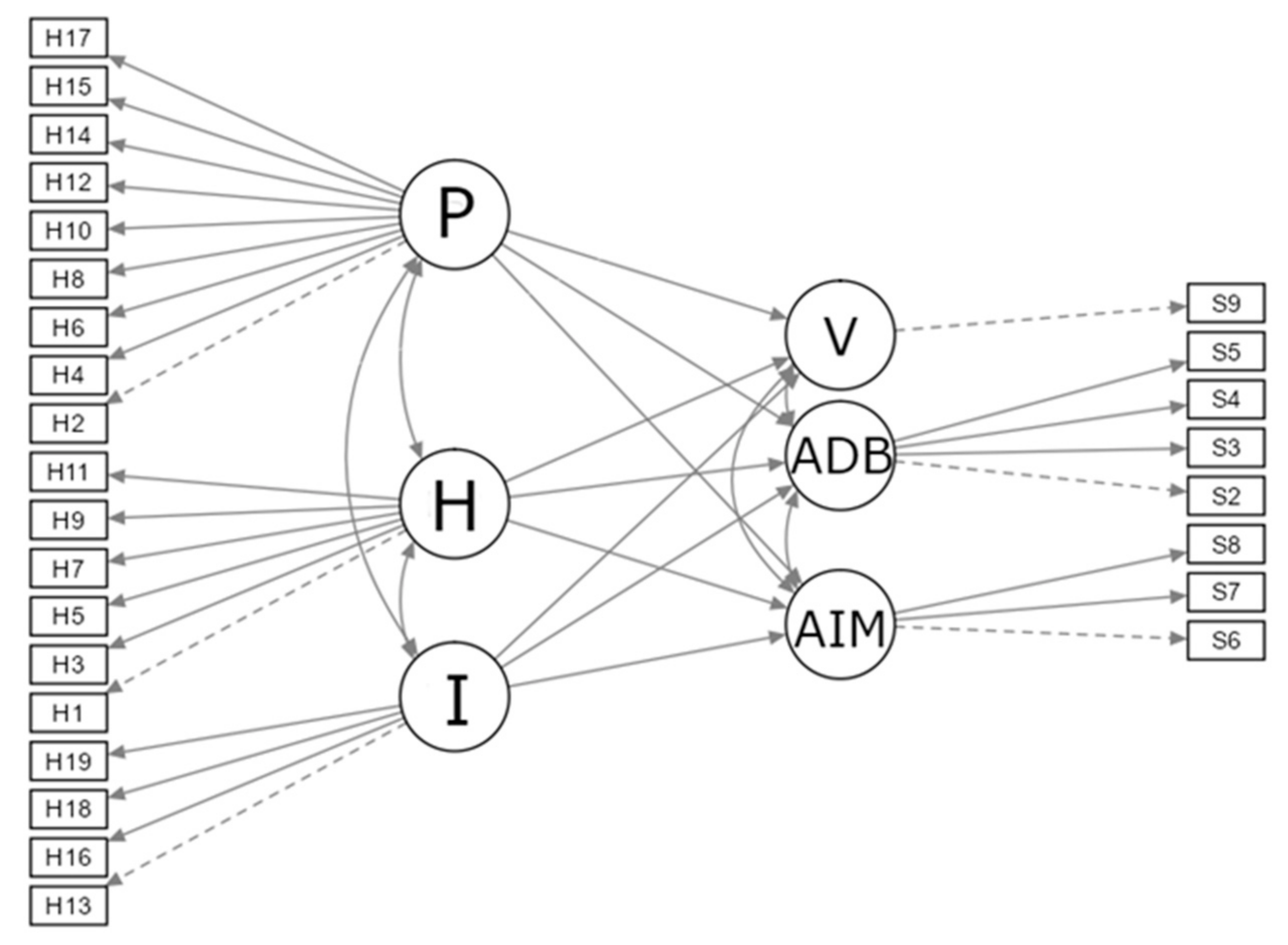
3.1. SEM Analyses
3.1.1. Model 1
3.1.2. Model 2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. ADHD and ODD Items (in Croatian and Translated into English)
| Hyperactivity (6) | |
| H1 | Teško mi je mirno sjediti na jednom mjestu. It is hard for me to sit still in one place. |
| H3 | Ne mogu biti miran i sjediti na jednom mjestu, već moram ustajati, mahati nogama i vrpoljiti se. I can’t be still and sit in one place, I have to stand up and fidget. |
| H5 | Za mene se može reći da sam nemirna i pretjerano aktivna osoba. I am a restless and overly active person. |
| H7 | Nemam strpljenja za aktivnosti i obaveze koje se moraju obavljati polako i tiho. I have no patience for activities and obligations that must be done slowly and quietly. |
| H9 | Nikad nemam mira. I am never at peace. |
| H11 | Brbljav sam i previše pričam. I’m chatty and I talk too much. |
| Impulsivity (4) | |
| H13 | Dajem odgovore i prije nego što čujem pitanje do kraja. I answer before I hear the end of the question. |
| H16 | Nemam strpljenja čekati u redu. I have no patience to wait in line. |
| H18 | Upadam drugima u razgovor. I interrupt other people’s conversations. |
| H19 | Prekidam ili ometam druge u onome što rade ili govore. I interrupt or disrupt others in what they are doing or saying. |
| Attention (9) | |
| H2 | Griješim u pisanju školske zadaće jer se ne mogu koncentrirati na ono što radim. I make mistakes in my homework because I can’t concentrate on what I’m doing. |
| H4 | Teško mi je održati pažnju tijekom pisanja zadaće ili neke igre. It’s hard for me to pay attention while doing homework or playing a game. |
| H6 | Ne slušam druge čak i kad mi se izravno obraćaju. I don’t listen to others even when they speak directly to me. |
| H8 | Događa mi se da ne završim školsku zadaću ili učenje do kraja jer više nemam strpljenja. I do not finish my homework because I lose focus and patience. |
| H10 | Teško mi je organizirati moje obveze, aktivnosti, učenje i dr. It is difficult for me to organize my obligations, activities, learning, etc. |
| H12 | Izbjegavam zadatke i obveze koji zahtijevaju dužu koncentraciju i veće mentalne napore. I avoid tasks and obligations that require longer concentration and greater mental effort. |
| H14 | Spadam u one učenike koji često gube stvari, na primjer školski pribor, knjige i sl. I often lose school things like supplies, books, etc. |
| H15 | Čini mi se da me sve oko mene može vrlo lako omesti. It seems to me that everything around me can easily distract me. |
| H17 | Zaboravljam i svakodnevne obveze. I forget my day-to-day obligations. |
| Angry/Irritable Mood (3) | |
| S6 | Lako sam se uzrujao. I often lose temper. |
| S7 | Bio sam osjetljiv na postupke drugih. I am often touchy or easily annoyed. |
| S8 | Bio sam ljutit i srdit. I am often angry and resentful. |
| Argumentative/Defiant Behaviour (4) | |
| S2 | Svađao sam se s odraslima. I often argue with authority figures or adults. |
| S3 | Aktivno sam se suprotstavljao ili odbijao pokoriti zahtjevima i pravilima odraslih. I often actively defy or refuse to comply with requests from authority figures or with rules. |
| S4 | Namjerno sam ometao druge ljude. I often deliberately annoy others. |
| S5 | Okrivio sam druge za vlastite pogreške ili loše ponašanje. I often blame others for my mistakes or misbehavior. |
| Vindictiveness (1) | |
| S9 | Bio sam zloban i osvetoljubiv. I have been spiteful or vindictive. |
References
- Moreno-De-Luca, A.; Myers, S.M.; Challman, T.D.; Moreno-De-Luca, D.; Evans, D.W.; Ledbetter, D.H. Developmental brain dysfunction: Revival and expansion of old concepts based on new genetic evidence. Lancet Neurol. 2013, 12, 406–414. [Google Scholar] [CrossRef] [PubMed]
- Cicchetti, D. Developmental psychopathology. In Developmental Psychopathology: Volume 1. Theory and Method, 2nd ed.; Cicchetti, D., Cohen, D.J., Eds.; Wiley: Hoboken, NJ, USA, 2006; pp. 1–23. [Google Scholar]
- Angold, A.; Costello, E.J.; Erkanli, A. Comorbidity. J. Child Psychol. Psychiatry 1999, 40, 57–97. [Google Scholar] [CrossRef] [PubMed]
- Beauchaine, T.P.; McNulty, T. Comorbidities and continuities as ontogenic processes: Toward a developmental spectrum model of externalizing psychopathology. Dev. Psychopathol. 2013, 25, 1505–1528. [Google Scholar] [CrossRef]
- Nigg, J.T.; Barkley, R.A. Attention Deficit/Hyperactivity Disorder. In Child Psychopathology: Third Edition; Mash, E.J., Barkley, R.A., Eds.; The Guilford Press: New York, NY, USA, 2014; pp. 75–145. [Google Scholar]
- Rowe, R.; Costello, J.; Angold, A.; Copeland, W.E.; Maughan, B. Developmental pathways in oppositional defiant disorder and conduct disorder. J. Abnorm. Psychol. 2010, 119, 726–738. [Google Scholar] [CrossRef] [PubMed]
- Beauchaine, T.P.; Hinshaw, S.P.; Pang, K.L. Comorbidity of attention-deficit/hyperactivity disorder and early onset conduct disorder: Biological, environmental, and developmental mechanisms. Clin. Psychol. Sci. Pract. 2010, 17, 327–336. [Google Scholar] [CrossRef]
- Steinhoff, K.W.; Lerner, M.; Kapilinsky, A.; Kotkin, R.; Wigal, S.; Steinberg-Epstein, R.; Wigal, T.; Swanson, J.M. Attention Deficit/Hyperactivity Disorder. In Handbook of Preschool Mental Health: Development, Disorders, and Treatment; Luby, J.L., Ed.; The Guilford Press: New York, NY, USA, 2006; pp. 63–80. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Olson, S.L.; Choe, D.E.; Sameroff, A.J. Trajectories of child externalizing problems between ages 3 and 10 years: Contributions of children’s early effortful control, theory of mind, and parenting experiences. Dev. Psychopathol. 2017, 29, 1333–1351. [Google Scholar] [CrossRef]
- Liu, J. Childhood externalizing behavior: Theory and implications. J. Child Adolesc. Psychiatr. Nurs. 2004, 17, 93–103. [Google Scholar] [CrossRef]
- Ersan, C.; Tok, Ş. The study of the aggression levels of preschool children in terms of emotion expression and emotion regulation. Educ. Sci. 2020, 45, 359–391. [Google Scholar] [CrossRef]
- Hay, D.F.; Payne, A.; Chadwick, A. Peer relations in childhood. J. Child Psychol. Psychiatry 2004, 45, 84–108. [Google Scholar] [CrossRef]
- Ehrenreich-May, J.; Chu, B.C. Overview of transdiagnostic mechanisms and treatments for youth psychopathology. In Transdiagnostic Treatments for Children and Adolescents: Principles and Practice; Ehrenreich-May, J., Chu, B.C., Eds.; The Guilford Press: New York, NY, USA, 2013; pp. 3–14. [Google Scholar]
- Newcorn, J.H.; Halperin, J.M.; Miller, C.J. ADHD with oppositionality and aggression. In ADHD Comorbidities: Handbook for ADHD Complications in Children and Adults; Brown, T.E., Ed.; American Psychiatric Publishing, Inc.: Washington, DC, USA, 2009; pp. 157–176. [Google Scholar]
- Pliszka, S. Comorbid Psychiatric Disorders in Children with ADHD. In Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis & Treatment; Barkley, R.A., Ed.; The Guilford Press: New York, NY, USA, 2018; pp. 81–116. [Google Scholar]
- Roberts, W.; Milich, R.; Barkley, R.A. Primary symptoms, diagnostic criteria, subtyping, and prevalence of ADHD. In Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis & Treatment; Barkley, R.A., Ed.; The Guilford Press: New York, NY, USA, 2018; pp. 51–81. [Google Scholar]
- Canino, G.; Polanczyk, G.; Bauermeister, J.J.; Rohde, L.A.; Frick, P.J. Doest the prevalence of CD and ODD vary across cultures? Soc. Psychiatry Psychiatr. Epidemiol. 2010, 45, 695–704. [Google Scholar] [CrossRef]
- Swanson, J.; Arnold, E.; Kraemer, H.; Hechtman, L.; Molina, B.; Hinshaw, S.; Vitiello, B.; Jensen, P.; Steinhoff, K.; Lerner, M.; et al. Evidence, interpretation, and qualification from the multiple reports of long-term outcomes in the Multimodal Treatment study of Children With ADHD (MTA): Part I: Executive summary. J. Atten. Disord. 2008, 12, 4–14. [Google Scholar] [CrossRef] [PubMed]
- Barkley, R.A. Emotional dysregulation is a core component of ADHD. In Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis & Treatment; Barkley, R.A., Ed.; The Guilford Press: New York, NY, USA, 2018; pp. 81–116. [Google Scholar]
- Gottman, J.M.; Katz, L.F. Effects of marital discord on young children’s peer interaction and health. Dev. Psychol. 1989, 25, 373–381. [Google Scholar] [CrossRef]
- Van Stralen, J. Emotional dysregulation in children with attention-deficit/hyperactivity disorder. ADHD Atten. Deficit Hyperact. Disord. 2016, 8, 175–184. [Google Scholar] [CrossRef]
- Cavanagh, M.; Quinn, M.; Duncan, D.; Graham, T.; Balbuena, L. Oppositional defiant disorder I better conceptualized as a disorder of emotional regulation. J. Atten. Disord. 2016, 21, 381–389. [Google Scholar] [CrossRef] [PubMed]
- Burke, J.D.; Romano-Verthelyi, A.M. Oppositional defiant disorder. In Developmental Pathways to Disruptive, Impulse-Control and Conduct Disorders; Martel, M.M., Ed.; Elsevier Inc.: Amsterdam, The Netherlands, 2018; pp. 21–52. [Google Scholar]
- Vulić-Prtorić, A. Skala agresivnosti za djecu i adolescente. In Zbirka psihologijskih skala i upitnika 4; Penezić, Z., Ćubela Adorić, V., Proroković, A., Tucak Junaković, I., Eds.; Sveučilište u Zadru: Zadar, Croatia, 2018; pp. 83–99. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th revised ed.; American Psychiatric Association: Arlington, VA, USA, 2000. [Google Scholar]
- Vulić-Prtorić, A. Skala hiperaktivnosti–impulzivnosti–pažnje–HIP. In Zbirka psihologijskih skala i upitnika 3; Ćubela Adorić, V., Proroković, A., Penezić, Z., Tucak, I., Eds.; Sveučilište u Zadru: Zadar, Croatia, 2006; pp. 41–49. [Google Scholar]
- Satorra, A.; Bentler, P.M. Corrections to test statistics and standard errors in covariance structure analysis. In Latent Variables Analysis: Applications for Developmental Research; von Eye, A., Clogg, C.C., Eds.; Sage Publications, Inc.: London, UK, 1994; pp. 399–419. [Google Scholar]
- Curran, P.J.; West, S.G.; Finch, J.F. The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychol. Methods 1996, 1, 16–29. [Google Scholar] [CrossRef]
- Yu, C.Y.; Muthén, B. Evaluation of Model Fit Indices for Latent Variable Models with Categorical and Continuous Outcomes; Technical Report; Graduate School of Education & Information Studies, University of California: Los Angeles, CA, USA, 2002. [Google Scholar]
- Yuan, K.-H. Fit indices versus test statistics. Multivar. Behav. Res. 2005, 40, 115–148. [Google Scholar] [CrossRef] [PubMed]
- Barkley, R.A.; Fischer, M. The unique contribution of emoional impulsiveness to impairment in major life activities in hyperactive children as adults. J. Am. Acad. Child Adolesc. Psychiatry 2010, 49, 503–513. [Google Scholar] [CrossRef]
- Barkley, R.A. Barkley Adult ADHD Rating Scale—IV (BAARS-IV); The Guilford Press: New York, NY, USA, 2011. [Google Scholar]
- Willcutt, E.G.; Nigg, J.T.; Pennington, B.F.; Solanto, M.V.; Rohde, L.A.; Tannock, R.; Loo, S.K.; Carlson, C.L.; McBurnett, K.; Lahey, B.B. Validity of DSM-IV attention deficit/Hyperactivity disorder symptom dimensions and subtypes. J. Abnorm. Psychol. 2012, 121, 991–1010. [Google Scholar] [CrossRef]
- Owens, E.B.; Cardoos, S.L.; Hinshaw, S.P. Developmental progression and gender differences among individuals with ADHD. In Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis & Treatment; Barkley, R.A., Ed.; The Guilford Press: New York, NY, USA, 2018; pp. 223–256. [Google Scholar]
- Biderman, J.; Petty, C.R.; Evans, M.; Small, J.; Faraone, S.V. How persistent is ADHD? A controlled 10-year follow-up study of boys with ADHD. Psychiatry Res. 2010, 177, 299–308. [Google Scholar] [CrossRef]
- DuPaul, G.J.; Langberg, J. Educational impairments in children with ADHD. In Attention-Deficit Hyperactivity Disorder: A Handbook for Diagnosis & Treatment; Barkley, R.A., Ed.; The Guilford Press: New York, NY, USA, 2018; pp. 169–191. [Google Scholar]
- Langberg, J.M.; Brooke, S.G.; Molina, L.; Eugene, A.; Epstein, J.N.; Altaye, M.; Hinshaw, S.P.; Swanson, J.M.; Wigal, T.; Hechtman, L. Patterns and predictors of adolescent academic achievement and performance in a sample of children with Attention-Deficit/Hyperactivity Disorder. J. Clin. Child Adolesc. Psychol. 2011, 40, 519–531. [Google Scholar] [CrossRef]
- Harty, S.C.; Miller, C.J.; Newcorn, J.H.; Halperin, J.M. Adolescents with childhood ADHD and comorbid disruptive behavior disorders: Aggression, anger and hostility. Child Psychiatry Hum. Dev. 2009, 40, 85–97. [Google Scholar] [CrossRef]
- Karalunas, S.L.; Fair, D.; Musser, E.D.; Aykes, K.; Iyer, S.P.; Nigg, J.T. Subtyping Attention Deficit/Hyperactivity Disorder using temperament dimensions. JAMA Psychiatry 2014, 71, 1015–1024. [Google Scholar] [CrossRef]
- Karalunas, S.L.; Gustafsson, H.C.; Fair, D.; Musser, E.D.; Nigg, J.T. Do we need an irritable subtype of ADHD? Replication and extension of a promising temperament profile approach to ADHD subtyping. Psychol. Assess. 2019, 1, 236–247. [Google Scholar] [CrossRef]
- Stringaris, A. Irritability in children and adolescents: A challenge for DSM-5. Eur. Child Adolesc. Psychiatry 2011, 20, 21–66. [Google Scholar] [CrossRef]
- Harvey, E.A.; Breaux, R.P.; Lugo-Candelas, C.I. Early development of comorbidity between symptoms of attention-deficit/hyperactivity disorder (ADHD) and oppositional defiant disorder (ODD). J. Abnorm. Psychol. 2016, 125, 154–167. [Google Scholar] [CrossRef]
- Burt, S.A.; Krueger, R.F.; McGue, M.; Iacono, W.G. Sources of covariation among attention-deficit/hyperactivity disorder, oppositional defiant disorder, and conduct disorder: The importance of shared environment. J. Abnorm. Psychol. 2001, 110, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Antonini, T.N.; Becker, S.P.; Tamm, L.; Epstein, J.N. Hot and cool executive functions in children with attention deficit/hyperactivity disorder and comorbid oppositional defiant disorder. J. Int. Neuropsychol. Soc. 2015, 21, 584–595. [Google Scholar] [CrossRef]
- Luman, M.; Sergeant, J.A.; Knol, D.L.; Oosterlaan, J. Impaired decision making in oppositional defiant disorder related to altered psychophysiological responses to reinforcement. Biol. Psychiatry 2010, 68, 337–344. [Google Scholar] [CrossRef]
| Class | Female | Male | Σ | % | |
|---|---|---|---|---|---|
| Primary school | 5. | 48 | 45 | 93 | 8.0 |
| 6. | 52 | 47 | 99 | 8.5 | |
| 7. | 47 | 55 | 102 | 8.8 | |
| 8. | 59 | 55 | 114 | 9.8 | |
| Σ: | 206 | 202 | 408 | ||
| Secondary school | 1. | 59 | 57 | 116 | 10.1 |
| 2. | 123 | 106 | 229 | 19.7 | |
| 3. | 208 | 135 | 343 | 29.5 | |
| 4. | 28 | 37 | 65 | 5.6 | |
| Σ: | 418 | 335 | 753 | ||
| Overall: | 624 | 537 | 1161 | ||
| % | 53,7 | 46,3 | 100% |
| HIP | H | I | P | ODD | AIM | ADB | V | |
|---|---|---|---|---|---|---|---|---|
| N | 1154 | 1158 | 1158 | 1156 | 1144 | 1152 | 1151 | 1158 |
| Number of items | 19 | 6 | 4 | 9 | 9 | 3 | 4 | 1 |
| Range | 19–95 | 6–30 | 4–20 | 9–45 | 9–45 | 3–15 | 4–20 | 1–5 |
| Median | 42 | 14 | 9 | 19 | 21 | 8 | 8 | 1 |
| IQR | 20 | 8 | 4 | 10 | 10 | 4 | 5 | 1 |
| ω | 0.92 | 0.84 | 0.77 | 0.86 | 0.85 | 0.76 | 0.75 | / |
| H | I | P | AIM | ADB | V | ||
|---|---|---|---|---|---|---|---|
| N | M | 533 | 533 | 530 | 531 | 528 | 533 |
| F | 623 | 622 | 623 | 618 | 620 | 622 | |
| PS | 406 | 406 | 404 | 407 | 405 | 407 | |
| SS | 752 | 752 | 752 | 745 | 746 | 751 | |
| Missing | M | 0 | 0 | 3 | 2 | 5 | 0 |
| F | 0 | 1 | 0 | 5 | 3 | 1 | |
| PS | 1 | 1 | 3 | 0 | 2 | 0 | |
| SS | 0 | 0 | 0 | 7 | 6 | 1 | |
| Min | M | 6 | 4 | 9 | 3 | 4 | 1 |
| F | 6 | 4 | 9 | 3 | 4 | 1 | |
| PS | 6 | 4 | 9 | 3 | 4 | 1 | |
| SS | 6 | 4 | 9 | 3 | 4 | 1 | |
| Max | M | 30 | 20 | 43 | 15 | 20 | 5 |
| F | 30 | 20 | 45 | 15 | 20 | 5 | |
| PS | 30 | 20 | 45 | 15 | 20 | 5 | |
| SS | 30 | 20 | 43 | 15 | 20 | 5 | |
| Median | M | 14 | 9 | 19 | 7 | 8 | 2 |
| F | 15 | 9 | 19 | 8 | 8 | 1 | |
| PS | 13 | 8 | 16 | 6 | 7 | 1 | |
| SS | 15 | 9 | 20 | 8 | 9 | 2 | |
| IQR | M | 7 | 5 | 10 | 4 | 5 | 2 |
| F | 8 | 4 | 10 | 4 | 4 | 1 | |
| PS | 8 | 5 | 9 | 5 | 5 | 1 | |
| SS | 7 | 5 | 9 | 4 | 4 | 1 | |
| Shapiro—Wilk W | M | 0.96 | 0.96 | 0.95 | 0.96 | 0.95 | 0.77 |
| F | 0.96 | 0.95 | 0.96 | 0.98 | 0.95 | 0.71 | |
| PS | 0.95 | 0.94 | 0.91 | 0.94 | 0.90 | 0.69 | |
| SS | 0.97 | 0.96 | 0.97 | 0.98 | 0.96 | 0.77 | |
| Shapiro—Wilk p | M | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| F | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| PS | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | |
| SS | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| U | p | Effect Size (rrb) | |
|---|---|---|---|
| H | 158,015 | 0.16 | 0.05 |
| I | 156,833 | 0.11 | 0.05 |
| P | 164,247 | 0.88 | 0.05 |
| AIM | 128,758 | <0.001 | 0.22 |
| ADB | 158,590 | 0.36 | 0.03 |
| V | 145,269 | <0.001 | 0.12 |
| U | p | Effect Size (rrb) | |
|---|---|---|---|
| H | 128,765 | <0.001 | 0.16 |
| I | 136,642 | 0.003 | 0.11 |
| P | 109,380 | <0.001 | 0.28 |
| AIM | 107,922 | <0.001 | 0.29 |
| ADB | 111,020 | <0.001 | 0.27 |
| V | 139,164 | 0.006 | 0.09 |
| HIP | H | I | P | ODD | AIM | ADB | V | |
|---|---|---|---|---|---|---|---|---|
| HIP | 1 | |||||||
| H | 0.73 *** | 1 | ||||||
| I | 0.65 *** | 0.51 *** | 1 | |||||
| P | 0.73 *** | 0.50 *** | 0.46 *** | 1 | ||||
| ODD | 0.48 *** | 0.38 *** | 0.41 *** | 0.46 *** | 1 | |||
| AIM | 0.37 *** | 0.29 *** | 0.31 *** | 0.39 *** | 0.73 *** | 1 | ||
| ADB | 0.47 *** | 0.39 *** | 0.41 *** | 0.41 *** | 0.72 *** | 0.43 *** | 1 | |
| V | 0.37 *** | 0.30 *** | 0.32 *** | 0.37 *** | 0.56 *** | 0.44 *** | 0.46 *** | 1 |
| HIP | H | I | P | ODD | AIM | ADB | V | |
|---|---|---|---|---|---|---|---|---|
| HIP | 1 | |||||||
| H | 0.75 *** | 1 | ||||||
| I | 0.63 *** | 0.47 *** | 1 | |||||
| P | 0.80 *** | 0.57 *** | 0.48 *** | 1 | ||||
| ODD | 0.48 *** | 0.43 *** | 0.42 *** | 0.43 *** | 1 | |||
| AIM | 0.37 *** | 0.34 *** | 0.31 *** | 0.35 *** | 0.67 *** | 1 | ||
| ADB | 0.44 *** | 0.39 *** | 0.40 *** | 0.40 *** | 0.69 *** | 0.35 *** | 1 | |
| V | 0.30 *** | 0.26 *** | 0.30 *** | 0.27 *** | 0.47 *** | 0.26 *** | 0.39 *** | 1 |
| χ2, df, p | CFI | SRMR | RMSEA | |
|---|---|---|---|---|
| Model 1 | 709, 310, <0.001 | 0.906 | 0.047 | 0.049 |
| Criterion | Predictor | Parameter Estimate | Standard Error | β | p |
|---|---|---|---|---|---|
| AIM | I | 0.21 | 0.29 | 0.12 | 0.47 |
| AIM | H | 0.10 | 0.14 | 0.08 | 0.51 |
| ADB | I | 0.57 | 0.25 | 0.37 | 0.02 |
| ADB | H | 0.14 | 0.13 | 0.13 | 0.30 |
| V | I | 0.43 | 0.30 | 0.23 | 0.15 |
| V | H | −0.08 | 0.15 | −0.06 | 0.58 |
| AIM | P | 0.62 | 0.19 | 0.48 | < 0.001 |
| ADB | P | 0.37 | 0.15 | 0.32 | 0.01 |
| V | P | 0.48 | 0.17 | 0.34 | 0.01 |
| χ2, df, p | CFI | SRMR | RMSEA | |
|---|---|---|---|---|
| Model | 1653, 310, <0.001 | 0.827 | 0.062 | 0.074 |
| Criterion | Predictor | Paramter Estimate | Standard Error | β | p |
|---|---|---|---|---|---|
| AIM | I | 0.10 | 0.10 | 0.08 | 0.30 |
| AIM | H | 0.35 | 0.16 | 0.28 | 0.03 |
| ADB | I | 0.40 | 0.07 | 0.41 | <0.001 |
| ADB | H | 0.21 | 0.11 | 0.23 | 0.06 |
| V | I | 0.50 | 0.11 | 0.36 | <0.001 |
| V | H | 0.21 | 0.18 | 0.15 | 0.24 |
| AIM | P | 0.38 | 0.18 | 0.27 | 0.04 |
| ADB | P | 0.16 | 0.13 | 0.15 | 0.23 |
| V | P | −0.06 | 0.20 | −0.04 | 0.76 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barać, B.; Vulić-Prtorić, A. Examination of the Transdiagnostic Role of Impulsivity in the Development of ADHD and ODD Symptoms in Primary and Secondary School Students. Educ. Sci. 2023, 13, 399. https://doi.org/10.3390/educsci13040399
Barać B, Vulić-Prtorić A. Examination of the Transdiagnostic Role of Impulsivity in the Development of ADHD and ODD Symptoms in Primary and Secondary School Students. Education Sciences. 2023; 13(4):399. https://doi.org/10.3390/educsci13040399
Chicago/Turabian StyleBarać, Bruno, and Anita Vulić-Prtorić. 2023. "Examination of the Transdiagnostic Role of Impulsivity in the Development of ADHD and ODD Symptoms in Primary and Secondary School Students" Education Sciences 13, no. 4: 399. https://doi.org/10.3390/educsci13040399
APA StyleBarać, B., & Vulić-Prtorić, A. (2023). Examination of the Transdiagnostic Role of Impulsivity in the Development of ADHD and ODD Symptoms in Primary and Secondary School Students. Education Sciences, 13(4), 399. https://doi.org/10.3390/educsci13040399






