1. Introduction
Using advanced information and communication technologies to deliver healthcare services remotely, telemedicine is a potential solution to improve access to healthcare and reduce healthcare costs [
1,
2]. In China, B2B teleconsultation is the most used telemedicine service, proving highly effective in mitigating the uneven distribution of high-quality medical resources. Via videoconferencing, primary hospitals gain access to the specialist resources of class-A tertiary hospitals, thereby enhancing the quality of medical services. Having been rolled out across 29 provinces, teleconsultation has benefited a vast number of patients [
3].
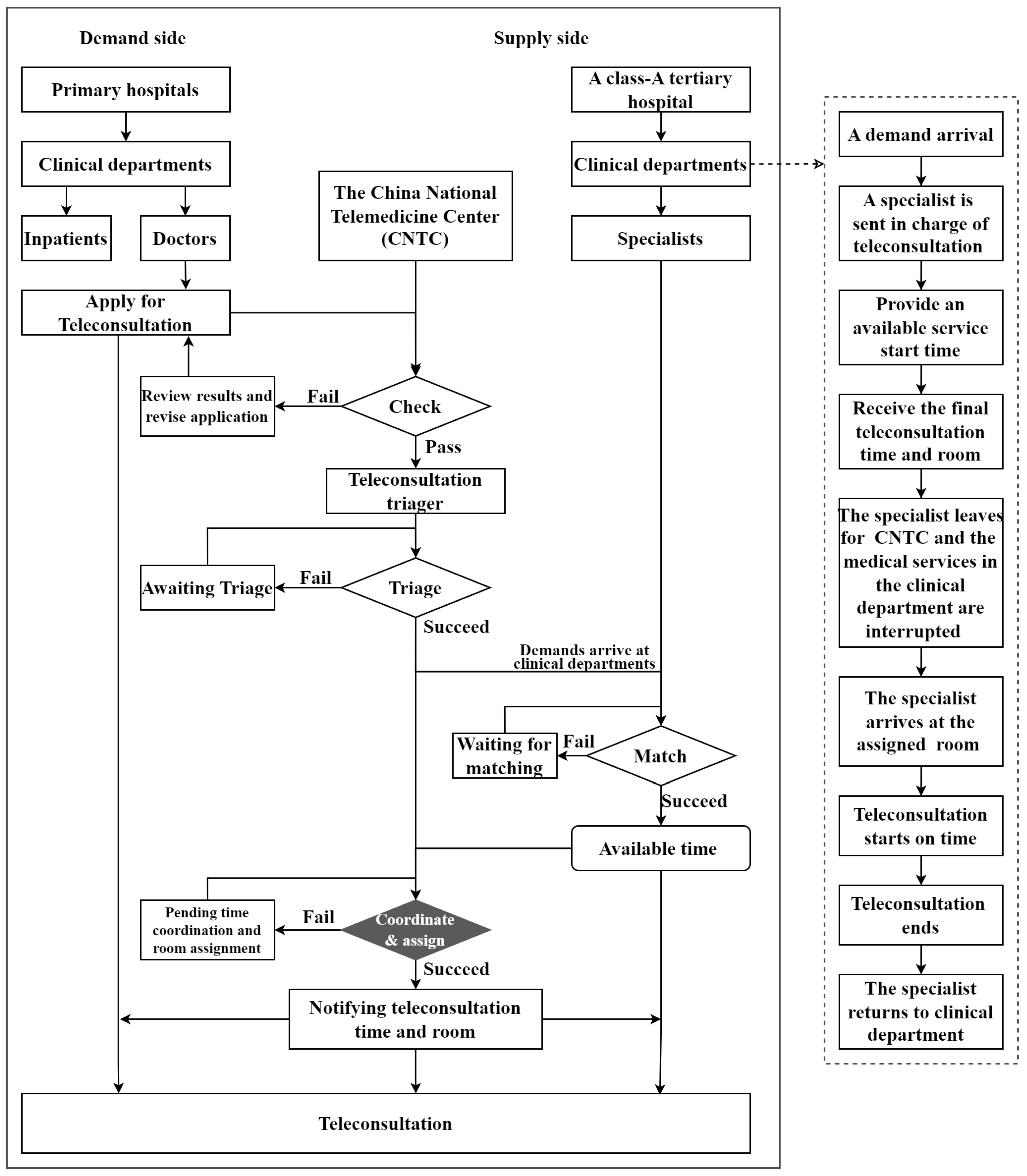
The characteristics of teleconsultation can be summarized as follows: it shares a similar service duration with outpatient services and has comparable room requirements to surgical services. However, it is also distinguished by three notable features: the involvement of four participants, service mobility, and intermittent demand. The four participants include doctors and inpatients in primary hospitals (demand side), and the China National Telemedicine Center (CNTC) and specialists in a class-A tertiary hospital (supply side), as shown in
Figure 1. Service mobility refers to the fact that specialists do not hold fixed office hours or reserve dedicated rooms for teleconsultations. Instead, they move from their clinical departments to CNTC to deliver teleconsultation services, as elaborated in the dashed-line block diagram of
Figure 1. Service mobility stems, on the one hand, from the specific requirements for teleconsultation, including devices, networks, and management, which are met at the CNTC. On the other hand, the lack of specialists dedicated exclusively to teleconsultations can be attributed to intermittent demand and short service durations. Intermittent demands did not cause system congestion issues. The average duration is about eight minutes [
4]. Specialists are only assigned to deliver teleconsultation services when a teleconsultation request is received.
Owing to the characteristic, the operational challenges of teleconsultation are more complex than those of traditional healthcare services. For instance, when modeling the specialist assignment problem, Ji et al. [
5] incorporated three distinct sources of uncertainty, including uncertain service durations and no-show behaviors from both the demand and supply sides. Regarding the allocation and scheduling of teleconsultation resources, clinical departments are integrated and grouped into five medical sections to mitigate the issue of intermittent demand [
6,
7]. In terms of the daily scheduling problem with a single teleconusltation server, Wan et al. [
8] considers the mobility of the specialist doctor and the time anxiety of primary doctors to build an approximate semidefinite programming model to reduce the risk level of overtime and waiting cost. Considering service mobility and demand intermittency, Chen and Li [
9] build a dynamic scheduling model for teleconsultation to optimize its start time to reduce long-term service cost. In the model, the objective includes the number of service times of specialists. Although a smaller number of service times can reduce the service cost, blindly pursuing a smaller number of it can lead to a high risk of overtime [
10].
To avoid long overtime, this study considers the adjustment of service start time to reduce the risk of overtime in teleconsultation. Furthermore, time also needs to be coordinated to assign rooms, seen in the highlighted black filled diamond in
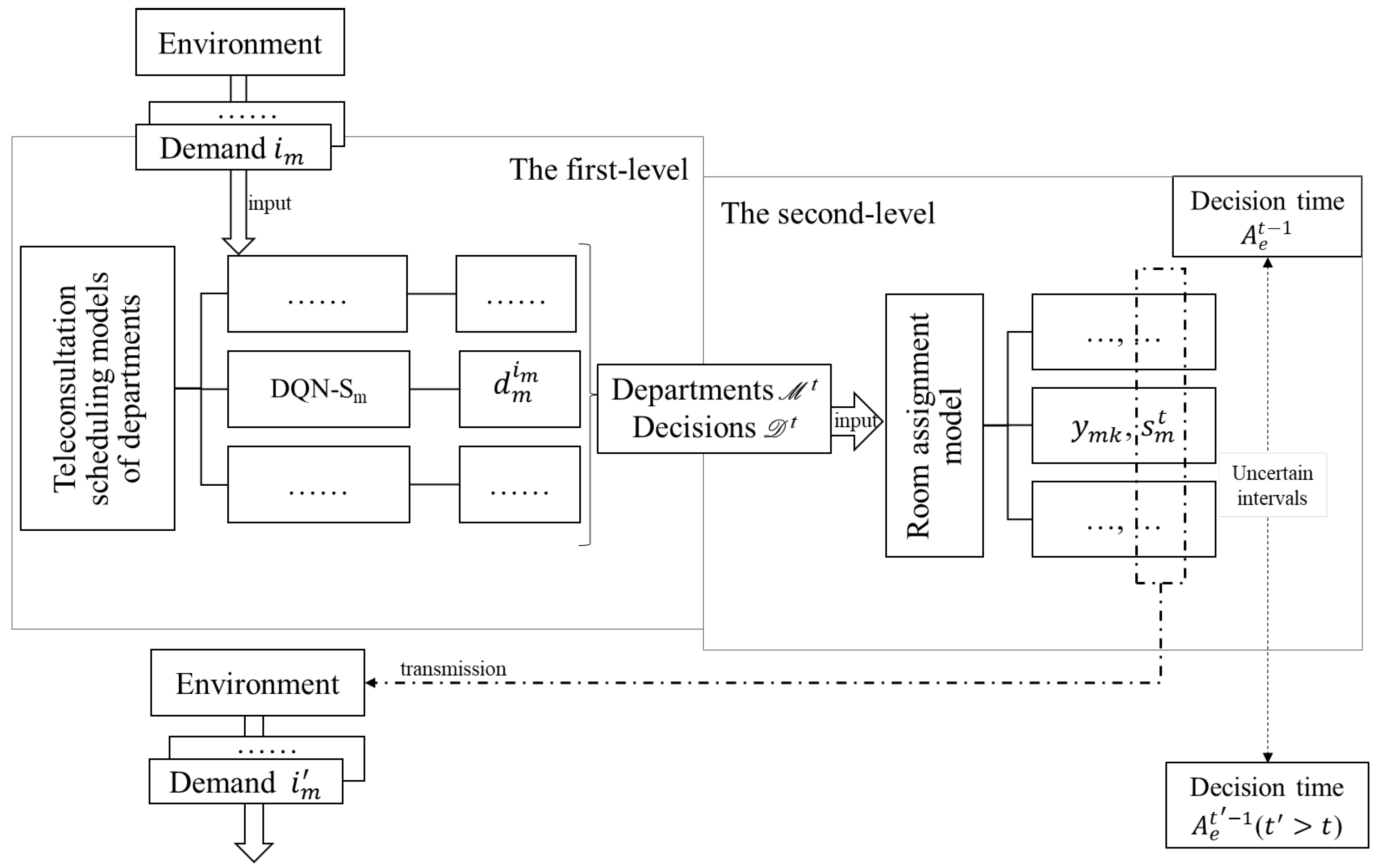
Figure 1. To our best knowledge, these have not been analyzed in the consideration of optimizing service frequency. Frequent teleconsultation services result in numerous round trips for specialists between clinical departments and the CNTC, wasting their time, undermining the quality of on-site medical services, and reducing the efficiency of teleconsultations. This is not conducive to the sustainability of teleconsultation with intermittent demands. Therefore, to fill the gap, optimizing service frequency is designated as a priority objective, with overtime risk and downstream teleconsultation room usage considered as secondary factors in the problem. For this purpose, we build a two-level approach for teleconsultation scheduling optimization. The first level is the dynamic start-time optimization model built by [
9], of which the objective includes reducing the service frequency. Room assignment and start time adjustment models are built based on each output of the first model, resulting in a main dynamic model embedded with multiply branch models. This two-level structure can avoid the decline in model solving efficiency caused by high-dimensional action sets. The dimension of action sets increases severalfold when optimizing service start time and allocating rooms simultaneously. For problem solving, deep reinforcement learning (DRL) and integer programming (IP) solver are combined to form an embedded algorithm. The applied data are actual records including the arrival time for the teleconsultation demand and the arranged start time of the service with a long-term observation of several months. The results demonstrate the effectiveness of the proposed approach and algorithm.
The remainder of this paper is structured as follows.
Section 2 reviews the relevant literature and elaborates on our contributions.
Section 3 and
Section 4 first describe and formulate the research problem, and then introduce the solution approaches.
Section 5 and
Section 6 present the experimental design, results, and discussions. Finally,
Section 7 concludes the paper and outlines directions for future research.
3. Problem Modeling
In constructing the models, this section first provides a brief description of the scheduling problem, followed by an introduction to the models at both the first and second levels.
After the clinical department provides the available service time, CNTC considers the available time of teleconsultation rooms to decide the final service start time and assign the service room. The start time are modeled and optimized in [
9]. Based on these models, this study constructs room assignment models, resulting in a two-level approach. For modeling, the priority of emergency is not considered for departments because emergency teleconsultation services are provided by the emergency department, which is not included in the current research sample. The demands of a department are serviced following the rule of first-come and first-service (FCFS) due to non-emergency.
3.1. The First-Level Model
The first-level model is used to optimize the teleconsultation start time of each clinical department. The notation are defined in
Table 2 and formulations are presented below.
From a data-driven perspective, we aim to optimize the start times of teleconsultations by constructing a general teleconsultation scheduling model based on the empirical cost minimization principle. Specifically, using a dataset collected over an observation period, the model seeks to learn an optimal decision function
that minimizes the value of the service cost function
L. Mathematically, this is expressed as
. In our study,
L specifically consists of demand waiting costs and service provision costs, as detailed in Equation (
1).
The first-level model incorporates five constraints. Constraints (
2) and (
3) calculate the demand waiting time by using an indicator function,
Constraint (
4) defines the feasible ranges of specific parameters.
denotes that the total number of teleconsultations provided is less than or equal to the total number of demands. This is understandable because one teleconsultation is provided for at least one demand.
indicates that the unit service cost of specialists exceeds the unit waiting cost of demands, a reasonable setting given the scarcity and high value of specialist resources.
imposes a non-zero time interval between two consecutive teleconsultations, as formalized in constraint (
5). The model defined by Equations (
1)–(
5) are built for department
m. Since
, there are
M scheduling models in the first level. Each model can be converted into a Markov decision process and then solved by the deep reinforcement algorithm proposed in [
9] to output the optimized start time of the corresponding department.
3.2. The Second-Level Model
The second-level model is a room assignments model. The notation are defined in
Table 3.
The objective function is shown as the Equation (
6). The objective is composed of a two-part cost, i.e., start time adjustment cost and room opening.
subject to:
Constraint (
7) calculates the adjustment degree of each department’s service time between the first level and second level. The degree of deviation is determined by the absolute distance between the two decisions. Constraints (
8) indicate that each department is arranged in one room for one teleconsultation service. Constraints (
9) ensure that services are arranged in open teleconsultation rooms. Constraints (
10) require the time interval between department services to cope with the uncertainty of the duration of services and the possible future demand. In constraints (
10),
represents the size of the time interval. In the case where
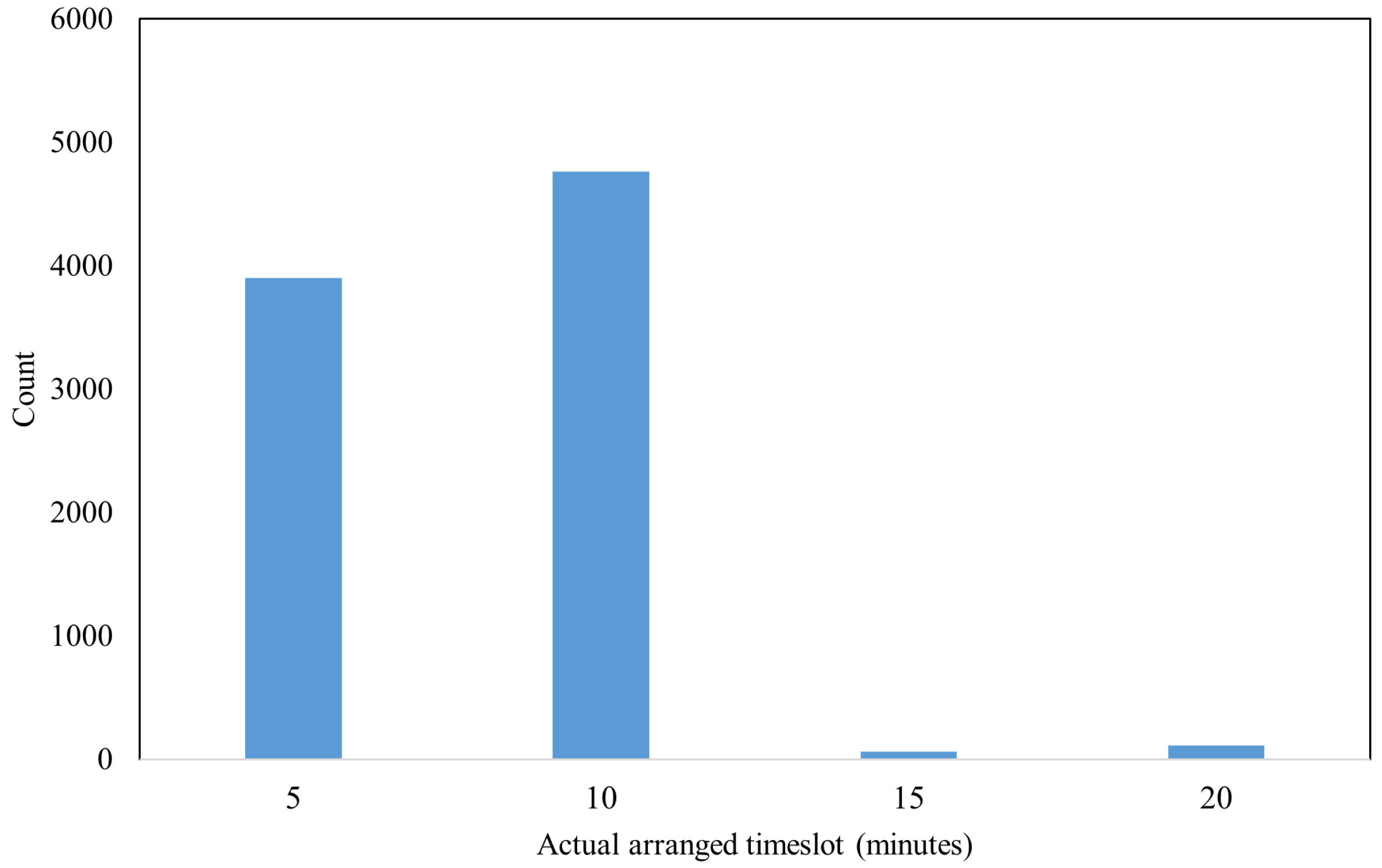
takes ten minutes based on the prevalence in practice (see
Figure A1 in
Appendix A.3), the size of the time interval is determined by
. Also, referring to the actual settings,
can be set to three. Constraint (
11) mitigates the risk of overtime by restricting the expected end time to be before the off-work hour. Constraint (
12) mitigates the risk of overtime by setting the start time to be the on-work hour if the number of waiting demands of departments are larger than or equal to the room expected capacity. These departments will use one room individually.
5. Experimental Results
To validate the proposed model and algorithm, this section conducts teleconsultation scheduling experiments using real-world data and presents a detailed analysis of the results. Specifically,
Section 5.1 and
Section 5.2 elaborate on the data sources and experimental design, while
Section 5.3 showcases the scheduling performance.
5.1. Data
The data utilized in this study are real teleconsultation records, including demand arriving time and service arranged start time provided by the CNTC. A sample of these records is presented in
Table A1 (see
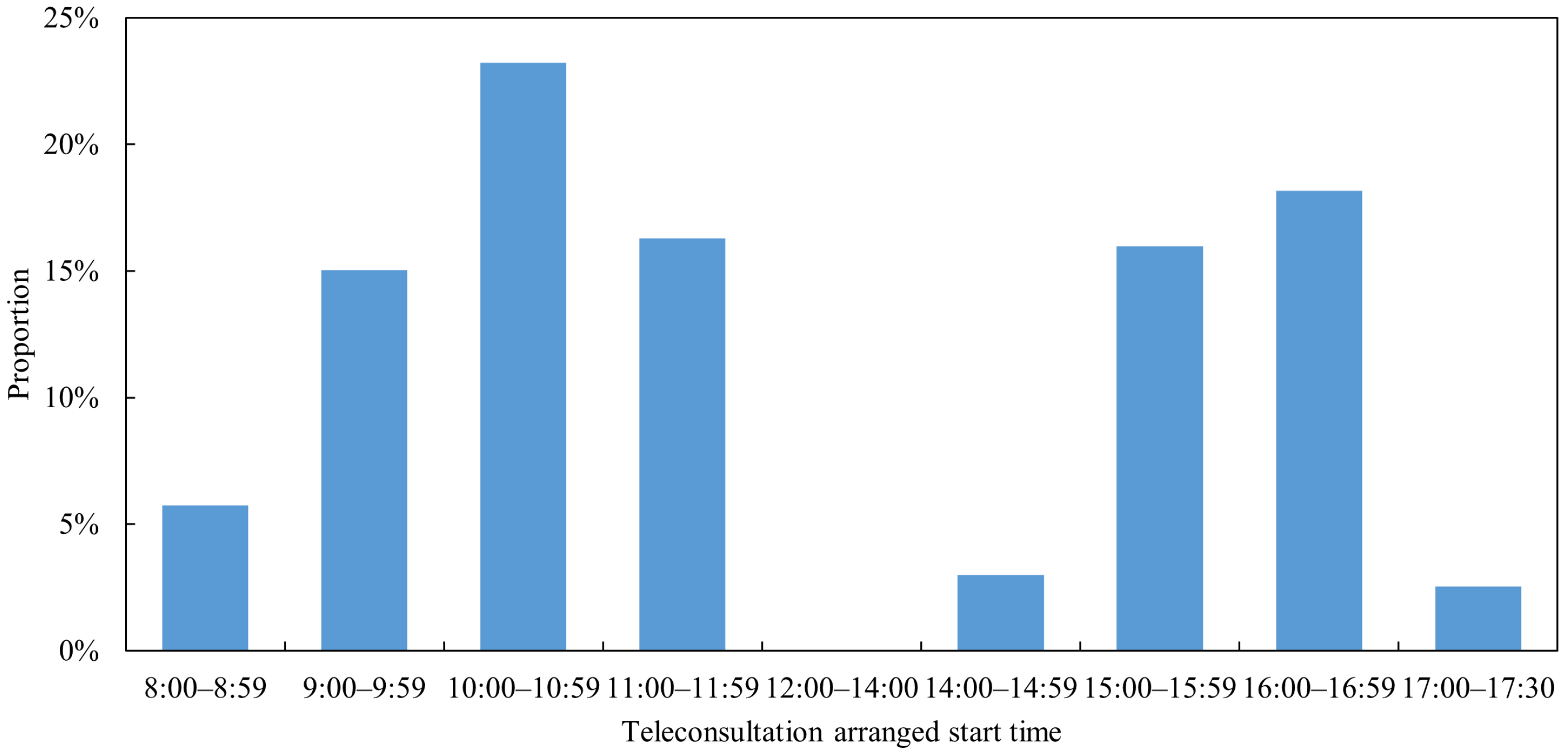
Appendix A.2). Specifically, demand arrival time is automatically recorded by the system upon submission of a teleconsultation application, and its reliability is guaranteed by the stable operation of the system. In contrast, the scheduled service start time for each department is determined by teleconsultation scheduling staff and documented in the system. Its reliability is validated through the actual teleconsultation services provided. Thus, the data employed in this research are reliable. The daily distributions of the data are displayed in
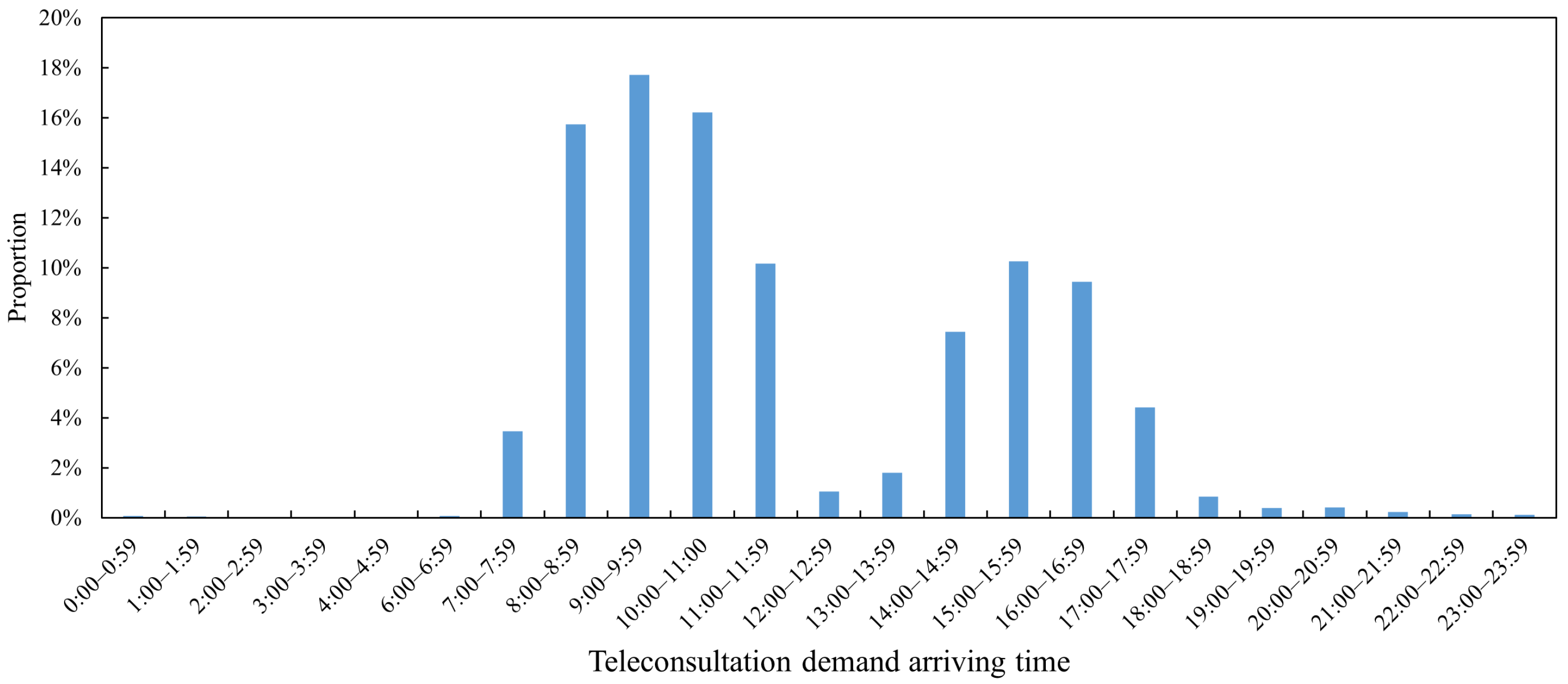
Figure 3 and
Figure 4. From the display, it can be seen that most demand arrival time are within the working time of CNTC, as are all arranged teleconsultation start times. At the CNTC, 76 clinical departments offer teleconsultation services. These departments face intermittent teleconsultation demands [
33], a key feature characterized by multiple periods of zero demand. Unlike conventional demand, intermittent demand is variable not only in terms of demand volume but also in the intervals between successive demand occurrences. The corresponding teleconsultation service exhibits intermittency equal to or greater than that of the demand, with uncertainties regarding both the start time of teleconsultations and the allocation of teleconsultation rooms.
For evaluation purposes, eight departments with relatively high demand volumes were selected as samples.
Table 4 presents the demand sizes of these sampled departments over the observation period. The data, collected from 1 January 2018, spans a 60-week period and is divided into three training sets and three testing sets, as detailed in
Table A2. The training sets are used to pre-train DQN-S, while the testing sets serve to evaluate scheduling performance.
5.2. Experimental Settings
The first-level model of each department is solved by DQN-S established in the previous study [
9]. The DQN-S settings are described below. The input of DQN-S includes the environment variables and the action set. The environmental variables include six date variables and fourteen historical arrival intervals. The six date variables are week; holiday; holiday length; and time information, such as day, hour, and minute. The action set adopts the action set A2 defined in [
9].
Based on the output results of DQN-S, Gurobi is used to solve the second-level room allocation model. In the allocation model, the maximum available number of teleconsultation rooms equals the number of departments that require room allocation. The model sets different cost coefficients to analyze the impact of cost coefficients on scheduling performance. The value of the cost coefficient is as follows: ; . For convenience of representation, the cost coefficient is represented in a simplified form; for example, 1-1 represents , .
To compare scheduling performance, actual schedules and the schedules of DQN-S are used as benchmarks. The four evaluation criteria used are defined in
Table 5. The calculation of room usage distinguishes between the morning and afternoon. The normal service hours in the morning are 8:00∼12:00, and the normal service hours in the afternoon are 14:00∼17:30. When there is a teleconsultation arrangement in a certain teleconsultation room in the morning, the room is used once, and the same applies in the afternoon.
All numerical experiments were coded in Python 3.8 and executed on a PC equipped with an Intel(R) Core(TM) i7-8550U CPU @ 1.80 GHz and 8 GB of RAM. The simulation environment and algorithms were implemented using Python libraries including NumPy, Pandas, DateTime, Math, TensorFlow, and Gurobi.
5.3. Scheduling Performance
5.3.1. The Impact of Cost Coefficients on Scheduling Performance
To investigate the impact of cost coefficients on scheduling performance, the two-level models are built based on three datasets with different cost coefficients for departments 1 (D1) and 2 (D2). The scheduling performance is shown in
Table 6.
From the results in
Table 6, two main findings can be obtained. First, the two-level model can improve teleconsultation scheduling effectively. The four performance criteria are decreased by the two-level models. Compared to the actuality, the DAWT of D1 and D2 are reduced by 39% and 29%, respectively. The NS of D1 and D2 are reduced by 22% and 46%. The OR is reduced to zero. And, the RU is reduced by 31% or 33%. Second, changes in cost coefficients have a relatively small impact on the scheduling performance of two-level models. In
Table 6, DAWT, NS, and OR of the five models have 0.01 differences in different cost coefficients for D1, and no difference for D2. The RU of two-level models under different cost coefficients are 28 or 29. When the cost of changing start time increases from 1 to 5 and 10, the RU of two-level models show an increasing trend.
To enhance the evaluation, scheduling experiments of D1 and D2 are also conducted on dataset-2 and dataset-3. The results are shown in
Table A3 and
Table A4 in
Appendix A.2, in which findings similar to those in
Table 6 can be obtained. In addition, it can be observed from
Table A4 that as the cost of opening the room increases, RU decreases. Despite this, changes in the cost coefficient have a relatively small impact on the entire scheduling performance of the two-level model. Therefore, the cost coefficients of 1-1 and 1-5 are used for subsequent experiments on dataset-1.
5.3.2. The Impact of Increasing the Number of Departments on Scheduling Performance
In this section, the number of departments is increased in experiments to analyze the scheduling performance. From the results presented in
Table 7, the two-level models maintain their superiority when the number of departments increases to four. Compared to the actuality, DAWT is lowered by 5∼39%, NS by 22∼48%, and RU by 36% and 37%. The total amount of OR declines from 8.58 h to 1.33 h.
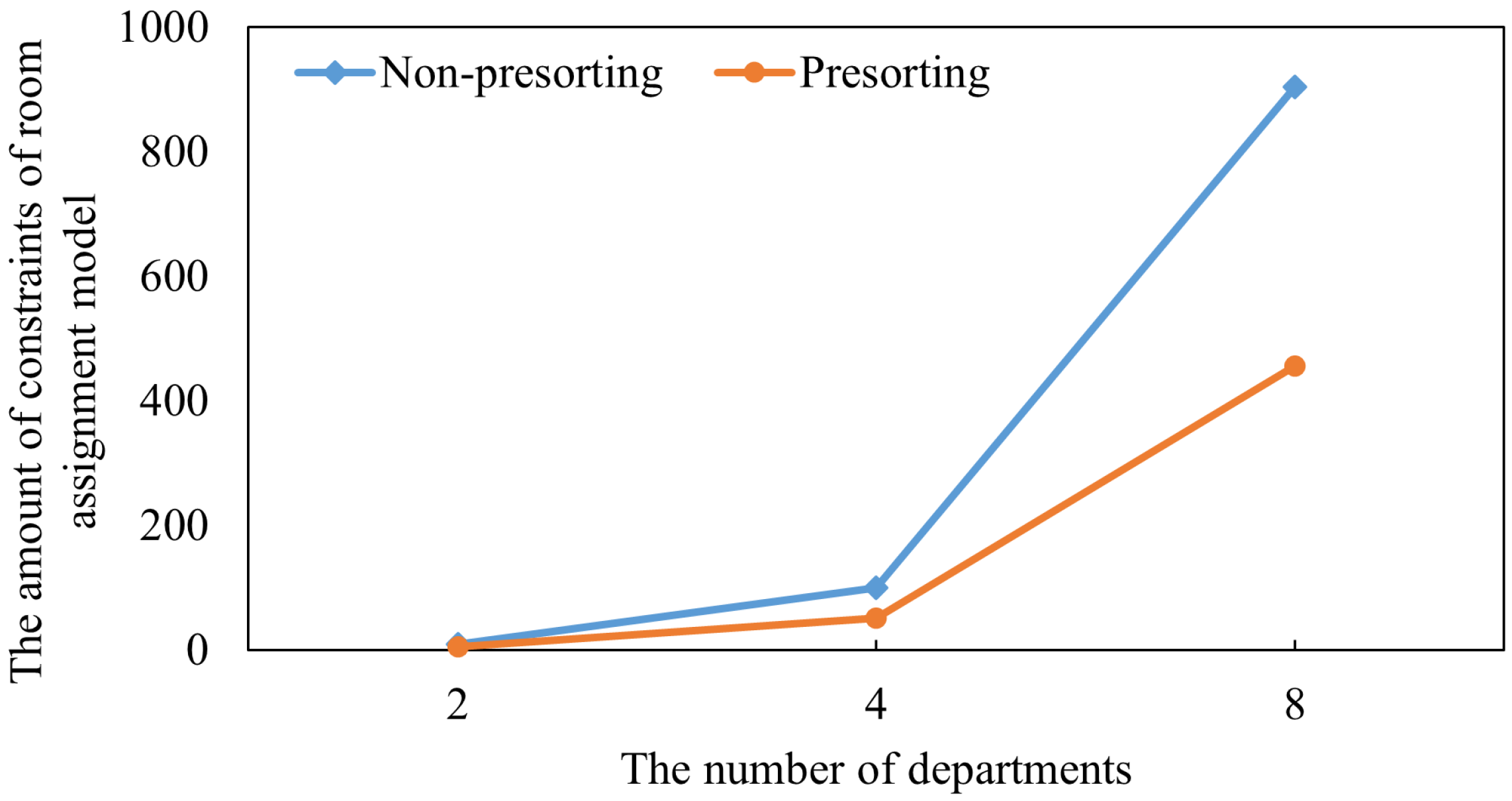
5.3.3. The Impact of Interval Constraint Presorting Mechanism on Scheduling Performance
In this section, the number of departments is increased to eight analyze the impact of the interval constraint presorting mechanism on scheduling performance. When the number of departments increased to eight, the results in
Table 8 not only demonstrate the superior scheduling performance of the two-level model but also prove the effectiveness of the interval constraint presorting mechanism on improving the scheduling. Whether the constraint (
10) is presorted or not has no significant impact on the scheduling performance of the two-level model in terms of DAWT, NS, and OR. An important difference is the reduced RU under interval constraint presorting. RU is reduced from 90 and 79 to 78 and 67, respectively. This reduction is explained in
Section 6.
7. Conclusions
In this paper, teleconsultation scheduling is further optimized by prioritizing the optimization of service frequency and incorporating downstream room utilization and overtime risk as considerations. For this purpose, a two-level approach is proposed based on a data-driven dynamic teleconsultation scheduling model. Based on the optimized start time in the first-level models to optimize service frequency, second-level models are built to allocate teleconsultation room and adjust the start time to reduce overtime risk. The frequency is optimized for service sustainability due to demand intermittency. The generally applicable environment of this study has the characteristic of intermittent demand and the target of control event frequency. For other analogous environments or problems, such as the purchase of spare parts, the proposed methods can be used with appropriate adjustments.
To solve the two-level model, an embedding DRL and IP solver method is constructed. And, to improve the solutions, an interval constraint presorting mechanism is developed. Based on actual teleconsultation data, numerical experiments verify the effectiveness of the proposed scheduling model, the solving method, and the presorting mechanism. There are three main conclusions.
In different experimental settings, two-level models can maintain their effectiveness in improving teleconsultation scheduling performance. When the cost coefficients are changed and the number of departments is increased, two-level models can outperform reality. The DAWT can be lowered by 5.86∼57.49% and NS by 14.29∼52.38%.
The two-level model further improves teleconsultation scheduling by reducing OR. Compared to reality, DQN-S can significantly reduce DAWT and NS for a single department but increase OR. Compared to DQN-S, the two-level model can significantly reduce OR by 0.17∼4.67 h, without losing the outperformance in DAWT and NS.
The two-level model also improves teleconsultation scheduling by reducing RU by 22.09∼37.18%. There are two effective approaches to lowering RU: one is increasing the opening cost in the two-level model, and the other is implementing the interval constraint presorting mechanism. When interval constraints are presorted, the number of department combinations for sharing teleconsultation rooms can be increased by 5 and 10. In the results of the two-level models, there are eight cases where three departments share a room.
While this study has made progress in teleconsultation scheduling, it has certain limitations that warrant further refinement in future research. From the perspective of modeling, the proposed teleconsultation scheduling model does not consider the uncertainties of service duration and no-show behavior, due to data limitation. This work can be extended by addressing such uncertainties either through theoretical simulation analysis or the collection of additional supporting data. Furthermore, incorporating emergency priority represents a valuable direction for extension. From the perspective of model solving, this study solves the first-level model based on a basic DRL algorithm. There are many other DRL algorithms and techniques that can be tested in future studies.