1. Introduction
The International Pharmaceutical Federation (FIP) has published the FIP Development Goals [
1], which is a key resource for transforming the pharmacy profession over the next decade globally, regionally, and nationally. They align with FIP’s mission to support global health by enabling the advancement of pharmaceutical practice, sciences, and education and are set to transform pharmacy in alignment with wider global imperatives underpinning the United Nations Sustainable Development Goals (SDGs).
Having a set of global development goals enables identification of commonalities across all areas of the profession, as well as some unique attributes in each area. FIP believes that it is imperative to bring pharmaceutical sciences, pharmacy practice, and the pharmaceutical workforce and education together into one transformative framework for the profession to clearly set out the goals for development for the next decade.
FIP Development Goal 21 (Sustainability in pharmacy) calls on pharmacy as a profession to have policies, regulations, and strategies to ensure the sustainability of pharmacy practice by utilising the pharmaceutical workforce to enhance the pharmacy and services [
1]. To ensure the sustainability of pharmacy practice and to provide health for all, pharmacy as a profession must embrace the digital transformation that has been changing healthcare at a rapid pace.
Digital healthcare has become, more than ever, common practice in hospitals, community pharmacies, and other sites of pharmaceutical care delivery, as well as an integral part of pharmaceutical research and development [
2]. FIP Development Goal 20 (Digital health) commits to having, globally, enablers of digital transformation within the pharmacy workforce and effective processes to facilitate the development of a digitally literate pharmaceutical workforce [
1].
To facilitate the implementation of FIP Development Goal 20, FIP has conducted a global study on digital health in pharmacy education [
2]. The research aims at investigating and describing the readiness, adaptability, and responsiveness of pharmacy education programmes to train the current and future pharmaceutical workforce on digital health and to identify the digital health knowledge and skill gaps of the existing pharmaceutical workforce. In this paper, we provide an overview of the key findings and provide a policy perspective on pharmacy education’s curricula and preparedness for a sustainable pharmacy profession.
2. Digital Health and Pharmacy Education
We all acknowledge that global health has improved dramatically in recent decades. However, the current model of care delivery is consistently and increasingly challenged, largely by ageing populations and fiscal constraints on government spending. Maintaining the status quo is not an option. Few industries have the potential to be changed so profoundly by digital technology as healthcare [
3], providing pharmacists and pharmaceutical sciences across the world with new opportunities to provide and improve pharmaceutical care. Implementation of new technologies in daily pharmaceutical practice, however, is still relatively limited even though current times require pharmacists to find alternative ways of providing pharmaceutical care [
2].
Implementation largely depends on the willingness and ability to use these tools by pharmacists. Keeping pace with those advancements that should be adopted and adapted to improve health can be challenging. Education and training of students and practitioners is a continuous process so that they remain up to date aligned with the developments in health technologies to assure they optimise the benefits of digital health. Pharmacy schools can play an important role in accelerating uptake of digital health by educating the future generation of pharmacists. Pharmacy schools should teach pharmacy students not only about the technical aspects of these technologies but also how to integrate them into pharmaceutical care.
There are multiple challenges to the implementation of digital health education [
4]. The following are highlighted areas to be evaluated and addressed before widespread digital health education in the healthcare professions can be initiated [
2]:
Lack of standards: there are currently little to no best practices in terms of what digital health education is required for healthcare professionals.
Lack of trained academics: one of the most considerable limitations is that there is a shortage of academics in the healthcare environment with both experience and knowledge to propagate digital health education at large [
5]. While interest is building, like the issue around standardisation, it is challenging to determine to what extent an academic is sufficiently up to date and trained to develop that knowledge in others.
Partnerships: healthcare education institutions cannot teach digital health topics alone. By its nature, digital health is an interdisciplinary endeavour spanning multiple market sectors and requires expertise in fields of science and backgrounds that are not traditionally thought of being directly related to medicine. This includes issues such as regulatory oversight and validation of the technology in health but also implications of behavioural sciences, user interface/user experience design, mathematical insight on artificial intelligence (AI)/machine learning construction, gamification design, and more.
Materials and samples: teaching digital health involves other issues regarding the technological needs for hands-on instruction. Similar issues now challenge healthcare academics to integrate electronic health records constructs into their teaching and course work to mimic current practice; identifying and then utilizing digital health technologies as teaching material will prove a logistical hurdle [
6].
Laboratory spaces: Lastly, in relation to the acquisition of devices and software for teaching just mentioned, the creation of a digital health space to house relevant technologies to be utilised may be an issue.
3. FIP’s Research on Digital Health in Pharmacy Education and Findings
In responding to the evolution of digital health utilisation in health care, reviewing how pharmacy education has integrated digital health in its current offering is imperative. It includes how the content and delivery of the course and training prepare the pharmaceutical workforce and students to leverage digital health in their practice. There is, however, a dearth of literature on the availability of digital health courses in pharmacy schools. Additionally, there is limited evidence on the current states of skills and knowledge that the pharmaceutical workforce has in utilising digital health in their practice and their needs in this area. Therefore, FIP conducted a study to explore how the current and future pharmaceutical workforce has been educated and trained in digital health. Two aims were set: the first aim was to investigate and describe the readiness and responsiveness of education programmes to train the current and future pharmaceutical workforce on digital health from the perspective of pharmacy schools or academics; the second was to identify the knowledge and skill gaps of the students and the pharmaceutical workforce on digital health as well as their needs in digital health education.
3.1. Methodology
An online questionnaire using survey software (QuestionPro) was developed to gather responses [
2]. The questions were derived from a wide team of experts, presenting expertise in practice and education. The experts consisted of 19 FIP members from 11 countries, including pharmacy students, pharmacy practitioners, and experts from academic institutions. They developed the questionnaire based on the projects’ aim, utilising survey themes found in the literature. The questionnaire included a combination of open-ended and multiple-choice questions. Four target audiences were approached, namely academic institutions (pharmacy schools), individual faculty members (academics), pharmacy students, and practitioners (pharmacists). The questionnaire’s wording was adapted according to each target audience. The survey was available in Arabic, Brazilian Portuguese, Chinese, English, French, Russian, Spanish, and Turkish.
The survey was distributed from 17 August 2020 to 1 October 2020 using electronic mailing lists and social media to the FIP network and collaborators. The data captured in other languages were translated into English by bilingual volunteers and compiled before the analysis [
2]. A survey analysis plan was developed to guide the analysis process based on the survey’s themes. The cleaned data were analysed descriptively using Microsoft Excel. The chi-square test and the Fisher’s exact test were used to assess the association between categorical variables within the dataset. Statistical analysis was performed using SPSS and SAS. The findings were analysed and described based on three categories of respondents: academia (combining institutions and faculty members), students, and practitioners. The methodology has been described in more detail in the FIP Digital Health in Pharmacy Education report [
2].
3.2. Results
In total, 1060 respondents from 91 countries completed this survey. The breakdown of the respondents’ distribution can be seen in
Table 1.
A total of 260 responses were received from academic institutions across 60 countries; the majority of the participants (60%) were faculty members (associate professor, assistant professor) (
Table 1). A number of participants (22%) were research assistants and students. Few of the respondents (17%) were from leadership positions, such as head of the department or head of the institution.
When surveying practising pharmacists, 526 responses were received from practitioners across 70 countries (
Table 1). The median years of experience was 15 (IQR: 6–26) years with the most common professional backgrounds among respondents being community pharmacy (298/526; 57%), hospital pharmacy (85/526; 16%), and social and administrative pharmacy (34/256; 6%).
A total of 274 students from 39 countries completed the survey (
Table 1). The majority of surveyed students (63%) were female and in the BPharm (Bachelor of Pharmacy) level (75%).
3.2.1. Faculty Perspective
A total of 57% of respondents stated that digital health was not taught in their university. Where digital health was included in the curriculum, it was either integrated into other courses (34%) or offered as a standalone course (5%). The extent of covering the digital health concept in pharmacy schools varied from around one to two lectures over an academic year (35%) to more than three lectures over an academic year (27%) or even a complete module or course (15%). In the majority of the pharmacy schools, digital health was offered in a classroom setting (63%), while in some it was offered in a virtual setting (43%). In most of the pharmacy schools, digital health was taught by lecturers from the pharmacy department (71%) while in a some of the schools it was taught by guest speakers from the digital health industry (24%) and visiting lecturers (13%). Digital health was taught to pharmacy students as a single group (71%) in the majority of the schools that provided education on digital health. In contrast, some of the schools (24%) provided digital health in liaison with other healthcare students (e.g., medicine, nursing) (
Table 2).
Nearly half of the respondents (48%) agreed their students were equipped with the competencies to deliver digital health services after graduation, and more than half (52%) agreed their school was able to readily identify and include new digital health skills/competencies in the curriculum as they emerge in practice.
The most common tool/service covered in pharmacy schools stated by respondents was mobile applications (63%), while the least common tool was bots (7%). The majority of the respondents who were from schools that did not offer digital health courses were interested in teaching about online (remote) patient counselling (39%) followed by mobile applications (37%).
The most common concepts included ethics and compliance (63%), followed by data privacy and security (53%). The least common concept included was cybersecurity (12%). Nearly half of the respondents from schools which did not provide digital health course were interested in teaching concepts, such as innovation and creativity (49%) followed by evidence-based digital medicine (41%).
According to the respondents, the infrastructures most commonly used for digital health education included e-learning (60%) and active learning sessions (54%), while infrastructures such as living lab (6%) and hackathon (6%) were the least commonly used. Among the respondents from schools which did not provide digital health courses, access to clinical care digital platforms (67%) was the most common infrastructure that was thought to be necessary for digital health education.
More than half of respondents mentioned that patient-centred digital health (58%) followed by knowledge of digital health tools (55%) were the most common competencies needed for digital health, whereas competency such as service design (19%) and design thinking (19%) were the least common ones. Patient-centred digital health (49%) and knowledge of digital health tools (46%) were the most common competencies that the respondents from schools which did not provide digital health course were interested in teaching.
Half of the respondents mentioned that the lack of experts (50%) followed by lack of resources (40%) were the most common challenges related to digital health. Most respondents mentioned that advancing pharmacy outcomes (86%) was the most common desired consequence of including digital health in the curriculum of pharmacy schools, followed by digital health applied in practice settings (71%). There was no difference in this response between schools which offered digital health education and those which did not.
Digital health was included in the general strategic plan in some of the schools. All the 148 respondents (100%) who indicated their pharmacy schools did not provide digital health education were interested in providing digital health education in the future, especially more in online/remote (patient) counselling, mobile applications, and telemedicine/telehealth/virtual care. When respondents were asked about the infrastructure that they would like to have in their pharmacy schools, some themes arose, including: access to digital platforms/software which include analytical software; a laboratory to test digital health concepts and tools; and e-learning infrastructure.
A total of 23% of respondents mentioned receiving support from national/regional pharmacy organisations for the development of digital health courses or lectures in pharmacy school. One hundred and fifteen (77%) respondents expressed that support was needed from FIP. The major support needed was guidance, training, and resources.
3.2.2. Practitioner Perspective
Only one in four practitioners reported receiving digital health education, either within pharmacy school or after pharmacy school as continuous education. Those who received digital health in pharmacy school were 2.5 times more likely to report also receiving continuous education in digital health (X2 (1, N = 526) = 17.46, p < 0.0001).
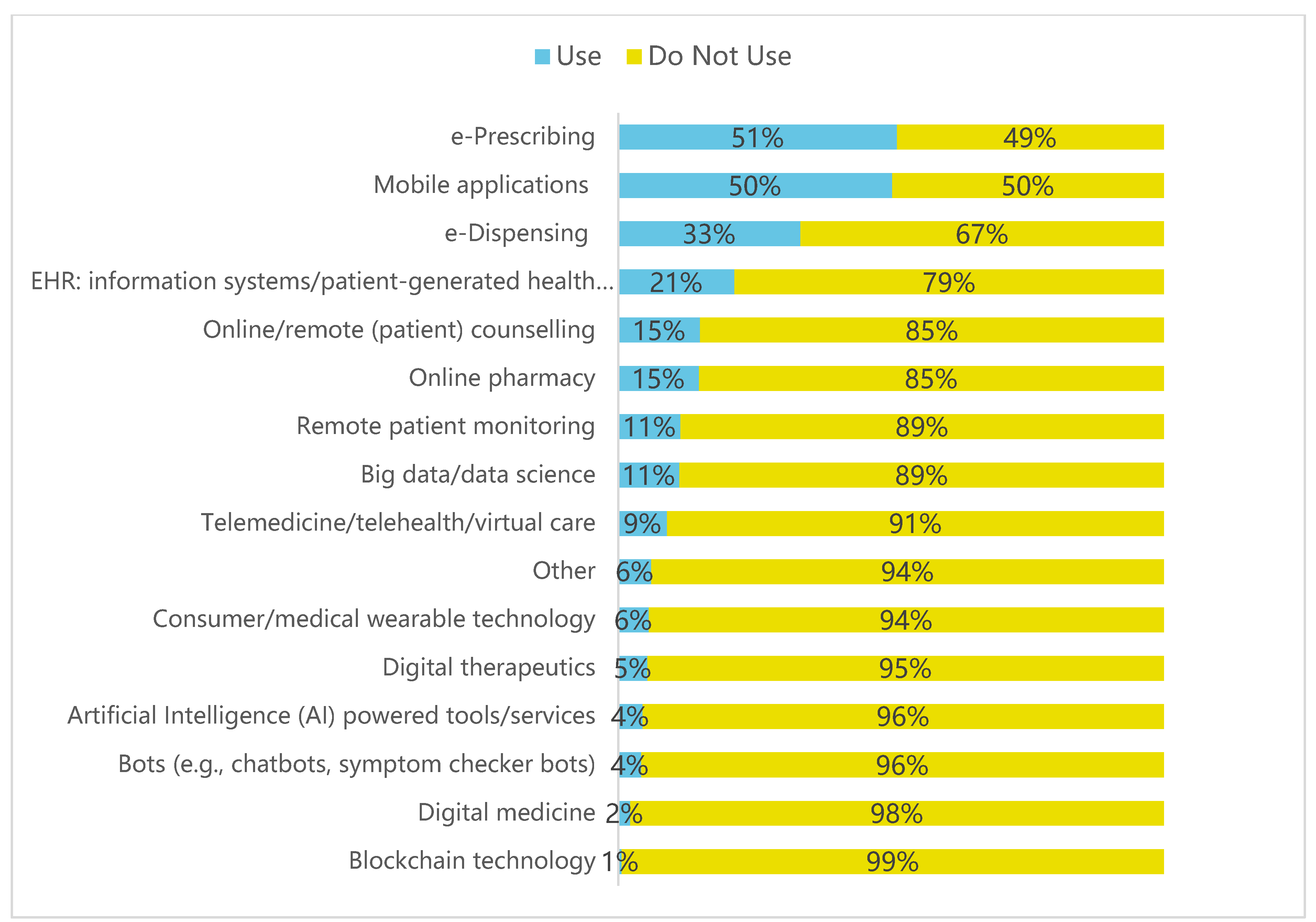
Over half of practitioners (61%) who responded stated they use digital health tools on a daily basis. However, there was low prevalence of use of emerging digital health technologies (
Figure 1). When respondents were asked about 15 different digital health tools, 77% (342/446) reported using only three different types of tools, at most, in their practice. Among those that reported using digital health tools, the most commonly utilised were e-prescribing (51%), mobile applications (50%), and e-dispensing (33%), with only a small fraction employing emerging tools such as digital therapeutics (5%) or AI (4%) in their practices (
Figure 1). Most practitioners cited time saving (311/446; 70%) as a primary benefit of digital health and were more likely to list this as a benefit over others, such as improved outcomes of medicine use (187/446; 42%).
When respondents were asked what support would be most helpful to them, a key need cited by practitioners was guidance on how to apply technology to solve existing clinical problems and implement digital health tools in practice. The top tools that practitioners stated they want to learn more about are summarised in
Figure 2 and include mobile applications (151/446; 34%), electronic health records (144/446; 32%), and telemedicine/virtual care (138/446; 31%). Other tools were less frequently cited, such as digital medicine (35/446; 8%) or consumer wearable technology (29/446; 7%) (
Figure 2). Overall, minimal practitioners (15%) reported receiving support and guidance from pharmacy associations in the use of digital health. Practitioners expressed the need for greater access to digital health tools, increased digital health education, and more guidance on how to apply digital health technologies in practice. The greatest challenges in digital health cited by practitioners were lack of enabling policies and guidance (51%) and technical limitations, such as lack of interoperability or access to data (54%).
3.2.3. Students’ Perspectives
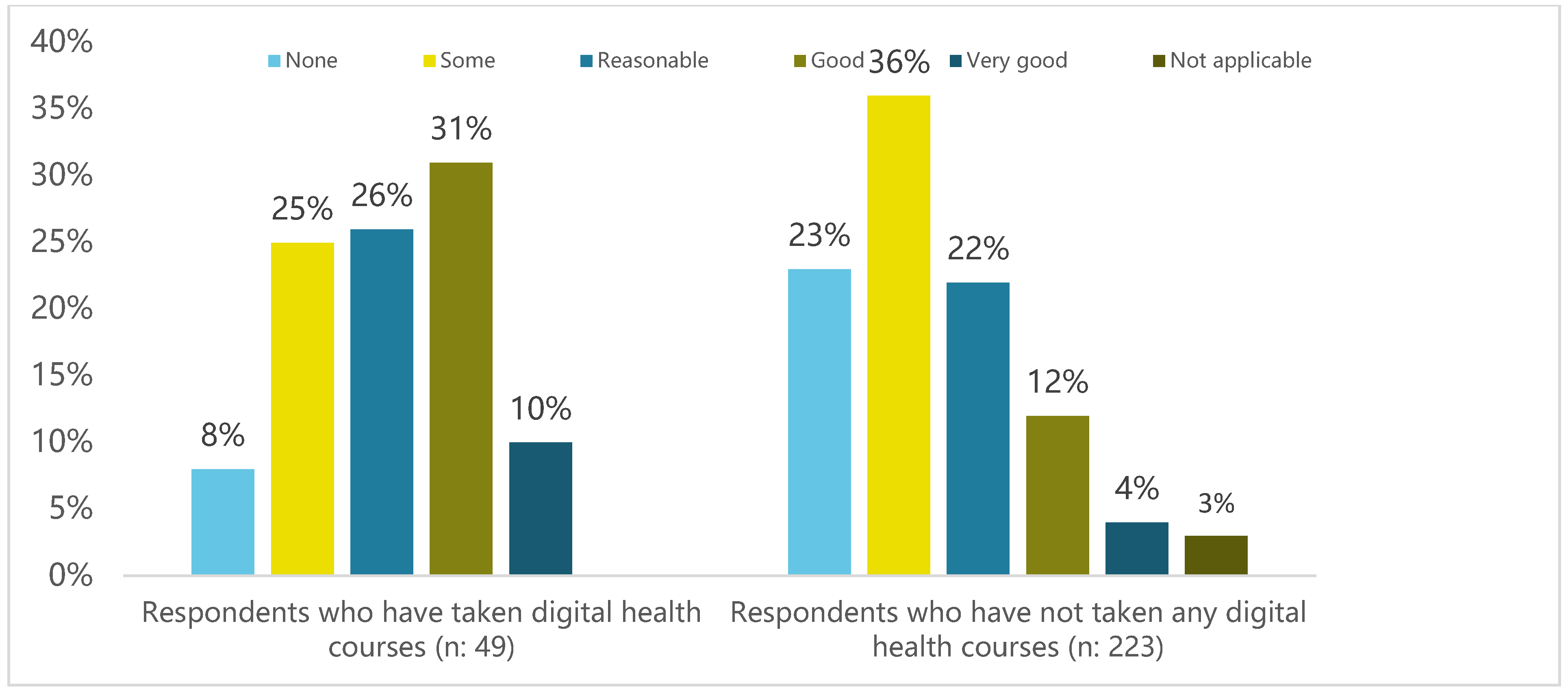
Only one-10th of respondents had received digital health education in their schools. Likewise, approximately one-10th of respondents learned digital health from online courses/webinars offered by professional organisations or some digital education platform. The study found that students who took a digital health course have better knowledge than students who did not take a digital health course (Fisher’s Exact Test, n: 272,
p = 0.001) (
Figure 3). When asked about how they defined digital health, most surveyed students defined the concept as applying digital tools or technology to advance healthcare. Out of 15 digital health tools/services categories stated in the survey, students expressed interest in learning more about online pharmacy (42%), mobile applications (35%), and telemedicine (29%) in their digital health courses; these tools had also been covered in their pharmacy schools. On the other hand, while some students expected to learn more about AI (14%), bots (10%), and blockchain technology (1%), these tools were not covered in their courses. Out of 11 categories of infrastructures in digital health education stated in the survey, the top three provided by pharmacy schools were e-learning (50%), active learning sessions (36%), and access to digital care clinical platforms (27%). Similarly, surveyed students who had not taken digital health courses identified access to digital care clinical platforms (60%), a laboratory to test digital health (59%), and active learning sessions (43%) as their top three needs of digital health infrastructure.
The majority of students received no support on employment opportunities in digital health from their schools. Similarly, only a minority of respondents received support from their national/regional students associations. Particularly, students expressed their interest in building their knowledge, skills, and applications in digital health. They wish to learn more about digital biomarkers, fields/applications of digital health, and patient information security. They also expressed interest in applying AI in industrial pharmacy settings and digital health in pharmaceutical care in community pharmacy settings.
3.3. Discussion
The evolving roles of pharmacists within the healthcare team demands utilisation of a range of digital technologies and requires digital literacy skills among pharmacists. There is a lack of research regarding digital health skills and related training among pharmacy students and pharmacists. To date, a limited number of studies have been conducted to explore the status of inclusion of digital health training in pharmacy schools and to assess the skills and competencies of pharmacists in digital health. Very limited research, mostly from countries such as the United States, Canada and the United Kingdom, was found related to digital health in the pharmacy curriculum [
7,
8,
9], while no studies were found which explored the status of digital health in the pharmacy curriculum at a global level.
The results of this study clearly demonstrate that most pharmacy schools globally do not offer any digital health education at present. About half of respondents stated that digital health was not taught in their universities. This finding was quite similar to the findings from a study conducted in United States, which showed pharmacy informatics education was prevalent in only 36% of pharmacy schools [
10]. In the survey, it was observed that students expressed an interest in learning more about online pharmacy (42%), mobile applications (35%), and telemedicine (29%) in their digital health courses. In a survey conducted in Canada, 77% of participants ranked medical database and internet searching as priority areas [
11]. This higher percentage might be a result of the Canadian study being conducted many years ago when there was only a limited use of various digital technologies. All the respondents who indicated their pharmacy schools did not provide digital health education in our study were interested in providing digital health education in future.
The majority of students received no support on employment opportunities in digital health from their schools. Similarly, only a minority of respondents received support from their national/regional students associations. This finding reflects opportunities for students’ organisations, such as the International Pharmaceutical Students’ Federation, to develop digital health support for their members. Particularly, students expressed their interest in building their knowledge, skills, and applications in digital health. The study found that those who received digital health education in pharmacy school were 2.5 times more likely to report also receiving continuous education in digital health, which suggests early exposure may be an important factor to increase the desire to seek further education later.
Over half of practitioners who responded stated that they use digital health tools on a daily basis, and they wanted to learn more, especially about mobile applications, electronic health records, and telemedicine/virtual care. Other tools were less frequently cited, such as digital medicine or consumer wearable technology, which may indicate lack of awareness of the purpose and use of these tools. This was similar to a finding from a study in the UK where there was overwhelming evidence that pharmacy staff at all levels, ages, and stages could not recollect information technology training as part of their pharmacy education, yet said that it was central to their everyday practice [
9].
Various findings from the study have highlighted the importance of enhancing the preparedness and responsiveness to digital health through education across the world. Only when pharmacists clearly understand the fundamentals of digital health technologies and know how to integrate them into their clinical practices can pharmacists and their patients fully benefit from the many potential benefits that digital health offers. It is important to design a digital health curriculum targeting competencies to provide the necessary knowledge and skills to help students practise digital health in their professional careers.
4. Enhancing Pharmacy Education in Preparedness for and to Responsiveness to Digital Health: Ways Forward
Building on the results of the survey, several areas for moving forward have been identified at the international level involving different stakeholder groups, i.e., academic institutions, educators, and students. These are described in more detail below.
4.1. Support of Educators: Train the Teachers
Key findings emanating from FIP’s global report on digital health in pharmacy education [
2] with regard to preparedness and responsiveness of academia are: (1) identification of competencies in digital health that are established in a needs-based pharmacy and pharmaceutical sciences education, which meets existing and emerging requirements relevant to a broad dimension of pharmaceutical scenarios; and (2) a positive responsiveness to prepare students for digital health. Through FIP’s Academic Pharmacy Section (its network of individual academics and educators in pharmacy), FIP is planning strategies to support pharmacy educators and mentors to plan and develop teaching experiences that integrate digital health in pharmacy and pharmaceutical sciences programmes. From FIP’s report, the challenges cited by educators in incorporating digital health in the curriculum included lack of experience and lack of guidance on how to approach such an innovation. A “Masterclass on Digital Health in Pharmacy Education” is currently being developed by FIP’s Academic Pharmacy Section within the context of the “One FIP” vision – which is a vision bringing together pharmacy practice, pharmaceutical sciences and pharmacy education under one roof. The One FIP vision ensures that the masterclass will address a broad scope of topics, ranging from direct patient-centred services to regulation, policy making, and drug research. A training package highlighting learning experiences that support the development of competencies for the digital age is being developed. The masterclass, which will be delivered online, is directed towards empowering pharmacy educators and colleagues involved in the training of pharmacists and pharmaceutical scientists to identify effective learning models that prepare graduates for the provision of a patient-centred digital pharmaceutical care that is driven by knowledge and fluency in the use of digital health tools.
4.2. Digital Health Initiatives from Pharmacy Schools: Sharing Best Practices
One of the objectives of the FIP report was to describe good practices on course descriptions, examples of assignments, and learning activities on digital health from pharmacy and pharmaceutical sciences schools. Through the survey, institutions and faculty members were asked to indicate their interest in sharing their experiences in their approach and innovations to digital health education by submitting a case study. Sixteen case studies were included in the report, highlighting innovative initiatives on the development of digital health education and skills. The various educational initiatives from pharmacy schools may help to build digital health competencies; to explore good practices on course descriptions, assignments, and learning activities on digital health; and to identify steps to develop similar initiatives in digital health at other institutions. These case studies can serve other pharmacy educators and institutions as they develop similar initiatives in their curricula and teaching methods to prepare current and future generations of the pharmaceutical workforce to become digitally enabled.
4.3. Developing an FIP Global Curriculum and Training Resources Toolkit for Digital Health Education
The FIP report indicates the global need for educational resources and standards for digital health in pharmacy education. As a way forward, building on the findings of the report, FIP is going to design and develop a global curriculum and training resources toolkit for digital health in initial pharmacy education that includes baseline digital health literacy and the integration of digital health with professional practice. FIP’s global curriculum and training resources toolkit will promote the mindsets and behaviours needed for the digital reform in education, as there might be cultural, regulatory, or systematic barriers preventing its adoption. The developed curriculum and training resources will provide for a broader perspective and include areas such as governance, ethics, and security to provide safe ways of working with new technologies.
4.4. Way Forward for Pharmacy Students by the International Pharmaceutical Students’ Federation (IPSF)
Digital health education is vital for equipping students with empowering skills, such as interprofessional collaboration, knowledge about digital health tools, and becoming familiarised with health systems and entrepreneurship. The IPSF, the leading international advocacy organisation for pharmacy and pharmaceutical sciences students and recent graduates, is working on different projects and activities to emphasise the importance of digital health literacy through webinars, professional development programmes, and workshops. Each region has led its own initiatives. The IPSF European Regional Office hosted its webinar entitled “The use of Digital Health Technologies and Data Collection during the COVID-19 Pandemic”, stressing the importance of digital health technologies in improving access to healthcare services and providing students with an overview of the digital health system in Europe. The Asia Pacific Regional Office included digital health as one of its Leaders in Training programme’s topics that aims to emphasise the possibilities students and future pharmacists have to foster digital health transformation into practices. The Eastern Mediterranean Regional Office is working on a World Health Organization Assembly simulation programme where the main topic would be “Strategy roadmap to digital health implementation”. The African Regional Office plans on having its policy session, which is a platform for dialogue among members, focused on digital health.
The IPSF is advocating for stronger curricular activities and extracurricular projects related to digital health practices and education in pharmacy schools. In addition, in collaboration with FIP, the IPSF is hoping to support developing programmes dedicated to closing the gap between pharmacy education and digital health.
5. Conclusions
FIP’s ‘’Digital health in pharmacy education report’’ is the first of its kind to investigate the readiness and responsiveness of pharmacy education and to identify knowledge and skills gaps of the pharmaceutical workforce. While the report focused on education and skills, the findings provide a broader view on the status of digital health in pharmacy and pharmaceutical sciences. We believe the report will catalyse further research and developments in the area to increase the adoption of digital health by the pharmaceutical workforce.
The global study strongly advocates that all students in pharmacy and pharmaceutical sciences need to graduate with basic knowledge and skills for patient-centred digital health. In order to upskill and train the existing workforce with digital health skills, continuous professional development and specialisation are critically important. To date, there has been insufficient attention given to workforce development for implementing new systems of digital health delivery. Employers and universities can unlock the potential of the pharmaceutical workforce through education strategies. In order to mitigate the variation of the readiness and responsiveness of pharmacy education and training, collaboration across pharmacy schools could be a way to speed up the adoption of digital health education.
Professional organisations should support the pharmaceutical workforce by providing access to digital health tools, investing in digital health education, and developing guidance on how to apply digital health technologies in practice. A professionally driven advocacy effort can ensure integration of digital health into pharmacy education and support the inclusion of digital health in educational and accreditation standards.
Building on the findings of the report, FIP will continue to identify key priorities for action globally and regionally, alongside areas that need further investigation and understanding, such as supporting the existing workforce or addressing barriers to the implementation of digital health education.
The future of pharmacy and pharmaceutical sciences is exciting to consider and it will be digitally enabled. Additionally, a digitally enabled and agile pharmaceutical workforce will capitalise on the benefits of digital health to serve the higher purpose of providing good health and wellbeing for all, leaving no one behind. Therefore, pharmacy and pharmaceutical sciences education should act now.
Author Contributions
A.K.M.-T., S.M., N.U., B.K., J.A.G., W.Y., L.M.A., G.G., and K.B. have contributed to the global study and this manuscript in various ways, such as conceptualisation, methodology, software, validation, formal analysis, and writing. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the International Pharmaceutical Federation (FIP). No external funds were received.
Institutional Review Board Statement
Ethical review and approval were waived for this study because according to Dutch law, no approval by a medical ethics committee was necessary. This was because the work was not a research study but a survey of FIP members and member organisations. Information was not attributed to individuals and participation in the study was voluntary. Access to the data with identifiable information was restricted to the research team who was directly involved in this study.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are not publicly available due to data privacy laws.
Acknowledgments
FIP Chief Executive Officer Catherine Duggan has reviewed the final draft of this paper. FIP acknowledges the contribution of all authors, reviewers, and translators of the report and the respondents of the global study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- International Pharmaceutical Federation (FIP). The Fip Development Goals: Transforming Global Pharmacy; International Pharmaceutical Federation: The Hague, The Netherlands, 2020. [Google Scholar]
- International Pharmaceutical Federation (FIP). FIP Digital Health in Pharmacy Education; International Pharmaceutical Federation: The Hague, The Netherlands, 2021. [Google Scholar]
- World Economic Forum. Healthcare: Building a Digital Healthcare System. Available online: https://reports.weforum.org/digital-transformation/healthcare-building-a-digital-healthcaresystem/ (accessed on 30 October 2020).
- Aungst, T.D.; Patel, R. Integrating digital health into the curriculum—Considerations on the current landscape and future developments. J. Med. Educ. Curric. Dev. 2020, 7. [Google Scholar] [CrossRef] [PubMed]
- Fernando, J.; Lindley, J. Lessons learned from piloting mHealth informatics practice curriculum into a medical elective. J. Am. Med. Inform. Assoc. 2018, 25, 380–384. [Google Scholar] [CrossRef] [PubMed]
- Haghi, M.; Thurow, K.; Stoll, R. Wearable devices in medical internet of things: Scientific research and commercially available devices. Healthc. Inform. Res. 2017, 23, 4–15. [Google Scholar] [CrossRef] [PubMed]
- Rodis, J.; Aungst, T.; Brown, N.; Cui, Y.; Tam, L. Enhancing Pharmacy Student Learning and Perceptions of Medical Apps. JMIR Mhealth Uhealth 2016, 4, e55. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Min, J. Exploring Canadian pharmacy students’ e-health literacy: A mixed method study. Pharm. Pract. 2020, 18, 1747. [Google Scholar] [CrossRef] [PubMed]
- MacLure, K.; Stewart, D. A qualitative case study of ehealth and digital literacy experiences of pharmacy staff. Res. Soc. Adm. Pharm. 2018, 14, 555–563. Available online: https://www.sciencedirect.com/science/article/pii/S1551741117301882 (accessed on 3 June 2021). [CrossRef] [PubMed]
- Fox, B.I.; Karcher, R.B.; Flynn, A.; Mitchell, S. Pharmacy informatics syllabi in doctor of pharmacy programs in the US. Am. J. Pharm. Educ. 2008, 72, 89. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Balen, R.M.; Jewesson, P.J. Pharmacist computer skills and needs assessment survey. J. Med. Internet Res. 2004, 6, e11. [Google Scholar] [CrossRef] [PubMed]
| Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).