Abstract
Exoskeletons can track the wearer’s movements in real time, thereby enhancing physical performance or restoring mobility for individuals with gait impairments. These wearable assistive devices have demonstrated significant potential in both rehabilitation and industrial applications. This review focuses on the major advancements in exoskeleton technology published since 2020, with particular emphasis on the development of structural designs for lower-limb exoskeletons employed in locomotion assistance. We employed a systematic literature review methodology, categorizing the included studies into three main types: rigid exoskeleton, soft exoskeleton, and tethered platform. The current development status of robotic exoskeletons is analyzed based on publication year, system weight, target assistive joints, and main effects. Furthermore, we examine the factors driving these advancements and their implications for the field. The key challenges and opportunities that may influence the future development of exoskeleton technologies are also highlighted in this review.
1. Introduction
Walking is one of the most essential daily activities for humans. On average, individuals take thousands of steps each day, amounting to hundreds of millions of steps over a lifetime [1,2]. The energy expenditure associated with walking significantly surpasses that of any other daily activity [3]. However, factors such as aging, spinal cord injuries, and strokes can severely impair an individual’s ability to walk [4]. Additionally, in fields such as the military [5] and industrial production [6,7], there is an increasing demand for external assistive devices to enhance work performance.
The term “exoskeleton” is derived from the Greek words (outer) and ó (skeleton) [8], originally referring to the chitinous outer shell found in arthropods and microorganisms, which serves to protect and support internal structures [9]. In the context of robotics, an exoskeleton refers to a type of wearable assistive device (WAD) designed to aid human movement and enhance mobility. By integrating sensors, actuators, and control algorithms, these devices can track the wearer’s movements in real time and provide tailored assistance for specific needs, such as supporting rehabilitation or enhancing physical performance. As early as 1890, researchers began exploring the use of WADs to assist individuals with walking [10]. Over the subsequent century, numerous WADs were developed to assist with walking [11], carrying loads [12], rehabilitation training [13], and energy harvesting from human movement [14]. Extensive research has demonstrated the significant potential of exoskeleton robots in both industrial and medical applications.
In recent years, substantial progress has been achieved in the development of robotic exoskeletons for locomotion assistance. Initial designs focused on rigid structures composed of rigid linkages and joints [15], prioritizing stability and load-bearing capabilities. Recent advancements have incorporated flexible materials and biomimetic designs [8,16,17,18] to enhance comfort and adaptability for wearers. Similarly, the assistance strategies of exoskeletons have evolved from basic pre-programmed modes to sophisticated intelligent systems capable of customizing and adapting to the individual user requirements [19,20,21]. However, despite these advancements, challenges such as weight penalties [15], joint misalignment [22], and the lack of personalized control strategies [23] continue to hinder the widespread adoption and optimization of exoskeleton technology.
There are numerous review articles on exoskeletons that have adopted systematic analysis methods to provide a detailed examination of the current state of development in robotics exoskeletons [24,25]. For instance, the study by L. Chen et al. [16] systematically defines and analyzes the key design factors influencing the wearing comfort of rigid exoskeleton robots, with a particular focus on the differences between traditional exoskeleton robots and those equipped with self-alignment mechanisms in addressing joint misalignment issues. The review by O. Coser et al. [26] outlines the research progress in applying artificial intelligence to the field of lower limb rehabilitative exoskeletons. They specifically highlight the suitability of different algorithms for specific tasks, aiming to provide guidance for future research and development. H. Lee et al. [27] categorized lower-limb exoskeletons into three types: assistive exoskeletons, rehabilitation exoskeletons, and augmentation exoskeletons. They conducted systematic analyses of the included studies, focusing on the degree of freedom, intention estimation methods, and actuator types. Based on their findings, the authors highlighted that current exoskeleton research has yet to meet the desire for machines capable of seamless cooperation with users. They emphasized the promising prospects of future research aimed at improving human–exoskeleton interaction. However, in recent years, there has been a lack of systematic review articles focusing on the prototype development of robotic exoskeletons designed for locomotion assistance.
The rationale for this study stems from the growing research on exoskeleton technology, particularly in rehabilitation and assistive applications. Despite significant advancements in this field, challenges remain in optimizing exoskeleton designs for improved performance, user comfort, and adaptability. There is a need to better understand the factors influencing the effectiveness of these devices in various contexts. This review consolidates recent studies to provide a comprehensive overview of the state of the art, highlight key technical challenges, and identify potential areas for further research. In doing so, it offers valuable insights that can inform the design and development of more effective and user-friendly exoskeletons, inspiring future improvements in the field.
2. Method
This study employs a systematic literature review methodology, which is a structured and rigorous approach to reviewing the literature. This methodology involves the use of transparent and reproducible search techniques and strategies to retrieve and evaluate relevant studies. The selected literature is subsequently screened and assessed based on predefined criteria or research questions, enabling a precise understanding of the current state and trends of the research topic to address specific research questions [28]. The advantages of the systematic literature review method lie in its rigor and transparency, characterized by clearly defined research questions, comprehensive search strategies, explicit inclusion criteria, high-quality assessment methods, integrated data analysis, and reliable research outcomes. This approach effectively mitigates issues such as subjectivity and bias commonly associated with traditional research methods.
To systematically review the relevant studies in the literature, we conducted a search in two major databases in January 2025, Web of Science and IEEE Xplore, with the search limited to English-language articles. The search in each database was performed using the following keyword structure: (“exoskeleton” OR “exosuit” OR “wearable assistive devices”) AND “locomotion assistive”.
To ensure the accuracy and reliability of the literature analysis, we established the exclusion criteria listed in Table 1 based on the research questions. Criteria C1 to C3 are commonly used selection standards in systematic literature reviews to ensure the accuracy and authority of the research sample. Criteria C4 and C5 restrict the study subjects, while C6 to C8 ensure that the findings reported in the included studies are statistically significant from a physiological perspective. Criterion C9 ensures the timeliness of the studies.

Table 1.
Exclusion criteria for the literature.
3. Results
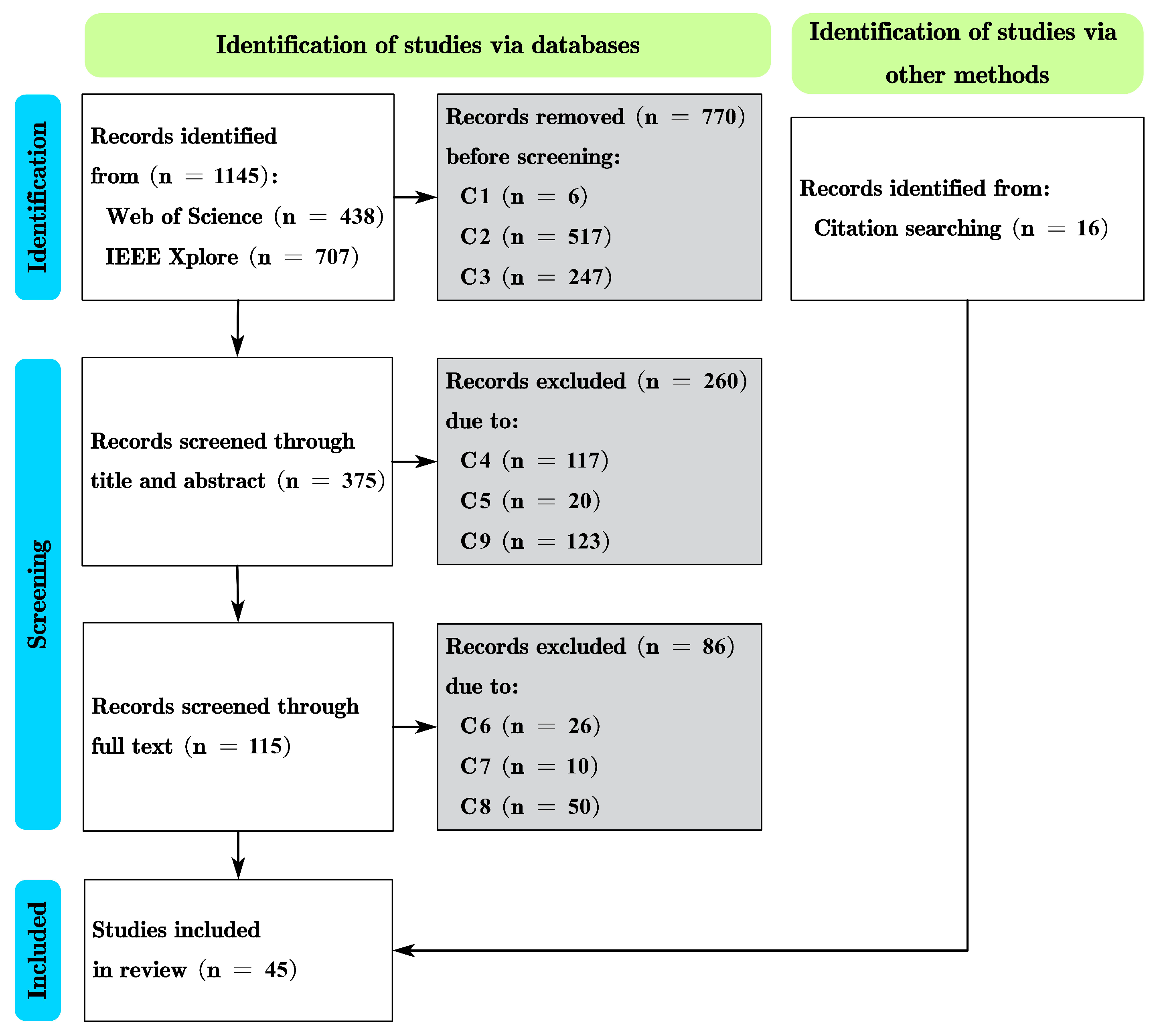
This study follows the systematic literature review and meta-analysis approach outlined by Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). This method is internationally recognized for systematic reviews and encompasses 27 criteria (such as title, abstract, methods, results, discussion, etc.) and 4 phases [29]. It mandates a transparent presentation of the literature identification, screening, inclusion, and exclusion processes, along with the rationale for each decision, to enhance the accuracy and reliability of systematic literature reviews and meta-analysis reports. Based on this approach, a total of 45 papers meeting the inclusion criteria were identified for this study, as illustrated in the PRISMA flow diagram in Figure 1.
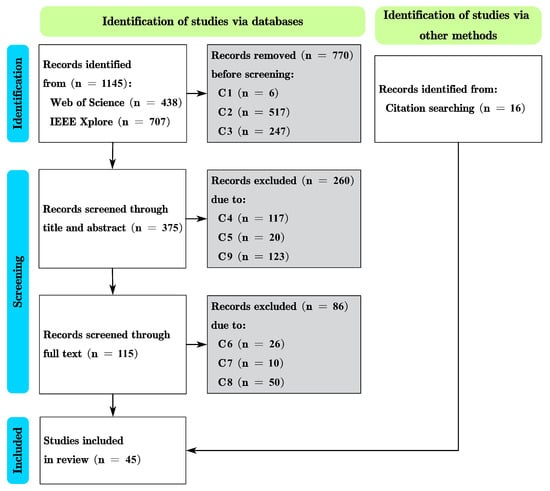
Figure 1.
PRISMA flow diagram of study selection and screening process.
For the 45 selected articles, this study analyzes them based on publication year, structural classification, system weight, degrees of freedom in assistance, physiological effects, and application scenarios.
In terms of structure, the exoskeletons are categorized into three primary types: rigid exoskeleton, soft exoskeleton, and tethered platform, based on the methods of force transmission and actuator arrangement reported in the literature.
Regarding physiological effects, for metabolic rate data, we utilize net metabolic change and gross metabolic change as the measurement standards, which can be represented by the following formulas [8]:
where refers to the metabolic rate of the subject when receiving assistance from the exoskeleton, refers to the metabolic rate of the subject when wearing the exoskeleton without assistance, refers to the metabolic rate of the subject when not wearing the exoskeleton, and refers to the metabolic rate of the subject at rest while standing.
In terms of application scenarios, we classify the studies based on the characteristics of the experimental participants. Studies involving participants with mobility impairments are categorized as rehabilitation, whereas the remaining studies are classified as assistance.
3.1. Rigid Exoskeleton
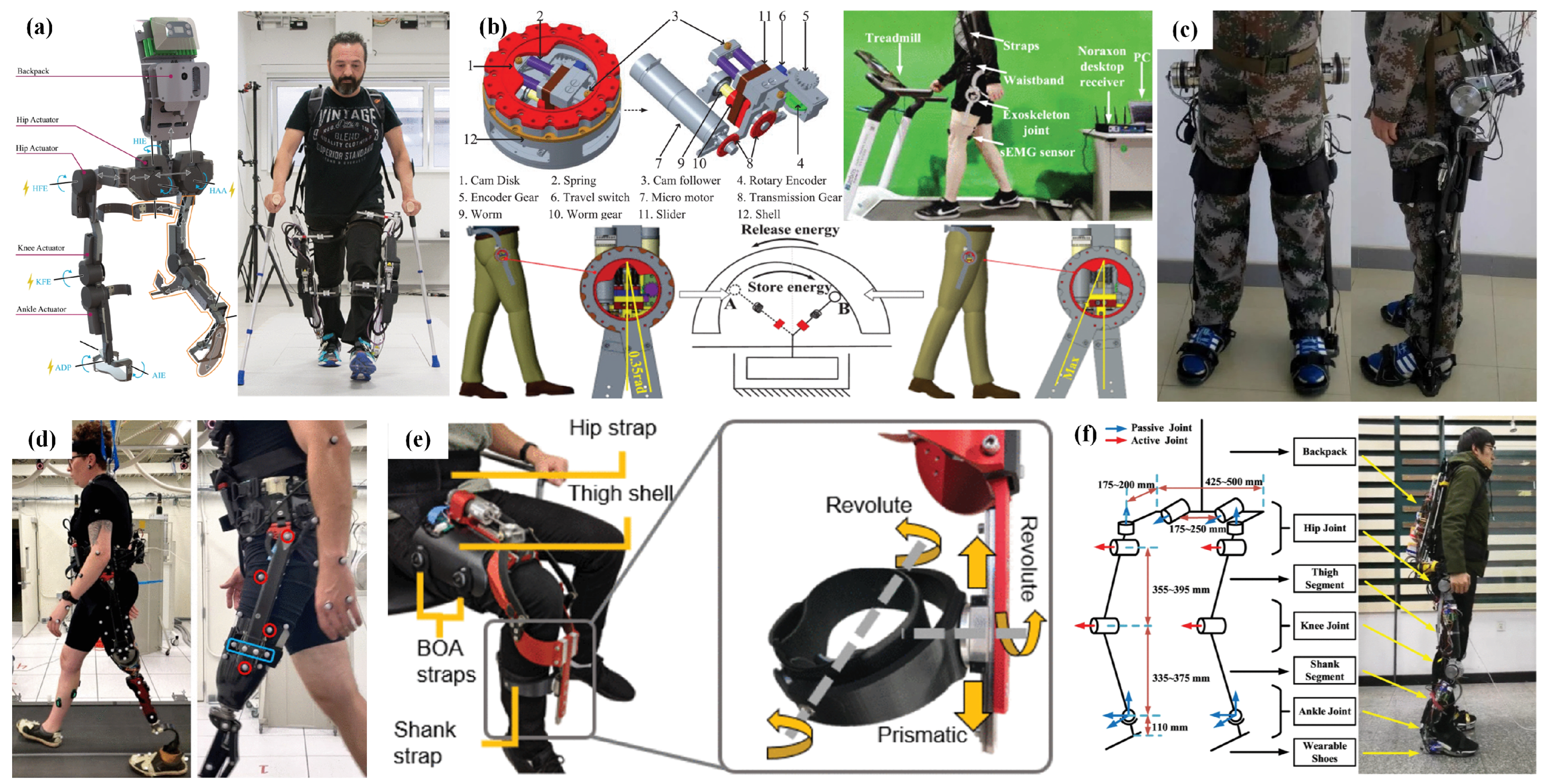
Rigid exoskeleton robots are wearable assistive devices constructed using rigid materials, as shown in Figure 2. They provide external mechanical support and assistance by connecting to the wearer’s limbs through a rigid framework and mechanical joints, thereby enhancing human mobility or aiding in rehabilitation training. Among the 45 articles analyzed in this study, 13 focus on rigid exoskeletons, as listed in Table 2.
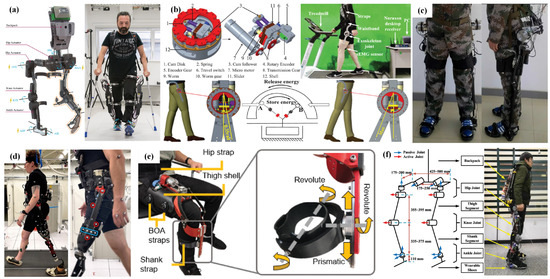
Figure 2.
Rigid exoskeletons for locomotion assistance. (a) C. Meijneke et al.’s full-size exoskeleton for hip, knee, and ankle assistance [30]. (b) B. Hu et al.’s variable stiffness hip exoskeleton [31]. (c) L. Wang et al.’s full-size exoskeleton for load carrying [32]. (d) M. Ishmael et al.’s for hip assistance [33]. (e) S. Sarkisian et al.’s self-aligning joint for knee [34]. (f) C. Chen et al.’s full-size exoskeleton with SEA joint for locomotion assistance [35].

Table 2.
Overview of the analyzed rigid exoskeletons.
The frame of a rigid exoskeleton is constructed from rigid materials such as aluminum alloy, titanium alloy, or carbon fiber composites. This design provides the exoskeleton with high stiffness and bending strength, enabling it to withstand large loads while evenly distributing forces across the body to reduce localized pressure. The frame is typically designed based on the anatomical structure of the human limbs, with support structures designed along areas such as the legs or waist. Some full-sized exoskeletons can transfer the load to the ground through their structure, as reported in the literature [30,35,36,40,41,44]. In the medical rehabilitation field, it supports the patient’s body weight, while in industrial applications, it enhances the worker’s ability to carry and move loads.
The mechanical joints of rigid exoskeletons are designed to replicate the rotational movement of human joints. These joints are typically equipped with hinges, and motion is achieved through the integration of high-torque motors. To prevent misalignment between the mechanical joints and the human joints, which could interfere with the natural movement of the wearer during human–machine collaborative motion [17,47], many exoskeletons incorporate adaptive structures into their mechanical joints, such as series elastic actuators (SEAs) [34,35,37,46,48,49] and variable stiffness mechanisms [50,51,52]. Here, we provide two illustrative examples. L. Wang et al. [53] proposed a novel SEA by integrating a specially designed elastic module between the servo motor and the joint link. This design enables the automatic alignment of the joint within a certain range and absorbs impact energy in the mechanical system, reducing the instantaneous load on the actuators and structure. Additionally, by measuring the deformation of the elastic module, the torque applied to the SEA can be indirectly calculated, eliminating the need for extra torque sensors and further reducing the overall weight of the system. B. Hu et al. [31], based on the analysis of the energy flow and stiffness variation characteristics of the lower limb joints during level human walking, proposed a novel variable-stiffness energy-storing assistive hip exoskeleton. This system utilizes a miniature servo motor to adjust the stiffness of the mechanical joints in real time, storing a significant portion of the negative work performed by the hip joint during walking. The stored energy is then used to assist human locomotion. Experimental results demonstrate that it can reduce the muscle activation of the rectus femoris by an average of 8.5% in subjects.
3.2. Soft Exoskeleton
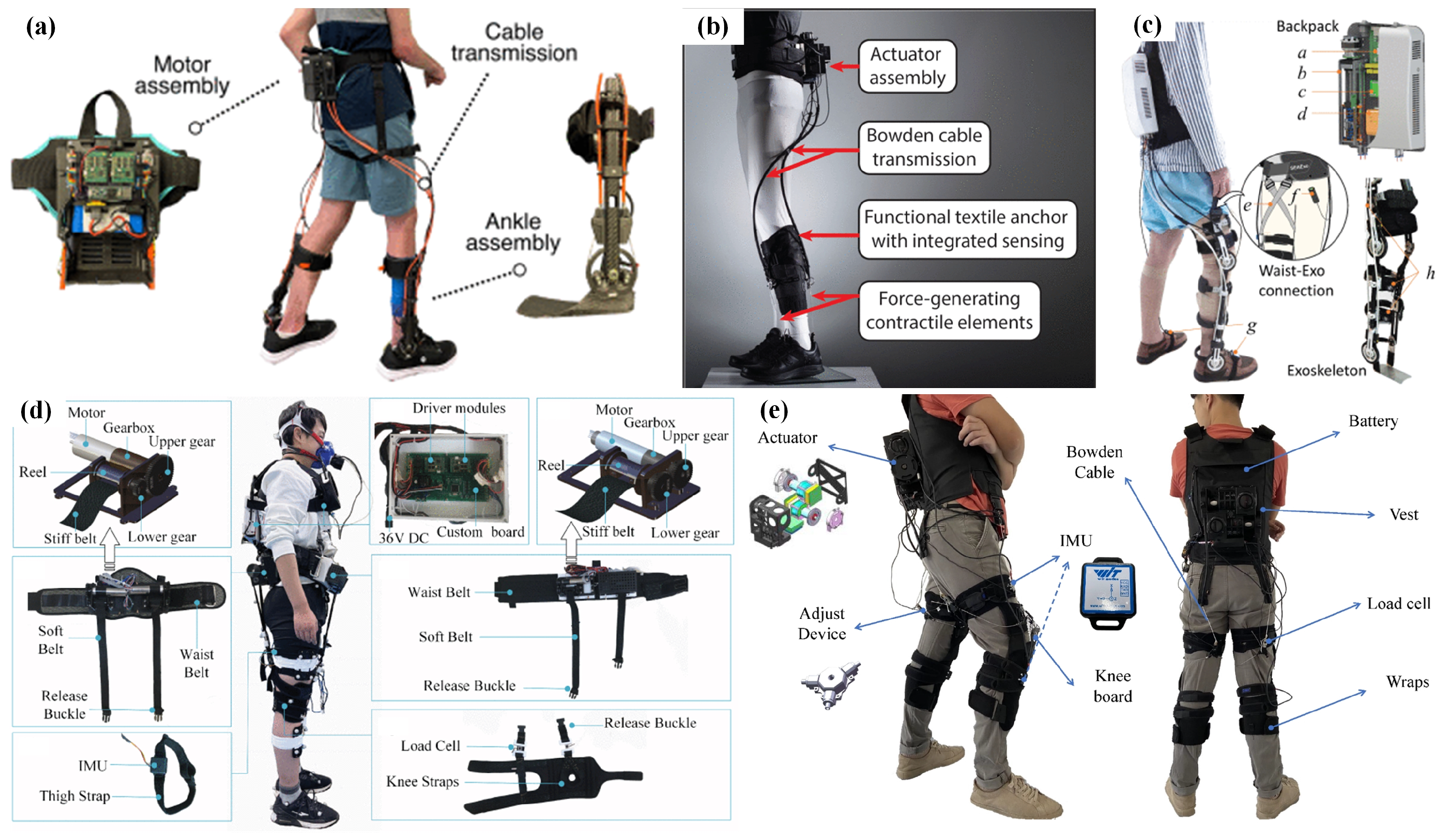
The soft exoskeleton is a wearable assistive device that provides support through flexible materials or cable systems, as shown in Figure 3. Compared to traditional rigid exoskeletons, flexible exoskeletons rely on lightweight, flexible structures and soft actuation technologies, which allow for a close fit with the human body while minimizing limitations on natural movement [54]. In this study, we focus on analyzing soft exoskeletons driven by motors and Bowden cables as the source of assistance. Among the 45 articles included in this study, 19 focus on soft exoskeletons, as listed in Table 3.

Figure 3.
Soft exoskeletons for locomotion assistance. (a) B. Conner et al.’s hybrid cable-driven exoskeleton for ankle assistance [55]. (b) L. Awad et al.’s cable-driven ankle exoskeleton [56]. (c) B. Zhong et al.’s hybrid cable-driven exoskeleton for stroke patients [57]. (d) Q. Chen et al.’s cable-driven exoskeleton for hip assistance [58]. (e) L. Zhu et al.’s cable-driven exoskeleton for hip and knee [59].

Table 3.
Overview of the analyzed soft exoskeletons.
Due to the inevitable phenomena of friction, slippage, and slack in flexible cables, a significant portion of the power output from the motor is lost during transmission [8,74], which reduces the assistance effectiveness of the soft exoskeleton. To address this issue, current research in the structural design of soft exoskeletons mainly follows two approaches. One approach involves altering the materials of the flexible textile, pre-tensioning the transmission cables, and adjusting the layout of anchor points [58,64,65,69,75] to optimize the power transmission path and improve the transmission efficiency of the flexible cables. For example, S. Lessard et al. [76] used infrared motion capture technology to identify the minimal extension lines on the human body during movement. Based on this, they proposed an improved tensioning design method to guide the cable layout for cable-driven actuation, thereby enhancing the overall power transmission efficiency of the system. Y. Shi et al. [77] introduced a Bowden cable pre-tensioning mechanism based on a differential gear system, which achieves the real-time pre-tensioning of two Bowden cables to drive the antagonistic motion of a human joint through the combined motion of the differential gears. The pre-tensioned Bowden cables effectively prevent slack and help mitigate the negative impact of cable plastic deformation on the exoskeleton’s control algorithm [78].
Another approach is to place a rigid structure near the target assistive joint to support the cables [55,57,66,67,68,71,72], thereby preventing unnecessary friction and slippage of the cables and reducing power loss during transmission. This method is referred to as the “hybrid cable-driven” type. For example, J. Chen et al. [68] proposed a hybrid cable-driven exoskeleton for ankle joint assistance. They conducted topology optimization and finite element analysis on the rigid structure based on the force characteristics of the foot and ankle, resulting in an 80% reduction in the overall weight of the rigid components. This design is capable of providing a peak assistive torque of 100 Nm and achieving an average reduction of 32.5% in the muscle activation of the soleus muscle in the participants.
3.3. Tethered Platform
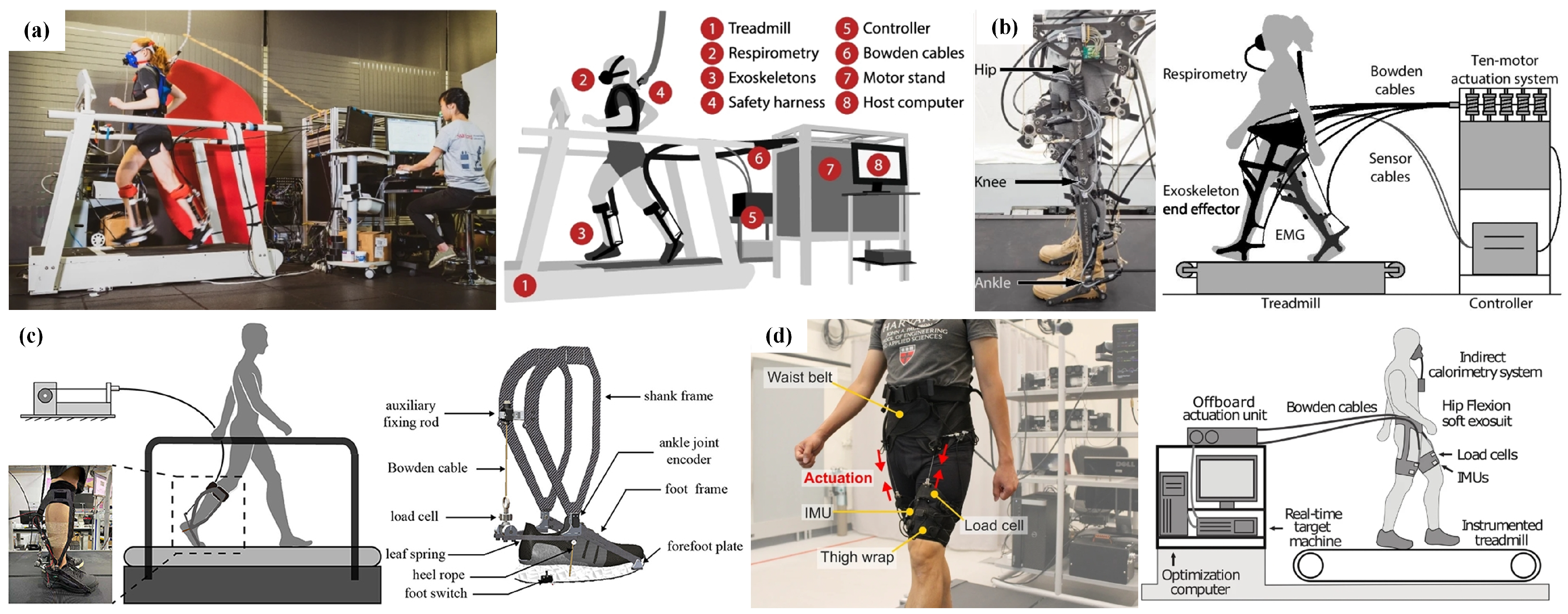
Peripheral extremities, which are located at a greater distance from the axial skeleton, exhibit heightened sensitivity to increments in load bearing [79,80]. An unreasonable weight distribution in the device can have a significant negative impact on the wearer’s metabolic rate [81,82], thereby reducing the assistive effectiveness of the exoskeleton during prolonged use. Compared to rigid exoskeletons, soft exoskeletons shift the actuating units, such as motors, to the wearer’s back or waist, an area less sensitive to weight increase, thereby enhancing the overall assistive performance. In recent years, researchers have proposed the concept of a tethered platform, where the servo motors, control modules, and power supply are all integrated into an off-board platform, as shown in Figure 4. The assistive force is transmitted to the wearer through flexible cables, minimizing the impact of the device’s weight on the wearer. Out of the total of 45 articles analyzed within the scope of this study, 13 publications specifically addressed the topic of tethered platforms, representing 28.9% of the analyzed corpus, as shown in Table 4.
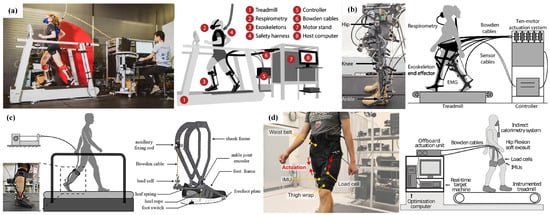
Figure 4.
Tethered platforms for physiological analysis and control algorithm testing. (a) D. Miller et al.’s tethered platform for ankle analysis [83]. (b) G. Bryan et al.’s tethered platform for hip, knee, and ankle analysis [84]. (c) W. Wang et al.’s tethered platform for ankle analysis [85]. (d) J. Kim et al.’s tethered platform/soft exoskeleton for hip analysis/assistance [86].

Table 4.
Overview of the analyzed tethered platform.
G. Bryan et al. [84] proposed an exoskeleton based on the tethered platform concept that provides assistance to the hip, knee, and ankle joints. Weighing only 13.5 kg, it delivers a maximum peak assistive torque of 250 Nm [96] and reduces the wearer’s gross metabolic cost by 50%. In contrast, C. Meijneke et al. [30] developed a rigid exoskeleton, also offering assistance to the hip, knee, and ankle joints but weighing 37.2 kg. The tethered design significantly reduces the overall weight of the exoskeleton, thereby improving its assistive performance.
By externalizing the actuating system to minimize the impact of device weight on the wearer, researchers can focus their efforts on studying the effects of exoskeleton assistance strategies on the wearer. For example, the impact of assistance timing and peak torque on the wearer’s metabolic cost [83,93,95], as well as the improvement in assistive performance through customized control strategies [71,85,94,97], are key areas of research. For instance, with the aid of the tethered platform, K. Poggensee et al. [95] focused on studying the impact of adaptive training on the assistive performance of exoskeletons. Their experimental results demonstrated that adaptive training improved the assistance effect by approximately 25%. Additionally, they also investigated the impact of customized assistance strategies on the wearer by adjusting the peak torque provided by the exoskeleton to the optimal level for each participant. Their results demonstrated that appropriately adjusted customized peak assistance could reduce the gross metabolic cost by 39%.
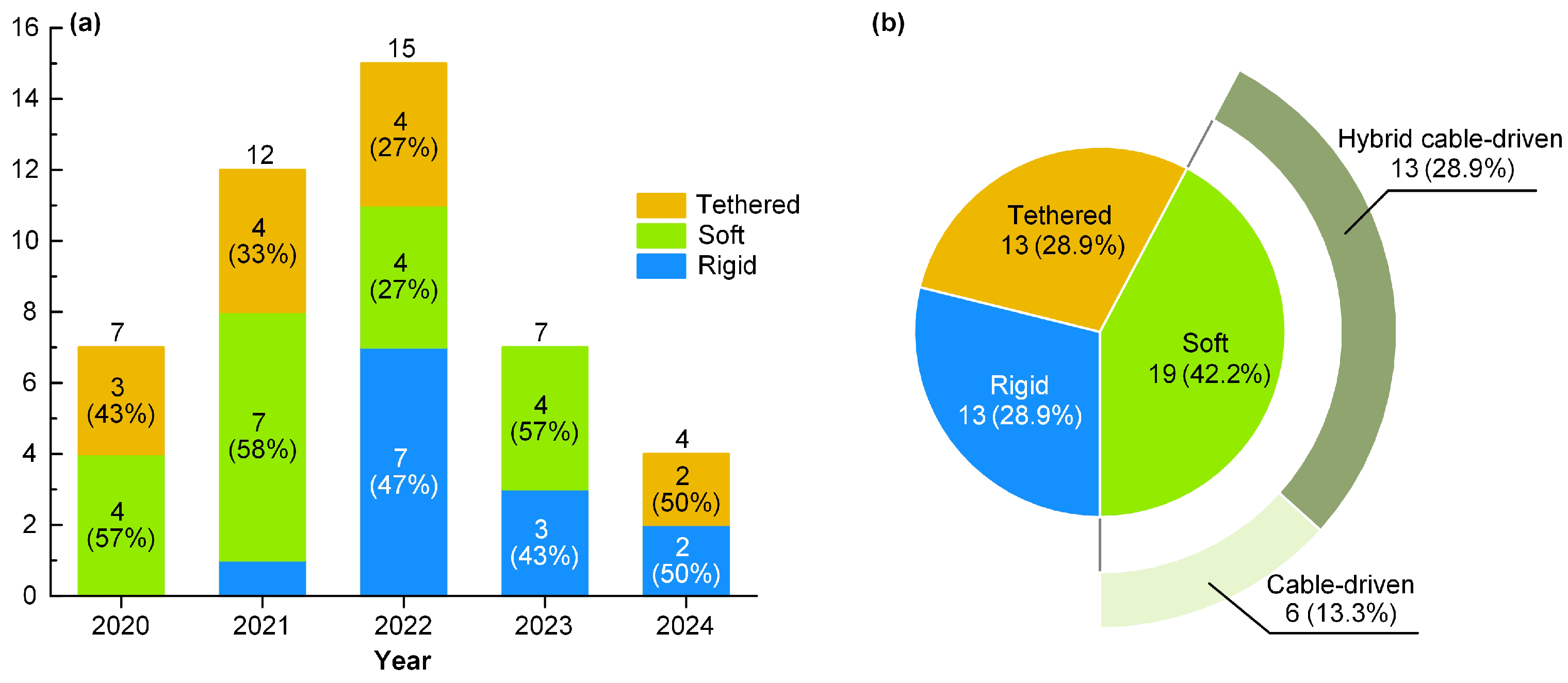
3.4. Categories and Year of First Publication
We analyzed the first publication years and device types of the 45 included studies, as shown in Figure 5. The majority of the studies were published between 2020 and 2022, with the number of publications increasing annually, peaking at 15 papers in 2022. Publications from 2023 and 2024 exhibit a decline in number, as they are more recent and may not have been indexed yet in the databases.
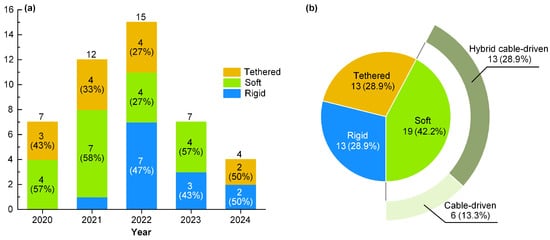
Figure 5.
The distribution of the studies included. (a) The distribution of studies over time. (b) The distribution of proportions among three configuration type.
From the perspective of system configuration, the distribution of literature topics related to exoskeleton robots over the past five years has been relatively balanced. The proportions of tethered platform, rigid exoskeleton, and soft exoskeleton are 28.9%, 28.9%, and 42.2%, respectively. Among soft exoskeletons, the hybrid cable-driven configuration accounts for a larger proportion compared to the cable-driven configuration, with percentages of 28.9% and 13.3%, respectively.
It is worth noting that W. Cao et al. [66] reported a special exoskeleton in their 2021 paper, which combines a rigid exoskeleton with a cable-driven exoskeleton. The exoskeleton transmits the load to the ground through a rigid frame, while the cable-driven mechanism applies assistive force to the human joints. The exoskeleton system reported in the paper weighs 5.6 kg and is capable of reducing the wearer’s net metabolic cost by 12.8%. Considering the definition of the hybrid cable-driven configuration mentioned earlier, our study ultimately classifies it under this category.
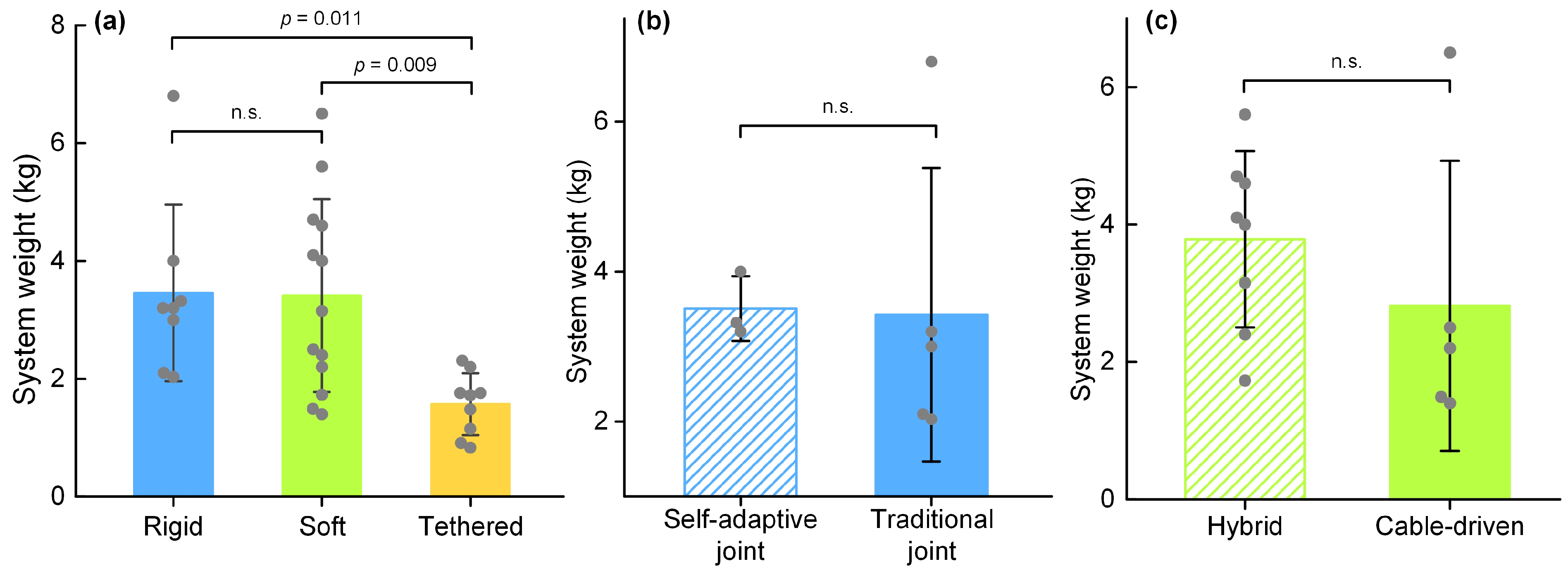
3.5. System Weight
We analyzed the system weight and device types of the 45 included articles. To ensure comparability, only exoskeleton systems providing assistance to a single joint were considered in this section. Therefore, the articles [41,57,84] were excluded. Additionally, the articles [36,39,40,45,55,59,60,67,69,87,89,94] were excluded due to the lack of information on system weight.
In this study, we compared the average system weights of the three structural types, as shown in Figure 6a. Additionally, for the rigid exoskeleton, we compared the use of adaptive mechanisms, as shown in Figure 6b. For the soft exoskeleton, we compared the hybrid cable-driven and cable-driven configurations, as shown in Figure 6c.
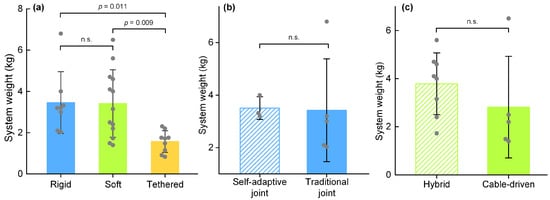
Figure 6.
The comparison of system weight; n.s. indicates not significant. (a) The comparison among three configurations. (b) The comparison of system weight between rigid exoskeletons with and without self-adaptive joint. (c) The comparison of system weight between hybrid cable-driven and cable-driven configurations.
For the weight data reported in all the included studies, we performed a Kruskal–Wallis H test for multi-sample related analysis, and applied Bonferroni correction for pairwise comparisons. For comparisons between two independent samples, we conducted the Mann–Whitney U test (significance level = 0.05; SPSS Statistics, IBM, New York, NY, USA).
In the 30 studies included in this section, no significant difference was observed in the average system weight between rigid exoskeletons and soft exoskeletons, with values of 3.45 ± 1.50 kg (n = 8; mean ± std) and 3.41 ± 1.64 kg (n = 13), respectively. The average system weight of the tethered platform was significantly lower than that of both rigid exoskeletons (p = 0.011) and soft exoskeletons (p = 0.009) at 1.57 ± 0.52 kg (n = 9).
In addition, among the eight studies on rigid exoskeletons analyzed in this section, three studies reported on adaptive joints [31,37,46], with an average system weight of 3.51 ± 0.43 kg. The remaining six studies reported an average system weight of 3.43 ± 1.96 kg. No significant difference in average system weight was observed between the two groups.
In the 13 studies on soft exoskeleton analyzed in this section, five studies utilized a cable-driven configuration with an average system weight of 2.82 ± 2.11 kg, whereas the remaining eight studies employed a hybrid cable-driven configuration with an average system weight of 3.79 ± 1.28 kg. No statistically significant difference in average system weight was observed between the two groups.
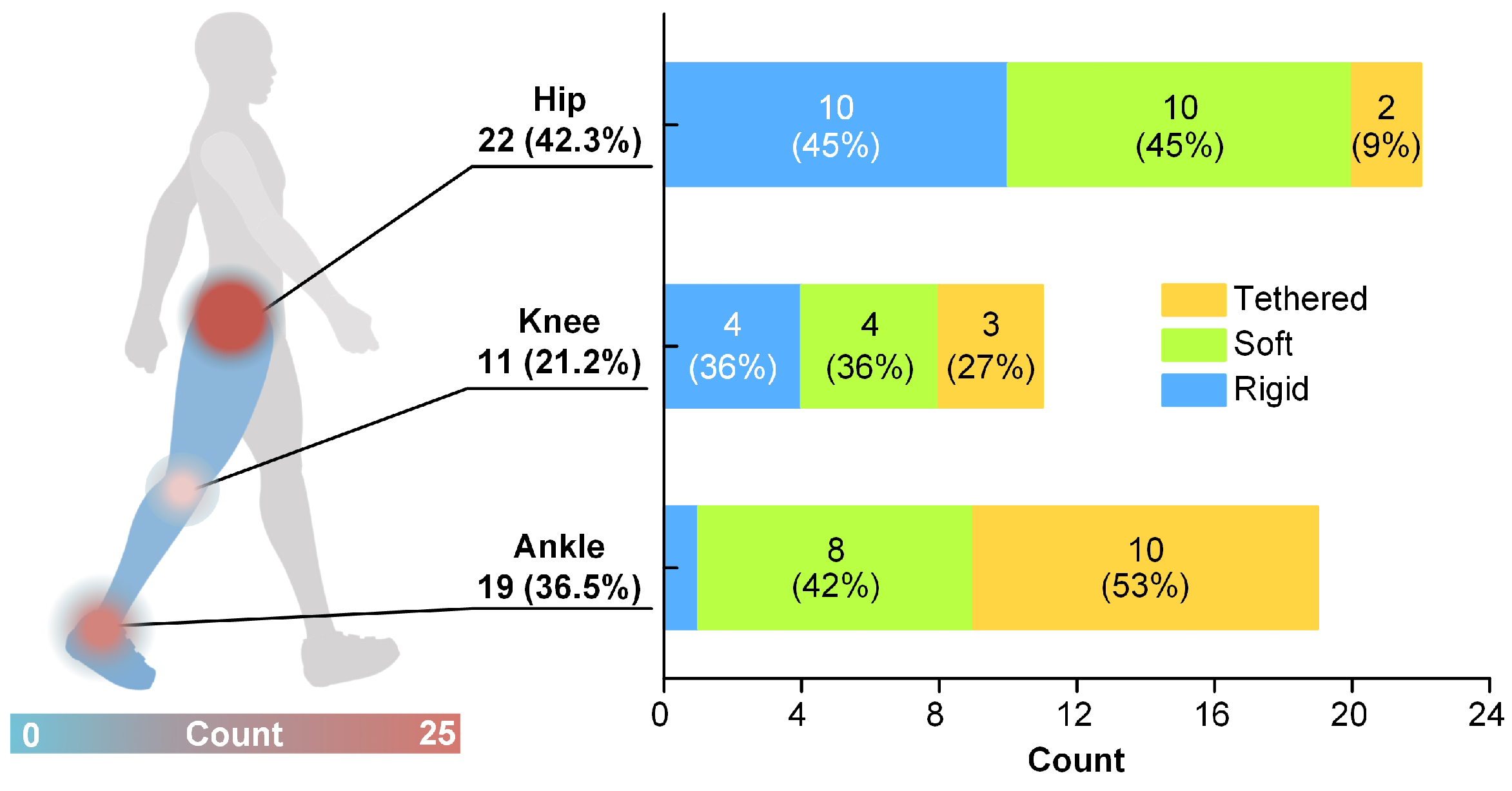
3.6. Target Joints
We analyzed the target assistive joints and device types across the 45 studies included in this research. For exoskeletons that provide assistance to multiple joints [40,41,57,59,60,84], we counted them as statistical data on the joints they assist. The statistical results are shown in Figure 7.
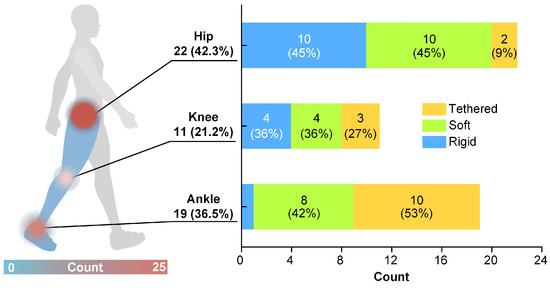
Figure 7.
The distribution of target assistive joints.
Among all the included reports, exoskeletons targeting the hip joint constituted the largest proportion, at 42.3%, followed by the ankle joint at 36.5%. For the knee joint, there is no clear preference across the three configurations, representing only 21.2% of the total. Most knee-targeting assistance is provided by multi-joint exoskeletons, with only four reports [43,70,90,92] focusing on single-joint knee assistance, which accounts for 36% of all knee-related exoskeleton reports. The majority of rigid exoskeletons target the hip joint, comprising 45% of all reports involving hip joint assistance. For tethered platforms, the primary target is the ankle joint, with 53% of all reports on ankle assistance involving this configuration.
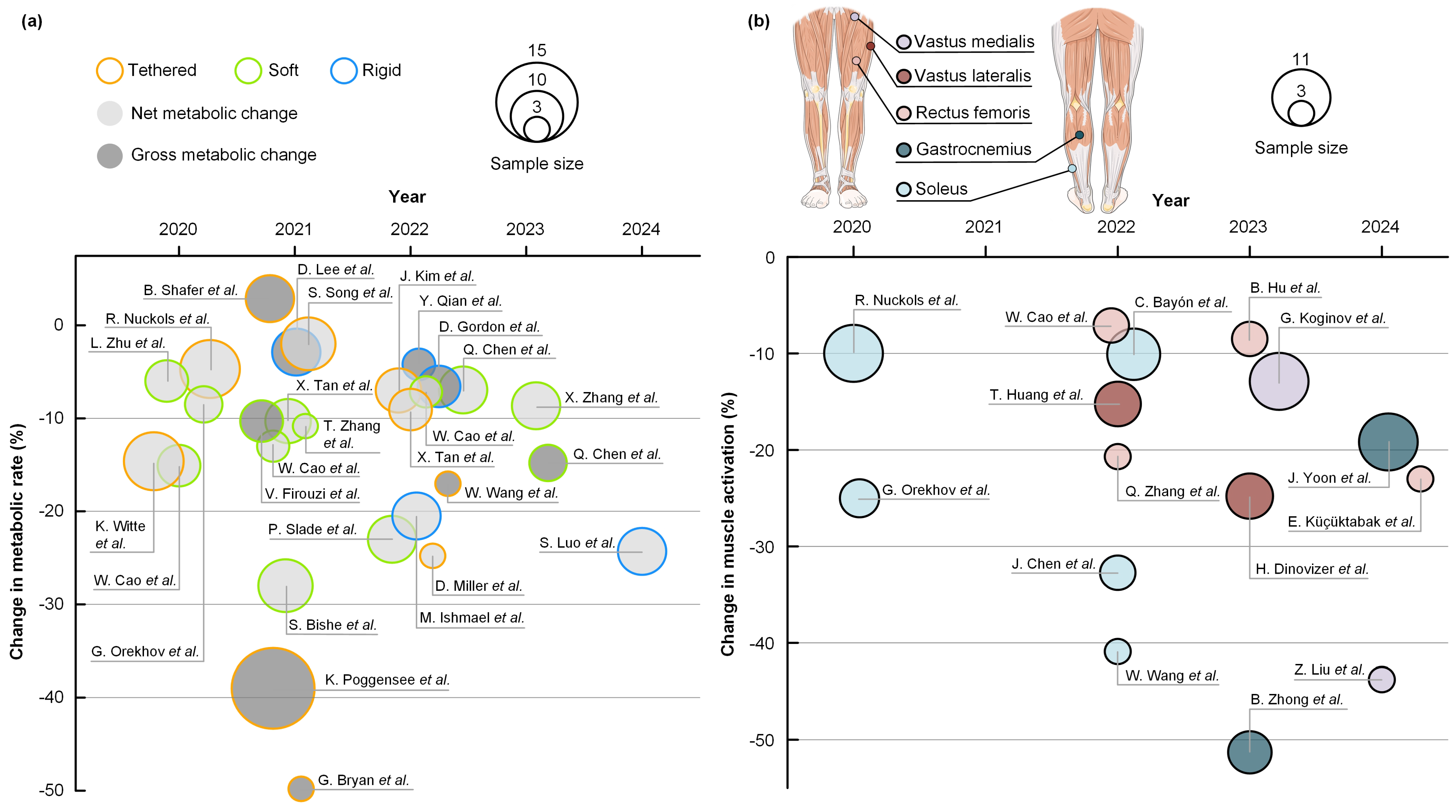
3.7. Major Effects
We analyzed the physiological experimental results reported in the 45 included studies. Six studies [37,39,55,56,63,90], which did not observe statistically significant differences in the experimental results, were excluded from this analysis. For studies that reported both gross metabolic change and net metabolic change, we considered the net metabolic change in our analysis. For studies that reported reduced muscle activation in multiple muscles, we selected the maximum value for analysis. The final statistical results are shown in Figure 8.
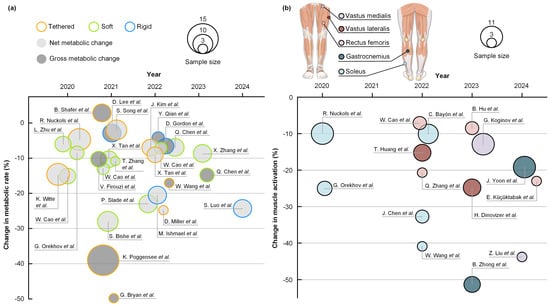
Figure 8.
Overview of physiological experimental results. The sample size refers to the number of participants reported in the study who were involved in physiological experiments. (a) The comparison of metabolic changes [33,37,38,42,44,46,58,59,60,61,62,64,66,67,71,72,73,83,84,85,86,87,88,93,94,95]. (b) The comparison of EMG muscle activity changes [31,36,40,41,43,45,57,62,68,70,72,85,88,89,92].
Human walking is a highly refined motion shaped by millions of years of evolution, and inappropriate external assistance can disrupt its natural movement balance, thereby increasing the body’s metabolic cost of movement [1,98]. To investigate the relationship between external assistance and human metabolic levels, D. Miller et al. [83] conducted a physiological study using a tethered platform designed for ankle assistance. The study focused on the effects of the peak assistive torque applied by the exoskeleton, as well as the timing of the application and removal of the assistive torque, on the participants’ metabolic rate during running. The experimental results demonstrated that the reduction in metabolic rate was nearly linearly related to the increase in peak torque but with diminishing returns at higher torque levels. When the peak torque reached 0.8 Nm/kg (normalized by body weight), the reduction in net metabolic cost was 24.8 ± 2.3%. Additionally, the timing of torque application should be as late as possible within the allowed range (80% support phase), and the removal of assistive torque should occur close to the toe-off time (100% support phase). These findings are consistent with those reported by U. Lee et al. [20].
Among the included soft exoskeletons, the study by S. Bishe et al. demonstrated the best assistive performance [67]. They proposed a novel ankle joint torque estimation model based on customized wearable sensors, which was integrated into a cable-driven exoskeleton controller for ankle joint assistance. This model enables the exoskeleton to provide assistive torques that can adapt in real time to the biological dorsi flexion torques of both healthy individuals and those with movement impairments. The control algorithm exhibited strong potential in clinical feasibility testing, including trials with four cerebral palsy patients. It was capable of providing precise assistance during gait activities such as uphill, downhill, stair climbing, and stair descending, resulting in an average reduction of 28% in net metabolic cost.
Traditional exoskeleton control system parameter adjustment methods heavily depend on the tuning expertise of control algorithm developers and physiological feedback from participants. This process is time-consuming and labor-intensive, severely limiting the development and widespread application of exoskeleton robots. To address this issue, S. Luo et al. [42] proposed a simulation-based reinforcement learning control algorithm that does not require experimental testing. This method utilizes three interrelated multilayer perception neural networks, each designed for mimicking human movement, adjusting the coordination of the musculoskeletal model, and controlling the exoskeleton robot. The proposed neural networks were trained using a dataset that included walking, running, and stair climbing, with the goal of improving control performance by maximizing the reward (i.e., reducing muscle activation). The trained controller was subsequently deployed on a rigid exoskeleton for hip assistance and tested with eight healthy participants. The experimental results demonstrated that the proposed controller effectively provided appropriate assistance for various movements, reducing the net metabolic cost of walking, running, and stair climbing by 24.3%, 13.1%, and 15.4%, respectively.
Among the 39 studies included in this section, 4 reported both metabolic rate changes and EMG activity experimental data [62,72,85,88]. It can be observed that the reported reductions in metabolic rate in these studies show a positive correlation with EMG activity, suggesting that muscle activation is a primary factor in metabolic energy expenditure [99]. Moreover, reducing the muscle activation of the rectus femoris [62] appears to be more effective compared to reducing the activation of the soleus [72,85,88] in reducing metabolic rate. This is because the hip muscles are relatively more adaptable in terms of power demand, allowing them to compensate for the reduced output at the ankle. Additionally, the hip’s power requirements are relatively lower, making it easier to achieve optimized assistance effects. The findings of B. Cseke et al. [100] further support this perspective.
4. Discussion
Notably, excluding three studies that did not report the age of participants [42,67,92], the remaining forty-two studies reported an average participant age of 27.00 ± 5.51. Among these, only studies [33,56] involved participants with relatively higher average ages, specifically 42.75 ± 15.16 and 46.50 ± 13.63, respectively. Previous studies [101] have shown that under the same loading conditions, young and middle-aged adults exhibit different kinematic responses, suggesting that the wearer’s age may influence the effectiveness of the exoskeleton. This suggests that future research on robotic exoskeleton should involve more recruitment of middle-aged and older adults as experimental participants, in order to explore the potential applications of exoskeletons in rehabilitation training and assistive technologies for the elderly and disabled.
From the statistical analysis of system weight across 45 articles, it can be observed that there is no significant difference in the overall weight between rigid exoskeletons and soft exoskeletons over the past five years. This is a noteworthy phenomenon, as researchers have long assumed that rigid exoskeletons are heavier due to the structural inclusion of more rigid links. For example, the rigid exoskeleton proposed by D. Hyun et al. [102] in 2017, designed for assisted weight-bearing walking, has a total system weight of 10 kg and features 12 degrees of freedom for both active and passive motions. It provides assistance to the wearer’s hip and knee joints, and experimental results show that it can assist in walking at 5 km/h or running at 10 km/h while carrying a 20 kg load. In contrast, the soft exoskeleton with a cable-driven configuration proposed by F. Panizzolo et al. [103] in 2019 weighs only 5.4 kg and provides walking assistance to the hip joint under load. Experimental results indicate that it can reduce the wearer’s gross metabolic cost by 10.1 ± 3.2% when carrying a load of 20.4 kg.
The reasons for the increasingly similar system weights of rigid exoskeletons and soft exoskeletons in recent years can be attributed to the following two aspects.
First, from the perspective of rigid exoskeletons, the introduction of new materials and manufacturing techniques, such as titanium alloys, carbon fiber materials, and additive manufacturing technologies, has significantly reduced the weight of rigid links [104]. Additionally, the advancement of finite element analysis techniques has led to the increasing application of topology optimization in the design of rigid components [105]. This enables further weight reduction while maintaining the performance and functionality of the rigid links. In addition, the maturation of servo motor technology has also changed the design approach of mechanical joints in rigid exoskeletons. Traditional mechanical joints typically consisted of high-speed servo motors, gear reducers with large reduction ratios, and torque sensors, with the weight of a single joint often exceeding 2 kg [35,49]. In recent years, the Quasi-Direct Drive (QDD) actuator has been introduced into the design of exoskeletons’ mechanical joints [43,104]. The primary components of QDD are high-torque servo motors and reducers with small reduction ratios. The highly back-drivable characteristic of this combination allows the servo motor controller to estimate the output torque based on the motor current, eliminating the need for integrated torque sensors. By removing the large reduction ratio gear reducer and torque sensors, the overall weight of QDD-based mechanical joints has been significantly reduced. For instance, the mechanical joint for hip assistance proposed by S. Yu et al. [106] weighs only 0.77 kg and produces an output torque of 17.5 Nm.
Secondly, as evidenced by the increasing proportion of hybrid configurations in recent soft exoskeleton studies, the current research focus is shifting toward hybrid designs. After years of research, it has been observed that soft exoskeletons with a cable-driven configuration suffer from significant slippage issues, known as “straps slippage” [8]. Specifically, while the Bowden cable provides assistive force, its sheath generates a reactive force in the opposite direction. This reactive force displaces the straps from their original positions, causing the anchor points on the straps to shift, thereby reducing the effectiveness of the assistive force [77]. Increasing the fixation strength of the straps can partially mitigate this issue, but excessive pressure on the straps can cause extreme discomfort for the wearer [22]. Previous studies have shown that when the straps’ pressure reaches 20–42 kPa, the wearer experiences pain, and when the pressure reaches 34–84 kPa, it becomes unbearable [107]. Furthermore, prolonged straps pressure may lead to nerve or vascular damage [108]. Additionally, there is a threshold for the tension that the human body can directly tolerate from the Bowden cable. When the cable tension exceeds this threshold, the wearer will experience intolerable pain [8,109]. All of these factors have collectively limited the development of cable-driven soft exoskeletons, prompting researchers to shift their focus toward hybrid configurations. The introduction of rigid components increases the contact area between the exoskeleton and the wearer’s body, making the transmission of assistance via Bowden cables more stable while reducing pressure on the wearer’s skin. However, this also inevitably adds to the overall weight of the system.
The statistical results for target assistive joints indicate that the primary target joints of exoskeletons for locomotion assistance are the hip and ankle joints, accounting for 78.8% of all cases. The hip and ankle joints are responsible for approximately 80% of the positive work output during human walking [12,110], making assistance for these joints more efficient. Notably, the majority of rigid exoskeletons target the hip joint for assistance. This is because the human body is more sensitive to weight increases at the extremities compared to the torso. Placing the same weight at the ankle joint has an impact on the wearer’s metabolic level that is approximately four times greater than placing it at the waist [80,81]. Rigid exoskeletons often position motors and other driving units near the target joint, which reduces the effectiveness of assisting the ankle joint due to the “weight penalty” issue. In contrast, soft exoskeletons place the motors on the back or waist, and tethered platforms place the motors on an off-board platform. Both approaches help minimize the impact of device weight on the wearer, thereby enabling effective assistance to the ankle joint.
The relatively small proportion of papers focusing on assisting the knee joint show that this is well understood, as the knee joint primarily absorbs energy during walking [111,112]. Therefore, providing active assistance to the knee joint during walking is less meaningful, as its primary function is energy absorption rather than motion output during the gait cycle. However, researchers have started to explore solutions that provide assistance by capturing the negative work of the knee joint during walking [113,114,115,116,117,118]. For example, M. Shepertycky et al. [14] utilized a cable-driven generator to provide decelerating assistance to the muscles near the knee joint during eccentric contraction while simultaneously converting the absorbed negative work into electrical energy for storage. This method can reduce the wearer’s net metabolic cost by 2.5% while generating 0.25 W of electrical power.
A cross-sectional comparison of studies published in the same year reveals that among the three configurations, the tethered platform performs the best in physiological experiments, followed by the soft exoskeleton, with the rigid exoskeleton performing the worst. This phenomenon highlights an issue that cannot be ignored, namely “joint misalignment” [22]. Most human joints are complex, composite joints, and the center of rotation changes with movement [119]. Although most current rigid exoskeletons have addressed the weight penalty issue, and statistical results regarding system weight show that the introduction of self-adaptive joints does not significantly increase the weight of the rigid exoskeleton, existing rigid exoskeletons still struggle to achieve real-time alignment with the human joints, resulting in misalignment issues. Joint misalignment can cause the rigid components of a rigid exoskeleton to impede the wearer’s natural movement, disrupting their normal walking pattern. This forces the wearer to expend additional effort to adjust their gait to achieve a new walking balance, increasing the metabolic cost of walking and reducing the assistive effect of the exoskeleton [1]. In contrast, the cable-driven design of soft exoskeletons and tethered platforms can automatically adapt to the human body’s structure without hindering the wearer’s movement. Additionally, tethered platforms have further addressed the weight penalty issue, resulting in even more favorable experimental outcomes.
Traditional servo motors consist of two main components: the stator and the rotor, which must be mounted on different parts of the exoskeleton. For rigid exoskeletons, these parts are two adjacent links; for soft exoskeletons, they are the motor base and the straps. This installation requirement is the primary cause of the aforementioned joint misalignment and strap slippage issues. In recent years, some researchers have proposed the use of wearable angular momentum exchange actuators, such as reaction wheels and control moment gyroscopes (CMGs) to provide support to human joints without relying on external links [120]. These devices apply assistance directly to the target limb through inertial or Coriolis forces without the need for linkages or Bowden cables. By removing these components, the root causes of joint misalignment and strap slippage are addressed. Researchers have already applied CMGs to assist limb swing [121], maintain balance [122], and prevent falls [123]. This approach holds significant application potential in wearable assistive devices and warrants further in-depth research.
Finally, due to individual variations in body characteristics and walking habits, a uniform exoskeleton assistance strategy may not be suitable for all wearers [23]. Inappropriate assistance may also disrupt the wearer’s natural walking balance, leading to negative effects from the exoskeleton’s support [97,98]. Among the 45 reviewed, those employing customized assistance strategies demonstrated superior results in physiological tests [42,57,71,83,93,95]. U. Lee et al. [20] proposed an online reinforcement-learning-based methodology for customizing assistance strategies. By providing participants with an interactive interface, they allowed subjects to select between two randomly generated ankle assistance strategies based on personal preference. This selection process was utilized to optimize the intervention timing and peak torque of the exoskeleton assistance. This method can swiftly determine the optimal assistance strategy for each individual, significantly reducing the tuning time for exoskeleton controllers. Moreover, current customization strategies for exoskeleton assistance predominantly concentrate on adjusting the timing of assistance intervention and peak torque [19]. This underscores the importance of developing a robust and reliable gait detection methodology to determine the optimal timing for assistance intervention as the interest in personalized customized assistance strategies will continue to grow in future research [124,125].
5. Conclusions
In summary, this review highlights the significant advancements in the development of robotic exoskeletons for locomotion assistance, with a particular focus on the analysis of structural designs. While rigid exoskeletons have demonstrated robust performance in load support and rehabilitation, their limitations, such as weight penalties and joint misalignments, highlight the need for more flexible and adaptive designs. Soft exoskeletons, characterized by compliant structures and innovative actuation mechanisms, offer promising solutions to enhance wearer comfort and metabolic efficiency. However, challenges such as optimizing control strategies for individualized assistance and ensuring seamless human–exoskeleton integration remain critical barriers to widespread adoption.
Looking ahead, addressing these challenges will necessitate multidisciplinary efforts. As the field advances, innovations in material science, biomechanics, and artificial intelligence are anticipated to play pivotal roles in shaping the future of exoskeleton technology. Ultimately, advancs in these wearable assistive devices will broaden their applications in rehabilitation, industrial support, and other domains, thereby significantly enhancing mobility and quality of life for diverse user populations.
Author Contributions
Methodology, data analysis, writing, W.L.; Conceptualization, project administration, W.D.; Investigation, visualization, W.W., Y.G., D.W., Y.L., L.H., and X.M.; Supervision, formal analysis, H.D. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China under Grant No. U21A20120.
Institutional Review Board Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
The authors thank everyone who provided suggestions and assistance for this research and paper.
Conflicts of Interest
L.H. and X.M. has been involved as a consultant and expert witness in the Zhiyuan Research Institute. The other authors declare no conflicts of interest.
References
- Collins, S.H.; Wiggin, M.B.; Sawicki, G.S. Reducing the energy cost of human walking using an unpowered exoskeleton. Nature 2015, 522, 212–215. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Johnson, W.D.; Katzmarzyk, P.T. Accelerometer-determined steps per day in US adults. Med. Sci. Sport. Exerc. 2009, 41, 1384–1391. [Google Scholar] [CrossRef] [PubMed]
- Westerterp, K.R. Physical activity and physical activity induced energy expenditure in humans: Measurement, determinants, and effects. Front. Physiol. 2013, 4, 90. [Google Scholar] [CrossRef] [PubMed]
- McGibbon, C.A. Toward a better understanding of gait changes with age and disablement: Neuromuscular adaptation. Exerc. Sport Sci. Rev. 2003, 31, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Proud, J.K.; Lai, D.T.; Mudie, K.L.; Carstairs, G.L.; Billing, D.C.; Garofolini, A.; Begg, R.K. Exoskeleton application to military manual handling tasks. Hum. Factors 2022, 64, 527–554. [Google Scholar] [CrossRef]
- Li, T.; Li, Q. A systematic review on load carriage assistive devices: Mechanism design and performance evaluation. Mech. Mach. Theory 2023, 180, 105142. [Google Scholar] [CrossRef]
- Zhuang, Z.; Guan, Y.; Xu, S.; Dai, J.S. Reconfigurability in automobiles—Structure, manufacturing and algorithm for automobiles. Int. J. Automot. Manuf. Mater. 2022, 1, 1. [Google Scholar] [CrossRef]
- Xiloyannis, M.; Alicea, R.; Georgarakis, A.M.; Haufe, F.L.; Wolf, P.; Masia, L.; Riener, R. Soft robotic suits: State of the art, core technologies, and open challenges. IEEE Trans. Robot. 2021, 38, 1343–1362. [Google Scholar] [CrossRef]
- Segura-Vega, J.; González-Herrera, A.; Molina-Bravo, R.; Solano-González, S. Computational identification and characterization of chitinase 1 and chitinase 2 from neotropical isolates of Beauveria bassiana. Front. Bioinform. 2024, 4, 1434442. [Google Scholar] [CrossRef]
- Bao, G.; Pan, L.; Fang, H.; Wu, X.; Yu, H.; Cai, S.; Yu, B.; Wan, Y. Academic review and perspectives on robotic exoskeletons. IEEE Trans. Neural Syst. Rehabil. Eng. 2019, 27, 2294–2304. [Google Scholar] [CrossRef]
- Fan, W.; Dai, Z.; Zhang, B.; He, L.; Pan, M.; Yi, J.; Liu, T. HyExo: A Novel Quasi-Passive Hydraulic Exoskeleton for Load-Carrying Augmentation. IEEE/ASME Trans. Mechatron. 2024. [Google Scholar] [CrossRef]
- Liang, J.; Zhang, Q.; Liu, Y.; Wang, T.; Wan, G. A review of the design of load-carrying exoskeletons. Sci. China Technol. Sci. 2022, 65, 2051–2067. [Google Scholar] [CrossRef] [PubMed]
- Colucci, A.; Vermehren, M.; Cavallo, A.; Angerhöfer, C.; Peekhaus, N.; Zollo, L.; Kim, W.S.; Paik, N.J.; Soekadar, S.R. Brain-computer interface-controlled exoskeletons in clinical neurorehabilitation: Ready or not? Neurorehabilit. Neural Repair 2022, 36, 747–756. [Google Scholar] [CrossRef] [PubMed]
- Shepertycky, M.; Burton, S.; Dickson, A.; Liu, Y.F.; Li, Q. Removing energy with an exoskeleton reduces the metabolic cost of walking. Science 2021, 372, 957–960. [Google Scholar] [CrossRef] [PubMed]
- Siviy, C.; Baker, L.M.; Quinlivan, B.T.; Porciuncula, F.; Swaminathan, K.; Awad, L.N.; Walsh, C.J. Opportunities and challenges in the development of exoskeletons for locomotor assistance. Nat. Biomed. Eng. 2023, 7, 456–472. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Zhou, D.; Leng, Y. A Systematic Review on Rigid Exoskeleton Robot Design for Wearing Comfort: Joint Self-Alignment, Attachment Interface, and Structure Customization. IEEE Trans. Neural Syst. Rehabil. Eng. 2024, 32, 3815–3827. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Li, X.; Huang, T.H.; Yu, S.; Li, Y.; Chen, T.; Carriero, A.; Oh-Park, M.; Su, H. Comfort-centered design of a lightweight and backdrivable knee exoskeleton. IEEE Robot. Autom. Lett. 2018, 3, 4265–4272. [Google Scholar] [CrossRef]
- Zhang, Q.; Dong, W.; Xu, Q.; Goteea, B.J.; Gao, Y. FlexDelta: A flexure-based fully decoupled parallel xyz positioning stage with a long stroke. Precis. Eng. 2024, 88, 707–717. [Google Scholar] [CrossRef]
- Ingraham, K.A.; Remy, C.D.; Rouse, E.J. The role of user preference in the customized control of robotic exoskeletons. Sci. Robot. 2022, 7, eabj3487. [Google Scholar] [CrossRef] [PubMed]
- Lee, U.H.; Shetty, V.S.; Franks, P.W.; Tan, J.; Evangelopoulos, G.; Ha, S.; Rouse, E.J. User preference optimization for control of ankle exoskeletons using sample efficient active learning. Sci. Robot. 2023, 8, eadg3705. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Gao, Y.; Meng, S.; Dong, H.; Ru, C.; Dong, W. A Novel Contouring Control Method Based on Optimal Vector-Referenced Moving Frame for 3D Trajectory with Zero Curvature. IEEE Trans. Autom. Sci. Eng. 2024. [Google Scholar] [CrossRef]
- Scherb, D.; Wartzack, S.; Miehling, J. Modelling the interaction between wearable assistive devices and digital human models—A systematic review. Front. Bioeng. Biotechnol. 2023, 10, 1044275. [Google Scholar] [CrossRef] [PubMed]
- Quinlivan, B.T.; Lee, S.; Malcolm, P.; Rossi, D.M.; Grimmer, M.; Siviy, C.; Karavas, N.; Wagner, D.; Asbeck, A.; Galiana, I.; et al. Assistance magnitude versus metabolic cost reductions for a tethered multiarticular soft exosuit. Sci. Robot. 2017, 2, eaah4416. [Google Scholar] [CrossRef] [PubMed]
- Fu, J.; Choudhury, R.; Hosseini, S.M.; Simpson, R.; Park, J.H. Myoelectric control systems for upper limb wearable robotic exoskeletons and exosuits—A systematic review. Sensors 2022, 22, 8134. [Google Scholar] [CrossRef]
- Donisi, L.; Cesarelli, G.; Pisani, N.; Ponsiglione, A.M.; Ricciardi, C.; Capodaglio, E. Wearable sensors and artificial intelligence for physical ergonomics: A systematic review of literature. Diagnostics 2022, 12, 3048. [Google Scholar] [CrossRef] [PubMed]
- Coser, O.; Tamantini, C.; Soda, P.; Zollo, L. AI-based methodologies for exoskeleton-assisted rehabilitation of the lower limb: A review. Front. Robot. AI 2024, 11, 1341580. [Google Scholar] [CrossRef]
- Lee, H.; Ferguson, P.W.; Rosen, J. Lower limb exoskeleton systems—Overview. Wearable Robot. 2020, 2020, 207–229. [Google Scholar]
- Rudnicka, A.R.; Owen, C.G. An introduction to systematic reviews and meta-analyses in health care. Ophthalmic Physiol. Opt. 2012, 32, 174–183. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, W-65–W-94. [Google Scholar] [CrossRef]
- Meijneke, C.; Van Oort, G.; Sluiter, V.; Van Asseldonk, E.; Tagliamonte, N.; Tamburella, F.; Pisotta, I.; Masciullo, M.; Arquilla, M.; Molinari, M.; et al. Symbitron exoskeleton: Design, control, and evaluation of a modular exoskeleton for incomplete and complete spinal cord injured individuals. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 330–339. [Google Scholar] [CrossRef]
- Hu, B.; Liu, F.; Cheng, K.; Chen, W.; Shan, X.; Yu, H. Stiffness optimal modulation of a variable stiffness energy storage hip exoskeleton and experiments on its assistance effect. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 1045–1055. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Du, Z.; Dong, W.; Shen, Y.; Zhao, G. Hierarchical human machine interaction learning for a lower extremity augmentation device. Int. J. Soc. Robot. 2019, 11, 123–139. [Google Scholar] [CrossRef]
- Ishmael, M.K.; Gunnell, A.; Pruyn, K.; Creveling, S.; Hunt, G.; Hood, S.; Archangeli, D.; Foreman, K.B.; Lenzi, T. Powered hip exoskeleton reduces residual hip effort without affecting kinematics and balance in individuals with above-knee amputations during walking. IEEE Trans. Biomed. Eng. 2022, 70, 1162–1171. [Google Scholar] [CrossRef] [PubMed]
- Sarkisian, S.V.; Ishmael, M.K.; Lenzi, T. Self-aligning mechanism improves comfort and performance with a powered knee exoskeleton. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 629–640. [Google Scholar] [CrossRef]
- Chen, C.F.; Du, Z.J.; He, L.; Shi, Y.J.; Wang, J.Q.; Xu, G.Q.; Zhang, Y.; Wu, D.M.; Dong, W. Development and hybrid control of an electrically actuated lower limb exoskeleton for motion assistance. IEEE Access 2019, 7, 169107–169122. [Google Scholar] [CrossRef]
- Bayón, C.; Keemink, A.Q.; van Mierlo, M.; Rampeltshammer, W.; van der Kooij, H.; van Asseldonk, E.H. Cooperative ankle-exoskeleton control can reduce effort to recover balance after unexpected disturbances during walking. J. Neuroeng. Rehabil. 2022, 19, 21. [Google Scholar] [CrossRef] [PubMed]
- Zhang, T.; Li, Y.; Ning, C.; Zeng, B. Development and adaptive assistance control of the robotic hip exoskeleton to improve gait symmetry and restore normal gait. IEEE Trans. Autom. Sci. Eng. 2022, 21, 799–809. [Google Scholar] [CrossRef]
- Gordon, D.F.; McGreavy, C.; Christou, A.; Vijayakumar, S. Human-in-the-loop optimization of exoskeleton assistance via online simulation of metabolic cost. IEEE Trans. Robot. 2022, 38, 1410–1429. [Google Scholar] [CrossRef]
- Alili, A.; Fleming, A.; Nalam, V.; Liu, M.; Dean, J.; Huang, H. Abduction/adduction assistance from powered hip exoskeleton enables modulation of user step width during walking. IEEE Trans. Biomed. Eng. 2023, 71, 334–342. [Google Scholar] [CrossRef] [PubMed]
- Dinovitzer, H.; Shushtari, M.; Arami, A. Feedforward Control of Lower Limb Exoskeletons: Which Torque Profile Should We Use? IEEE Robot. Autom. Lett. 2023, 9, 382–389. [Google Scholar] [CrossRef]
- Barıs, E.; Wen, Y.; Kim, S.J.; Short, M.R.; Ludvig, D.; Hargrove, L.; Perreault, E.J.; Lynch, K.M.; Pons, J.L. Haptic transparency and interaction force control for a lower-limb exoskeleton. IEEE Trans. Robot. 2024, 40, 1842–1859. [Google Scholar]
- Luo, S.; Jiang, M.; Zhang, S.; Zhu, J.; Yu, S.; Dominguez Silva, I.; Wang, T.; Rouse, E.; Zhou, B.; Yuk, H.; et al. Experiment-free exoskeleton assistance via learning in simulation. Nature 2024, 630, 353–359. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.H.; Zhang, S.; Yu, S.; MacLean, M.K.; Zhu, J.; Di Lallo, A.; Jiao, C.; Bulea, T.C.; Zheng, M.; Su, H. Modeling and stiffness-based continuous torque control of lightweight quasi-direct-drive knee exoskeletons for versatile walking assistance. IEEE Trans. Robot. 2022, 38, 1442–1459. [Google Scholar] [CrossRef]
- Lee, D.; McLain, B.J.; Kang, I.; Young, A.J. Biomechanical comparison of assistance strategies using a bilateral robotic knee exoskeleton. IEEE Trans. Biomed. Eng. 2021, 68, 2870–2879. [Google Scholar] [CrossRef]
- Zhang, Q.; Nalam, V.; Tu, X.; Li, M.; Si, J.; Lewek, M.D.; Huang, H.H. Imposing healthy hip motion pattern and range by exoskeleton control for individualized assistance. IEEE Robot. Autom. Lett. 2022, 7, 11126–11133. [Google Scholar] [CrossRef]
- Qian, Y.; Han, S.; Wang, Y.; Yu, H.; Fu, C. Toward improving actuation transparency and safety of a hip exoskeleton with a novel nonlinear series elastic actuator. IEEE/ASME Trans. Mechatron. 2022, 28, 417–428. [Google Scholar] [CrossRef]
- Moreno, J.C.; Vitiello, N.; Walsh, C.; Huang, H.; Mohammed, S. Introduction to the special section on wearable robots. IEEE Trans. Robot. 2022, 38, 1338–1342. [Google Scholar] [CrossRef]
- Wang, L.; Chen, C.; Li, Z.; Dong, W.; Du, Z.; Shen, Y.; Zhao, G. High precision data-driven force control of compact elastic module for a lower extremity augmentation device. J. Bionic Eng. 2018, 15, 805–819. [Google Scholar] [CrossRef]
- Long, Y.; Du, Z.; Chen, C.; Wang, W.; Dong, W. Development of a lower extremity wearable exoskeleton with double compact elastic module: Preliminary experiments. Mech. Sci. 2017, 8, 249–258. [Google Scholar] [CrossRef]
- Zhou, L.; Chen, W.; Chen, W.; Bai, S.; Zhang, J.; Wang, J. Design of a passive lower limb exoskeleton for walking assistance with gravity compensation. Mech. Mach. Theory 2020, 150, 103840. [Google Scholar] [CrossRef]
- Liu, L.; Leonhardt, S.; Ngo, C.; Misgeld, B.J. Impedance-controlled variable stiffness actuator for lower limb robot applications. IEEE Trans. Autom. Sci. Eng. 2019, 17, 991–1004. [Google Scholar] [CrossRef]
- Jafari, A.; Tsagarakis, N.G.; Caldwell, D.G. A novel intrinsically energy efficient actuator with adjustable stiffness (AwAS). IEEE/ASME Trans. Mechatron. 2011, 18, 355–365. [Google Scholar] [CrossRef]
- Wang, L.; Du, Z.; Dong, W.; Shen, Y.; Zhao, G. Intrinsic sensing and evolving internal model control of compact elastic module for a lower extremity exoskeleton. Sensors 2018, 18, 909. [Google Scholar] [CrossRef]
- Cammarata, A.; Maddio, P.D.; Sinatra, R.; Belfiore, N.P. Direct Kinetostatic analysis of a gripper with curved flexures. Micromachines 2022, 13, 2172. [Google Scholar] [CrossRef] [PubMed]
- Conner, B.C.; Orekhov, G.; Lerner, Z.F. Ankle exoskeleton assistance increases six-minute walk test performance in cerebral palsy. IEEE Open J. Eng. Med. Biol. 2021, 2, 320–323. [Google Scholar] [CrossRef]
- Awad, L.N.; Kudzia, P.; Revi, D.A.; Ellis, T.D.; Walsh, C.J. Walking faster and farther with a soft robotic exosuit: Implications for post-stroke gait assistance and rehabilitation. IEEE Open J. Eng. Med. Biol. 2020, 1, 108–115. [Google Scholar] [CrossRef] [PubMed]
- Zhong, B.; Shen, M.; Liu, H.; Zhao, Y.; Qian, Q.; Wang, W.; Yu, H.; Zhang, M. A cable-driven exoskeleton with personalized assistance improves the gait metrics of people in subacute stroke. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 31, 2560–2569. [Google Scholar] [CrossRef]
- Chen, Q.; Guo, S.; Wang, J.; Wang, J.; Zhang, D.; Jin, S. Biomechanical and physiological evaluation of biologically-inspired hip assistance with belt-type soft exosuits. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 30, 2802–2814. [Google Scholar] [CrossRef]
- Zhu, L.; Wang, Z.; Ning, Z.; Zhang, Y.; Liu, Y.; Cao, W.; Wu, X.; Chen, C. A novel motion intention recognition approach for soft exoskeleton via IMU. Electronics 2020, 9, 2176. [Google Scholar] [CrossRef]
- Firouzi, V.; Davoodi, A.; Bahrami, F.; Sharbafi, M.A. From a biological template model to gait assistance with an exosuit. Bioinspir. Biomim. 2021, 16, 066024. [Google Scholar] [CrossRef]
- Zhang, X.; Tricomi, E.; Missiroli, F.; Lotti, N.; Masia, L. Real-Time Assistive Control via IMU Locomotion Mode Detection in a Soft Exosuit: An Effective Approach to Enhance Walking Metabolic Efficiency. IEEE/ASME Trans. Mechatron. 2024, 29, 1797–1808. [Google Scholar] [CrossRef]
- Cao, W.; Ma, Y.; Chen, C.; Zhang, J.; Wu, X. Hardware circuits design and performance evaluation of a soft lower limb exoskeleton. IEEE Trans. Biomed. Circuits Syst. 2022, 16, 384–394. [Google Scholar] [CrossRef]
- Tricomi, E.; Lotti, N.; Missiroli, F.; Zhang, X.; Xiloyannis, M.; Müller, T.; Crea, S.; Papp, E.; Krzywinski, J.; Vitiello, N.; et al. Underactuated soft hip exosuit based on adaptive oscillators to assist human locomotion. IEEE Robot. Autom. Lett. 2021, 7, 936–943. [Google Scholar] [CrossRef]
- Tan, X.; Zhang, B.; Liu, G.; Zhao, X.; Zhao, Y. Cadence-insensitive soft exoskeleton design with adaptive gait state detection and iterative force control. IEEE Trans. Autom. Sci. Eng. 2021, 19, 2108–2121. [Google Scholar] [CrossRef]
- Zhang, T.; Feng, K.; Zeng, B.; Gong, Z. Design and validation of a lightweight soft hip exosuit with series-wedge-structures for assistive walking and running. IEEE/ASME Trans. Mechatron. 2021, 27, 2863–2874. [Google Scholar] [CrossRef]
- Cao, W.; Chen, C.; Wang, D.; Wu, X.; Chen, L.; Xu, T.; Liu, J. A lower limb exoskeleton with rigid and soft structure for loaded walking assistance. IEEE Robot. Autom. Lett. 2021, 7, 454–461. [Google Scholar] [CrossRef]
- Bishe, S.S.P.A.; Nguyen, T.; Fang, Y.; Lerner, Z.F. Adaptive ankle exoskeleton control: Validation across diverse walking conditions. IEEE Trans. Med. Robot. Bionics 2021, 3, 801–812. [Google Scholar] [CrossRef]
- Chen, J.; Han, J.; Zhang, J. Design and evaluation of a mobile ankle exoskeleton with switchable actuation configurations. IEEE/ASME Trans. Mechatron. 2022, 27, 1846–1853. [Google Scholar] [CrossRef]
- Chen, Q.; Guo, S.; Zhang, D. Force Tracking Control with Adaptive Stiffness and Iterative Position of Hip-Assistive Soft Exosuits. IEEE Trans. Autom. Sci. Eng. 2024, 21, 7203–7218. [Google Scholar] [CrossRef]
- Koginov, G.; Bergmann, L.; Xiloyannis, M.; Rohner, N.; Ngo, C.; Duarte, J.E.; Leonhardt, S.; Riener, R. Human-in-the-Loop Personalization of a Bi-Articular Wearable Robot’s Assistance for Downhill Walking. IEEE Trans. Med. Robot. Bionics 2024, 6, 328–339. [Google Scholar] [CrossRef]
- Slade, P.; Kochenderfer, M.J.; Delp, S.L.; Collins, S.H. Personalizing exoskeleton assistance while walking in the real world. Nature 2022, 610, 277–282. [Google Scholar] [CrossRef]
- Orekhov, G.; Fang, Y.; Luque, J.; Lerner, Z.F. Ankle exoskeleton assistance can improve over-ground walking economy in individuals with cerebral palsy. IEEE Trans. Neural Syst. Rehabil. Eng. 2020, 28, 461–467. [Google Scholar] [CrossRef] [PubMed]
- Cao, W.; Chen, C.; Hu, H.; Fang, K.; Wu, X. Effect of hip assistance modes on metabolic cost of walking with a soft exoskeleton. IEEE Trans. Autom. Sci. Eng. 2020, 18, 426–436. [Google Scholar] [CrossRef]
- Gao, F.; Li, J.; Sun, G. Efficient and accurate flexible multibody dynamics modeling for complex spacecraft with integrated control applications. Acta Astronaut. 2024, 219, 818–825. [Google Scholar] [CrossRef]
- Zorkot, M.; Dac, L.H.; Morya, E.; Brasil, F.L. G-Exos: A wearable gait exoskeleton for walk assistance. Front. Neurorobot. 2022, 16, 939241. [Google Scholar]
- Lessard, S.; Pansodtee, P.; Robbins, A.; Trombadore, J.M.; Kurniawan, S.; Teodorescu, M. A soft exosuit for flexible upper-extremity rehabilitation. IEEE Trans. Neural Syst. Rehabil. Eng. 2018, 26, 1604–1617. [Google Scholar] [CrossRef] [PubMed]
- Shi, Y.; Gao, Y.; Lin, W.; He, L.; Mao, X.; Long, Y.; Dong, W. A cable-driven exosuit for upper limbs: Design, control, and evaluation. Proc. Inst. Mech. Eng. Part C J. Mech. Eng. Sci. 2024, 238, 9810–9824. [Google Scholar] [CrossRef]
- Shi, Y.; Gao, Y.; Lin, W.; He, L.; Mao, X.; Long, Y.; Dong, W. Human-in-the-Loop Modeling and Control of an Upper Limb Exosuit with Tendon-Sheath Actuation. IEEE Robot. Autom. Lett. 2024, 9, 5919–5926. [Google Scholar] [CrossRef]
- Hoogkamer, W.; Kipp, S.; Spiering, B.A.; Kram, R. Altered running economy directly translates to altered distance-running performance. Med. Sci. Sport. Exerc. 2016, 48, 2175–2180. [Google Scholar] [CrossRef]
- Browning, R.C.; Modica, J.R.; Kram, R.; Goswami, A. The effects of adding mass to the legs on the energetics and biomechanics of walking. Med. Sci. Sport. Exerc. 2007, 39, 515–525. [Google Scholar] [CrossRef] [PubMed]
- Schertzer, E.; Riemer, R. Metabolic rate of carrying added mass: A function of walking speed, carried mass and mass location. Appl. Ergon. 2014, 45, 1422–1432. [Google Scholar] [CrossRef] [PubMed]
- Coifman, I.; Kram, R.; Riemer, R. Metabolic power response to added mass on the lower extremities during running. Appl. Ergon. 2024, 114, 104109. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.E.; Tan, G.R.; Farina, E.M.; Sheets-Singer, A.L.; Collins, S.H. Characterizing the relationship between peak assistance torque and metabolic cost reduction during running with ankle exoskeletons. J. Neuroeng. Rehabil. 2022, 19, 46. [Google Scholar] [CrossRef] [PubMed]
- Bryan, G.M.; Franks, P.W.; Song, S.; Voloshina, A.S.; Reyes, R.; O’Donovan, M.P.; Gregorczyk, K.N.; Collins, S.H. Optimized hip-knee-ankle exoskeleton assistance at a range of walking speeds. J. Neuroeng. Rehabil. 2021, 18, 152. [Google Scholar] [CrossRef]
- Wang, W.; Chen, J.; Ding, J.; Zhang, J.; Liu, J. Improving walking economy with an ankle exoskeleton prior to human-in-the-loop optimization. Front. Neurorobot. 2022, 15, 797147. [Google Scholar] [CrossRef]
- Kim, J.; Quinlivan, B.T.; Deprey, L.A.; Arumukhom Revi, D.; Eckert-Erdheim, A.; Murphy, P.; Orzel, D.; Walsh, C.J. Reducing the energy cost of walking with low assistance levels through optimized hip flexion assistance from a soft exosuit. Sci. Rep. 2022, 12, 11004. [Google Scholar] [CrossRef] [PubMed]
- Shafer, B.A.; Philius, S.A.; Nuckols, R.W.; McCall, J.; Young, A.J.; Sawicki, G.S. Neuromechanics and energetics of walking with an ankle exoskeleton using neuromuscular-model based control: A parameter study. Front. Bioeng. Biotechnol. 2021, 9, 615358. [Google Scholar] [CrossRef]
- Nuckols, R.W.; Sawicki, G.S. Impact of elastic ankle exoskeleton stiffness on neuromechanics and energetics of human walking across multiple speeds. J. Neuroeng. Rehabil. 2020, 17, 1–19. [Google Scholar] [CrossRef]
- Yoon, J.E.; Chung, J.; Park, S.; Won, H.; Kim, C.; Baek, I.; Koh, J.S.; Koo, S.H. Evaluation of Gait-assistive soft wearable robot designs for wear comfort, focusing on electroencephalogram and satisfaction. IEEE Robot. Autom. Lett. 2024, 9, 8834–8841. [Google Scholar] [CrossRef]
- Park, E.J.; Akbas, T.; Eckert-Erdheim, A.; Sloot, L.H.; Nuckols, R.W.; Orzel, D.; Schumm, L.; Ellis, T.D.; Awad, L.N.; Walsh, C.J. A hinge-free, non-restrictive, lightweight tethered exosuit for knee extension assistance during walking. IEEE Trans. Med. Robot. Bionics 2020, 2, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Tan, X.; Zhang, B.; Liu, G.; Zhao, X.; Zhao, Y. A time-independent control system for natural human gait assistance with a soft exoskeleton. IEEE Trans. Robot. 2022, 39, 1653–1667. [Google Scholar] [CrossRef]
- Liu, Z.; Han, J.; Han, J.; Zhang, J. Design and Evaluation of a Lightweight, Ligaments-Inspired Knee Exoskeleton for Walking Assistance. IEEE Robot. Autom. Lett. 2024, 9, 8491–8498. [Google Scholar] [CrossRef]
- Witte, K.A.; Fiers, P.; Sheets-Singer, A.L.; Collins, S.H. Improving the energy economy of human running with powered and unpowered ankle exoskeleton assistance. Sci. Robot. 2020, 5, eaay9108. [Google Scholar] [CrossRef] [PubMed]
- Song, S.; Collins, S.H. Optimizing exoskeleton assistance for faster self-selected walking. IEEE Trans. Neural Syst. Rehabil. Eng. 2021, 29, 786–795. [Google Scholar] [CrossRef]
- Poggensee, K.L.; Collins, S.H. How adaptation, training, and customization contribute to benefits from exoskeleton assistance. Sci. Robot. 2021, 6, eabf1078. [Google Scholar] [CrossRef]
- Bryan, G.M.; Franks, P.W.; Klein, S.C.; Peuchen, R.J.; Collins, S.H. A hip-knee-ankle exoskeleton emulator for studying gait assistance. Int. J. Robot. Res. 2021, 40, 722–746. [Google Scholar] [CrossRef]
- Zhang, J.; Fiers, P.; Witte, K.A.; Jackson, R.W.; Poggensee, K.L.; Atkeson, C.G.; Collins, S.H. Human-in-the-loop optimization of exoskeleton assistance during walking. Science 2017, 356, 1280–1284. [Google Scholar] [CrossRef]
- Beck, O.N.; Shepherd, M.K.; Rastogi, R.; Martino, G.; Ting, L.H.; Sawicki, G.S. Exoskeletons need to react faster than physiological responses to improve standing balance. Sci. Robot. 2023, 8, eadf1080. [Google Scholar] [CrossRef]
- Chen, W.; Wu, S.; Zhou, T.; Xiong, C. On the biological mechanics and energetics of the hip joint muscle–tendon system assisted by passive hip exoskeleton. Bioinspir. Biomim. 2018, 14, 016012. [Google Scholar] [CrossRef] [PubMed]
- Cseke, B.; Uchida, T.K.; Doumit, M. Simulating ideal assistive strategies to reduce the metabolic cost of walking in the elderly. IEEE Trans. Biomed. Eng. 2022, 69, 2797–2805. [Google Scholar] [CrossRef]
- Vijayan, V.; Fang, S.; Reissman, T.; Reissman, M.E.; Kinney, A.L. How does added mass affect the gait of middle-aged adults? An assessment using statistical parametric mapping. Sensors 2022, 22, 6154. [Google Scholar] [CrossRef]
- Hyun, D.J.; Park, H.; Ha, T.; Park, S.; Jung, K. Biomechanical design of an agile, electricity-powered lower-limb exoskeleton for weight-bearing assistance. Robot. Auton. Syst. 2017, 95, 181–195. [Google Scholar] [CrossRef]
- Panizzolo, F.A.; Freisinger, G.M.; Karavas, N.; Eckert-Erdheim, A.M.; Siviy, C.; Long, A.; Zifchock, R.A.; LaFiandra, M.E.; Walsh, C.J. Metabolic cost adaptations during training with a soft exosuit assisting the hip joint. Sci. Rep. 2019, 9, 9779. [Google Scholar] [CrossRef]
- Wu, X.; Zhu, A.; Dang, D.; Shi, L. Novel Lightweight Lower Limb Exoskeleton Design for Single-Motor Sequential Assistance of Knee & Ankle Joints in Real World. IEEE Robot. Autom. Lett. 2024, 9, 2391–2398. [Google Scholar]
- He, Y.; Liu, J.; Li, F.; Cao, W.; Wu, X. Design and analysis of a lightweight lower extremity exoskeleton with novel compliant ankle joints. Technol. Health Care 2022, 30, 881–894. [Google Scholar] [CrossRef] [PubMed]
- Yu, S.; Huang, T.H.; Yang, X.; Jiao, C.; Yang, J.; Chen, Y.; Yi, J.; Su, H. Quasi-direct drive actuation for a lightweight hip exoskeleton with high backdrivability and high bandwidth. IEEE/ASME Trans. Mechatron. 2020, 25, 1794–1802. [Google Scholar] [CrossRef]
- Kermavnar, T.; Power, V.; de Eyto, A.; O’Sullivan, L. Cuff pressure algometry in patients with chronic pain as guidance for circumferential tissue compression for wearable soft exoskeletons: A systematic review. Soft Robot. 2018, 5, 497–511. [Google Scholar] [CrossRef]
- Linnenberg, C.; Weidner, R. Industrial exoskeletons for overhead work: Circumferential pressures on the upper arm caused by the physical human–machine-interface. Appl. Ergon. 2022, 101, 103706. [Google Scholar] [CrossRef] [PubMed]
- Yandell, M.B.; Ziemnicki, D.M.; McDonald, K.A.; Zelik, K.E. Characterizing the comfort limits of forces applied to the shoulders, thigh and shank to inform exosuit design. PLoS ONE 2020, 15, e0228536. [Google Scholar] [CrossRef]
- Kao, P.C.; Lomasney, C.; Gu, Y.; Clark, J.P.; Yanco, H.A. Effects of induced motor fatigue on walking mechanics and energetics. J. Biomech. 2023, 156, 111688. [Google Scholar] [CrossRef]
- Hu, Z.; Ren, L.; Hu, D.; Gao, Y.; Wei, G.; Qian, Z.; Wang, K. Speed-related energy flow and joint function change during human walking. Front. Bioeng. Biotechnol. 2021, 9, 666428. [Google Scholar] [CrossRef]
- Hu, Z.; Ren, L.; Wei, G.; Qian, Z.; Liang, W.; Chen, W.; Lu, X.; Ren, L.; Wang, K. Energy flow and functional behavior of individual muscles at different speeds during human walking. IEEE Trans. Neural Syst. Rehabil. Eng. 2022, 31, 294–303. [Google Scholar] [CrossRef]
- Hu, X.; Ma, Z.; Zhao, F.; Guo, S. Recent Advances in Self-Powered Wearable Flexible Sensors for Human Gaits Analysis. Nanomaterials 2024, 14, 1173. [Google Scholar] [CrossRef]
- Kong, L.; Fang, Z.; Zhang, T.; Zhang, Z.; Pan, Y.; Hao, D.; Chen, J.; Qi, L. A self-powered and self-sensing lower-limb system for smart healthcare. Adv. Energy Mater. 2023, 13, 2301254. [Google Scholar] [CrossRef]
- Xie, L.; Huang, G.; Huang, L.; Cai, S.; Li, X. An unpowered flexible lower limb exoskeleton: Walking assisting and energy harvesting. IEEE/ASME Trans. Mechatron. 2019, 24, 2236–2247. [Google Scholar] [CrossRef]
- Cong, M.; Gao, Y.; Wang, W.; He, L.; Mao, X.; Long, Y.; Dong, W. A broadband hybrid energy harvester with displacement amplification decoupling structure for ultra-low vibration energy harvesting. Energy 2024, 290, 130089. [Google Scholar] [CrossRef]
- Cong, M.; Gao, Y.; Wang, W.; He, L.; Mao, X.; Long, Y.; Dong, W. Asymmetry stagger array structure ultra-wideband vibration harvester integrating magnetically coupled nonlinear effects. Appl. Energy 2024, 356, 122366. [Google Scholar] [CrossRef]
- Cong, M.; Dong, W.; Gao, Y.; Long, Y.; Wang, W.; Dong, H. A New Type of Time-varying Terminal Load Energy Harvester: Design, Simulation, and Experiments. Energy 2024, 313, 133882. [Google Scholar] [CrossRef]
- Wang, D.; Lee, K.M.; Guo, J.; Yang, C. Adaptive knee joint exoskeleton based on biological geometries. IEEE/ASME Trans. Mechatron. 2013, 19, 1268–1278. [Google Scholar] [CrossRef]
- Jabeen, S.; Berry, A.; Geijtenbeek, T.; Harlaar, J.; Vallery, H. Assisting gait with free moments or joint moments on the swing leg. In Proceedings of the 2019 IEEE 16th International Conference on Rehabilitation Robotics (ICORR), Toronto, ON, Canada, 24–28 June 2019; IEEE: Piscataway, NJ, USA, 2019; pp. 1079–1084. [Google Scholar]
- Jabeen, S.; Sterke, B.; Vallery, H.; Lemus, D. Self-induced Gyroscopic Torques in Lower Extremities During Gait: A Pilot Study. In Wearable Robotics: Challenges and Trends, Proceedings of the 5th International Symposium on Wearable Robotics, WeRob2020, and of WearRAcon Europe 2020, Online, 13–16 October 2020; Springer: Cham, Switzerland, 2022; pp. 59–62. [Google Scholar]
- Wojtara, T.; Sasaki, M.; Konosu, H.; Yamashita, M.; Shimoda, S.; Alnajjar, F.; Kimura, H. Artificial balancer—Supporting device for postural reflex. Gait Posture 2012, 35, 316–321. [Google Scholar] [CrossRef] [PubMed]
- Lemus, D.; van Frankenhuyzen, J.; Vallery, H. Design and evaluation of a balance assistance control moment gyroscope. J. Mech. Robot. 2017, 9, 051007. [Google Scholar] [CrossRef]
- Liu, X.; Zhang, X.; Zhang, B.; Zhou, B.; He, Z.; Liu, T. An IMU-based ground reaction force estimation method and its application in walking balance assessment. IEEE Trans. Neural Syst. Rehabil. Eng. 2023, 32, 223–232. [Google Scholar] [CrossRef]
- Liu, X.; Zhou, B.; Zhang, B.; Liu, T. A potential-real-time thigh orientation prediction method based on two shanks-mounted IMUs and its clinical application. IEEE Trans. Autom. Sci. Eng. 2022, 21, 696–705. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).