Abstract
In this paper, we utilize the 2019/20 Uganda National Household Survey data to answer three related questions: (i) To what extent did out-of-pocket payments (OOPs) for health care services exceed the threshold for household financial catastrophe amidst COVID-19? (ii) What is the impoverishing effect of OOPs for health care services on household welfare? (iii) What are the socioeconomic and demographic determinants of OOPs for health care services in Uganda? Leveraging three health expenditure thresholds (10%, 25%, and 40%), we run a Tobit model for “left-censored” health expenditures and quantile regressions, and we find that among households which incur any form of health care expense, 37.7%, 33.6%, and 28.7% spend more than 10%, 25%, and 40% of their non-food expenditures on health care, respectively. Their average OOP budget share exceeds the respective thresholds by 82.9, 78.0, and 75.8 percentage points. While, on average, household expenditures on medicine increased amidst the COVID-19 pandemic, expenditures on consultations, transport, traditional doctors’ medicines, and other unbroken hospital charges were reduced during the same period. We find that the comparatively low incidence and intensity of catastrophic health expenditures (CHEs) in the pandemic period was not necessarily due to low household health spending, but due to foregone and substituted care. Precisely, considering the entire weighted sample, about 22% of Ugandans did not seek medical care during the pandemic due to a lack of funds, compared to 18.6% in the pre-pandemic period. More Ugandans substituted medical care from health facilities with herbs and home remedies. We further find that a 10% increase in OOPs reduces household food consumption expenditures by 2.6%. This modality of health care financing, where households incur CHEs, keeps people in chronic poverty.
JEL Classification:
I10; I11; I12
1. Introduction
Health expenditure shocks are one of the most peculiar income shocks and the main reason why many individuals and households fall into poverty (Atake, 2018). A catastrophic health expenditure (CHE) refers to any expenditure for medical treatment that poses a threat to a household’s financial ability to maintain its subsistence needs (Wagstaff & Doorslaer, 2003; Uganda Bureau of Statistics, 2021). For instance, a total household health expenditure of 10 percent or more of a household’s total expenditures is often considered catastrophic. Although the health system in Uganda continues to be financed by a multiplicity of stakeholders, including the government, private sector, households, and health development partners [HDPs] (Ministry of Health, 2021), households still contribute the biggest portion of health care financing through OOPs. Therefore, increasing the financial risk protection for households against impoverishment due to CHEs is critical.
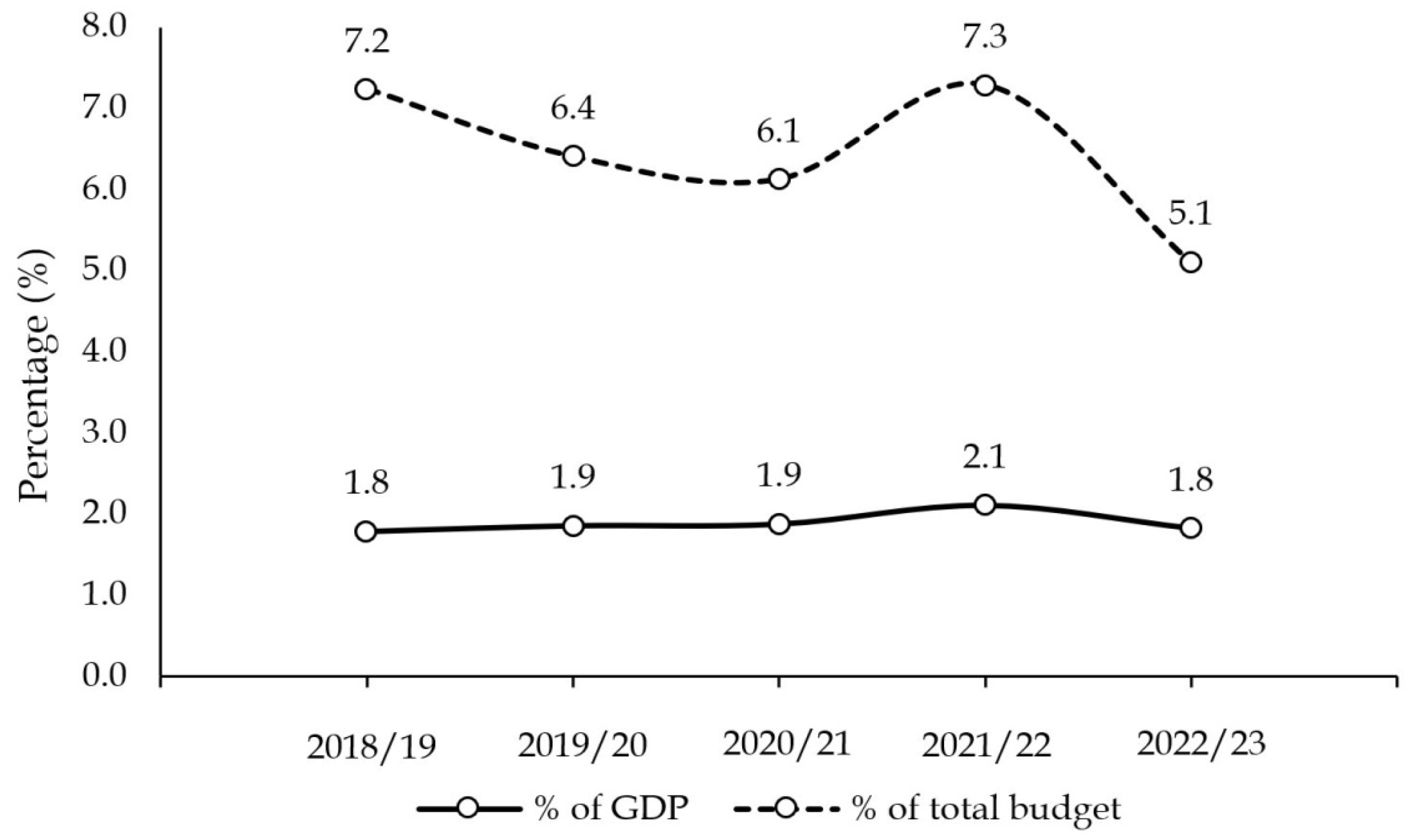
Uganda has consistently fallen short in living up to the 2001 Abuja declaration expectations of allocating at least 15% of its national budget each year to improving the health care system. The size of the health sector budget has been less than half of the declaration’s requirement for the past five years (see Figure 1). More precisely, the health sector budget as a share of the total budget and GDP has averaged 6.4% and 1.9%, respectively, for the financial years 2018/19 to 2022/23. Although the external funds allocated to the sector have fluctuated over the years, the development component of the health budget has largely been funded by health development partners (HDPs). For instance, for the 2020/21 financial year, the share of the government’s contribution towards the entire sector was 57%, of which 53% was allocated to recurrent expenditures and only 4% to development expenditures. More precisely, 93% of the government’s contribution to the health budget was allocated to recurrent expenditures, whereas the remaining 7% went to development expenditures (Ministry of Health, 2021). This re-affirms that the development component of the health budget is almost entirely externally funded. This overreliance on external funding, coupled with the absence of a national health insurance scheme, further exacerbates households’ health-financing burden1 (Mpuuga et al., 2020).
Figure 1.
Uganda’s health sector budget as a share of the total budget and GDP. Source: data from the Annual Health Sector Performance Reports and National Budget Framework Papers (2018/19–2022/23).
This study addresses three related questions. Firstly, to what extent did OOPs for health care services exceed the threshold for household financial catastrophe amidst COVID-19? Secondly, what is the impoverishing effect of OOPs on household welfare? Thirdly, what are the socioeconomic and demographic determinants of OOPs in Uganda? We take advantage of the most recent Uganda National Household Survey (UNHS)—UNHS 2019/20—to answer the posed questions. This is not only the most recent UNHS, but also the first ever to collect information on the pre- and COVID-19 period. We use three health expenditure thresholds (10%, 25%, and 40%), as adopted by Wagstaff and Doorslaer (2003), Ssewanyana and Kasirye (2020), and the World Health Organization (2020), respectively.
First, we use each threshold separately to estimate the overall incidence (headcount) and intensity (poverty gap) of CHEs among households. We find that among households that incur any form of health care expense, 37.7%, 33.6%, and 28.7% of them spend more than 10%, 25%, and 40% of their non-food expenditures on health care, respectively. In terms of the intensity of CHEs, we find that the mean positive poverty gap is worryingly high for all three thresholds, i.e., 82.9%, 78.0%, and 75.8%. Specifically, among households that spend more than 10%, 25%, and 40% of their non-food expenditures on out-of-pocket health payments, their average out-of-pocket budget share exceeds the respective thresholds by 82.9, 78.0, and 75.8 percentage points.
Second, we estimate the incidence and intensity of CHEs among households in the pre-COVID-19 and COVID-19 periods. The main reason for the comparative analysis is the rise in the number of poor Ugandans, from 8 million in 2016/17 to 8.3 million in 2019/20 (Uganda Bureau of Statistics, 2021); yet, it is still not clear how much of this impoverishment can be attributed to health expenditure shocks amidst COVID-19. We find that whereas, on average, household expenditures on medicines increased amidst the COVID-19 pandemic, expenditures on consultation fees, transport to and from health facilities, traditional doctors, and other unbroken hospital charges were reduced during the pandemic period. Overall, the incidence and intensity of CHEs were less severe during the COVID-19 pandemic compared to the pre-pandemic period. We then investigate the health care-seeking behavior of Ugandans in both periods to understand why the incidence and intensity of CHEs were lower during the pandemic. We find that during the COVID-19 pandemic period, 21.5% of Ugandans did not seek medical care because they lacked the money or funds to do so, compared to only 18.6% who did not seek care for the same reason in the pre-pandemic period. This leads us to argue that when the pandemic ravaged the economy, many Ugandans could not afford to pay for medical care costs and thus decided to forego it. Relatedly, during the pandemic period, 12.0% of Ugandans did not seek medical care because they used herbs or home remedies, which was an increase from the 11.4% that substituted facility care with home remedies before the pandemic. Thus, the comparatively low incidence and intensity of CHEs in the pandemic period is not necessarily due to low household health expenditures, but due to foregone and substituted care.
Third, we run a Tobit regression for the “left-censored” health expenditures sample and quantile regressions for the 25th, 50th, and 75th quantiles, in addition to a baseline ordinary least squares regression. We concentrate on the peculiarities among the different quantiles, since the direction of effect presented using the Tobit model is the same compared to the three quantile regressions. Comparisons of the magnitudes of, for example, the OLS and Tobit estimates are less informative (Wooldridge, 2010). We find that households with members above 65 years of age and those with a member with a non-communicable disease, such as diabetes, hypertension, heart disease, and cancer, face significantly higher OOP health payments compared to their counterparts. OOPs for health care increase as the distance in kilometers to a health facility increases. This speaks to the need to bring health facilities closer to communities to cut down on catastrophic health expenses. Relatedly, visiting a public rather than a private health facility reduces OOPs for health care by 52 percent. We note that the effect of a reduction in health expenses shrinks as we move into higher expenditure quantiles. This implies that households in the 25th and 50th quantiles benefit more from the services of public facilities. Such households tend to be poor with some in the middle class. The low effect of public facilities services on the 75th quantile of households is informative for policy makers, suggesting that they should subsidize public health services targeting poor households since they exhibit the biggest reduction in OOPs.
Lastly, we run a two-stage least squares log–log model to examine the effect of out-of-pocket health payments on household food consumption expenditures. We find that a 10% increase in out-of-pocket health payments for health care reduces household food consumption expenditures by 2.6%. Our paper contributes to the literature that elucidates the link between household health care expenditure shocks and household poverty, cognizant of the ravaging pandemic.
The rest of the paper is organized as follows. Section 2 presents a survey of the literature, and Section 3 presents a detailed description of the data, as well as the theoretical and empirical strategies. The results, discussion, and robustness checks are presented in Section 4. Finally, Section 5 concludes this paper and highlights its key policy implications.
2. Health Care Expenditure and Household Welfare
Health is both a direct component of human well-being and a form of human capital that raises an individual’s capabilities (Bloom & Canning, 2003). This justifies an increased investment in health mainly because of the large effect that improved health has on household incomes and broad economic growth, which makes it instrumental in poverty eradication. Therefore, there are clear links between economic growth, poverty, and health (Gupta & Mitra, 2004). Although growth tends to reduce poverty, significant improvements in health status are necessary for poverty to decrease. Notably, there is a two-way relationship between economic growth and health status, implying that better health enhances growth by improving household productivity, which further enhances human capital formation.
Poor health is a top cause of household impoverishment in low- and middle-income countries (Alam & Mahal, 2014), because health shocks cause significant reductions in the labor supply. Due to health expenditure shocks, households are often unable to fully smooth income. Although health financing reforms have received much attention in developing countries like Uganda2, out-of-pocket payments remain substantial (Ataguba, 2012). For instance, Ssewanyana and Kasirye (2020) found that Uganda has the second highest rate of catastrophic expenditures among the five countries of Ethiopia, Malawi, Nigeria, Tanzania, and Uganda. It is important to note that it is mainly the relatively poor individuals/households that make catastrophic payments. Although OOPs for health care affect households differently, it is often the poor that are most hit since they are also often excluded from the available safety nets, specifically health insurance (Mpuuga & Eshete, 2022).
The lack of health insurance coverage has a significant effect by increasing the incidence of welfare loss from health shocks (Atake, 2018). For poor households, a reduction in user fees for health care at the point of service or an expansion of health insurance would mitigate their vulnerability to poverty. However, other challenges, such as birth control policy, inadequate sanitation facilities, and limited basic education need to be addressed to reduce the effects of health shocks on their vulnerability to poverty. In a related study, Séne and Cissé (2015) confirmed that out-of-pocket payments are the primary source through which health expenditure is met in Senegal and, hence, such payments are financial burdens that lead to impoverishment when they become catastrophic.
Amidst the COVID-19 pandemic, a lot has changed in regard to health care financing, both globally and nationally (in Uganda). Households face unprecedented economic constraints and are thus forced to make hard expenditure choices, including whether or how to spend on health care. Wasswa (2021) argued that during Uganda’s second wave of the pandemic, there were high hospital costs and household resources were greatly overstretched, which led many to opt for herbal remedies. According to the Uganda Bureau of Statistics (2021), the number of poor Ugandans increased from 8 million in 2016/17 to 8.3 million in 2019/20, but it is still not clear how much of this impoverishment can be attributed to health expenditure shocks amidst the pandemic.
To our knowledge, all the studies that have estimated the extent of the burden of household health expenditures in Uganda were carried out before the COVID-19 pandemic; therefore, existing reports on household financial catastrophes do not capture well the impacts of the evolving health shocks. For instance, Ssewanyana and Kasirye (2020) estimated catastrophic health expenditures from 2013 to 2015 from household surveys and did not consider recent changes in health care financing in Uganda. More precisely, a lot has changed due to the COVID-19 pandemic as well as the episodic Ebola outbreaks. Therefore, our study provides an opportunity to understand the changes in Uganda’s health care financing landscape as well as the current burden of out-of-pocket health expenditures on households. Considering that the health financing situation in the country has changed significantly, this study leverages the latest Uganda National Household Survey data (2019/20) to fill this knowledge gap.
3. Methodology
This section highlights the different methods and techniques that we adopt to answer our research questions. The data, a summary of how household health and medical care expenditures are captured in the data, theoretical framework, and the estimation strategy are presented here.
3.1. Data
This study uses data from the most recent Uganda National Household Survey (UNHS), i.e., UNHS 2019/20. The 2019/20 UNHS is not only the most recent, but also the first survey ever to collect information on the pre-COVID-19 and COVID-19 periods. The Uganda Bureau of Statistics collected information on household out-of-pocket payments for health care services, which include the following: consultation fees, medicines, hospital/clinic charges, traditional doctor’s fees/medicines, transport, and other health expenses that cannot be broken down. Fifty-five (55) percent of all persons that visited a health care facility after falling sick reported having paid to access the respective services. Of the 55 percent, 51 percent paid official health facility fees while three percent paid unofficial fees. Persons in rural areas were twice as likely to pay unofficial fees compared to their urban counterparts, i.e., 3.3 percent and 1.6 percent, respectively (Uganda Bureau of Statistics, 2021). The data entail other information, such as distance to a health facility as well as demographic and socioeconomic characteristics. Table 1 presents a summary of how household health and medical care expenditures are captured in the data.

Table 1.
Summary of household health and medical care expenditures.
3.2. Theoretical Framework and Empirical Strategy
This study adapts the framework by Wagstaff and Doorslaer (2003), which measures catastrophic health expenditures based on a specified threshold. Just like Ssewanyana and Kasirye (2020), we account for food expenditures by considering total non-food expenses in comparison with health expenses. The main proposition is that a household should not spend more than a given threshold, , of their total non-food expenditures on health care. In case of a household exceeding the set threshold, such expenditure is regarded as catastrophic.
where is the monthly catastrophic health expenditure, is the monthly out-of-pocket health payment, and is the total monthly non-food expenditure for a household, i.e., (total household expenditure minus food expenditure). We adopt three expenditure thresholds, i.e., 10%, 25%, and 40%, as used by Wagstaff and Doorslaer (2003), Ssewanyana and Kasirye (2020), and World Health Organization (2020), respectively.
3.2.1. CHE Headcount ()
This study adopts one of the most common measures of poverty—the poverty headcount (P0)—which is the percentage of the population living on less than USD 1.90 a day at 2011 international prices (Uganda Bureau of Statistics, 2021). Assuming that , if and zero (0) otherwise, the CHE headcount is equal to
where is the sample size and µche is the mean of . Noteworthy, the headcount measure does not capture how much households exceed the threshold (Wagstaff & Doorslaer, 2003). To remedy this, we proceed to measure the CHE poverty gap.
3.2.2. CHE Poverty Gap ()
Here, we intend to capture the degree by which OOPs, as a share of TNE, exceeds the threshold Zcat. Therefore, the CHE poverty gap is defined as
where is the out-of-pocket payment for household and is the total non-food expenditure for household . Dividing (3) by the sample size we obtain the average CHE poverty gap, as given by
where is the mean of . Thus, the mean positive gap is defined as
with , the overall mean catastrophic gap, equals the fraction with a positive gap times the mean positive gap.
3.2.3. The Impoverishing Effect of CHEs in the Pre- and COVID-19 Periods
To ascertain how CHEs affected households in the pre-COVID-19 and COVID-19 period, we calculate the aforementioned two measures for both periods. We then perform a comparative analysis of the incidence and intensity of catastrophic health expenditures in the pre-COVID-19 and COVID-19 periods to examine the effect of health expenditures on household welfare amidst the pandemic.
In pre-COVID-19 period,
where is the mean of . Thus, the pre-COVID-19 mean positive gap is defined as
We replace the pre-COVID-19 period with the COVID-19 period, following all other superscripts and subscripts to obtain similar COVID-19 measures.
3.2.4. Demographic and Socioeconomic Determinants of OOPs
We utilize information on household demographic and socioeconomic factors to examine their effect on household OOPs. Studies have shown that there is a need for targeted interventions to reduce OOPs, especially among the most affected groups, and this is aimed at increasing financial risk protection, which consequently reduces vulnerability to poverty. For instance, Kwesiga et al. (2020), Aregbeshola and Khan (2017), and Nabyonga Orem et al. (2013) postulated that household size, household socio-economic status, type of illness suffered, type of health facility visited, geo-political zones, education of household heads, and location are some of the key determinants of impoverishment due to OOPs.
Our unit of analysis is the household; we restrict our sample to households that incurred at least one health and medical care expense. This implies that we are introducing some degree of bias due to “left-censoring” of household health expenditure, since we decided to only observe households whose expenditure is above zero; thus, we run a Tobit model (Wooldridge, 2010). For comparative analysis, we run quantile regressions for the 25th, 50th, and 75th quantiles. But first, we transform our outcome variable, OOP, by taking its logarithm using a general econometric model, specified as follows:
where is the logarithm of monthly out-of-pocket payments for health care for household is the error term. Key policy variable is NCD (non-communicable disease), which is a dummy of 1 if a household has any member with either diabetes, high blood pressure, heart disease, and/or cancer, and 0 otherwise. The NCD variable is critical considering that non-communicable diseases require huge sums of money to treat. The fact that they are chronic illnesses means that treatment can go on for prolonged periods until the patient dies, and expenditure on such diseases keeps the household facing catastrophic expenses and consequently in chronic poverty. Adult > 65 years is a dummy of 1 if a household has a member above 65 years of age and 0 otherwise. Other controls are Sex, which is 1—female and 0—male; HHsize is the number people in a household; Mstatus is the marital status (1—married monogamous/living together, 2—married polygamous/living together, 3—separated/divorced, 4—widow/widower, 5—never married); RurUrban (rural = 0 and urban = 1); and Distance is the distance in km to the facility of first consultation (1 = 0–<3 km; 2 = 3–<5 km; 3 = 5–<8 km; and 4—≥8 km). Facility is the type of health facility visited (1 = public facility and 0 = private facility); Smoker is 1 if a household has a smoker and 0 otherwise; COV ID is the COVID-19 pandemic dummy, which is 1 if a household’s data were collected during the pandemic and 0 otherwise; Malaria is 1 if any household member suffered from malaria and 0 otherwise; and Region represents the four regions of Uganda, i.e., 1 = central, 2 = eastern, 3 = northern, and 4 = western.
We run the Breusch–Pagan/Cook–Weisberg test for heteroskedasticity to ascertain whether we are faced with a constant variance or not. The null hypothesis is that the variance is constant and the assumption of independent and identically distributed (i.i.d) errors holds. If the variance is not constant, quantile regressions produce reliable estimates to supplement estimates from the ordinary least squares regression. More precisely, quantile regression analysis produces credible estimates in the event of heteroskedasticity
3.2.5. The Effect of Catastrophic Health Expenditures on Household Welfare
Here, we proxy household welfare by household food consumption expenditure. The goal is to ascertain how much catastrophic health expenditures affect what would have been spent on food in a household. We estimate the effect of catastrophic health expenditures on household welfare proxied by household food consumption expenditure adjusted for regional prices.
The OLS econometric model is specified as follows:
where is the logarithm of monthly food consumption expenditure for household is the error term. First, we use the conventional OLS method to examine the effect of catastrophic health expenditure on household food consumption. However, we recognize that there is simultaneous causality between our measure of household welfare and OOPs, which introduces endogeneity, rendering OLS estimates spurious. Generally, measurement errors in the regressors and simultaneity of the dependent variable and the regressor bring endogeneity (Gujarati & Porter, 2009; Cameron & Trivedi, 2005; Green, 2012). Therefore, we run a two-stage least squares (2SLS) model instrumenting OOPs with the maximum number of times a household member fell sick3. This number acts as the value for the entire household. We do not consider the average number of times as the mean as that would be misleading if a household has some members who rarely fall sick. Such individuals would greatly lower the mean number with their zero (0) number of times of falling sick. More precisely, we run Equation (10) by instrumenting lnOOP by Median Number days sick—median number of times of falling sick within a household, i.e., . The instrumental variable (IV) model is specified as follows:
4. Results
Among the households that spend on medical and health care, on average each household spends approximately UGX 45,145 monthly. The total monthly household expenditure after adjusting for inflation is approximately UGX 372,128 on average. In addition, seven percent of the households have elders who are above 65 years of age, whereas the results show that there is a high prevalence of malaria in the country, with close to 50 percent of households having someone who had suffered from malaria. This indicates that malaria is a significant contributor to household out-of-pocket payments for medical care. The majority of Ugandans visit private health facilities for their first consultation (71%), compared to only 29 percent who go to a public facility for their first consultation whenever they fall sick. This might be due to a number of factors that range from the proximity of private facilities to confidence in and individuals’ perceptions of the services provided by private and public facilities. Furthermore, the majority of the households that incur health care expenditures are found in rural areas, representing 77 percent compared to only 23 percent in urban areas (see Table 2).

Table 2.
Summary statistics (UNHS 2019/20).
We attempted to find out whether there were significant differences in household health expenditure between the pre-COVID-19 and COVID-19 periods using the t-test. Our expectation was that all expenditure categories should exhibit high and significant differences, with more money being spent during the COVID-19 pandemic. However, our analysis showed that this was not the case, except for expenditure on medicines. Household expenditure on medicines was higher during COVID-19 compared to the pre-COVID-19 period. The rest of the health and medical care expenditure components indicate that households spent more in the pre-COVID-19 than the COVID-19 period. For instance, the results indicate that households spent more on consultations in the pre-COVID-19 period than in the COVID-19 period. This was because most consultations were curtailed by the COVID-19 containment measures, such as curfews and lockdowns, which greatly reduced visits to health facilities for consultations and instead increased self-medication at home (see Table 3).

Table 3.
Monthly household health expenditures in the pre-COVID-19 and COVID-19 periods.
In Table 4, we present the incidence and intensity of catastrophic health payments based on non-food household expenditures using the three thresholds of 10%, 25%, and 40%. As expected, the catastrophe faced by a household reduces as we move up the thresholds. The table presents the headcount and poverty gap as well as the mean positive poverty gap.

Table 4.
Incidence (headcount) and intensity (gap) of catastrophic health expenditures in Uganda.
Based on the 10% threshold for the headcount measure, catastrophic health expenditures are as high as 37.7%. More precisely, 37.7%, 33.6%, and 28.7% of households spend more than 10%, 25%, and 40% of their non-food expenditures on health care, respectively. The estimates of the poverty gap are in line with the headcount estimates. However, they are slightly lower than the headcount estimates, i.e., the poverty gap is at 31.3%, 26.2%, and 21.7% for the three respective thresholds. In terms of the intensity of the catastrophic payments, the results in Table 4 indicate that the mean positive poverty gap is worryingly high for all three thresholds, i.e., 82.9%, 78.0%, and 75.8% for the 10%, 25%, and 40% thresholds. Specifically, among the households that spend more than 10%, 25%, and 40% of their non-food expenditure on out-of-pocket health payments, their average out-of-pocket budget share exceeds the respective thresholds by 82.9, 78.0, and 75.8 percentage points.
We then performed the same analysis for both the pre-COVID-19 and COVID-19 pandemic periods, as presented in Table 5. The aim was to investigate if there were significant differences in both the incidence and intensity of the catastrophic health expenditures for both periods. The results confirm what we saw in the descriptive analysis, that it is indeed not entirely true that households faced extreme catastrophic health expenditures for all components of health and medical care. It is, rather, that some expenditures on health were reduced during the COVID-19 pandemic. This is partly attributed to the effect of pandemic containment measures, which reduced expenditures on some components of medical care, such as consultation fees, as people reduced visits to health facilities out of fear of catching the COVID-19 virus. Wasswa (2021) highlighted that Uganda had low inpatient numbers as desperate patients turned to alternative medicines, such as herbs.

Table 5.
Incidence (headcount) and intensity (gap) of catastrophic health expenditures in the pre-COVID-19 and COVID-19 periods in Uganda.
Foregone or Substituted Care?
Leveraging the entire UNHS sample and using the sample weights to reflect the entire population, we investigated the health care-seeking behaviors of Ugandans. We found that of the 19.5% of Ugandans who suffered a major illness or injury, 85.9% sought care and consulted either a doctor, nurse, pharmacist, or traditional healer. Here, we were majorly interested in knowing why the remaining 14.1% did not seek care even though they duly suffered an illness or injury. We performed a comparative analysis—between the pre-COVID-19 and COVID-19 pandemic periods—of the reasons why care was not sought.
We found that during the COVID-19 pandemic period, 21.5% of Ugandans did not seek medical care because they lacked the money or funds to do so. This is an increase from the 18.6% that failed to seek medical care due to a lack of money in the pre-pandemic period. This implies that when the pandemic ravaged the economy, many Ugandans could not afford to pay for medical care costs and thus decided to forego care. Relatedly, during the pandemic period, 12.0% of Ugandans did not seek medical care because they used herbs or home remedies, which was an increase from the 11.4% that substituted facility care with home remedies before the pandemic.
This shows that the comparatively low incidence and intensity of CHEs during the pandemic period (see Table 4 and Table 5) is not entirely due to low health expenditure by households, but rather foregone and substituted care. We also ruled out the possibility of illnesses being comparatively mild or less severe during the pandemic period. This is because in the pre-pandemic period, more Ugandans (27.1%) did not seek medical care due to their illness being mild compared to only 23.6% during the pandemic period (see Table 6). We conclude that not seeking care during the COVID-19 period was not due to the lesser severity of the illnesses suffered by Ugandans—confirming the prevalence of foregoing and/or substituting medical care with cheaper alternatives, such as local remedies and herbs. Our findings on the substitution of medical facility medical with other alternatives are in line with those of Wasswa (2021), who argued that Uganda’s low inpatient numbers amidst the pandemic masked high community infection as desperate patients turned to herbs.

Table 6.
Reasons why medical care was not sought.
The results in Table 7 show that the directions of effect (as seen from the signs of the coefficients) are exactly the same under the Tobit and quantile regressions as well as the OLS regression. A slight difference is noticed only in terms of magnitude. According to Wooldridge (2010), there is always a temptation to compare the magnitudes of, for example, OLS and Tobit estimates, but such comparisons are not very informative. Thus, we did not labor to explain the different models separately, but instead concentrated on the peculiarities among the different quantiles.

Table 7.
Demographic and socioeconomic determinants of OOPs.
A household with a member aged above 65 years experiences increased household out-of-pocket health payments by 44 percent on average (50th quantile). Noteworthily, the results mimic a similar pattern for all three quantile regressions, with the highest effect reported for the 50th quantile, at about 45 percent. Furthermore, out-of-pocket payments for health and medical care increase as the distance in kilometers to a health facility increases. More precisely, the longer the distance to a health facility, the higher the household out-of-pocket payments for medical care. This speaks to the need to bring health facilities closer to communities to cut down on CHEs. However, the results show that visiting a public rather than a private health facility reduces out-of-pocket payments by 52 percent. This is a similar trend for all the quantile regressions, as health expenses are reduced by 62.4, 62.2, and 35.3 percent for the 25th, 50th, and 75th quantiles, respectively.
We note that the effect of a reduction in health expenses shrinks as we move to higher quantiles (higher health expenditure), i.e., as we move to households that spend highly on health and medical care. This implies that households in the 25th and 50th quantiles benefit more from the services of public facilities and such households tend to be poor or in the middle class. The effect is rather low for households in the 75th quantile because they utilize more private as compared to public health facilities. This is informative for policy makers to target and subsidize public health services for a section of households that would exhibit the largest reduction in out-of-pocket health payments. Furthermore, households with members suffering from non-communicable diseases (diabetes, hypertension, heart diseases, and/or cancer) exhibit an increase in expenditure on medical care by 33 percent. This effect is lower for the 25th quantile (28.6 percent), but increases to 30.3 percent for the 50th quantile, and finally reduces to the lowest value of 28.2 percent for the 75th quantile.
Using the sqreg command in Stata 18, we ran a simultaneous quantile regression (with 500 bootstrap replications) to compare the regression coefficients estimated for the different quantiles. Indeed, we confirmed that the effect of the regressors on household health expenditure is not constant across the distribution.
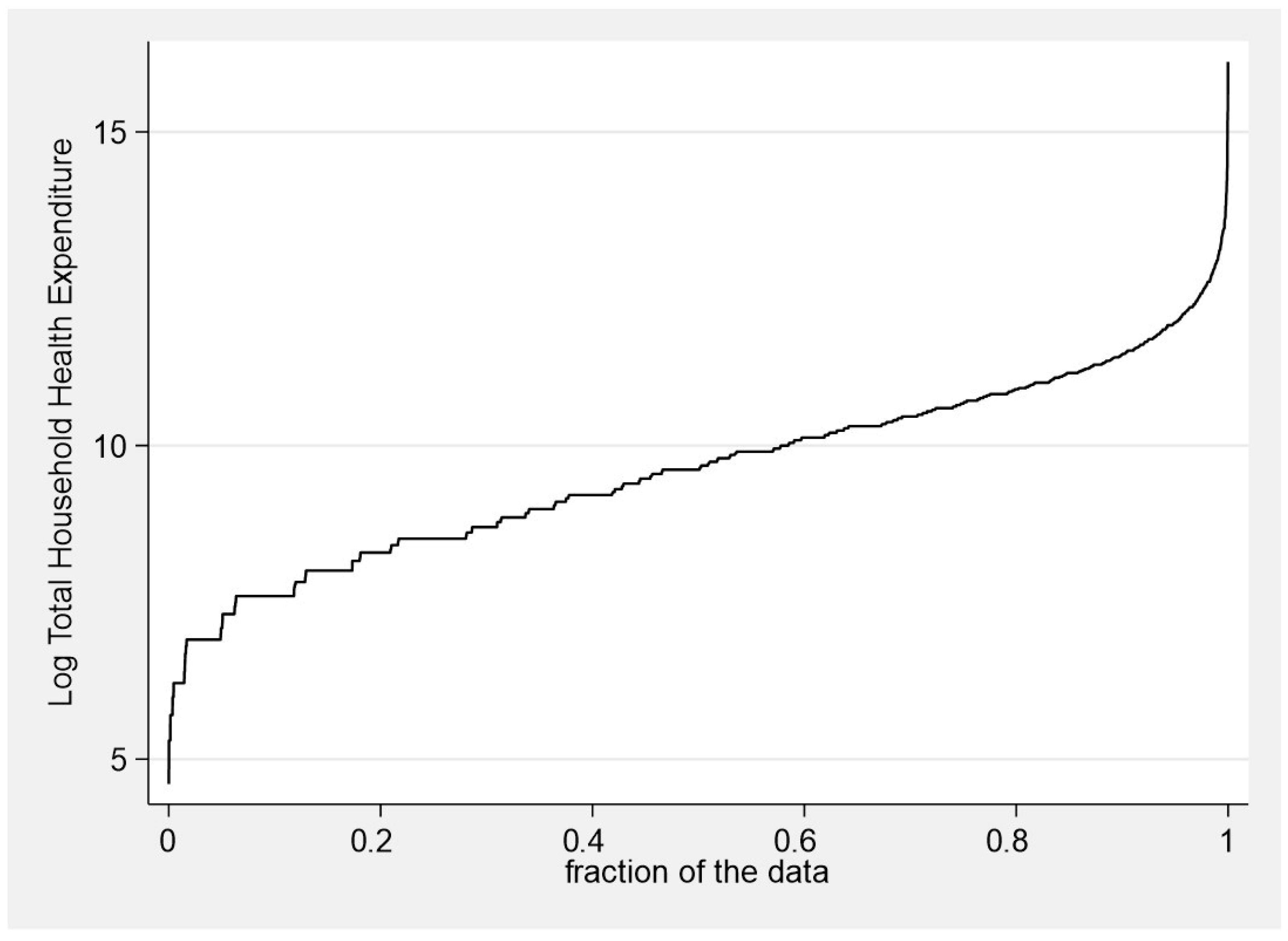
Figure 2 shows a graphical representation of household health expenditure, and how it changes over the different expenditure quantiles. There is a sharp increase in household expenditure on health at the lowest quantile—the households that spend the least on health expenditure. Such households are often the poorest in terms of income. The same result is mimicked among the households that spend the highest amounts on health and medical care.
Figure 2.
Household health expenditure over the quantiles. Source: data from the UNHS 2019/20.
In Table 8, we present a two-stage least squares log–log model of the effect of out-of-pocket health payments on household food consumption expenditure. We concentrate on the instrumental variable regression results, which are free from any possible endogeneity bias caused by the simultaneous causality between household food consumption expenditure as a measure of welfare and out-of-pocket health payments. The coefficient is the estimated percent change in the dependent variable for a percent change in the independent variable. An elasticity of −0.256 means that a one percent increase in household health expenditure reduces household food consumption by 0.256 percent, holding all other factors constant. In other words, a 10% increase in out-of-pocket health payments reduces household food consumption expenditure and consequently household welfare by 2.6%.

Table 8.
The effect of out-of-pocket payments on household welfare.
Our first-stage regression results indicate that our instrument (median number of times of falling sick in a household) is relevant since it is statistically significant in the OOP regression. To proceed to the second stage—IV regression—we tested for the validity of the instrument and consequently rejected the null hypothesis (H0: instrument is weak), since the Prob > F = 0.000 of the F (1,3477) = 20.6638. We concluded that our instrument is valid and not weak since the minimum eigenvalue statistic, or the F-statistic = 20.66, is also greater than the critical value of 16.38.
5. Conclusions
This paper studies the financial burden on households due to health expenditure shocks amidst a bigger and global health shock. We take advantage of the most recent (2019/20) Uganda National Household Survey data that were collected in two phases—before and during COVID-19. Our comparative analysis of the pre-COVID-19 and COVID-19 times indicates that households spent more on medicine in the COVID-19 period compared to the pre-COVID-19 period, but the on average expenditures on consultation fees, transport to and from hospitals/clinics, traditional doctor’s fees, hospital/clinic charges, and all other expenses not broken down were reduced during the pandemic period.
We find that among households which incur any form of health care expense, 37.7%, 33.6%, and 28.7% spend more than 10%, 25%, and 40% of their non-food expenditures on health care, respectively. Yet, public expenditure on health is not increasing as expected. For instance, Uganda’s health sector budget as a share of the total budget and GDP averaged 1.9% and 6.4%, respectively, for the financial years 2018/19 to 2022/23. In terms of the intensity of CHEs, the household average OOP health budget share exceeds the respective thresholds by 82.9, 78.0, and 75.8 percentage points. Relatedly, households with members above 65 years of age and those with a member suffering from a non-communicable disease face significantly higher OOPs. Overall, we find fascinating results showing that, on average, the incidence and intensity of catastrophic health expenses was less severe during the COVID-19 period compared to the pre-pandemic period. Generally, households spent less on health and medical care from their pockets amidst the pandemic compared to how much they used to spend before the pandemic.
To understand why the incidence and intensity of CHEs was lower during the pandemic compared to the pre-pandemic period, we investigated the health care-seeking behaviors of Ugandans in both periods. We found that during the COVID-19 pandemic period, 21.5% of Ugandans did not seek medical care because they lacked the money or funds to do so, compared to only 18.6% who did not seek care for the same reason in the pre-pandemic period. This finding leads us to argue that when the pandemic distorted the economy, many Ugandans could not afford to pay for medical care costs and thus decided to forego care. We further unearthed that during the pandemic period, 12.0% of Ugandans did not seek medical care because they used herbs or home remedies, which was an increase from the 11.4% that substituted facility care with home remedies before the pandemic. This shows that the comparatively low incidence and intensity of CHEs during the pandemic period was not entirely due to low health expenditure by households, but rather foregone and substituted care. This conclusion was reached after ruling out the possibility of illnesses being comparatively mild or less severe during the pandemic period—in the pre-pandemic period, more Ugandans (27.1%) did not seek medical care due to an illness being mild, compared to only 23.6% during the pandemic period.
When we went a step further to estimate the impoverishing effect of OOPs for health on household welfare, we found that a 10% increase in OOPs on health reduces household food consumption expenditure by 2.6%. This implies that when households are faced with two conflicting basic needs to finance, that is, food and medical care, there is an inevitable tradeoff. The high incidence and intensity of the CHEs we found in our study is not unprecedented, and similar findings have been documented by other studies. For instance, Ssewanyana and Kasirye (2020) postulated that Uganda has the second highest rate of CHEs among five sub-Saharan African countries (Ethiopia, Malawi, Nigeria, Tanzania, and Uganda), even after user fees for public health facilities were abolished in 2001. We also learned that when individuals or households are constrained financially, they will either forego to seek health care or substitute the expensive care with alternatives, such as herbs or home remedies. Therefore, the current modality of health care financing, where households incur CHEs, keeps them in chronic poverty. Thus, enhancing public health expenditure as well as the pooling of resources by households through different forms of health insurance, including community health insurance schemes, are critical to mitigate the impact of CHEs.
While we have approached closer to understanding the extent to which out-of-pocket health payments exceeded the threshold for household financial catastrophe amidst the pandemic, we did not explicitly estimate virus-specific expenditures due to data limitations. In addition, we did not delve into the causal mechanisms behind the correlations we found. In this regard, we believe that further research can concentrate on unearthing the causal mechanisms behind some of our results. However, we believe that the fascinating results we present in this paper are a basis for sparking a discussion around how the pandemic affected households’ expenditures and welfare.
Author Contributions
Conceptualization, D.M.; Methodology, D.M.; Software, D.M.; Validation, D.M., S.N. and B.L.Y.; Formal analysis, D.M.; Investigation, D.M., S.N. and B.L.Y.; Resources, D.M.; Data curation, D.M.; Writing—original draft, D.M., S.N. and B.L.Y.; Writing—review & editing, D.M., S.N. and B.L.Y.; Visualization, D.M.; Supervision, D.M.; Project administration, D.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the African Economic Research Consortium (AERC) through the Addressing Health Financing Vulnerabilities in Africa due to the COVID-19 Pandemic, grant number RC22517.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The original data presented in this study are available at the Uganda Bureau of Statistics, upon request at: https://www.ubos.org/publications/statistical/ (accessed on 21 April 2025).
Acknowledgments
We are grateful to Ingrid Woolard, Tomson Ogwang, Germano Mwabu, Bernadette Kamgnia, and participants of the AERC review workshops on “Addressing Health Financing Vulnerabilities in Africa due to the COVID-19 Pandemic” for the valuable comments and suggestions. This paper was written while the leading author was still at the Economic Policy Research Centre, Kampala, Uganda. All remaining errors are our own.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix A
Appendix A.1. Weighting of Regressions (Summary of Survey Regressions)
All the regressions were run on the estimation sample, not only to report consistent estimates, but also to make policy recommendations at a national level.

Table A1.
Weighting of regressions.
Table A1.
Weighting of regressions.
| Regression | y = LogOOP | y = LogFoodExpenditure |
|---|---|---|
| Number of strata | 17 | 17 |
| Number of PSUs | 4061 | 4061 |
| Number of observations | 4061 | 4061 |
| Design df | 4044 | 4044 |
| F(19, 4026), F(24, 4021) | 36.05 | 171.79 |
| Prob > F | 0.0000 | 0.0000 |
| Population size (No. of Households) | 2,663,969 | 2,663,969 |
Source: data from the UNHS 2019/20.
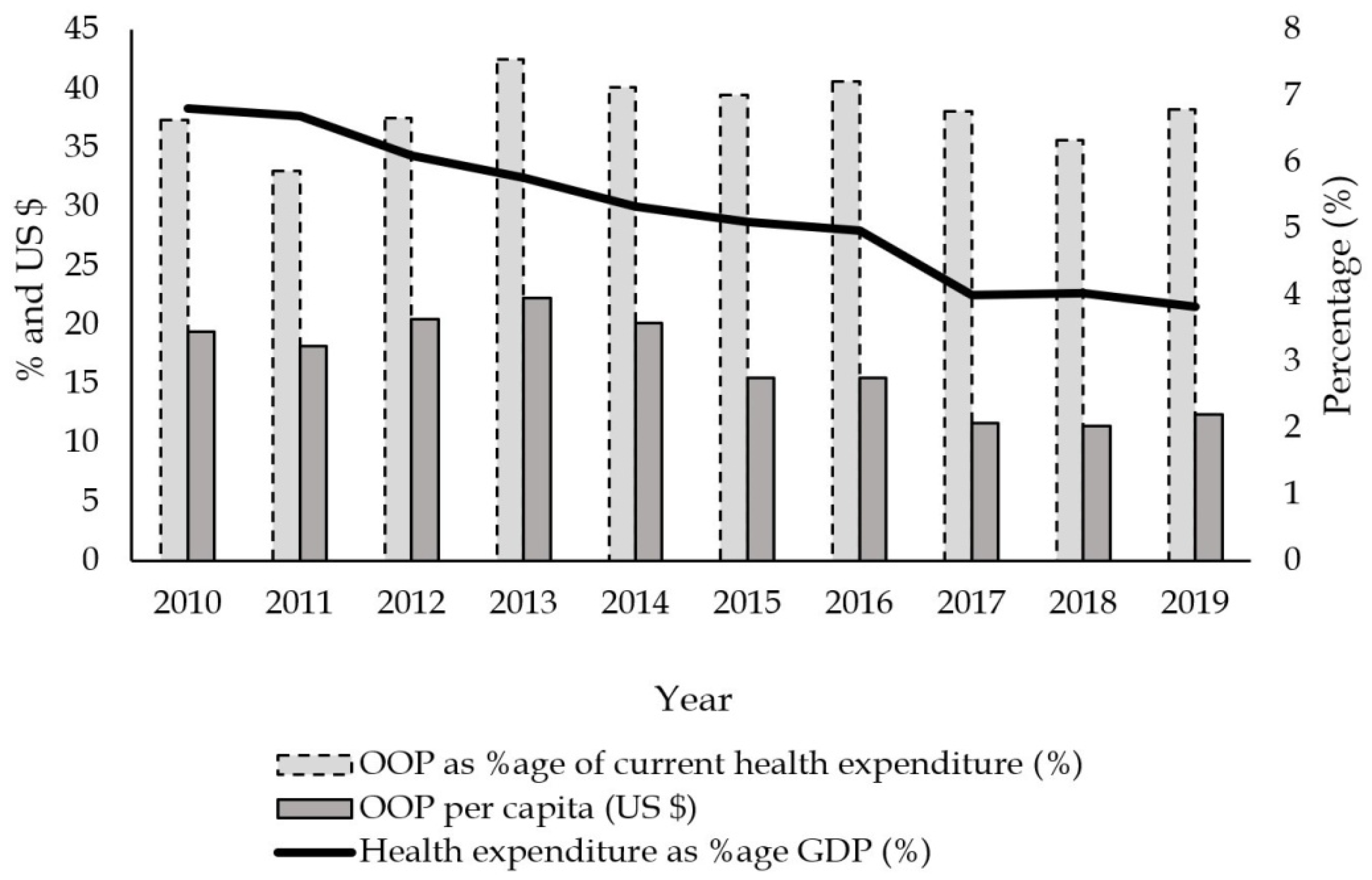
Appendix A.2. Out-of-Pocket Payments vs. Public Health Expenditure
Figure A1.
Out-of-pocket and public health expenditure over time (2010–2019). Source: data from the Global Health Observatory data repository: World Health Organization (2022).
Figure A1.
Out-of-pocket and public health expenditure over time (2010–2019). Source: data from the Global Health Observatory data repository: World Health Organization (2022).
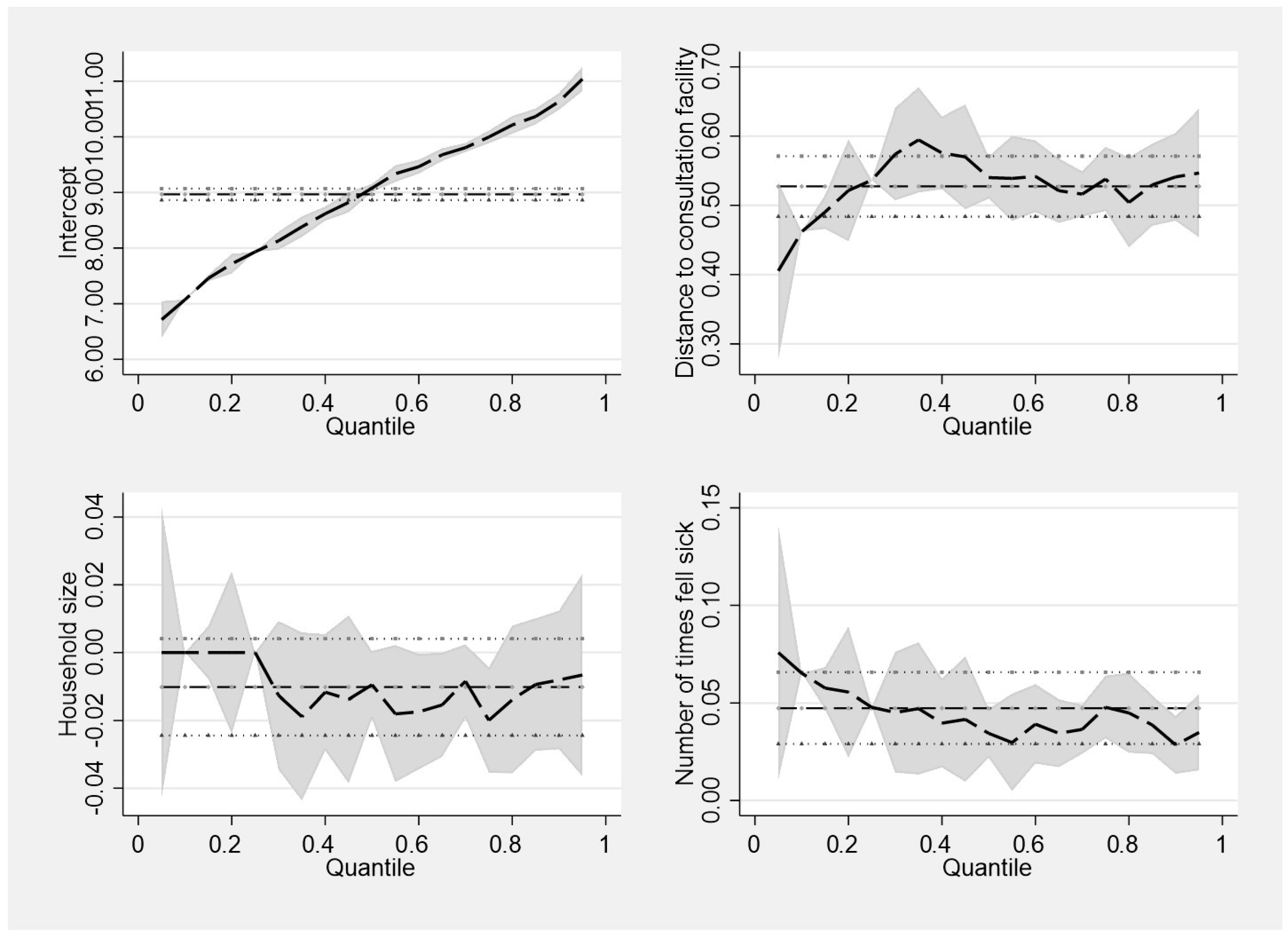
Appendix A.3. Distance, Number of Times Experiencing Sickness, and Household Size Across the Quantiles
Here, we present the coefficients of selected regressors and the intercept from the quantile regressions. The horizontal, bold, dotted lines in each graph represent the OLS coefficients and they do not vary across the quantiles. The horizontal dotted lines that surround the horizontal, bold, dotted middle lines represent the confidence intervals for the OLS. Noteworthily, the coefficients that change/vary across the OLS confidence intervals are for the quantile coefficients and whenever they vary, they signify significant differences between the OLS and the quantile regression coefficients.
Figure A2.
Coefficients of selected regressors from the quantile regressions. Source: data from the UNHS 2019/20.
Figure A2.
Coefficients of selected regressors from the quantile regressions. Source: data from the UNHS 2019/20.
Appendix A.4. Variance Inflation Factor
The mean V IF for the health expenditure and food consumption expenditure model is 1.260 and 1.509, respectively. This is far lower than the acceptable maximum of 10, which is an indication of an absence of multicollinearity in the models.
| y = LogOOP | ||
| Variable | VIF | 1/VIF |
| Eastern region | 2.09 | 0.478 |
| Northern region | 1.905 | 0.525 |
| Western region | 1.777 | 0.563 |
| Widow/widower | 1.432 | 0.698 |
| HH with elder > 65 yrs | 1.258 | 0.795 |
| Never married | 1.211 | 0.826 |
| Female | 1.174 | 0.851 |
| NCD | 1.153 | 0.867 |
| Household size | 1.153 | 0.868 |
| Divorced/separated | 1.141 | 0.877 |
| Smoker | 1.108 | 0.902 |
| Married polygamous | 1.088 | 0.919 |
| Distance (>8 km) | 1.085 | 0.922 |
| Urban | 1.082 | 0.924 |
| Distance (3–<5 km) | 1.077 | 0.928 |
| Public facility | 1.076 | 0.929 |
| Malaria | 1.056 | 0.947 |
| In-COVID-19 | 1.038 | 0.964 |
| Distance (5–<8 km) | 1.031 | 0.97 |
| Mean VIF | 1.260 | |
| y = LogFoodExpenditure | ||
| Variable | VIF | 1/VIF |
| Income quintile 5 | 3.225 | 0.31 |
| Income quintile 4 | 2.55 | 0.392 |
| Income quintile 3 | 2.367 | 0.422 |
| Eastern region | 2.157 | 0.464 |
| Income quintile 2 | 2.048 | 0.488 |
| Northern region | 1.982 | 0.504 |
| Western region | 1.803 | 0.554 |
| Widow/widower | 1.437 | 0.696 |
| Log health expenditure | 1.426 | 0.701 |
| Household size | 1.308 | 0.765 |
| HH with elder > 65 yrs | 1.269 | 0.788 |
| Distance (>8 km) | 1.226 | 0.816 |
| Never married | 1.217 | 0.822 |
| Female | 1.184 | 0.845 |
| NCD | 1.16 | 0.862 |
| Divorced/separated | 1.145 | 0.873 |
| Urban | 1.137 | 0.88 |
| Public facility | 1.112 | 0.9 |
| Smoker | 1.111 | 0.9 |
| Distance (3–<5 km) | 1.102 | 0.907 |
| Married polygamous | 1.09 | 0.917 |
| Distance (5–<8 km) | 1.062 | 0.942 |
| Malaria | 1.06 | 0.943 |
| In-COVID-19 | 1.04 | 0.961 |
| Mean VIF | 1.509 | |
| The variance inflation factor is defined as . Source: data from the UNHS 2019/20. | ||
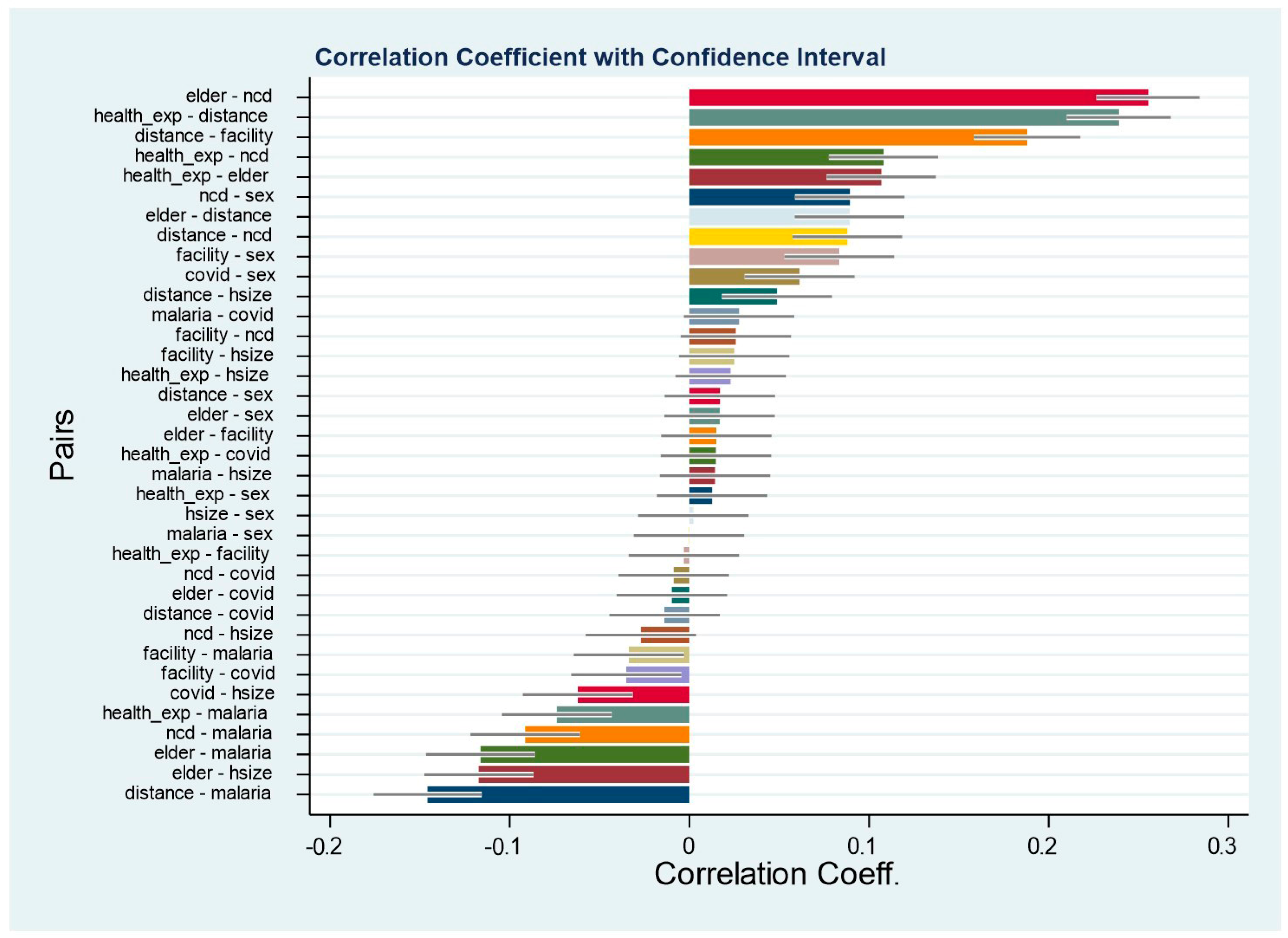
Appendix A.5. Pairwise Correlation Coefficients
The pairwise correlation coefficients between the variables are normal (all the coefficients are below 0.7 in absolute terms), which confirms that our models do not suffer from perfect multicollinearity and thus yield reliable estimates.
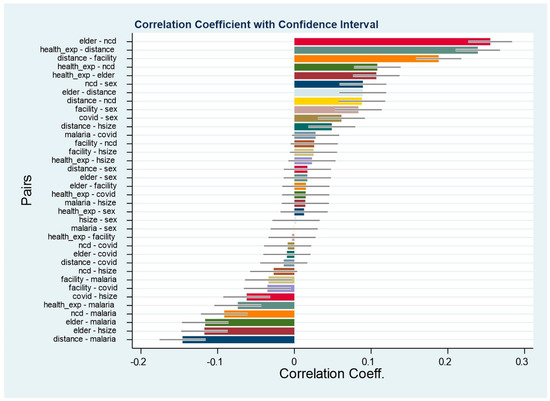
Figure A3.
Pairwise correlation coefficients. Source: data from the UNHS 2019/20.
Figure A3.
Pairwise correlation coefficients. Source: data from the UNHS 2019/20.
Notes
| 1 | See Mpuuga and Eshete (2022) and Mpuuga et al. (2019) for a review of the health care financing double jeopardy faced by households in the wake of limited health insurance coverage and an upsurge of noncommunicable diseases. |
| 2 | The government of Uganda abolished user fees for all public health units on 1 March 2001. |
| 3 | Our instrument was generated from the question, which was asked verbatim, “How many times did [NAME] fall sick during the last 30 days?”. Since all our expenditure estimates are measured monthly, we consider the median number of times of falling sick within a household in a month. Considering that our unit of analysis is a household and not an individual, we take the median number of times for each unique household. We do not consider the average to avoid underestimating the health expenditure burden in the event a household has a common sickly person when the rest of the members rarely fall sick. |
References
- Alam, K., & Mahal, A. (2014). Economic impacts of health shocks on households in low- and middle-income countries: A review of the literature. Globalization and Health, 10(1), 1–18. [Google Scholar] [CrossRef] [PubMed]
- Aregbeshola, B. S., & Khan, S. M. (2017). Determinants of impoverishment due to out-of-pocket payments in Nigeria. Journal of Ayub Medical College Abbottabad, 29(2), 194–199. [Google Scholar]
- Ataguba, J. E. O. (2012). Reassessing catastrophic health-care payments with a Nigerian case study. Health Economics, Policy and Law, 7(3), 309–326. [Google Scholar] [CrossRef] [PubMed]
- Atake, E. H. (2018). Health Shocks in Sub-Saharan Africa: Are the poor and uninsured households more vulnerable? Health Economics Review, 8(1), 26. [Google Scholar] [CrossRef] [PubMed]
- Bloom, D., & Canning, D. (2003). The health and poverty of nations: From theory to practice. Journal of Human Development, 4(1), 47–71. [Google Scholar] [CrossRef]
- Cameron, A. C., & Trivedi, K. P. (2005). Microeconometrics methods and applications. Cambridge University Press. [Google Scholar]
- Green, H. W. (2012). Econometric analysis (7th ed.). Pearson Education Inc. [Google Scholar]
- Gujarati, N. D., & Porter, C. D. (2009). Basic econometrics (5th ed.). McGraw-Hill International. [Google Scholar]
- Gupta, I., & Mitra, A. (2004). Economic growth, health and poverty: An exploratory study for India. Development Policy Review, 22(2), 193–206. [Google Scholar] [CrossRef]
- Kwesiga, B., Aliti, T., Nabukhonzo, P., Najuko, S., Byawaka, P., Hsu, J., & Kabaniha, G. (2020). What has been the progress in addressing financial risk in Uganda? Analysis of catastrophe and impoverishment due to health payments. BMC Health Services Research, 20(1), 741. [Google Scholar]
- Ministry of Health. (2021). Annual health sector performance report—Financial year 2020/21. Ministry of Health. [Google Scholar]
- Mpuuga, D., & Eshete, Z. S. (2022). Uncovered silent killers: The prevalence of non-communicable diseases and health insurance coverage in Uganda. African Journal of Economic Review, 10(1), 95–116. [Google Scholar]
- Mpuuga, D., Mbowa, S., & Odokonyero, T. (2019). Limited health insurance coverage amidst upsurge of non-communicable diseases in Uganda. Economic Policy Research Centre (EPRC). [Google Scholar]
- Mpuuga, D., Yawe, B. L., & Muwanga, J. (2020). Determinants of demand for health insurance in Uganda: An analysis of utilisation and willingness to pay. Tanzania Economic Review, 10(1), 1–22. [Google Scholar] [CrossRef]
- Nabyonga Orem, J., Mugisha, F., Okui, A. P., Musango, L., & Kirigia, J. M. (2013). Health care seeking patterns and determinants of out-of-pocket expenditure for malaria for the children under-five in Uganda. Malaria Journal, 12(1), 175. [Google Scholar] [CrossRef] [PubMed]
- Séne, L. M., & Cissé, M. (2015). Catastrophic out-of-pocket payments for health and poverty nexus: Evidence from Senegal. International Journal of Health Economics and Management, 15(3), 307–328. [Google Scholar] [CrossRef] [PubMed]
- Ssewanyana, S., & Kasirye, I. (2020). Estimating catastrophic health expenditures from household surveys: Evidence from living standard measurement surveys (LSMS)-integrated surveys on agriculture (ISA) from sub-Saharan Africa. Applied Health Economics and Health Policy, 18(6), 781–788. [Google Scholar] [CrossRef] [PubMed]
- Uganda Bureau of Statistics. (2021). Uganda national household survey 2019/2020. Uganda Bureau of Statistics. [Google Scholar]
- Wagstaff, A., & Doorslaer, E. V. (2003). Catastrophe and impoverishment in paying for health care: With applications to Vietnam 1993–1998. Health Economics, 12(11), 921–933. [Google Scholar] [CrossRef] [PubMed]
- Wasswa, H. (2021). Covid-19: Uganda’s low inpatient numbers mask high community infection as desperate patients turn to herbs. BMJ: British Medical Journal, 374, n1909. [Google Scholar] [CrossRef] [PubMed]
- Wooldridge, J. M. (2010). Econometric analysis of cross section and panel data. MIT press. [Google Scholar]
- World Health Organization. (2020). Monitoring health for sustainable development goals (SDGs). World Health Statistics. [Google Scholar]
- World Health Organization. (2022). Global health observatory database, 2022. World Health Organization. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).