“Growing as a Stronger Clinician in Adverse Conditions”—A Snapshot of Clinical Training during COVID-19
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Data Collection
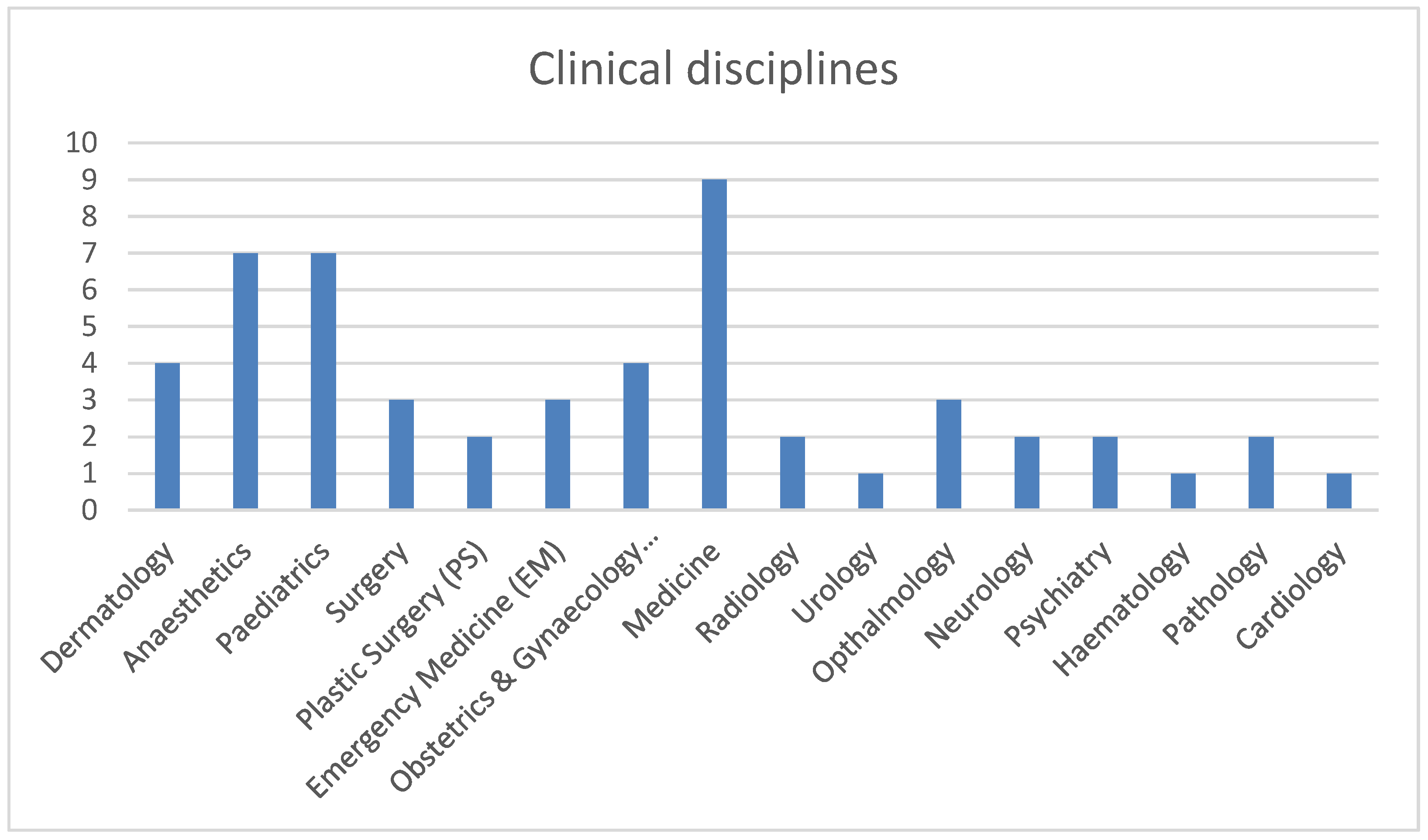
2.3. Sample
2.4. Data Analysis
3. Results
3.1. Challenges
3.1.1. Mental Distress
“…very few childcare options …[and] kids are only at school intermittently… this means anything currently “optional” on a work-front is NOT getting done in my off time e.g., studying and MMED”.(Medicine-P32)
“Being isolated from colleagues due to social distancing has had an impact on mental health”(Psychiatry-P43)
“Inability to see family has affected my psychological wellbeing so much, I’m not as productive as before”.(O&G-P41)
3.1.2. Resource Constraints and Systemic Deficiencies
“there are no resources or infrastructure”(Surgery-P28);
“extreme staff and resource shortages—gloves, masks”(EM-P14)
3.1.3. Compromised and Inadequate Training
3.2. Strengths and Opportunities
Resilience and Coping Strategies
3.3. Development of Graduate Competencies
3.3.1. Leadership
3.3.2. Health Advocacy, Collaboration, and Communication
3.4. New Learning and Training Opportunities
4. Discussion
5. Limitations and Concluding Remarks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Moonasar, D.; Pillay, A.; Leonard, E.; Naidoo, R.; Mngemane, S.; Ramkrishna, W.; Jamaloodien, K.; Lebese, L.; Chetty, K.; Bamford, L.; et al. COVID-19: Lessons and experiences from South Africa’ ’s first surge. BMJ Glob. Health 2021, 6, e004393. [Google Scholar] [CrossRef]
- Konopińska, J.; Obuchowska, I.; Lisowski, Ł.; Dub, N.; Dmuchowska, D.A.; Rękas, M. Impact of the COVID-19 pandemic on ophthalmic specialist training in Poland. PLoS ONE 2021, 16, e0257876. [Google Scholar] [CrossRef]
- Payne, A.; Rahman, R.; Bullingham, R.; Vamadeva, S.; Alfa-Wali, M. Redeployment of surgical trainees to intensive care during the COVID-19 pandemic: Evaluation of the impact on training and wellbeing. J. Surg. Educ. 2021, 78, 813–819. [Google Scholar] [CrossRef]
- Al-Hayouti, H.; Hinds, A.M.; Adams, G.G. Impact of COVID-19 on preparation for the Certificate of Eligibility for Specialist Registration (CESR) in Ophthalmology. Eye 2021, 27, 1–4. [Google Scholar] [CrossRef]
- Nedungadi, A.; Ming, C.; Woodward, F.; Lasoye, T.; Birns, J. Supporting the transition to becoming a medical registrar. Future Healthc. J. 2021, 8, e160–e163. [Google Scholar] [CrossRef] [PubMed]
- Clements, J.M.; Burke, J.; Nally, D.; Rabie, M.; Kane, E.; Barlow, E.; Mohamed, W.; King, M.; McClymont, L.; George, M.; et al. COVID-19 impact on Surgical Training and Recovery Planning (COVID-STAR)-A cross-sectional observational study. Int. J. Surg. 2021, 88, 105903. [Google Scholar] [CrossRef] [PubMed]
- Alexander, A.; Radke, H. Reshaping surgical specialist training in small animal surgery during and after the COVID-19 pandemic. Vet. Surg. 2021, 50, 924–932. [Google Scholar] [CrossRef] [PubMed]
- Hilburg, R.; Patel, N.; Ambruso, S.; Biewald, M.A.; Farouk, S.S. Medical education during the Coronavirus Disease-2019 pandemic: Learning from a distance. Adv. Chronic Kidney Dis. 2020, 27, 412–417. [Google Scholar] [CrossRef]
- Woolliscroft, J.O. Innovation in response to the COVID-19 pandemic crisis. Acad. Med. 2020, 95, 1140–1142. [Google Scholar] [CrossRef]
- Forsythe, R.O.; Suttie, S.A. Enhancing junior doctors’ working lives. Surgery 2020, 38, 607–611. [Google Scholar] [CrossRef]
- Bagwandeen, C.I.; Singaram, V.S. Feedback as a means to improve clinical competencies: Registrars’ perceptions of the quality of feedback provided by consultants in an academic hospital setting. Afr. J. Health Prof. Educ. 2016, 8, 117–120. [Google Scholar] [CrossRef]
- Mezirow, J.; Taylor, E.W. Transformative Learning in Practice: Insights from Community, Workplace, and Higher Education; John Wiley & Sons: San Francisco, CA, USA, 2009. [Google Scholar]
- Van Schalkwyk, S.C.; Hafler, J.; Brewer, T.F.; Maley, M.A.; Margolis, C.; McNamee, L.; Meyer, I.; Peluso, M.J.; Schmutz, A.M.; Spak, J.M.; et al. Transformative learning as pedagogy for the health professions: A scoping review. Med. Educ. 2019, 53, 547–558. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V.; Boulton, E.; Davey, L.; McEvoy, C. The online survey as a qualitative research tool. Int. J. Soc. Res. Methodol. 2020, 16, 1–4. [Google Scholar] [CrossRef]
- Emet, G.; Tat, M. Swot analysis: A theoretical review. J. Int. Soc. Res. 2017, 10, 994–1006. [Google Scholar] [CrossRef]
- SurveyMonkey Inc. Available online: www.surveymonkey.com (accessed on 14 December 2021).
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Boyatzis, R.E. Transforming Qualitative Information: Thematic Analysis and Code Development; Sage: Thousand Oaks, CA, USA, 1998. [Google Scholar]
- Vaismoradi, M.; Turunen, H.; Bondas, T. Content analysis and thematic analysis: Implications for conducting a qualitative descriptive study. Nurs. Health Sci. 2013, 15, 398–405. [Google Scholar] [CrossRef] [PubMed]
- Vaismoradi, M.; Jones, J.; Turunen, H.; Snelgrove, S. Theme development in qualitative content analysis and thematic analysis. J. Nurs. Educ. 2016, 6, 100–110. [Google Scholar] [CrossRef]
- Saldaña, J. The Coding Manual for Qualitative Researchers, 2nd ed.; SAGE: London, UK, 2013. [Google Scholar]
- Glaser, B.G. The constant comparative method of qualitative analysis. Soc. Probl. 1965, 12, 436–445. [Google Scholar] [CrossRef]
- Breakwell, G.M.; Jaspal, R. Identity change, uncertainty and mistrust in relation to fear and risk of COVID-19. J. Risk Res. 2020, 24, 335–351. [Google Scholar] [CrossRef]
- Polizzi, C.; Lynn, S.J.; Perry, A. Stress and coping in the time of COVID-19: Pathways to resilience and recovery. Clin. Neuropsychiatry 2020, 17, 59–62. [Google Scholar]
- Deveci, T. The transformative learning experiences of learners of English as a foreign language at a university preparatory programme. Transform. Dialogues Teach. Learn. J. 2014, 7, 1–19. [Google Scholar]
- Maseko, L.; Harris, B. People-centeredness in health system reform. Public perceptions of private and public hospitals in South Africa. S. Afr. J. Occup. Ther. 2018, 48, 22–27. [Google Scholar] [CrossRef][Green Version]
- Bradshaw, R.A.; Stahl, P.D. On pandemics, pandemonium, and possibilities…. FASEB BioAdv. 2020, 2, 329. [Google Scholar] [CrossRef]
- Matiz, A.; Fabbro, F.; Paschetto, A.; Cantone, D.; Paolone, A.R.; Crescentini, C. Positive impact of mindfulness meditation on mental health of female teachers during the COVID-19 outbreak in Italy. Int. J. Environ. Res. Public Health 2020, 17, 6450. [Google Scholar] [CrossRef]
- Yıldırım, M.; Arslan, G.; Özaslan, A. Perceived risk and mental health problems among healthcare professionals during COVID-19 pandemic: Exploring the mediating effects of resilience and coronavirus fear. Int. J. Ment. Health Addict. 2020, 16, 1–11. [Google Scholar] [CrossRef]
- Blake, H.; Bermingham, F.; Johnson, G.; Tabner, A. Mitigating the psychological impact of COVID-19 on healthcare workers: A digital learning package. Int. J. Environ. Res. Public Health 2020, 17, 2997. [Google Scholar] [CrossRef] [PubMed]
- Jenkins, L.; Mash, B.; Derese, A. The national portfolio of learning for postgraduate family medicine training in South Africa: Experiences of registrars and supervisors in clinical practice. BMC Med. Educ. 2013, 13, 1–2. [Google Scholar] [CrossRef]
- Sharma, D.; Bhaskar, S. Addressing the COVID-19 burden on medical education and training: The role of telemedicine and tele-education during and beyond the pandemic. Front. Public Health 2020, 8, 838. [Google Scholar] [CrossRef]
- Shufutinsky, A.; DePorres, D.; Long, B.; Sibel, J.R. Shock Leadership Development for the Modern Era of Pandemic Management and Preparedness. Int. J. Organ. Innov. 2020, 13, 1–23. [Google Scholar]
- Shehata, M.H.; Abouzeid, E.; Wasfy, N.F.; Abdelaziz, A.; Wells, R.L.; Ahmed, S.A. Medical education adaptations post COVID-19: An Egyptian reflection. J. Med. Educ. Curric. Dev. 2020, 7, 2382120520951819. [Google Scholar] [CrossRef] [PubMed]
- Frank, J.R.; Danoff, D. The CanMEDS initiative: Implementing an outcomes-based framework of physician competencies. Med. Teach. 2007, 29, 642–647. [Google Scholar] [CrossRef]
- Wood, V.; Flavell, A.; Vanstolk, D.; Bainbridge, L.; Nasmith, L. The road to collaboration: Developing an interprofessional competency framework. J. Interprof. Care 2009, 23, 621–629. [Google Scholar] [CrossRef]
- Blake, T.; Whallett, A. Leadership and the medical registrar: How can organisations support these unsung heroes? Postgrad. Med. J. 2016, 92, 735–740. [Google Scholar] [CrossRef]
- Osman, I.; Hamid, S.; Singaram, V. Efficacy of a brief online mindfulness-based intervention on the psychological well-being of health care professionals and trainees during the COVID-19 pandemic: A mixed method design. Health SA Gesondheid 2021, 26, a1882. [Google Scholar] [CrossRef]
- Singaram, V.S.; Naidoo, K.L.; Singh, S. Self-Directed Learning during the COVID-19 Pandemic: Perspectives of South African Final-Year Health Professions Students. Adv. Med. Educ. Pract. 2022, 13, 1–13. [Google Scholar] [CrossRef]
| Challenges | Strengths and Opportunities |
|---|---|
| Mental distress Resource constraints/system deficiencies Compromised and inadequate training | Resilience and coping strategies Development of competencies
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Singaram, V.S.; Sofika, D.A.N. “Growing as a Stronger Clinician in Adverse Conditions”—A Snapshot of Clinical Training during COVID-19. Educ. Sci. 2022, 12, 156. https://doi.org/10.3390/educsci12030156
Singaram VS, Sofika DAN. “Growing as a Stronger Clinician in Adverse Conditions”—A Snapshot of Clinical Training during COVID-19. Education Sciences. 2022; 12(3):156. https://doi.org/10.3390/educsci12030156
Chicago/Turabian StyleSingaram, Veena S., and Dumisa A. N. Sofika. 2022. "“Growing as a Stronger Clinician in Adverse Conditions”—A Snapshot of Clinical Training during COVID-19" Education Sciences 12, no. 3: 156. https://doi.org/10.3390/educsci12030156
APA StyleSingaram, V. S., & Sofika, D. A. N. (2022). “Growing as a Stronger Clinician in Adverse Conditions”—A Snapshot of Clinical Training during COVID-19. Education Sciences, 12(3), 156. https://doi.org/10.3390/educsci12030156






