Cost Analysis of COVID-19 in Australia
Abstract
1. Introduction
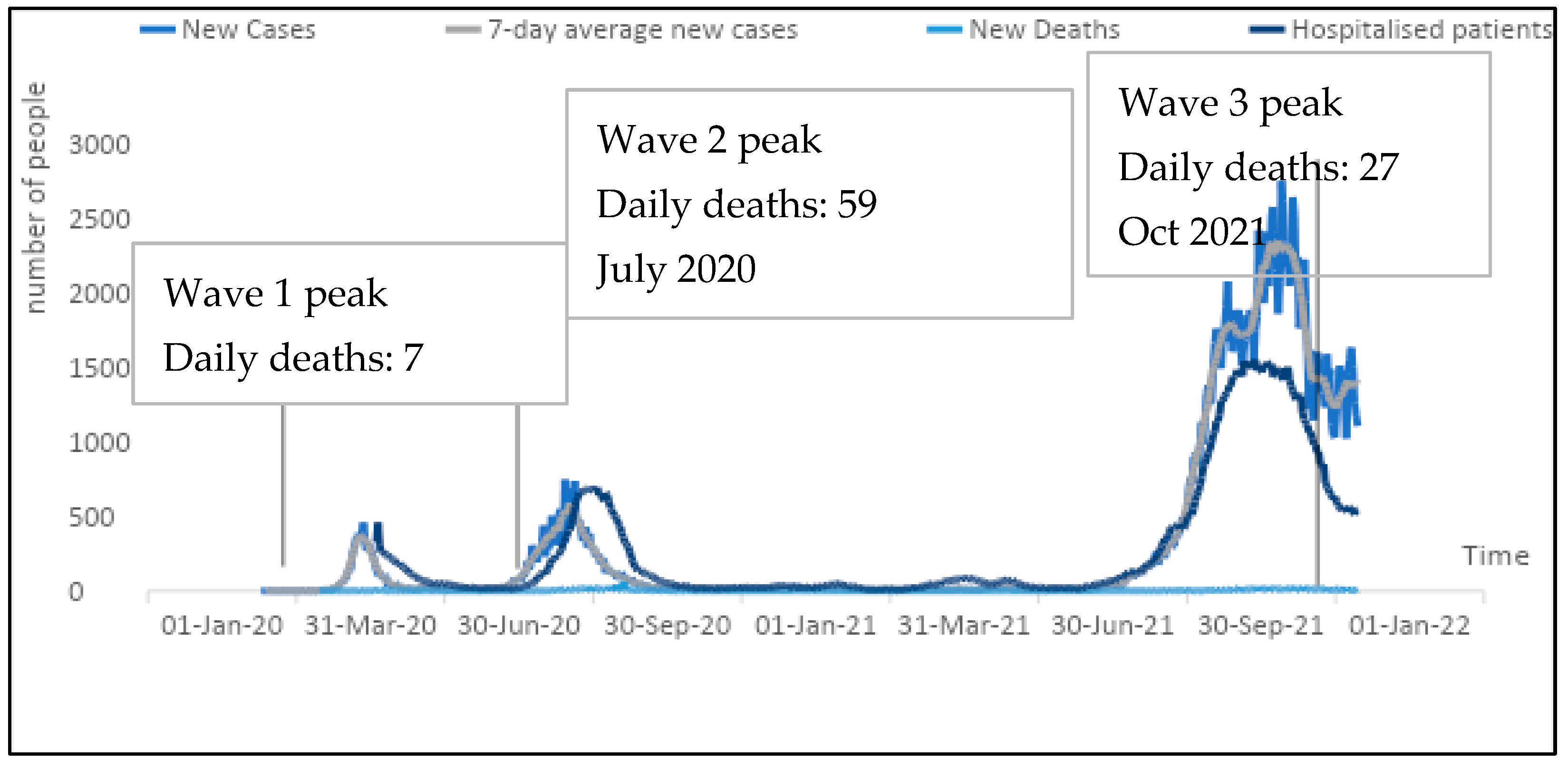
2. Public Health Responses to COVID-19 in Australia
3. Literature Review
4. Data and Methodology
Data Collection
5. Methodology
6. Results
6.1. Direct Cost
6.2. WHO-CHOICE Specific Cost Factors for Inpatient Health Service Delivery
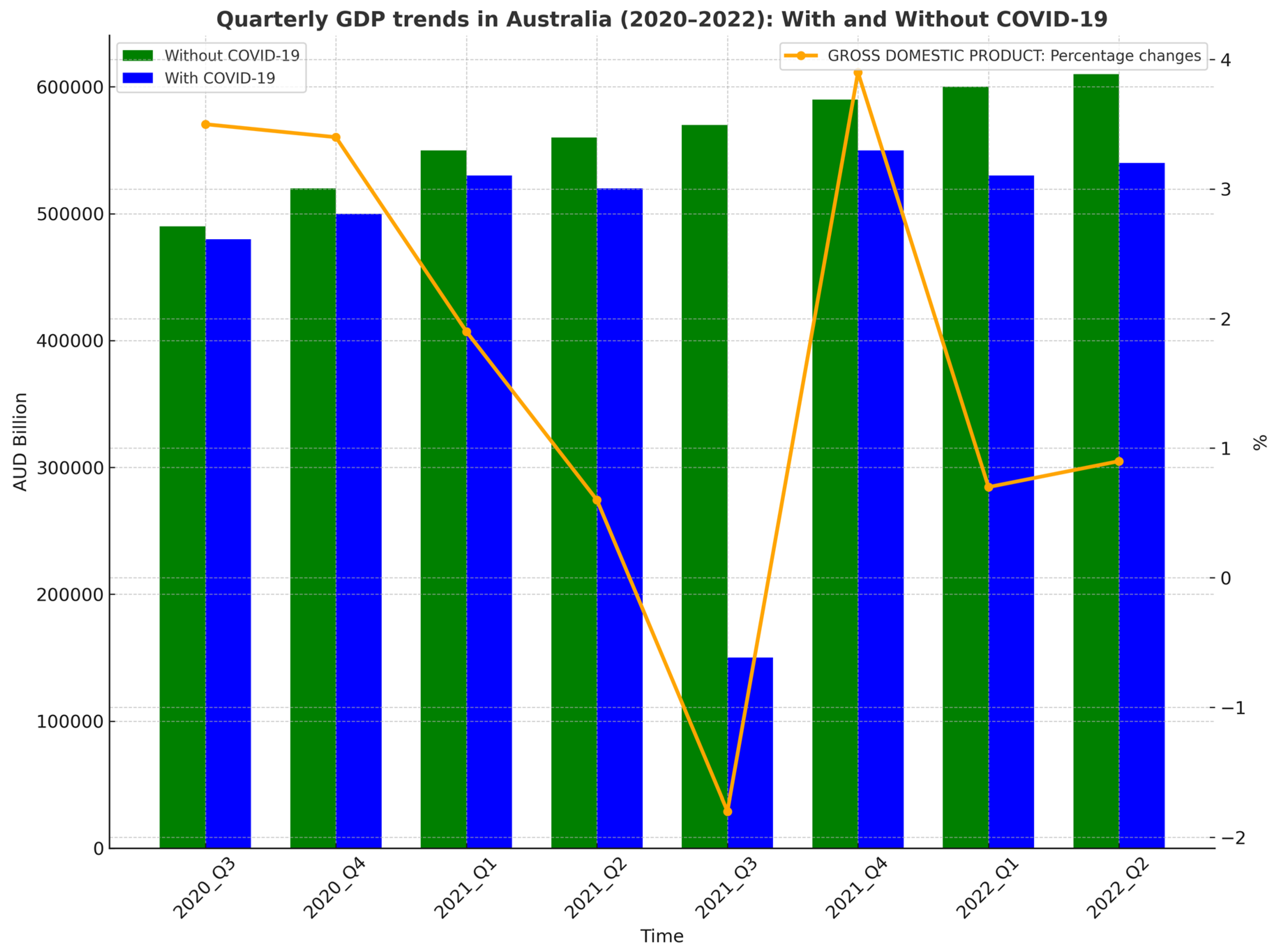
6.3. Indirect Cost
7. Conclusions and Policy Recommendations
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Appendix A
| State | Gross State Product per Capita: 2020 | Total Confirmed Cases 2020 | Natural log of Total Inpatient Admissions | Bed Occupancy Rate | Public Patients (a) | Private Health Insurance | Self-Funded | Workers Compensation | Motor Vehicle Third Party Personal Claim | Department of Veterans’ Affairs | Other (b) | Median Length of Stay for Separations with a COVID-19 Diagnosis 2020–2021 |
| NSW | 76,760 | 4923 | 2049 | 20.72 | 5,260,917 | 3,829,711 | 249,509 | 95,888 | 60,770 | 211,794 | 89,866 | 8 |
| VIC | 70,571 | 20,368 | 737 | 14.95 | 4,557,914 | 2,724,248 | 161,449 | 44,637 | 50,818 | 127,182 | 56,030 | 8 |
| QLD | 70,416 | 1253 | 860 | 12.89 | 3,796,869 | 2,639,012 | 110,933 | 44,213 | 25,842 | 252,390 | 25,588 | 10 |
| SA | 62,821 | 576 | 246 | 4.53 | 1,264,535 | 745,464 | 26,863 | 11,162 | 15,076 | 51,464 | 18,615 | 1 |
| WA | 118,108 | 861 | 297 | 5.83 | 1,755,640 | 1,069,941 | 24,654 | 14,173 | 18,679 | 58,889 | 21,721 | 4 |
| TAS | 61,011 | 234 | 100 | 1.47 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 25 |
| NT | 107,412 | 75 | 39 | 0.98 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 13 |
| ACT | 98,513 | 118 | 140 | 1.15 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 |
| (a) Public hospitals include separations at public psychiatric hospitals. (b) Excludes separation for which the care type was. Notes: Appendix information with notes on definitions and data limitations is available to download at the link below: https://www.aihw.gov.au/reports-data/myhospitals/content/about-the-data (accessed on 12 January 2023). |
Appendix B
| Funding Source | Public Hospitals (a) | Private Hospitals | Total |
| Public patients (b) | 2,336,476 | 42,969 | 2,379,445 |
| Private health insurance | 378,652 | 1,005,473 | 1,384,125 |
| Self-funded | 19,728 | 48,596 | 68,324 |
| Workers’ compensation | 10,792 | 27,071 | 37,863 |
| Motor vehicle third-party personal claim | 17,842 | 2880 | 20,722 |
| Department of Veterans’ Affairs | 26,850 | 44,340 | 71,190 |
| Other (c) | 15,339 | 10,410 | 25,749 |
| Total | 2,805,679 | 1,181,739 | 3,987,418 |
| (a) Public hospitals include separations at public psychiatric hospitals. (b) Public patients include separations with a funding source of health service budget, other hospital or public authority (with a public patient election status), health service budget (due to eligibility for reciprocal health care agreements), and health service budget—no charge raised due to hospital decision (in public hospitals). (c) Other includes separations with a funding source of other compensation, Department of Defence, correctional facilities, other hospital or public authority (without a public patient election status), other, and health service budget—no charge raised due to hospital decision (in private hospitals) and not reported. Notes: Appendix information with notes on definitions and data limitations is available to download at the link below: https://www.aihw.gov.au/reports-data/myhospitals/content/about-the-data (accessed on 12 January 2023). |
| 1 | WHO-CHOICE (Choosing Interventions that are Cost-Effective) is an initiative started by the World Health Organisation in 1998 to help countries choose their healthcare priorities. |
References
- Adam, T., Evans, D. B., & Murray, C. J. (2003). Econometric estimation of country-specific hospital costs. Cost Effectiveness and Resource Allocation, 1, 3. [Google Scholar] [CrossRef] [PubMed]
- Ajmal, M. M., Khan, M., & Shad, M. K. (2021). The global economic cost of coronavirus pandemic: Current and future implications. Public Administration and Policy, 24(3), 290–305. [Google Scholar] [CrossRef]
- Australian Bureau of Statistics. (2022a). Australian national accounts: National income, expenditure and product. Available online: https://www.abs.gov.au/statistics/economy/national-accounts/australian-national-accounts-national-income-expenditure-and-product/jun-2022 (accessed on 15 October 2025).
- Australian Bureau of Statistics. (2022b). Statistics. Australia’s National Statistical Agency. Available online: https://www.abs.gov.au/ (accessed on 15 October 2025).
- Australian Institute of Health and Welfare. (2021). Health expenditure Australia 2019–20. Available online: https://www.aihw.gov.au/reports/health-welfare-expenditure/health-expenditure-australia-2019-20/contents/summary (accessed on 15 October 2025).
- Baldwin, R., & Mauro, B. W. D. (2020). Mitigating the COVID economic crisis: Act fast and do whatever it takes. Centre for Economic Policy Research. ISBN 978-1-912179-29-9. [Google Scholar]
- Beck, E. J., Avila, C., Gerbase, S., Harling, G., & De Lay, P. (2012). Counting the cost of not costing HIV health facilities accurately: Pay now, or pay more later. Pharmacoeconomics, 30(10), 887–902. [Google Scholar] [CrossRef] [PubMed]
- Boissay, F., & Rungcharoenkitkul, P. (2020). Macroeconomic effects of COVID-19: An early review (No. 7). Bank for International Settlements. [Google Scholar]
- Commonwealth of Australia. (2022). Budget strategy and outlook. Commonwealth of Australia. [Google Scholar]
- Debata, B., Patnaik, P., & Mishra, A. (2020). COVID-19 pandemic! It’s impact on people, economy, and environment. Journal of Public Affairs, 20(4), e2372. [Google Scholar] [CrossRef]
- Department of Health and Aged Care. (2022a). Coronavirus (COVID-19) case numbers and statistics. Department of Health and Aged Care. Available online: https://www.health.gov.au/health-alerts/covid-19/case-numbers-and-statistics (accessed on 1 January 2022).
- Department of Health and Aged Care. (2022b). The hierarchy of controls for minimising the risk of COVID-19 transmission. Department of Health and Aged Care. Available online: https://www.health.gov.au/resources/publications/the-hierarchy-of-controls-for-minimising-the-risk-of-covid-19-transmission (accessed on 14 December 2022).
- Eichenbaum, M. S., Rebelo, S., & Trabandt, M. (2021). The macroeconomics of epidemics. The Review of Financial Studies, 34(11), 5149–5187. [Google Scholar] [CrossRef]
- Ghaffari Darab, M., Keshavarz, K., Sadeghi, E., Shahmohamadi, J., & Kavosi, Z. (2021). The economic burden of coronavirus disease 2019 (COVID-19): Evidence from Iran. BMC Health Services Research, 21, 132. [Google Scholar] [CrossRef] [PubMed]
- International Labour Organization. (2021). The impact of the COVID-19 pandemic on jobs and incomes in G20 economies. Available online: https://www.ilo.org/publications/impact-covid-19-pandemic-jobs-and-incomes-g20-economies-0 (accessed on 30 March 2023).
- International Monetary Fund. (2020). Macroeconomic and financial data. International Monetary Fund. Available online: https://www.imf.org/en/Data (accessed on 30 March 2023).
- Jin, H., Wang, H., Li, X., Zheng, W., Ye, S., Zhang, S., Zhou, J., & Pennington, M. (2021). Economic burden of COVID-19, China, January–March 2020: A cost-of-illness study. Bull World Health Organ, 99, 112–124. [Google Scholar] [CrossRef] [PubMed]
- Maliszewska, M., Mattoo, A., & Van Der Mensbrugghe, D. (2020). The potential impact of COVID-19 on GDP and trade: A preliminary assessment (Policy Research Working Paper; No. 9211). World Bank. [Google Scholar]
- Marcolino, M. S., Ziegelmann, P. K., Souza-Silva, M. V., Nascimento, I. J. B. D., Oliveira, L. M., Monteiro, L. S., Sales, T. L., Ruschel, K. B., Martins, K. P., & Etges, A. P. B. (2021). Clinical characteristics and outcomes of patients hospitalized with COVID-19 in Brazil: Results from the Brazilian COVID-19 registry. International Journal of Infectious Diseases, 107, 300–310. [Google Scholar] [CrossRef] [PubMed]
- Mckibbin, W., & Fernando, R. (2020). The global macroeconomic impacts of COVID-19: Seven scenarios. Asian Economic Papers, 20, 1–30. [Google Scholar] [CrossRef]
- Mishra, M. K. (2020). The world after COVID-19 and its impact on global economy. ZBW—Leibniz Information Centre for Economics. Available online: http://hdl.handle.net/10419/215931 (accessed on 2 February 2023).
- Pearson, C. A. B., Bozzani, F., Procter, S. R., Davies, N. G., Huda, M., Jensen, H. T., Keogh-Brown, M., Khalid, M., Sweeney, S., Torres-Rueda, S., Group, C. H. C.-W., Group, C. C.-W., Eggo, R. M., Vassall, A., & Jit, M. (2021). COVID-19 vaccination in Sindh Province, Pakistan: A modelling study of health impact and cost-effectiveness. PLoS Medicine, 18, e1003815. [Google Scholar] [CrossRef] [PubMed]
- Stenberg, K., Lauer, J. A., Gkountouras, G., Fitzpatrick, C., & Stanciole, A. (2018). Econometric estimation of WHO-CHOICE country-specific costs for inpatient and outpatient health service delivery. Cost Effectiveness and Resource Allocation, 16(1), 11. [Google Scholar] [CrossRef] [PubMed]
- Stock, J. H., & Watson, M. W. (2018). Identification and estimation of dynamic causal effects in macroeconomics using external instruments. The Economic Journal, 128(610), 917–948. [Google Scholar] [CrossRef]
- Warren, D. K., Shukla, S. J., Olsen, M. A., Kollef, M. H., Hollenbeak, C. S., Cox, M. J., Cohen, M. M., & Fraser, V. J. (2003). Outcome and attributable cost of ventilator-associated pneumonia among intensive care unit patients in a suburban medical centre. Critical Care Medicine, 31, 1312–1317. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. (2020). WHO COVID-19 preparedness and response progress report—1 February to 30 June 2020. Available online: https://www.who.int/publications/m/item/who-covid-19-preparedness-and-response-progress-report---1-february-to-30-june-2020 (accessed on 1 January 2022).
- World Health Organisation. (2021). WHO COVID-19 dashboard. World Health Organisation. Available online: https://covid19.who.int/ (accessed on 12 December 2021).


| Hierarchy of Control Ranking | Examples of Control Measures to Prevent Transmission | |
|---|---|---|
| Most Effective | Elimination Decrease the opportunities for the virus to spread | Vaccination Testing and quarantine at borders Travel restrictions |
| Substitution Find different approaches to provide care that minimise the risk of transmission. | Physical distancing Symptomatic health workers and agency groups to stay home and not come to work, remote working, telehealth | |
| Less Effective | Engineering controls Use physical barriers and other forms of hazard reduction | Ventilation and improved air changes Registration of all people entering the facility (symptom check, QR code), negative pressure rooms, single room with ensuite, isolation of patients |
| Administrative controls Implement effective and consistent policies and protocols | Audit and feedback, hand hygiene, cleaning and disinfection, signs, posters, information sheets, infection prevention and control guidance documents, training, and education of health workers | |
| Personal protective equipment | Symptomatic patients to wear surgical masks, correct transmission-based precautions, personal protective equipment worn when in contact with infectious patients |
| Risk Category | Treatment Method |
|---|---|
| Mild symptoms | Rest and recover at home. |
| Worsening symptoms | Contact a general practitioner (GP), GP respiratory clinic, or the National Coronavirus Helpline. |
| Severe symptoms | Immediate hospitalisation Authorise a drug, supplemental oxygen, or mechanical ventilation as needed. |
| Cost Categories | Amount (Australian Dollars) | Percentage of Total Cost per COVID-19-Infected Patient |
|---|---|---|
| Human capital cost (International Labour Organization, 2021) | 122 | 14.61 |
| Medicinal consumables | 343 | 40.92 |
| Diagnostic test (Polymerase Chain Reaction (PCR)) | 100 | 11.94 |
| Laboratory tests | 50 | 5.97 |
| Radiological examinations (Computed Tomography scans) | 222 | 26.52 |
| Total cost per COVID-19-infected patient | 836 | |
| Total inpatient cost of COVID-19 (TC * No. of patients for a year) in 2021 (based on 4473 patients) | 3,738,974.089 |
| Cost Component | Nature of Cost | Amount (AUD) | Allocation Method |
|---|---|---|---|
| Human capital cost | Daily recurring | 122.33 | Per day |
| Medicinal consumables | Daily recurring | 342.50 | Per day |
| Diagnostic test (Polymerase Chain Reaction (PCR)) | Daily recurring | 50.00 | Per day |
| Laboratory tests | One-off episode | 100.00 | spread over ALOS |
| Radiological examinations | One-off episode | 222.00 | spread over ALOS |
| State | ALOS (Days) | Total Inpatient Admissions | Adjusted Total Cost (AUD) |
|---|---|---|---|
| South Australia | 1 | 246 | 137,753.00 |
| Victoria | 8 | 737 | 3,301,583.00 |
| New South Wales | 8 | 2049 | 9,179,028.00 |
| Queensland | 10 | 860 | 4,815,742.00 |
| Tasmania | 25 | 100 | 1,399,925 |
| Western Australia | 4 | 297 | 665,244.4 |
| Northern Territory | 13 | 39 | 665,244.36 |
| Australian Capital Territory | 2 | 140 | 283,904.79 |
| Variable | Regression Coefficient | p Value |
|---|---|---|
| Ln GDP per capita | 0.2786 (0.0941) | 0.0042 |
| Ln occupancy rate | 1.0506 (0.1173) | 0.0010 |
| Ln ALOS | −0.0422 (0.0046) | 0.0017 |
| Ln admissions | 0.0140 (0.0017) | 0.0290 |
| Dummy H1—public hospital | −0.1125 (0.0507) | 0.1490 |
| Dummy H2—private hospital | 0.1101 (0.0756) | 0.0010 |
| R2 | 0.6980 | |
| Adjusted R2 | 0.6850 | |
| F-stat | 251.0800 (0.0040) | |
| Durbin–Watson stat | 1.5650 |
| Variable | Coefficient Variance | Uncentered VIF | Centred VIF |
|---|---|---|---|
| Ln GDP per capita | 0.0089 | 3.25 | 1.85 |
| Ln occupancy rate | 0.0138 | 4.10 | 2.10 |
| Ln ALOS | 0.0001 | 2.50 | 1.65 |
| Ln admissions | 0.0001 | 4.55 | 2.25 |
| public hospital | 0.0026 | 1.20 | 1.15 |
| private hospital | 0.0057 | 1.15 | 1.10 |
| Heteroskedasticity Test: Breusch–Pagan–Godfrey | |||
|---|---|---|---|
| F-statistic | 1.2700 | Prob. F(6,2) | 0.2740 |
| Obs*R-squared | 8.7200 | Prob. Chi-Square(6) | 0.1930 |
| Scaled explained SS | 0.7980 | Prob. Chi-Square(6) | 0.2450 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rathnayaka, I.W.; Khanam, R.; Rahman, M.M. Cost Analysis of COVID-19 in Australia. Economies 2025, 13, 305. https://doi.org/10.3390/economies13110305
Rathnayaka IW, Khanam R, Rahman MM. Cost Analysis of COVID-19 in Australia. Economies. 2025; 13(11):305. https://doi.org/10.3390/economies13110305
Chicago/Turabian StyleRathnayaka, Imalka Wasana, Rasheda Khanam, and Mohammad Mafizur Rahman. 2025. "Cost Analysis of COVID-19 in Australia" Economies 13, no. 11: 305. https://doi.org/10.3390/economies13110305
APA StyleRathnayaka, I. W., Khanam, R., & Rahman, M. M. (2025). Cost Analysis of COVID-19 in Australia. Economies, 13(11), 305. https://doi.org/10.3390/economies13110305








