Abstract
In recent decades, China has experienced rapid economic growth and rising health inequality. The government has introduced a nationwide health care reform aimed at achieving affordable and equitable basic health care for all. This paper investigates income-related inequality in health care utilization and out-of-pocket (OOP) payments and explores the underlying factors that drive the inequalities. Using data running from 2000 to 2015 and covering nine of thirty-one provinces in China, we calculate indices to measure income-related inequality and adopt a regression-based decomposition approach to explore the sources of inequality. We find pro-rich inequality in the use of preventive care and pro-poor inequality in the use of folk doctors. In addition, the better-off have preferential access to higher level hospitals, while the use of primary care facilities is more concentrated among the poor. The poor are also found to face a heavier financial burden since they tend to spend a larger share of their income on OOP payments. Education, employment and geographic regions all appear to contribute to the total inequality. Our results indicate that affordability remains a common barrier for the poor to access health care, and that the inequality is largely driven by socio-economic factors.
1. Introduction
Many low- and middle-income countries are seeking ways to pursue the goal of equity in health care utilization. The Chinese experience is important to understand how health care inequality changed during the course of a transition from a command to a market economy. China’s market-oriented reforms in the late 1970s brought higher efficiency in the economy and dramatically increased household income; however, they also led to health inequalities due to market failures in health sectors and the removal of social health insurance as a safety net. Health care financing relied heavily on out-of-pocket (OOP) payments, and the poor usually had limited access to necessary health services (Gong and Brixi 2005). Both demand-side subsidies and supply-side infrastructure investments disproportionately served the better-off (Wagstaff et al. 2009), leading to a widening gap in health status and utilization across income groups (Liu et al. 1999; Gao et al. 2002; Zhang and Kanbur 2005; Tang et al. 2008; Wagstaff 2009a). Along with aging and disease transitions from infectious to chronic conditions, the poor were far more vulnerable to the financial and physical consequences of illness.
In response to increasing pressure for equitable access to quality care, from the end of the 1990s onwards the Chinese government introduced a series of health care reforms that incorporated a number of pro-poor measures. Since the effects of these health care reforms differ across income groups, it is important to examine the pre- and post-reform changes in the distribution of health care utilization and medical expenditure and to estimate the contributions of various factors to the observed inequality. An increasing body of studies in recent years attempted to compare the income-related inequality in terms of the use of outpatient and inpatient care (Wang et al. 2012; Xie 2011; Zhang et al. 2015; Zhou et al. 2011; Chen et al. 2015), preventive care (Yang 2013), maternal health services (Li et al. 2015; Shen et al. 2014) and treatment of major chronic conditions (Elwell-Sutton et al. 2013; Xie et al. 2014). Previous evidence showed that the health care reforms were characterised by an overall improvement in insurance coverage, but the rich still seemed to have better access to health care compared to the poor. The impact of health insurance on financial protection appeared to be limited, and in some cases there was even a widening of social disparities in health care access among the insured.
While previous studies have provided important insights into the socio-economic differentials in health care access, most of them focus on either earlier periods of the health care reforms or a limited number of geographic regions, so that we still know little about the longer term trends for the total population following the reforms. In this paper, we use a recent dataset over a 15-year period from 2000 to 2015 to capture the long-term impact of policy changes. The data also cover nine provinces that spread across the eastern, middle and western areas of China, and therefore provide a much broader picture of health care inequality. We assess the evolution of health care inequality and its determinants during the period of rapid economic development and the implementation of the nationwide health care reforms. By examining how types of health services and choice of facilities differ among people with different income levels, we explore both financial and non-financial access barriers related to insurance coverage and quality of care. We calculate both rank- and level-dependent indices to measure income-related inequality and to obtain robust results (Erreygers and Kessels 2017). We also adopt a direct regression-based decomposition of inequality indices to explore the sources of inequality, taking into account the correlation of health and income (Kessels and Erreygers 2019). Our empirical findings could feed back into the policy making process in China and other developing countries to move towards an efficient and equitable health care system.
2. Background
The Chinese government launched three main social health schemes to achieve universal coverage: the Urban Employee Basic Medical Insurance (UEBMI) for the urban employees and retirees, the New Cooperative Medical Scheme (NCMS) for the rural residents and the Urban Resident Basic Medical Insurance (URBMI) for the unemployed urban population (including students and children). Initiated in 1998, UEBMI is a compulsory scheme based on employment, but it only provides coverage to formal-sector workers in urban areas and leaves the majority of the population uninsured. During the 2000s, two new voluntary insurance schemes were introduced, both of which were heavily subsidised by the central and local governments. The NCMS was launched in 2003 and expanded rapidly from 13 to 97.5% of the rural population of about 800 million between 2003 and 2008 (Yang and Wu 2017). The URBMI targeted 420 million urban residents who were not covered by the UEBMI (e.g., the elderly, students, children and the unemployed) and was first implemented in 79 pilot cities in 2007 (Dong 2009). It was then extended to other cities and covered about 49% of urban residents in 2015 (Si 2021). Universal coverage was nearly achieved under these three schemes by the end of 2015, but the reimbursement and types of services covered remained limited. The benefit packages varied geographically, but a typical package covered inpatient services and catastrophic outpatient services. Beneficiaries needed to bear most of their outpatient expenses and about half of their inpatient costs. The average reimbursement rates for inpatient care ranged from 65–68% for the UEBMI, 44–48% for the URBMI and 38–44% for the NCMS, considering the deductibles, co-payments and reimbursement cap (Yip et al. 2012). Over time, the government aimed to gradually extend insurance coverage to more types of care and to reduce co-payments. The central government also assisted local governments in relatively poor regions of western and middle provinces, while the funding of insurance premiums fell solely on local governments in eastern provinces.
With effective risk-sharing at the community/city level, the insurance schemes have the potential to offer better protection for individuals from low- and middle-income backgrounds. In addition, the insurance reimbursement varies with the level and type of health facilities, with much more generous reimbursement rates for low-level facilities. The various reimbursement rate schedules provide incentives for people to seek care from primary care facilities and purchase generic drugs in order to contain overall medical costs. However, due to inadequate resources and insufficient medical training, primary care facilities tend to provide low quality care and are more likely to misdiagnose or inappropriately treat their patients (Sylvia et al. 2014; Li et al. 2017a; Sylvia et al. 2017; Wong et al. 2017). During the past decades, they mainly catered for economically disadvantaged patients, who are highly price-elastic and tend to compromise on quality. In absence of a strict referral or gatekeeping health care system, wealthy patients would rather bypass primary care and seek care at high-level hospitals even for minor conditions (Babiarz et al. 2010; Sylvia et al. 2017). To strengthen the primary care system, recent reforms increased government funding for community health centres in cities and township health centres and village clinics in rural areas. A number of measures, such as imposing strict licensing requirements and promoting regular in-service medical trainings, were implemented to update the clinicians’ professional knowledge and skills that are essential to the provision of appropriate patient care (Yi et al. 2020). These measures encourage people to switch from hospitals to primary care facilities and aim to benefit more low-income households. Therefore, both the demand- and supply-side measures have the potential to improve the general population’s access to health care and to reduce socio-economic disparities in health and health care.
3. Methodology
3.1. Data and Variables
We use data from the China Health and Nutrition Survey (CHNS), a large-scale panel dataset that employed a multi-stage stratified sampling method to select households from 12 provinces and municipal cities in China, spread across the eastern, central and western regions. The selected households were followed for 10 waves (from 1989 to 2015), and surveyed on a wide range of topics including demographics, socio-economic characteristics and health outcomes (Popkin et al. 2010).
In this study, we use six waves of data from 2000 to 2015 and exclude three newly added municipal cities from 2011. Data before 2000 are not used since the structure of the early questionnaires was different from that of the following waves. We measure income-related inequality for the use of different types of health services (formal medical care, preventive care, folk doctors and inpatient care) and different levels of health facilities (from low-level to high-level facilities: village clinics/community health centres, township health centres, county hospitals and city hospitals). We also consider the burden of OOP payments, defined as the proportion of the OOP payments in the last month to the total monthly per capita household income following previous literature (Wagstaff and Lindelow 2008). We censored the maximum value of this variable at 100% in order to eliminate extremely high OOP values for individuals belonging to households with a very low income (3.25% of the sample). To measure living standards, we adjust household income by applying the Organisation for Economic Co-operation and Development (OECD)-modified equivalence scale to household income, assigning a value of 1 to the household head, 0.5 to each additional adult and 0.3 to each child (OECD n.d.). The CHNS income measure is net monetary income received by the household members and includes income from farming, fishing, gardening, livestock and small commercial household business. Notice that we exclude households with negative income, so the final sample size consists of 24,762 individuals, 6789 households and 67,856 person-wave observations. About 34.9% of respondents were only interviewed once in the survey, 20.2% twice, 13.8% three times, 9.8% four times, 10.2% five times, and 11.3% in all waves. The attrition rate is quite high, and individuals reporting more use of formal medical care and higher level of OOP payments were more likely to drop out of the sample.
In the decomposition analysis we explore how the major determinants of individuals’ care-seeking behaviour are associated with income-related health inequality. We look at health-related (number of major diseases, number of symptoms and illness status during the past four weeks preceding the survey), demographic (age, gender, number of children, ethnicity, urban/rural residential status, marital status) and socio-economic characteristics (house ownership, education levels, employment, occupation, social health insurance coverage and geographics). Specifically, health status is thought to be the most important factor that drives utilization of health care. Since self-rated health status is not available in the CHNS 2009 and 2011 surveys, we use the number of major diseases and illness status during the past four weeks preceding the survey as proxy variables for patients’ health status (O’Donnell and Propper 1991; Van Doorslaer et al. 1992). We create 14 variables by interacting age categories with gender and control for other demographics such as ethnicity, urban/rural residential status, marital status. The socio-economic characteristics include house ownership, education levels and job status. Household ownership can be a good indicator of the households’ wealth level in addition to income, especially for rural households who live from subsistence farming and have little or no income. Better education can either lead to an increase in health care use or better health status that results in lower needs for health care. Job status is particularly relevant in the Chinese context since most state welfare benefits (including UEBMI) are associated with the types of industry. For example, we would expect that state government officials are more likely than self-employed businessmen to have better access to health care facilities because they are granted more generous state welfare benefits. We also investigate the impact of geographic factors by dividing the nine provinces into three groups: eastern, middle and western regions. The eastern coastal area is generally more affluent and supplied with better quality medical infrastructures and services than the middle and western areas. The coverage of the three social health insurance schemes is also included: UEBMI and URBMI for urban residents and NCMS for rural residents. Table 1 shows the definitions of all variables and their summary statistics.

Table 1.
Number of observations, mean, standard deviation of all variables, pooling all years from 2000 to 2015.
3.2. Measurement of Inequality
Our first goal in this paper is to measure to what extent the health outcomes we have selected are related to incomes, and to examine whether and how these relationships have changed over the study period. Put differently: is there any evidence that wealthy people tend to have better access to health services than poor people, and have the health reforms changed anything? It is customary to use indices to measure the degree of socioeconomic inequality. Since we are looking at the joint distribution of health and income, the indices must be of the bivariate type. Positive index values indicate that health and income are positively correlated, and negative values that they are negatively correlated. Due to a lack of reliability in self-reported health measures in the setting of low-income countries (Van Doorslaer and O’Donnell 2011), we focus on measuring inequality in the allocation of health care resources without standardizing for the differences in health needs.
Broadly speaking, two types of bivariate indices of socioeconomic inequality of health can be distinguished: rank-dependent indices, such as the well-known concentration index (CI) (Wagstaff et al. 1991), and level-dependent indices. Rank-dependent indices measure the degree of correlation between health levels and income ranks, and can be expressed as weighted sums of health levels, where the weights are defined by a function of the income ranks (Coveney et al. 2016). The standard (or relative) CI is usually applied to non-negative ratio-scale health variables (Erreygers and Van Ourti 2011). Given that our health care and OOP burden variables are bounded variables, we use a modified version of the CI developed for bounded health variables (Erreygers 2009; Erreygers and Van Ourti 2011). However, since rank-dependent indices only rely on income ranks, they ignore relevant information about the levels of income (Erreygers and Kessels 2017). Level-dependent indices are similar to rank-dependent indices, but take into account the income levels rather than the income ranks. They too can be expressed as weighted sums of health levels, but the weights are now determined by a function of the income levels. These indices exploit more information about the income distribution and measure both income and health consistently by their levels. Additionally, in this case we have to use a modified version appropriate for bounded variables. The precise definitions of the indices calculated in this paper can be found in Appendix A.
3.3. Decomposition of Inequality
Our second goal is to increase our understanding of the determinants of income-related inequalities. To this end, we decompose the inequality indices by means of demographic, socio-economic and health-related variables at the individual level. The conventional regression-based decomposition approach rests on a regression of the health variable only (Wagstaff et al. 2003), and for this reason has been subjected to criticism (Erreygers and Kessels 2013). In recent years, two alternative methods have been developed. The first is based on the recentred influence function approach (Heckley et al. 2016) and has already been applied to Chinese data (Cai et al. 2017). In this study we employ a new approach, based on a regression of a composite variable that incorporates both health and income (Kessels and Erreygers 2019). The idea is that this variable can be interpreted as an indicator of an individual’s deviation from a reference position in the income-health space, with the reference position determined by average health and average income. The exact definitions of the dependent variables of our decomposition regressions can be found in Appendix A.
We apply ordinary least square (OLS) regressions to estimate the marginal effects of each individual variable on the inequality index. Previous studies found there is little difference between OLS and non-linear models for decomposition analysis, while the approximation techniques required by non-linear models might introduce additional errors (Van Doorslaer et al. 2004; Van Doorslaer and Masseria 2004; Van Doorslaer et al. 2000). A positive (negative) regression coefficient means that the associated explanatory variable is positively (negatively) correlated with both income and health. In contrast to what is often done in applications of the conventional regression-based decomposition technique, we do not estimate the contribution of each factor to the inequality indices. Instead, we calculate the logworth values based on the p value of the F tests to evaluate the relative importance of the (groups of) variables in influencing the correlation between the income and health dimensions.
4. Results
4.1. Income-Related Inequality in Health Care Utilization and OOP Burden
Table 2 and Table 3 present the rank- and level-dependent indices measuring income-related inequality for health care utilization and OOP burden. Broadly speaking, both rank- and level-dependent indices give similar results in terms of the direction of inequality and its significance. There is substantial pro-rich inequality in the use of preventive care and pro-poor inequality in the use of folk doctors. The results suggest that low-income people have limited access to preventive services and are more likely to use folk doctors, who are traditional Chinese medical practitioners in rural areas. They are usually less qualified providers who received minimal basic medical and paramedical training and had no more than middle or high school education (Li et al. 2017b). They offer cheaper services compared to formal health providers, but also tend to conduct unnecessary or even dangerous practices. However, some folk doctor care also includes traditional Chinese medicine, which is considered appropriate in some clinical settings (Cui et al. 2004; Chen et al. 2008; Xiang et al. 2019; Harmsworth and Lewith 2001).

Table 2.
Rank-dependent indices for income-related inequality of health care utilization and medical expenditure in China.

Table 3.
Level-dependent indices for income-related inequality of health care utilization and medical expenditure in China.
Significant values of the inequality indices are found for the health categories preventive care, folk doctors, village clinics/community health centres, and city hospitals. For clarity we represent the values in Figure 1 and Figure 2, respectively for rank-dependent indices and level-dependent indices. In terms of health facility use, the direction of inequality varies by provider levels where pro-poor inequality is observed for the use of village clinics/community health centres and pro-rich inequality for the use of city hospitals. Wealthier people seem to have better access to high-level hospitals that offer more sophisticated care and require higher OOP expenditures.
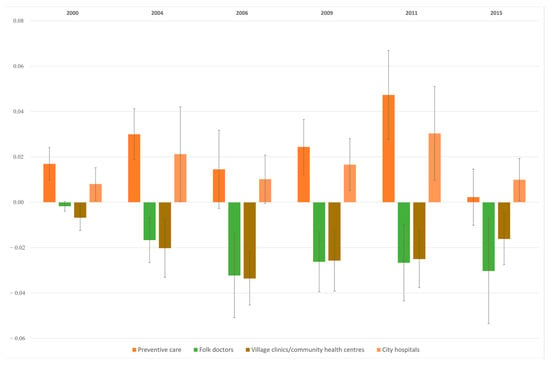
Figure 1.
Rank-dependent indices for income-related inequality of health care utilization in China.
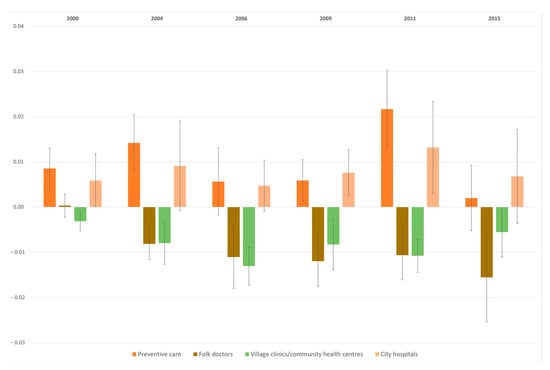
Figure 2.
Level-dependent indices for income-related inequality of health care utilization in China.
Even though the rich tend to use more expensive health care facilities than the poor, OOP expenditures seem to impose a higher weight on the poor than on the rich. As we defined the OOP burden as the proportion of the absolute amount of OOP payments relative to the per capita household income, a pro-poor distribution of the OOP burden indicates that in relative terms OOP expenditures tend to fall more heavily on the poor than on the rich (see Figure 3). In spite of the rapid expansion of social health insurance and other health care reform efforts, the disparities in health care utilization across incomes remain similar over time.
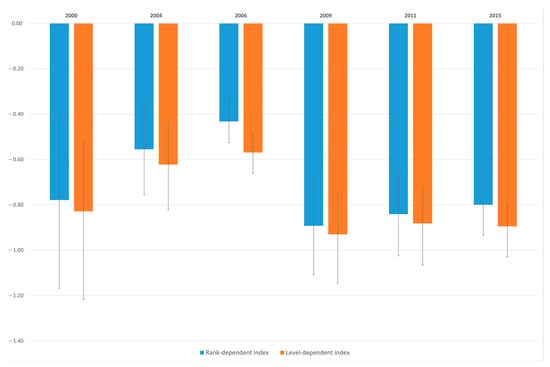
Figure 3.
Rank- and level-dependent indices for income-related inequality of OOP burden in China.
4.2. Decomposition of Income-Related Inequality in OOP Burden
The regression-based decomposition analysis we introduced above can be applied to income-related inequality of both health care utilization and OOP burden, allowing us to identify which covariates have a significant effect on each form of inequality. Here, we apply it to the burden of OOP only. Note that since OOP burden is a bounded ill-health variable, we have to define the dependent variable of our regression as explained in Appendix A. Income is excluded as an explanatory variable since it would distort the explanation of the correlation between income and health (Erreygers and Kessels 2013). For each wave of the survey we estimate two regressions, one for the rank-dependent index and the other for the level-dependent index, based on the same set of independent variables. We present both the marginal effects and the logworth values for key covariates to assess their importance as explanatory variables in Table 4 (rank-dependent indices) and Table 5 (level-dependent indices). The full results of all covariates can be found in Appendix B. A logworth value larger than 1.3 indicates that a variable (or group of variables) is significant at the 5% level and a logworth value above 2 indicates significance at the 1% level. For variables with more than two categories, the logworth values are combined over the categories.

Table 4.
Effect of selected demographic and socioeconomic variables in the decomposition of the rank-dependent indices for OOP burden.

Table 5.
Effect of selected demographic and socioeconomic variables in the decomposition of the level-dependent indices for OOP burden.
Demographic and socio-economic factors such as education levels, employment status, occupation, residential regions, are among the most important determinants of income-related inequality in OOP burden across all years. Positive coefficients indicate that variables have a positive marginal effect on the observed inequality, i.e., tend to make income-related inequality of OOP burden less pro-poor, and the opposite holds for negative coefficients. For example, suffering from more major diseases tends to make income-related inequality of OOP burden more pro-poor, although the effect is often insignificant. The magnitudes of the coefficients in the decomposition of the level-dependent index in 2015 appear to be larger than the ones in other years. This might be due to the relatively high values of the OOP payments and household incomes in 2015. For both indices, factors that contribute to more pronounced pro-poor inequality in OOP burden seem to be higher education levels, being employed, having white-collar jobs and living in cities, given that the marginal effects of the associated variables are all negative. Social health insurance coverage appears to reduce the pro-poor inequality in OOP burden in some of the years, but in others the effects remain rather limited.
5. Discussion
The measurement and explanation of income-related inequality in health care attracts much policy interest, especially if reducing health inequality is high on the agenda. In this study, we track changes in the distribution of health care resources across income levels over a 15-year period, during which the government adopted a series of measures that gradually led to a profound reform of the health care system in China. We also explore the influence of various factors (e.g., demographic, socio-economic and health-related characteristics) on inequality.
Our study provides fresh evidence on the uneven access to health care and facilities. The results for the two types of indices we have used to estimate the extent of income-related inequality of health point in the same direction: high-income people tend to obtain more preventive care and use more hospital services, while low-income patients mostly seek care from village clinics/community health centres and folk doctors. The gap of preventive care between the rich and poor might be due to the fact that preventive care is only partially reimbursed by insurance and requires more cost-sharing. Although folk doctor care is not covered by insurance either, it is usually less costly and more accessible compared with hospital services, especially in remote rural areas. This utilization pattern is consistent with evidence from developed countries, with a pro-poor distribution in primary care use and pro-rich distribution in the use of specialised care (Van Doorslaer et al. 2000; Van Doorslaer et al. 2004; Van Doorslaer and Masseria 2004). The pro-poor distribution of the OOP burden is in line with the findings of utilization patterns, indicating that affordability remains a common barrier for the poor to access health care. Further decomposition analysis of the pro-poor inequality in OOP burden suggests that the inequality is largely driven by demographic and socio-economic factors. Higher levels of education, employment and occupation tend to be associated with a larger extent of pro-poor inequality of the OOP burden. In line with the findings of previous research, our results suggest that the recent expansion of social health insurance has a limited impact on the reduction of this inequality (Coté et al. 2013; Cai et al. 2017).
The study findings need to be interpreted in the light of the following limitations. First, we use equivalised household income to measure living standard, but in low- and middle-income countries income is not always a dependable indicator of a household’s socioeconomic status, especially when day labour with volatile incomes and subsistence farming and fishing are common (Wagstaff 2009b; Wagstaff et al. 2003). However, in the context of China, income measures were regarded as more reliable than household expenditure since expenditure data might be distorted by the high saving rates of Chinese households (Sun et al. 2010; Yang 2013). Second, the nine provinces included in our analyses vary considerably in terms of demographics and economic development levels, so that comparing households’ incomes in fairly rich and prosperous areas in the eastern region with those in worse-off and more rural areas without accounting for the differences in purchasing power might be problematic. Third, although the data have a longitudinal (panel) structure, this feature is not exploited in the empirical analysis since health care utilization was only reported by people who fell sick during the study period. Therefore, our results indicate the association between income-related inequality in the burden of OOP payments and various demographic and socio-economic characteristics and do not intend to obtain causal inference. Fourth, in the survey OOP payments are reported for the last four weeks only, and therefore there is a high risk of random high expenditure and random zero expenditure. Previous literature also pointed out that CHNS has a much lower OOP level on average compared to other household surveys in China because it might ignore the expenditure of people who were still in hospital at the time of the interview (Wagstaff and Lindelow 2008). However, with a longer reporting period (e.g., one year), OOP might also suffer from recall bias. As far as OOP payments are concerned, data on the previous month is the only source we could obtain. We need to bear in mind that we might underestimate or overestimate the OOP burden given the limitations stated above. Fifth, health care utilization behaviour is usually shaped by both financial (e.g., price elasticity, income levels, insurance coverage) and non-financial factors (e.g., health care need, quality of care, availability of transportation, health care personnel and infrastructure). In this paper, we focus on financial access to care, but evidence is lacking with respect to whether or not the health care reforms led to any change in non-financial access barriers and how this varied across different socioeconomic groups. Finally, primary care facilities and high-level specialised hospitals tend to serve different types of patients so that the observed inequality in facility use might also be related with differential levels of health care needs across income. It would be valuable to obtain more objective and reliable quality measurements for a rigorous assessment of the scale of inequality in health care use. The above issues could be the subject of future research through well-designed surveys and field studies conducted in more recent years.
6. Conclusions
Inequality in health care is a common challenge worldwide, especially in low- and middle-income countries that are looking for means of ensuring access to basic health care and protecting poor patients from health payment-induced impoverishment. Our findings have high relevance in the debate over the use of publicly sponsored health insurance programmes in tackling income dependence of health care use in China and other developing countries. An important policy lesson drawn from the study is that broad insurance coverage at population level does not necessarily lead to equal access to good quality health care. Our findings show there are still inequalities in the use of preventive care and hospital services across people from different income groups, indicating that the poor are faced with a heavy financial burden due to high insurance co-payments and insufficient coverage. Insufficient coverage of preventive care among the poor could lead to a disease-poverty trap as minor conditions would develop into severe illnesses that require specialist care from high-level hospitals and long-term use of medication (Xu et al. 2007). Early detection through screening or diagnostic tests could be a more cost-effective strategy compared with expensive acute care to tackle the challenges of the recent epidemiological transitions from infectious diseases to non-communicable diseases. Therefore, preventive care should be an integral part of a comprehensive insurance coverage to adjust for the socio-economic gradient in disease burdens (Yang 2013). To reduce the socio-economic gap in the access to health services, it is important to extend benefit packages to preventive care and hospital services. The expansion can be achieved incrementally as government subsidies and insurance premiums increase over the years, so that the means to extend the types of services covered by the insurance are compatible with the means to achieve equity. In addition, a well-functioning primary care system would provide more affordable and good-quality health care for patients from vulnerable socio-economic groups. Compared to investing most of the public resources in specialised hospitals, strengthening the delivery of basic needs-oriented primary care is a more viable way to benefit the majority of the patients.
In recent years, the Chinese government has attached greater importance to achieving a more balanced allocation of resources to primary care clinics and high-level hospitals by increasing funding for strengthening community health centres in cities and village clinics and township hospitals in rural areas. However, there is still a lack of well-trained personnel in many primary care facilities so that they cannot sufficiently meet the needs of the wide population (Mossialos et al. 2016). A comprehensive insurance coverage for health services combined with a strong primary care delivery system could help reduce disparities in health and health care across incomes. Even though Chinese policymakers have already started to address some of the issues identified above, stronger and more positive policy responses still need to be developed to close the socioeconomic gap in the access to health resources.
Author Contributions
Conceptualization, M.Y. and G.E.; methodology, M.Y. and G.E.; formal analysis, M.Y. and G.E.; data curation, M.Y.; writing—original draft preparation, M.Y.; writing—review and editing, G.E.; funding acquisition, M.Y. and G.E. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by PhD scholarship from the Lancaster University Management School.
Informed Consent Statement
The data collectors of the China Health and Nutrition Survey (CHNS) obtained informed consent from all subjects involved in the study.
Data Availability Statement
The data used by this study are publicly available at: http://www.cpc.unc.edu/projects/china. Data were accessed and downloaded in January 2020.
Acknowledgments
Financial support by PhD scholarship from Lancaster University Management School is gratefully acknowledged. This research uses data from China Health and Nutrition Survey (CHNS). We thank the National Institute for Nutrition and Health, China Centre for Disease Control and Prevention, Carolina Population Centre (P2C HD050924, T32 HD007168), the University of North Carolina at Chapel Hill, the NIH (R01-HD30880, DK056350, R24 HD050924, and R01-HD38700) and the NIH Fogarty International Centre (D43 TW009077, D43 TW007709) for financial support for the CHNS data collection and analysis files from 1989 to 2015 and future surveys, and the China-Japan Friendship Hospital, Ministry of Health for support for CHNS 2009, Chinese National Human Genome Centre at Shanghai since 2009, and Beijing Municipal Centre for Disease Prevention and Control since 2011.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Appendix A
In this appendix we provide the formulas of the indices we have calculated and of the dependent variables we have used in the regression-based decompositions. More details can be found in Kessels and Erreygers (2019).
We consider a population of n individuals, labelled by the subscript i = 1, 2, …, n. Let h stand for health, y for income, and r for income rank (with the poorest person having rank 1, the second poorest rank 2, etc.). Since all health outcome variables of the paper are bounded between 0 and 1, we have used the bounded-variable versions of the indices. The rank-dependent index is equal to:
while the level-dependent index is equal to:
where represents mean income.
The decomposition analysis in the paper is applied to OOP burden, which is an ill-health variable. Let z be this variable. The dependent variable of the decomposition regression for the rank-dependent index is then defined as:
where is the mean of the ill-health variable. Likewise, the dependent variable of the decomposition regression for the level-dependent index is equal to:
Appendix B

Table A1.
Effect of selected demographic and socioeconomic variables in the decomposition of the rank-dependent indices for OOP burden (full results).
Table A1.
Effect of selected demographic and socioeconomic variables in the decomposition of the rank-dependent indices for OOP burden (full results).
| 2000 | 2004 | 2006 | 2009 | 2011 | 2015 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable 1 | Coefficient | Logworth | Coefficient | Logworth | Coefficient | Logworth | Coefficient | Logworth | Coefficient | Logworth | Coefficient | Logworth |
| Female × age 18 below | −0.006 | 22.03 | −0.028 | 10.84 | 0.000 | 3.93 | −0.006 | 3.81 | −0.016 | 5.91 | 0.055 | 8.74 |
| Female × age 18–24 | −0.001 | 0.003 | 0.007 | 0.000 | 0.005 | −0.006 | ||||||
| Female × age 25–34 | 0.004 | 0.002 | 0.010 | 0.000 | 0.004 | 0.000 | ||||||
| Female × age 35–44 | 0.003 | 0.003 | 0.006 | −0.003 | 0.005 | 0.006 | ||||||
| Female × age 45–54 | −0.005 | −0.004 | 0.003 | −0.005 | 0.001 | 0.005 | ||||||
| Female × age 55–64 | 0.000 | −0.008 | 0.003 | −0.010 | −0.005 | 0.006 | ||||||
| Female × age 65 above | 0.012 | −0.001 | 0.003 | −0.009 | 0.000 | 0.008 | ||||||
| Male × age 18–24 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | ||||||
| Male × age 25–34 | 0.007 | 0.008 | 0.009 | 0.000 | −0.001 | 0.006 | ||||||
| Male × age 35–44 | 0.015 | 0.008 | 0.010 | 0.000 | 0.006 | 0.007 | ||||||
| Male × age 45–54 | 0.003 | 0.004 | 0.009 | 0.000 | 0.007 | 0.009 | ||||||
| Male × age 55–64 | 0.006 | 0.000 | 0.008 | −0.001 | 0.003 | 0.012 | ||||||
| Male × age 65 above | 0.014 | 0.003 | 0.007 | −0.004 | 0.004 | 0.012 | ||||||
| Number of major diseases | −0.002 | 0.52 | 0.000 | 0.15 | −0.001 | 0.60 | −0.001 | 0.83 | 0.000 | 0.22 | −0.001 | 0.49 |
| Sickness in the last month | 0.013 | 3.72 | 0.010 | 7.74 | 0.013 | 12.72 | 0.013 | 13.26 | 0.015 | 14.12 | 0.012 | 11.88 |
| Number of symptoms in the last month | 0.011 | 5.47 | 0.006 | 9.91 | 0.003 | 2.38 | 0.002 | 1.59 | 0.002 | 1.10 | 0.003 | 2.69 |
| Private dwelling | −0.004 | 1.45 | −0.005 | 2.32 | −0.003 | 1.05 | −0.013 | 9.87 | −0.007 | 4.72 | −0.007 | 4.90 |
| Social health insurance | −0.013 | 6.11 | −0.007 | 3.58 | −0.008 | 15.94 | −0.002 | 1.26 | −0.004 | 2.18 | 0.002 | 0.70 |
| Ethnicity | −0.013 | 14.85 | −0.005 | 3.18 | −0.002 | 0.86 | −0.001 | 0.47 | −0.009 | 8.94 | −0.008 | 7.95 |
| Marital status | −0.001 | 0.34 | −0.005 | 3.21 | −0.007 | 7.15 | −0.009 | 10.97 | −0.013 | 22.46 | −0.011 | 14.57 |
| Primary school | −0.009 | 35.44 | −0.006 | 51.53 | −0.005 | 64.32 | −0.006 | 51.27 | −0.007 | 55.83 | −0.006 | 40.49 |
| Junior high school | −0.013 | −0.011 | −0.011 | −0.011 | −0.012 | −0.010 | ||||||
| Senior high school or above | −0.021 | −0.022 | −0.023 | −0.023 | −0.020 | −0.017 | ||||||
| University degree | −0.039 | −0.039 | −0.037 | −0.035 | −0.035 | −0.030 | ||||||
| In employment | −0.015 | 20.89 | −0.016 | 33.38 | −0.013 | 21.96 | −0.016 | 32.83 | −0.014 | 25.10 | −0.013 | 24.27 |
| White collar worker | −0.010 | 5.77 | −0.012 | 9.67 | −0.012 | 9.95 | −0.010 | 6.15 | −0.009 | 6.26 | −0.011 | 8.65 |
| Farmer | 0.025 | 61.17 | 0.016 | 28.33 | 0.012 | 16.32 | 0.014 | 21.46 | 0.014 | 22.18 | 0.007 | 4.29 |
| Rural resident | 0.011 | 13.89 | 0.016 | 41.57 | 0.012 | 25.13 | 0.011 | 18.02 | 0.018 | 51.25 | 0.014 | 34.62 |
| East region | −0.002 | 60.27 | −0.015 | 43.46 | −0.009 | 15.38 | −0.013 | 28.68 | −0.005 | 56.34 | 0.004 | 21.26 |
| Middle region | 0.018 | 0.001 | 0.000 | −0.001 | 0.013 | 0.010 | ||||||
| Number of children aged 0–4 in the household | 0.001 | 0.82 | −0.001 | 2.19 | 0.001 | 1.82 | 0.000 | 0.05 | 0.001 | 1.73 | 0.002 | 5.56 |
| Number of children aged 5–14 in the household | 0.002 | 8.47 | 0.001 | 1.25 | 0.000 | 0.86 | 0.000 | 0.59 | 0.001 | 2.68 | 0.003 | 32.08 |
| Number of observations | 9886 | 8561 | 8444 | 8717 | 9595 | 9377 | ||||||
| Adjusted R-squared | 0.2225 | 0.2466 | 0.2415 | 0.2070 | 0.2563 | 0.2388 | ||||||
| F statistic | 90.96 | 90.04 | 89.27 | 73.15 | 106.32 | 94.58 | ||||||
1. For each wave, the first column shows the estimated marginal effects and the second the logworth values. Logworth values in bold indicate significance at or below 5% level.

Table A2.
Effect of selected demographic and socioeconomic variables in the decomposition of the level-dependent indices for OOP burden (full results).
Table A2.
Effect of selected demographic and socioeconomic variables in the decomposition of the level-dependent indices for OOP burden (full results).
| 2000 | 2004 | 2006 | 2009 | 2011 | 2015 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable 1 | Coefficient | Logworth | Coefficient | Logworth | Coefficient | Logworth | Coefficient | Logworth | Coefficient | Logworth | Coefficient | Logworth |
| Female × age 18 below | −0.049 | 9.44 | −0.096 | 8.20 | 0.000 | 1.68 | 0.011 | 2.31 | 0.126 | 2.92 | 0.910 | 2.84 |
| Female × age 18–24 | 0.015 | 0.002 | 0.029 | 0.096 | 0.352 | −0.977 | ||||||
| Female × age 25–34 | −0.012 | −0.034 | 0.030 | 0.104 | 0.193 | −0.782 | ||||||
| Female × age 35–44 | 0.054 | 0.003 | −0.031 | −0.014 | 0.166 | −0.452 | ||||||
| Female × age 45–54 | −0.014 | −0.061 | −0.056 | −0.052 | 0.140 | 0.120 | ||||||
| Female × age 55–64 | 0.002 | −0.085 | −0.040 | −0.127 | 0.035 | 0.166 | ||||||
| Female × age 65 above | 0.064 | −0.030 | −0.023 | −0.128 | 0.178 | 0.574 | ||||||
| Male × age 18–24 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 | ||||||
| Male × age 25–34 | −0.002 | 0.016 | −0.004 | 0.075 | 0.094 | −0.630 | ||||||
| Male × age 35–44 | 0.130 | 0.066 | 0.024 | 0.018 | 0.202 | −0.578 | ||||||
| Male × age 45–54 | 0.043 | 0.021 | 0.027 | 0.046 | 0.246 | 0.038 | ||||||
| Male × age 55–64 | 0.037 | −0.017 | 0.010 | 0.010 | 0.210 | 0.540 | ||||||
| Male × age 65 above | 0.053 | 0.014 | 0.038 | −0.089 | 0.244 | 0.520 | ||||||
| Number of major diseases | 0.010 | 0.29 | 0.011 | 0.45 | −0.017 | 0.57 | −0.019 | 0.39 | −0.031 | 0.68 | 0.007 | 0.02 |
| Sickness in the last month | 0.009 | 0.10 | 0.031 | 1.06 | 0.070 | 2.17 | 0.107 | 1.87 | 0.149 | 2.18 | 0.309 | 0.63 |
| Number of symptoms in the last month | 0.064 | 2.18 | 0.037 | 3.90 | 0.021 | 0.82 | 0.026 | 0.52 | 0.045 | 0.73 | 0.050 | 0.13 |
| Private dwelling | −0.033 | 1.31 | −0.040 | 1.69 | −0.014 | 0.25 | −0.202 | 4.71 | −0.124 | 2.12 | −0.573 | 1.59 |
| Social health insurance | −0.039 | 0.85 | −0.016 | 0.41 | −0.077 | 7.48 | −0.014 | 0.18 | −0.130 | 2.69 | 0.482 | 1.12 |
| Ethnicity | −0.087 | 7.50 | −0.046 | 2.74 | −0.038 | 1.22 | −0.073 | 1.53 | −0.238 | 7.60 | −0.681 | 2.78 |
| Marital status | 0.003 | 0.06 | −0.026 | 1.13 | −0.051 | 1.87 | −0.180 | 7.23 | −0.249 | 9.43 | −0.596 | 2.21 |
| Primary school | −0.039 | 51.90 | −0.027 | 39.00 | −0.038 | 35.36 | −0.075 | 17.14 | −0.071 | 35.13 | 0.172 | 3.05 |
| Junior high school | −0.068 | −0.066 | −0.090 | −0.162 | −0.163 | 0.221 | ||||||
| Senior high school | −0.141 | −0.146 | −0.198 | −0.331 | −0.320 | −0.093 | ||||||
| University degree | −0.498 | −0.383 | −0.448 | −0.473 | −0.822 | −0.978 | ||||||
| In employment | −0.102 | 9.85 | −0.131 | 20.66 | −0.104 | 6.80 | −0.269 | 15.73 | −0.237 | 8.66 | −0.349 | 1.15 |
| White collar worker | −0.091 | 4.83 | −0.182 | 19.18 | −0.206 | 12.69 | −0.304 | 10.13 | −0.362 | 10.69 | −0.581 | 1.44 |
| Farmer | 0.150 | 22.52 | 0.128 | 18.00 | 0.133 | 10.08 | 0.290 | 16.26 | 0.296 | 11.38 | 0.103 | 0.16 |
| Rural resident | 0.080 | 7.74 | 0.158 | 35.70 | 0.101 | 8.73 | 0.111 | 3.88 | 0.316 | 19.02 | 0.993 | 8.49 |
| East region | −0.025 | 18.55 | −0.157 | 36.95 | −0.112 | 8.09 | −0.151 | 6.29 | 0.031 | 26.02 | 0.939 | 7.99 |
| Middle region | 0.088 | −0.006 | −0.026 | −0.021 | 0.318 | 0.869 | ||||||
| Number of children aged 0–4 in the household | −0.007 | 0.66 | −0.015 | 2.71 | 0.003 | 0.15 | −0.034 | 2.60 | 0.019 | 0.75 | 0.233 | 2.69 |
| Number of children aged 5–14 in the household | 0.028 | 16.80 | 0.005 | 1.19 | 0.008 | 1.41 | 0.009 | 0.80 | 0.015 | 1.12 | 0.171 | 3.99 |
| Number of observations | 9886 | 8561 | 8444 | 8717 | 9595 | 9377 | ||||||
| Adjusted R-squared | 0.1400 | 0.1987 | 0.1404 | 0.0964 | 0.1528 | 0.0401 | ||||||
| F statistic | 51.76 | 69.49 | 45.79 | 29.88 | 55.63 | 12.60 | ||||||
1. For each wave, the first column shows the estimated marginal effects and the second the logworth values. Logworth values in bold indicate significance at or below 5% level.
References
- Babiarz, Kimberly Singer, Grant Miller, Hongmei Yi, Linxiu Zhang, and Scott Rozelle. 2010. New evidence on the impact of China’s New Rural Cooperative Medical Scheme and its implications for rural primary healthcare: Multivariate difference-in-difference analysis. BMJ 341: c5617. [Google Scholar] [CrossRef] [PubMed]
- Cai, Jiaoli, Peter C. Coyte, and Hongzhong Zhao. 2017. Decomposing the causes of socioeconomic-related health inequality among urban and rural populations in China: A new decomposition approach. International Journal for Equity in Health 16: 128. [Google Scholar] [CrossRef]
- Chen, Mingsheng, Guixia Fang, Lidan Wang, Zhonghua Wang, Yuxin Zhao, and Lei Si. 2015. Who Benefits from Government Healthcare Subsidies? An Assessment of the Equity of Healthcare Benefits Distribution in China. PLoS ONE 10: e0119840. [Google Scholar] [CrossRef] [PubMed]
- Chen, Zhi, Kai Gu, Ying Zheng, Wei Zheng, Wei Lu, and Xiao Ou Shu. 2008. The use of complementary and alternative medicine among Chinese women with breast cancer. The Journal of Alternative and Complementary Medicine 14: 1049–55. [Google Scholar] [CrossRef]
- Coté, Pierre, Xiaoqing Yang, Vicki Kristman, Sheilah Hogg-Johnson, Dwayne Van Eerd, Mana Rezai, and Marjan Vidmar. 2013. The association between workers’ compensation claims involving neck pain and future health care utilization: A population-based cohort study. Journal of Occupational Rehabilitation 23: 547–56. [Google Scholar] [CrossRef] [PubMed]
- Coveney, Max, Pilar García-Gómez, Eddy Van Doorslaer, and Tom Van Ourti. 2016. Health Disparities by Income in Spain Before and After the Economic Crisis. Health Economics 25: 141–58. [Google Scholar] [CrossRef]
- Cui, Yong, Xiao-Ou Shu, Yutang Gao, Wanqing Wen, Zhi-Xian Ruan, Fan Jin, and Wei Zheng. 2004. Use of complementary and alternative medicine by chinese women with breast cancer. Breast Cancer Research and Treatment 85: 263–70. [Google Scholar] [CrossRef]
- Dong, Keyong. 2009. Medical insurance system evolution in China. China Economic Review 20: 591–97. [Google Scholar] [CrossRef]
- Elwell-Sutton, Timothy M., Chao Qiang Jiang, Wei Sen Zhang, Kar Keung Cheng, Tai H. Lam, Gabriel M. Leung, and Catherine Mary Schooling. 2013. Inequality and inequity in access to health care and treatment for chronic conditions in China: The Guangzhou Biobank Cohort Study. Health Policy and Planning 28: 467–79. [Google Scholar] [CrossRef]
- Erreygers, Guido. 2009. Correcting the concentration index. Journal of Health Economics 28: 504–15. [Google Scholar] [CrossRef]
- Erreygers, Guido, and Roselinde Kessels. 2013. Regression-based decompositions of rank-dependent indicators of socioeconomic inequality of health. Health and Inequality 21: 227–59. [Google Scholar]
- Erreygers, Guido, and Roselinde Kessels. 2017. Socioeconomic Status and Health: A New Approach to the Measurement of Bivariate Inequality. International Journal of Environmental Research and Public Health 14: 673. [Google Scholar] [CrossRef] [PubMed]
- Erreygers, Guido, and Tom Van Ourti. 2011. Measuring socioeconomic inequality in health, health care and health financing by means of rank-dependent indices: A recipe for good practice. Journal of Health Economics 30: 685–94. [Google Scholar] [CrossRef] [PubMed]
- Gao, Jun, Juncheng Qian, Shenglan Tang, Bo Eriksson, and Erik Blas. 2002. Health equity in transition from planned to market economy in China. Health Policy and Planning 17: 20–29. [Google Scholar] [CrossRef]
- Gong, Sen, and Hana Brixi. 2005. China: Health, Poverty and Economic Development. Beijing: Office of the World Health Organization Representative in China and Social Development Department of China State Council Development Research Centre. [Google Scholar]
- Harmsworth, K., and George T. Lewith. 2001. Attitudes to traditional Chinese medicine amongst Western trained doctors in the People’s Republic of China. Social Science & Medicine 52: 149–53. [Google Scholar] [CrossRef]
- Heckley, Gawain, Ulf-G. Gerdtham, and Gustav Kjellsson. 2016. A general method for decomposing the causes of socioeconomic inequality in health. Journal of Health Economics 48: 89–106. [Google Scholar] [CrossRef]
- Kessels, Roselinde, and Guido Erreygers. 2019. A direct regression approach to decomposing socioeconomic inequality of health. Health Economics 28: 884–905. [Google Scholar] [CrossRef]
- Li, Chao, Lingxia Zeng, Michael John Dibley, Duolao Wang, Leilei Pei, and Hong Yan. 2015. Evaluation of socio-economic inequalities in the use of maternal health services in rural western China. Public Health 129: 1251–57. [Google Scholar] [CrossRef]
- Li, Xi, Jiapeng Lu, Shuang Hu, K. K. Cheng, Jan De Maeseneer, Qingyue Meng, Elias Mossialos, Dong Roman Xu, Winnie Yip, Hongzhao Zhang, and et al. 2017a. The primary health-care system in China. The Lancet 390: 2584–94. [Google Scholar] [CrossRef]
- Li, Yanping, Vasanti Malik, and Frank B. Hu. 2017b. Health Insurance in China: After Declining In The 1990s, Coverage Rates Rebounded To Near-Universal Levels By 2011. Health Affairs 36: 1452–60. [Google Scholar] [CrossRef]
- Liu, Yuanli, William C. Hsiao, and Karen Eggleston. 1999. Equity in health and health care: The Chinese experience. Social Science & Medicine 49: 1349–56. [Google Scholar]
- Mossialos, Elias, Yanfeng Ge, Jia Hu, and Liejun Wang. 2016. Pharmaceutical Policy in China Challenges and Opportunities for Reform. Geneva: World Health Organization. [Google Scholar]
- O’Donnell, Owen, and Carol Propper. 1991. Equity and the Distribution of United Kingdom National Health Service Resources. Journal of Health Economics 10: 1–19. [Google Scholar] [CrossRef] [PubMed]
- OECD. n.d. What Are Equivalence Scales? Edited by OECD Project on Income Distribution and Poverty. Paris: OECD.
- Popkin, Barry M., Shufa Du, Fengying Zhai, and Bing Zhang. 2010. Cohort Profile: The China Health and Nutrition Survey—Monitoring and understanding socio-economic and health change in China, 1989–2011. International Journal of Epidemiology 39: 1435–40. [Google Scholar] [CrossRef] [PubMed]
- Shen, Yuan, Hong Yan, Klemetti Reija, Qiang Li, Shengbin Xiao, Jianmin Gao, and Zhongliang Zhou. 2014. Equity in use of maternal health services in Western Rural China: A survey from Shaanxi province. BMC Health Services Research 14: 155. [Google Scholar] [CrossRef]
- Si, Wei. 2021. Public health insurance and the labor market: Evidence from China’s Urban Resident Basic Medical Insurance. Health Economics 30: 403–31. [Google Scholar] [CrossRef]
- Sun, Xiaoyun, Adrian C. Sleigh, Gordon A. Carmichael, and Sukhan Jackson. 2010. Health payment-induced poverty under China’s New Cooperative Medical Scheme in rural Shandong. Health Policy and Planning 25: 419–26. [Google Scholar] [CrossRef]
- Sylvia, Sean, Hao Xue, Chengchao Zhou, Yaojiang Shi, Hongmei Yi, Huan Zhou, Scott Rozelle, Madhukar Pai, and Jishnu Das. 2017. Tuberculosis detection and the challenges of integrated care in rural China: A cross-sectional standardized patient study. PLoS Medicine 14: e1002405. [Google Scholar] [CrossRef]
- Sylvia, Sean, Yaojiang Shi, Hao Xue, Xin Tian, Huan Wang, Qingmei Liu, Alexis Medina, and Scott Rozelle. 2014. Survey using incognito standardized patients shows poor quality care in China’s rural clinics. Health Policy and Planning 30: 322–33. [Google Scholar] [CrossRef]
- Tang, Shenglan, Qingyue Meng, Lincoln Chen, Henk Bekedam, Tim Evans, and Margaret Whitehead. 2008. Tackling the challenges to health equity in China. The Lancet 372: 1493–501. [Google Scholar] [CrossRef]
- Van Doorslaer, Eddy, Adam Wagstaff, and Frans Rutten. 1992. Equity in the Finance and Delivery of Health Care: An International Perspective. Oxford: Oxford University Press. [Google Scholar]
- Van Doorslaer, Eddy, Adam Wagstaff, Hattem Van der Burg, Terkel Christiansen, Diana De Graeve, Inge Duchesne, Ulf-G. Gerdtham, Michael Gerfin, José Geurts, and Lorna Gross. 2000. Equity in the delivery of health care in Europe and the US. Journal of Health Economics 19: 553–83. [Google Scholar] [CrossRef]
- Van Doorslaer, Eddy, and Cristina Masseria. 2004. Income-Related Inequality in the Use of Medical Care in 21 OECD Countries. Paris: OECD. [Google Scholar]
- Van Doorslaer, Eddy, and Owen O’Donnell. 2011. Measurement and Explanation of Inequality in Health and Health Care in Low-Income Settings. In Health Inequality and Development. Edited by Marc McGillivray, Indranil Dutta and David Lawson. London: Palgrave Macmillan. [Google Scholar]
- Van Doorslaer, Eddy, Xander Koolman, and Andrew M. Jones. 2004. Explaining income-related inequalities in doctor utilisation in Europe. Health Economics 13: 629–47. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, Adam. 2009a. Reforming China’s Rural Health System, Directions in Development—Human Development. Washington, DC: The World Bank. [Google Scholar]
- Wagstaff, Adam. 2009b. Reranking and Pro-Poor Growth: Decompositions for China and Vietnam. The Journal of Development Studies 45: 1403–25. [Google Scholar] [CrossRef]
- Wagstaff, Adam, and Magnus Lindelow. 2008. Can insurance increase financial risk?: The curious case of health insurance in China. Journal of Health Economics 27: 990–1005. [Google Scholar] [CrossRef]
- Wagstaff, Adam, Eddy Van Doorslaer, and Naoko Watanabe. 2003. On decomposing the causes of health sector inequalities with an application to malnutrition inequalities in Vietnam. Journal of Econometrics 112: 207–23. [Google Scholar] [CrossRef]
- Wagstaff, Adam, Pierella Paci, and Eddy Van Doorslaer. 1991. On the measurement of inequalities in health. Social Science & Medicine 33: 545–57. [Google Scholar] [CrossRef]
- Wagstaff, Adam, Winnie Yip, Magnus Lindelow, and William C. Hsiao. 2009. China’s health system and its reform: A review of recent studies. Health Economics 18: S7–S23. [Google Scholar] [CrossRef]
- Wang, Yang, Jian Wang, Elizabeth Maitland, Yaohui Zhao, Stephen Nicholas, and Mingshan Lu. 2012. Growing old before growing rich: Inequality in health service utilization among the mid-aged and elderly in Gansu and Zhejiang Provinces, China. BMC Health Services Research 12: 302. [Google Scholar] [CrossRef]
- Wong, William C. W., Shanzhu Zhu, Jason J. Ong, Minghui Peng, Cindy L. K. Lam, Michael R. Kidd, Martin Roland, and Sunfang Jiang. 2017. Primary care workforce and continuous medical education in China: Lessons to learn from a nationwide cross-sectional survey. BMJ Open 7: e015145. [Google Scholar] [CrossRef]
- Xiang, Yuening, Zimu Guo, Pengfei Zhu, Jia Chen, and Yongye Huang. 2019. Traditional Chinese medicine as a cancer treatment: Modern perspectives of ancient but advanced science. Cancer Medicine 8: 1958–75. [Google Scholar] [CrossRef]
- Xie, E. 2011. Income-related inequalities of health and health care utilization. Frontiers of Economics in China 6: 131–56. [Google Scholar] [CrossRef]
- Xie, Xin, Qunhong Wu, Yanhua Hao, Hui Yin, Wenqi Fu, Ning Ning, Ling Xu, Chaojie Liu, Ye Li, Zheng Kang, and et al. 2014. Identifying Determinants of Socioeconomic Inequality in Health Service Utilization among Patients with Chronic Non-Communicable Diseases in China. PLoS ONE 9: e100231. [Google Scholar] [CrossRef] [PubMed]
- Xu, Ke, David B. Evans, Guido Carrin, Ana Mylena Aguilar-Rivera, Philip Musgrove, and Timothy Evans. 2007. Protecting Households From Catastrophic Health Spending. Health Affairs 26: 972–83. [Google Scholar] [CrossRef] [PubMed]
- Yang, Wei. 2013. China’s new cooperative medical scheme and equity in access to health care: Evidence from a longitudinal household survey. International Journal for Equity in Health 12: 20. [Google Scholar] [CrossRef] [PubMed]
- Yang, Wei, and Xun Wu. 2017. Providing comprehensive health insurance coverage in rural China: A critical appraisal of the New Cooperative Medical Scheme and ways forward. Global Policy 8: 110–16. [Google Scholar] [CrossRef]
- Yi, Hongmei, Paiou Wu, Xiaoyuan Zhang, Dirk E. Teuwen, and Sean Sylvia. 2020. Market competition and demand for skills in a credence goods market: Evidence from face-to-face and web-based non-physician clinician training in rural China. PLoS ONE 15: e0233955. [Google Scholar] [CrossRef]
- Yip, Winnie Chi-Man, William C. Hsiao, Wen Chen, Shanlian Hu, Jin Ma, and Alan Maynard. 2012. Early appraisal of China’s huge and complex health-care reforms. The Lancet 379: 833–42. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Xiaobo, and Ravi Kanbur. 2005. Spatial inequality in education and health care in China. China Economic Review 16: 189–204. [Google Scholar] [CrossRef]
- Zhang, Xin, Qunhong Wu, Yongxiang Shao, Wenqi Fu, Guoxiang Liu, and Peter C. Coyte. 2015. Socioeconomic Inequities in Health Care Utilization in China. Asia-Pacific Journal of Public Health 27: 429–38. [Google Scholar] [CrossRef]
- Zhou, Zhongliang, Jianmin Gao, Ashley Fox, Keqin Rao, Ke Xu, Ling Xu, and Yaoguang Zhang. 2011. Measuring the equity of inpatient utilization in Chinese rural areas. BMC Health Services Research 11: 201. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).