Understanding the Potential for Pharmacy Expertise in Palliative Care: The Value of Stakeholder Engagement in a Theoretically Driven Mapping Process for Research
Abstract
1. Introduction
2. Stakeholder Engagement
3. Themes
3.1. The Decision to Prescribe
3.2. The Act of Prescribing
3.3. Monitoring and Supply of Medications
3.4. Use (Administration)
3.5. Stopping and Disposal
3.6. Contextual Issues
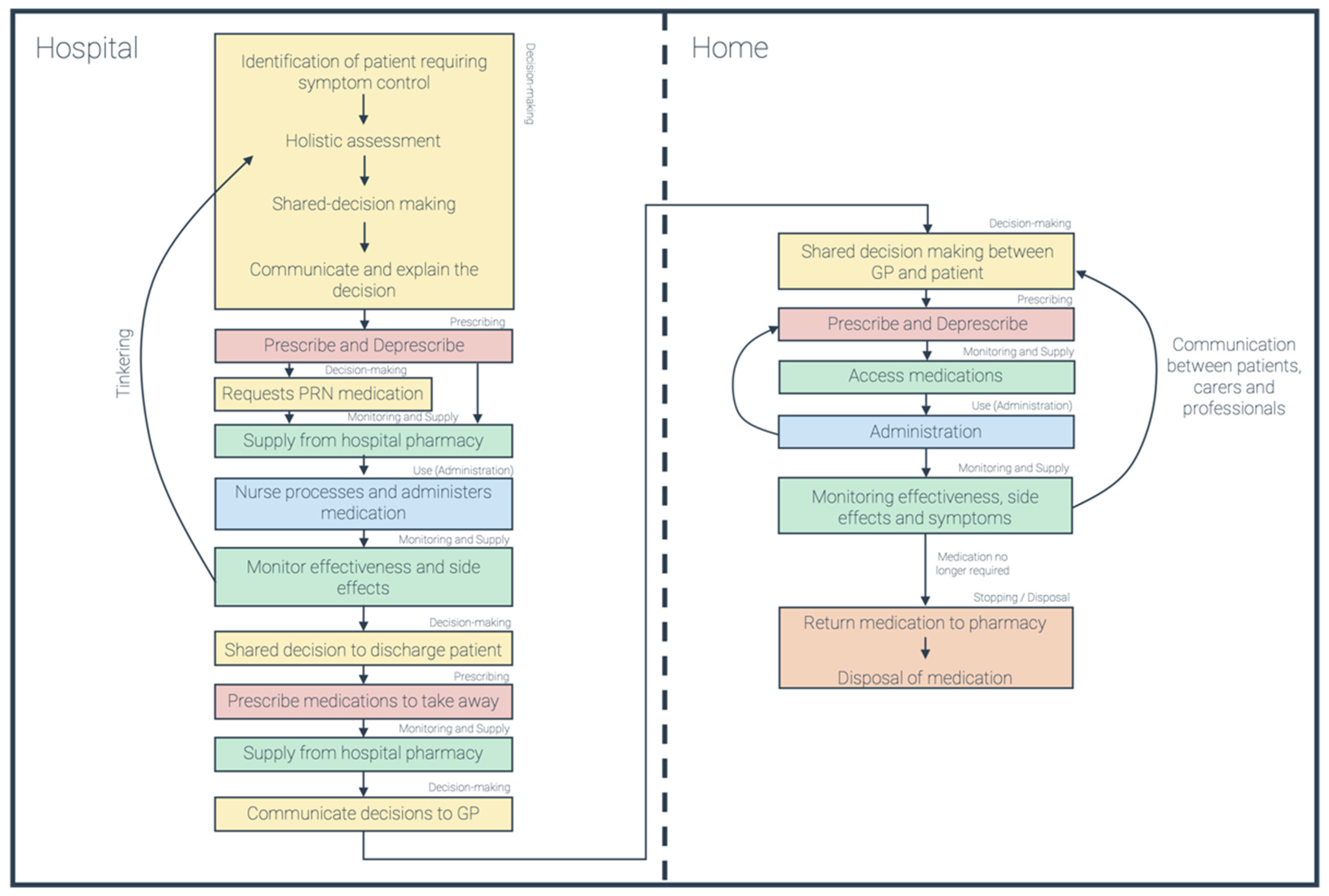
3.7. Visual Intended Medicines Process
4. Concluding Remarks
4.1. Implications for Our Own and Others’ Research
4.2. Implications for Pharmacists and Commissioners of Pharmacy Services
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Donaldson, L.J.; Kelley, E.T.; Dhingra-Kumar, N.; Kieny, M.P.; Sheikh, A. Medication without Harm: WHO’s Third Global Patient Safety Challenge. Lancet 2017, 389, 1680–1681. [Google Scholar] [CrossRef]
- Lewis, P.J.; Dornan, T.; Taylor, D.; Tully, M.P.; Wass, V.; Ashcroft, D.M. Prevalence, Incidence and Nature of Prescribing Errors in Hospital Inpatients. Drug Saf. 2009, 32, 379–389. [Google Scholar] [CrossRef] [PubMed]
- Shaheen, P.E.; LeGrand, S.B.; Walsh, D.; Estfan, B.; Davis, M.P.; Lagman, R.L.; Riaz, M.; Cheema, B. Errors in Opioid Prescribing: A Prospective Survey in Cancer Pain. J. Pain Symptom Manag. 2010, 39, 702–711. [Google Scholar] [CrossRef]
- Nevin, M.; Hynes, G.; Smith, V. Healthcare Providers’ Views and Experiences of Non-Specialist Palliative Care in Hospitals: A Qualitative Systematic Review and Thematic Synthesis. Palliat. Med. 2020, 34, 605–618. [Google Scholar] [CrossRef]
- Smith, F. Patient Safety and Patient Error: The Carer’s Perspective. Lancet 2007, 369, 823. [Google Scholar] [CrossRef]
- Payne, S.; Smith, P.; Dean, S. Identifying the Concerns of Informal Carers in Palliative Care. Palliat. Med. 1999, 13, 37–44. [Google Scholar] [CrossRef]
- Yardley, I.; Yardley, S.; Williams, H.; Carson-Stevens, A.; Donaldson, L.J. Patient Safety in Palliative Care: A Mixed-Methods Study of Reports to a National Database of Serious Incidents. Palliat. Med. 2018, 32, 1353–1362. [Google Scholar] [CrossRef]
- O’Connor, M.; Pugh, J.; Jiwa, M.; Hughes, J.; Fisher, C. The Palliative Care Interdisciplinary Team: Where Is the Community Pharmacist? J. Palliat. Med. 2011, 14, 7–11. [Google Scholar] [CrossRef]
- Wilson, E. Preface: The Role of Pharmacists in Palliative and End of Life Care. Pharmacy 2021, 9, 139. [Google Scholar] [CrossRef]
- Wilson, E.; Caswell, G.; Latif, A.; Anderson, C.; Faull, C.; Pollock, K. An Exploration of the Experiences of Professionals Supporting Patients Approaching the End of Life in Medicines Management at Home. A Qualitative Study. BMC Palliat. Care 2020, 19, 1–10. [Google Scholar] [CrossRef]
- Latif, A.; Faull, C.; Wilson, E.; Caswell, G.; Ali, A. Managing Medicines for Patients with Palliative Care Needs Being Cared for at Home: Insights for Community Pharmacy Professionals. Pharm. J. 2020. Available online: https://pharmaceutical-journal.com/article/ld/caring-for-palliative-care-patients-at-home-medicines-management-principles-and-considerations (accessed on 25 November 2021). [CrossRef]
- Krzyzaniak, N.; Pawłowska, I.; Bajorek, B. An Overview of Pharmacist Roles in Palliative Care: A Worldwide Comparison. Med. Paliat. Prakt. 2016, 10, 160–173. [Google Scholar]
- Savage, I.; Blenkinsopp, A.; Closs, S.J.; Bennett, M.I. “Like Doing a Jigsaw with Half the Parts Missing”: Community Pharmacists and the Management of Cancer Pain in the Community. Int. J. Pharm. Pract. 2013, 21, 151–160. [Google Scholar] [CrossRef]
- Kiesewetter, I.; Schulz, C.; Bausewein, C.; Fountain, R.; Schmitz, A. Patients’ Perception of Types of Errors in Palliative Care—Results from a Qualitative Interview Study. BMC Palliat. Care 2016, 15, 75. [Google Scholar] [CrossRef]
- Royal Pharmaceutical Society; Royal College of General Practitioners. Joint Policy Statement on General Practice Based Pharmacists; Royal Pharmaceutical Society: London, UK, 2015. [Google Scholar]
- National Institute for Health and Care Excellence End of Life Care for Adults (QS13). Available online: https://www.nice.org.uk/guidance/qs13 (accessed on 16 August 2021).
- NHS England. Specialist Level Palliative Care: Information for Commissioners; NHS England: Leeds, UK, 2016.
- Herndon, C.M.; Nee, D.; Atayee, R.S.; Craig, D.S.; Lehn, J.; Moore, P.S.; Nesbit, S.A.; Ray, J.B.; Scullion, B.F.; Wahler, R.G.; et al. ASHP Guidelines on the Pharmacist’s Role in Palliative and Hospice Care. Am. J. Health Pharm. 2016, 73, 1351–1367. [Google Scholar] [CrossRef]
- Abuzour, A.S.; Lewis, P.J.; Tully, M.P. Practice Makes Perfect: A Systematic Review of the Expertise Development of Pharmacist and Nurse Independent Prescribers in the United Kingdom. Res. Soc. Adm. Pharm. 2018, 14, 6–17. [Google Scholar] [CrossRef]
- Hill, R.R. Clinical Pharmacy Services in a Home-Based Palliative Care Program. Am. J. Health Pharm. 2007, 64, 806–810. [Google Scholar] [CrossRef]
- Dispennette, R.; Hall, L.A.; Elliott, D.P. Activities of Palliative Care and Pain Management Clinical Pharmacists. Am. J. Health Pharm. 2015, 72, 999–1000. [Google Scholar] [CrossRef]
- Myotoku, M.; Murayama, Y.; Nakanishi, A.; Hashimoto, N.; Koyama, F.; Irishio, K.; Kawaguchi, S.; Yamaguchi, S.; Ikeda, K.; Hirotani, Y. Assessment of Palliative Care Team Activities—Survey of Medications Prescribed Immediately before and at the Beginning of Opioid Usage. Yakugaku Zasshi 2008, 128, 299–304. [Google Scholar] [CrossRef][Green Version]
- Tuffaha, H.W.; Koopmans, S.M. Development and Implementation of a Method for Characterizing Clinical Pharmacy Interventions and Medication Use in a Cancer Center. J. Oncol. Pharm. Pract. 2012, 18, 180–185. [Google Scholar] [CrossRef]
- Wilson, S.; Wahler, R.; Brown, J.; Doloresco, F.; Monte, S.V. Impact of Pharmacist Intervention on Clinical Outcomes in the Palliative Care Setting. Am. J. Hosp. Palliat. Med. 2011, 28, 316–320. [Google Scholar] [CrossRef]
- Lee, J.; McPherson, M.L. Outcomes of Recommendations by Hospice Pharmacists. Am. J. Health Pharm. 2006, 63, 2235–2239. [Google Scholar] [CrossRef] [PubMed]
- Kajamaa, A.; Mattick, K.; Parker, H.; Hilli, A.; Rees, C. Trainee Doctors’ Experiences of Common Problems in the Antibiotic Prescribing Process: An Activity Theory Analysis of Narrative Data from UK Hospitals. BMJ Open 2019, 9, e028733. [Google Scholar] [CrossRef]
- Engeström, Y.; Davydov, V.; Toulmin, S.; Lektorsky, V.; Tolman, C.; Cole, M.; Eskola, A.; Häyrynen, Y.-P.; Tobach, E.; Colucci, F. Theoretical Issues. In Perspectives on Activity Theory; Engeström, Y., Miettinen, R., Punämaki, R.-L., Eds.; Cambridge University Press: Cambridge, UK, 1999; pp. 1–146. ISBN 9780511812774. [Google Scholar]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping Studies: Advancing the Methodology. Implement. Sci. 2010, 5, 1–9. [Google Scholar] [CrossRef]
- The Joanna Briggs Institute. The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews; The Joanna Briggs Institute: Adelaide, Australia, 2015; pp. 1–24. [Google Scholar]
- Arksey, H.; O’Malley, L. Scoping Studies: Towards a Methodological Framework. Int. J. Soc. Res. Methodol. Theory Pract. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Hagemann, V.; Bausewein, C.; Rémi, C. Off-Label-Prescriptions in Daily Clinical Practice—A Cross-Sectional National Survey of Palliative Medicine Physicians. Prog. Palliat. Care 2019, 27, 154–159. [Google Scholar] [CrossRef]
- Vivat, B.; Bemand-Qureshi, L.; Harrington, J.; Davis, S.; Stone, P. Palliative Care Specialists in Hospice and Hospital/Community Teams Predominantly Use Low Doses of Sedative Medication at the End of Life for Patient Comfort Rather than Sedation: Findings from Focus Groups and Patient Records for I-CAN-CARE. Palliat. Med. 2019, 33, 578–588. [Google Scholar] [CrossRef]
- Faull, C.; Windridge, K.; Ockleford, E.; Hudson, M. Anticipatory Prescribing in Terminal Care at Home: What Challenges Do Community Health Professionals Encounter? BMJ Support. Palliat. Care 2013, 3, 91–97. [Google Scholar] [CrossRef]
- Virdun, C.; Luckett, T.; Davidson, P.M.; Phillips, J. Dying in the Hospital Setting: A Systematic Review of Quantitative Studies Identifying the Elements of End-of-Life Care That Patients and Their Families Rank as Being Most Important. Palliat. Med. 2015, 29, 774–796. [Google Scholar] [CrossRef]
- Roodbeen, R.; Vreke, A.; Boland, G.; Rademakers, J.; van den Muijsenbergh, M.; Noordman, J.; van Dulmen, S. Communication and Shared Decision-Making with Patients with Limited Health Literacy; Helpful Strategies, Barriers and Suggestions for Improvement Reported by Hospital-Based Palliative Care Providers. PLoS ONE 2020, 15, e0234926. [Google Scholar] [CrossRef]
- Jansen, J.; van Weert, J.C.M.; de Groot, J.; van Dulmen, S.; Heeren, T.J.; Bensing, J.M. Emotional and Informational Patient Cues: The Impact of Nurses’ Responses on Recall. Patient Educ. Couns. 2010, 79, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Mori, M.; Matsunuma, R.; Suzuki, K.; Matsuda, Y.; Watanabe, H.; Yamaguchi, T. Palliative Care Physicians’ Practice in the Titration of Parenteral Opioids for Dyspnea in Terminally Ill Cancer Patients: A Nationwide Survey. J. Pain Symptom Manag. 2019, 58, e2–e5. [Google Scholar] [CrossRef] [PubMed]
- Klepstad, P.; Kaasa, S.; Borchgrevink, P.C. Starting Step III Opioids for Moderate to Severe Pain in Cancer Patients: Dose Titration: A Systematic Review. Palliat. Med. 2011, 25, 424–430. [Google Scholar] [CrossRef]
- Masman, A.D.; van Dijk, M.; Tibboel, D.; Baar, F.P.M.; Mathôt, R.A.A. Medication Use during End-of-Life Care in a Palliative Care Centre. Int. J. Clin. Pharm. 2015, 37, 767–775. [Google Scholar] [CrossRef]
- Lawton, S.; Denholm, M.; Macaulay, L.; Grant, E.; Davie, A. Timely Symptom Management at End of Life Using ‘Just in Case’ Boxes. Br. J. Commun. Nurs. 2012, 17, 182–190. [Google Scholar] [CrossRef]
- Bowers, B.; Barclay, S.S.; Pollock, K.; Barclay, S. GPs’ Decisions about Prescribing End-of-Life Anticipatory Medications: A Qualitative Study. Br. J. Gen. Pract. 2020, 70, e731–e739. [Google Scholar] [CrossRef]
- Bowers, B.; Redsell, S.A. A Qualitative Study of Community Nurses’ Decision-Making around the Anticipatory Prescribing of End-of-Life Medications. J. Adv. Nurs. 2017, 73, 2385–2394. [Google Scholar] [CrossRef] [PubMed]
- Wilson, E.; Seymour, J.; Seale, C. Anticipatory Prescribing for End of Life Care: A Survey of Community Nurses in England. Prim. Health Care 2016, 26, 22–27. [Google Scholar] [CrossRef]
- Wilson, E.; Morbey, H.; Brown, J.; Payne, S.; Seale, C.; Seymour, J. Administering Anticipatory Medications in End-of-Life Care: A Qualitative Study of Nursing Practice in the Community and in Nursing Homes. Palliat. Med. 2015, 29, 60–70. [Google Scholar] [CrossRef]
- Bowers, B.; Ryan, R.; Kuhn, I.; Barclay, S. Anticipatory Prescribing of Injectable Medications for Adults at the End of Life in the Community: A Systematic Literature Review and Narrative Synthesis. Palliat. Med. 2019, 33, 160–177. [Google Scholar] [CrossRef]
- Antunes, B.; Bowers, B.; Winterburn, I.; Kelly, M.P.; Brodrick, R.; Pollock, K.; Majumder, M.; Spathis, A.; Lawrie, I.; George, R.; et al. Anticipatory Prescribing in Community End-of-Life Care in the UK and Ireland during the COVID-19 Pandemic: Online Survey. BMJ Support. Palliat. Care 2020, 10, 343–349. [Google Scholar] [CrossRef]
- Wilson, E.; Seymour, J. The Importance of Interdisciplinary Communication in the Process of Anticipatory Prescribing. Int. J. Palliat. Nurs. 2017, 23, 129–135. [Google Scholar] [CrossRef]
- Taubert, M.; Nelson, A. Out-of-Hours GPs and Palliative Care-a Qualitative Study Exploring Information Exchange and Communication Issues. BMC Palliat. Care 2010, 9, 18. [Google Scholar] [CrossRef]
- Thompson, J. Deprescribing in Palliative Care. Clin. Med. 2019, 19, 311–314. [Google Scholar] [CrossRef]
- Fede, A.; Miranda, M.; Antonangelo, D.; Trevizan, L.; Schaffhausser, H.; Hamermesz, B.; Zimmermann, C.; Del Giglio, A.; Riechelmann, R.P. Use of Unnecessary Medications by Patients with Advanced Cancer: Cross-Sectional Survey. Support. Care Cancer 2011, 19, 1313–1318. [Google Scholar] [CrossRef]
- Miller, E.J.; Morgan, J.D.; Blenkinsopp, A. How Timely Is Access to Palliative Care Medicines in the Community? Amixed Methods Study in a UK City. BMJ Open 2019, 9, e029016. [Google Scholar] [CrossRef] [PubMed]
- Anderson, B.A.; Kralik, D. Palliative Care at Home: Carers and Medication Management. Palliat. Support. Care 2008, 6, 349–356. [Google Scholar] [CrossRef]
- Corless, I.B.; Nicholas, P.K.; Davis, S.M.; Dolan, S.A.; McGibbon, C.A. Symptom Status, Medication Adherence, and Quality of Life in HIV Disease. J. Hosp. Palliat. Nurs. 2005, 7, 129–138. [Google Scholar] [CrossRef]
- Sanders, S.; Herr, K.A.; Fine, P.G.; Fiala, C.; Tang, X.; Forcucci, C. An Examination of Adherence to Pain Medication Plans in Older Cancer Patients in Hospice Care. J. Pain Symptom Manag. 2013, 45, 43–55. [Google Scholar] [CrossRef]
- Zeppetella, G. How Do Terminally Ill Patients at Home Take Their Medication? Palliat. Med. 1999, 13, 469–475. [Google Scholar] [CrossRef]
- Dayer, L.; Harrington, S.; Martin, B. A Palliative Care Clinic’s Experience with Medication Adherence to Neuropathic Pain Medications. J. Palliat. Med. 2018, 21, 245–248. [Google Scholar] [CrossRef] [PubMed]
- Den Herder-Van Der Eerden, M.; Hasselaar, J.; Payne, S.; Varey, S.; Schwabe, S.; Radbruch, L.; van Beek, K.; Menten, J.; Busa, C.; Csikos, A.; et al. How Continuity of Care Is Experienced within the Context of Integrated Palliative Care: A Qualitative Study with Patients and Family Caregivers in Five European Countries. Palliat. Med. 2017, 31, 946–955. [Google Scholar] [CrossRef]
- Walshe, C.; Payne, S.; Luker, K. Observing District Nurses Roles in Palliative Care: An Understanding of Aims and Actions. BMJ Support. Palliat. Care 2012, 2, A2–A3. [Google Scholar] [CrossRef]
- Walshe, C.; Luker, K.A. District Nurses’ Role in Palliative Care Provision: A Realist Review. Int. J. Nurs. Stud. 2010, 47, 1167–1183. [Google Scholar] [CrossRef] [PubMed]
- Walker, K.A.; Scarpaci, L.; McPherson, M.L. Fifty Reasons to Love Your Palliative Care Pharmacist. Am. J. Hosp. Palliat. Med. 2010, 27, 511–513. [Google Scholar] [CrossRef] [PubMed]
- Royal Pharmaceutical Society Wales Cumru. Palliative & End of Life Care: Pharmacy’s Contribution to Improved Patient Care; Royal Pharmaceutical Society: Wales, UK, 2018. [Google Scholar]
- Austwick, E.A.; Brown, L.C.; Goodyear, K.H.; Brooks, D.J. Pharmacist’s Input into a Palliative Care Clinic. Pharm. J. 2002, 268, 404–406. [Google Scholar]
| Stakeholder | Background | Total |
|---|---|---|
| 1 | Non-clinical researcher | 3 |
| 2 | Non-clinical researcher | |
| 3 | Non-clinical researcher | |
| 4 | General practitioner | 3 |
| 5 | General practitioner | |
| 6 | General practitioner (with specialist palliative care interest) | |
| 7 | carer | 7 |
| 8 | carer | |
| 9 | carer | |
| 10 | carer | |
| 11 | carer | |
| 12 | carer | |
| 13 | carer | |
| 14 | Pharmacist (non-specialist) | 4 |
| 15 | Pharmacist (non-specialist) | |
| 16 | Pharmacist (non-specialist) | |
| 17 | Pharmacist (specialist) | |
| 18 | Specialist palliative care professional (nurse) | 4 |
| 19 | Specialist palliative care professional (physician) | |
| 20 | Specialist palliative care professional (physician) | |
| 21 | Specialist palliative care professional (physician) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Elyan, J.; Francis, S.-A.; Yardley, S. Understanding the Potential for Pharmacy Expertise in Palliative Care: The Value of Stakeholder Engagement in a Theoretically Driven Mapping Process for Research. Pharmacy 2021, 9, 192. https://doi.org/10.3390/pharmacy9040192
Elyan J, Francis S-A, Yardley S. Understanding the Potential for Pharmacy Expertise in Palliative Care: The Value of Stakeholder Engagement in a Theoretically Driven Mapping Process for Research. Pharmacy. 2021; 9(4):192. https://doi.org/10.3390/pharmacy9040192
Chicago/Turabian StyleElyan, Joseph, Sally-Anne Francis, and Sarah Yardley. 2021. "Understanding the Potential for Pharmacy Expertise in Palliative Care: The Value of Stakeholder Engagement in a Theoretically Driven Mapping Process for Research" Pharmacy 9, no. 4: 192. https://doi.org/10.3390/pharmacy9040192
APA StyleElyan, J., Francis, S.-A., & Yardley, S. (2021). Understanding the Potential for Pharmacy Expertise in Palliative Care: The Value of Stakeholder Engagement in a Theoretically Driven Mapping Process for Research. Pharmacy, 9(4), 192. https://doi.org/10.3390/pharmacy9040192






