Telepharmacy during COVID-19: A Scoping Review
Abstract
:1. Introduction
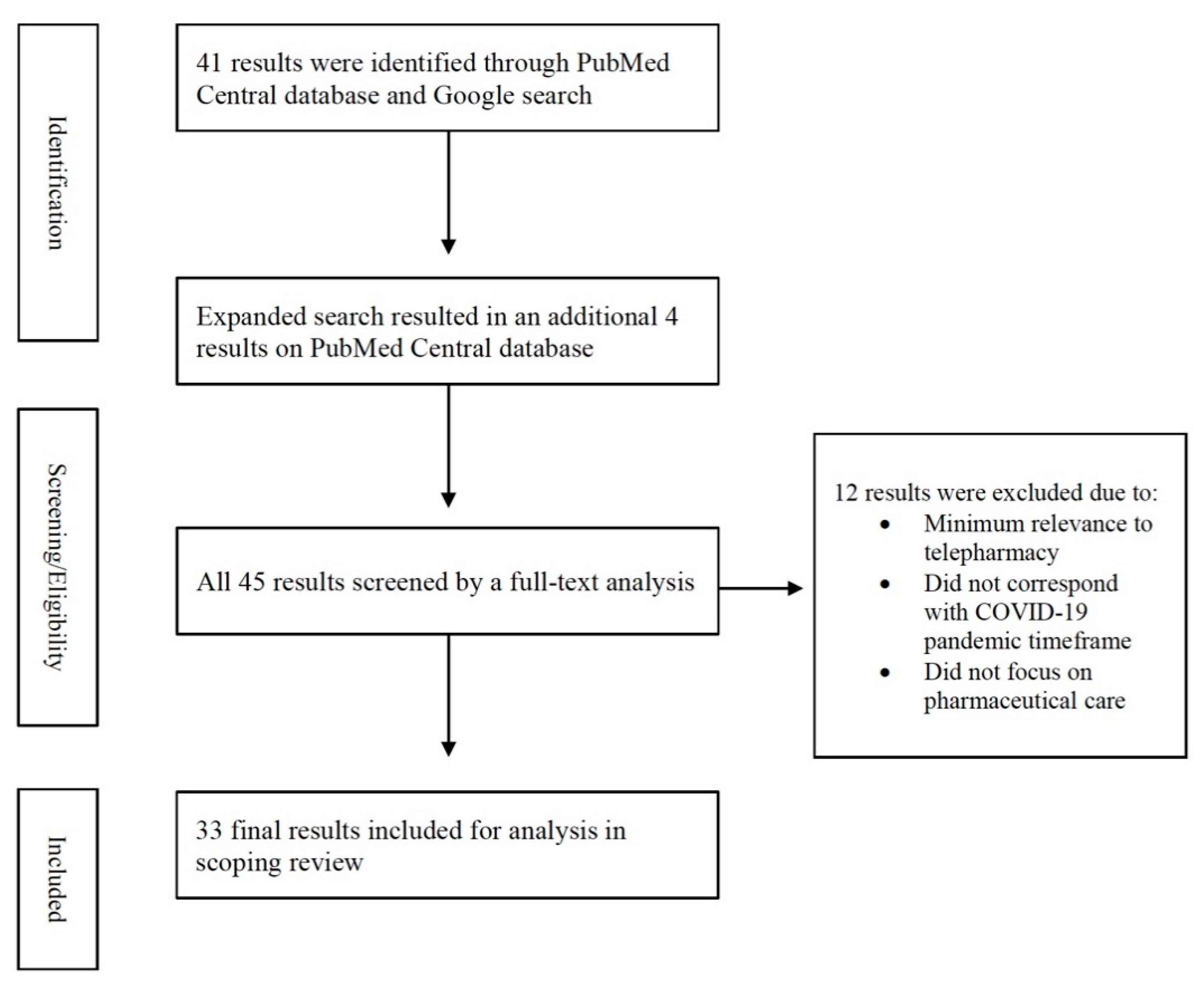
2. Materials and Methods
3. Results
3.1. What Were the Various Telepharmacy Initiatives Implemented?
3.2. What Were the Challenges Faced by Pharmacies When Implementing Telehealth Initiatives?
3.3. What Were the Strategies Used by Pharmacies to Overcome the Challenges?
3.4. What Were Some of the Innovative Methods Used by Pharmacies to Implement Telepharmacy?
4. Discussion
4.1. Future Steps
4.2. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 4 August 2021).
- Centers for Disease Control and Prevention. Basics of COVID-19. Available online: https://www.cdc.gov/coronavirus/2019-ncov/your-health/about-covid-19/basics-covid-19.html (accessed on 15 August 2021).
- Miller, I.F.; Becker, A.D.; Grenfell, B.T.; Metcalf, C.J.E. Disease and healthcare burden of COVID-19 in the United States. Nat. Med. 2020, 26, 1212–1217. [Google Scholar] [CrossRef]
- Diaz, A.; Sarac, B.A.; Schoenbrunner, A.R.; Janis, J.E.; Pawlik, T.M. Elective surgery in the time of COVID-19. Am. J. Surg. 2020, 219, 900–902. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef] [Green Version]
- Hossain, M.M.; Tasnim, S.; Sultana, A.; Faizah, F.; Mazumder, H.; Zou, L.; McKyer, E.L.J.; Ahmed, H.U.; Ma, P. Epidemiology of mental health problems in COVID-19: A review. F1000Research 2020, 9, 636. [Google Scholar] [CrossRef]
- Nicola, M.; Alsafi, Z.; Sohrabi, C.; Kerwan, A.; Al-Jabir, A.; Iosifidis, C.; Agha, M.; Agha, R. The socio-economic implications of the coronavirus pandemic (COVID-19): A review. Int. J. Surg. 2020, 78, 185–193. [Google Scholar] [CrossRef]
- Birkmeyer, J.D.; Barnato, A.; Birkmeyer, N.; Bessler, R.; Skinner, J. The impact of the COVID-19 pandemic on hospital admissions in the United States. Health Aff. (Millwood) 2020, 39, 2010–2017. [Google Scholar] [CrossRef]
- Health Resources & Services Administration. Office for the Advancement of Telehealth. Available online: https://www.hrsa.gov/rural-health/telehealth (accessed on 14 October 2021).
- American Society of Health-Systems Pharmacists. ASHP Statement on Telepharmacy. Available online: https://www.ashp.org/-/media/assets/pharmacy-informaticist/docs/sopit-bp-telepharmacy-statement.ashx (accessed on 14 October 2021).
- Centers for Disease Control and Prevention. Using Telehealth to Expand Access to Essential Health Services during the COVID-19 Pandemic. Available online: https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html (accessed on 15 August 2021).
- Hayden, J.C.; Parkin, R. The challenges of COVID-19 for community pharmacists and opportunities for the future. Ir. J. Psychol. Med. 2020, 37, 198–203. [Google Scholar] [CrossRef]
- Wickware, C.; Wilkinson, E. The new abnormal: Vulnerable patients hit by pharmacy closures. Pharm. J. 2020, 305. [Google Scholar] [CrossRef]
- Shuman, A.G.; Fox, E.R.; Unguru, Y. COVID-19 and drug shortages: A call to action. J. Manag. Care Spec. Pharm. 2020, 26, 945–947. [Google Scholar] [CrossRef]
- McLaughlin, M.; Kotis, D.; Thomson, K.; Harrison, M.; Fennessy, G.; Postelnick, M.; Scheetz, M.H. Effects on patient care caused by drug shortages: A survey. J. Manag. Care Pharm. 2013, 19, 783–788. [Google Scholar] [CrossRef] [Green Version]
- Poudel, A.; Nissen, L.M. Telepharmacy: A pharmacist’s perspective on the clinical benefits and challenges. Integr. Pharm. Res. Pract. 2016, 5, 75–82. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tzanetakos, G.; Ullrich, F.; Meuller, K. Telepharmacy rules and statutes: A 50-state survey. Rural Policy Brief 2017, 4, 1–4. [Google Scholar]
- United States Congress. H.R.6074-Coronavirus Preparedness and Response Supplemental Appropriations Act. Available online: https://www.congress.gov/bill/116th-congress/house-bill/6074/titles (accessed on 29 June 2021).
- Department of Health and Human Services Office of the Secretary. Federal Register Vol. 85, No. 52 Declaration under the Public Readiness and Emergency Preparedness Act for Medical Countermeasures against COVID-19. Available online: https://www.federalregister.gov/d/2020-05484 (accessed on 20 June 2021).
- Elbeddini, A.; Yeats, A. Pharmacist intervention amid the coronavirus disease 2019 (COVID-19) pandemic: From direct patient care to telemedicine. J. Pharm. Policy Pract. 2020, 13, 23. [Google Scholar] [CrossRef] [PubMed]
- Kilova, K.; Mihaylova, A.; Peikova, L. Opportunities of information communication technologies for providing pharmaceutical care in the COVID-19 pandemic. Pharmacia 2021, 68, 9. [Google Scholar] [CrossRef]
- Martin, R.D. Leveraging telecommuting pharmacists in the post-COVID-19 world. J. Am. Pharm. Assoc. 2020, 60, e113–e115. [Google Scholar] [CrossRef] [PubMed]
- Karimian, Z.; Gholami, K. The shifting landscape of pharmaceutical care—During and beyond the COVID-19 pandemic. J. Pharm. Care 2020, 8, 96–98. [Google Scholar] [CrossRef]
- Bukhari, N.; Rasheed, H.; Nayyer, B.; Babar, Z.U. Pharmacists at the frontline beating the COVID-19 pandemic. J. Pharm. Policy Pract. 2020, 13, 8. [Google Scholar] [CrossRef] [Green Version]
- Bernstein, I. An expert shares pharmacy’s biggest COVID-19 lessons—So far. Pharmacy Today 2021, 27, 22–23. [Google Scholar] [CrossRef]
- Shafiee Hanjani, L.; Bell, J.S.; Freeman, C. Undertaking medication review by telehealth. Aust. J. Gen. Pract. 2020, 49, 826–831. [Google Scholar] [CrossRef]
- Liu, S.; Luo, P.; Tang, M.; Hu, Q.; Polidoro, J.P.; Sun, S.; Gong, Z. Providing pharmacy services during the coronavirus pandemic. Int. J. Clin. Pharm. 2020, 42, 299–304. [Google Scholar] [CrossRef] [Green Version]
- Killeen, R.M.; Grindrod, K.; Ong, S.W. Innovations in practice: Telepharmacy’s time has arrived. Can. Pharm. J. (Ott) 2020, 153, 252–255. [Google Scholar] [CrossRef]
- Mohammad, I.; Berlie, H.D.; Lipari, M.; Martirosov, A.L.; Duong, A.A.; Faraj, M.; Bacon, O.; Garwood, C.L. Ambulatory care practice in the COVID-19 era: Redesigning clinical services and experiential learning. J. Am. Coll. Clin. Pharm. 2020. [Google Scholar] [CrossRef] [PubMed]
- Traynor, K. Pharmacists turn to telehealth to meet patients’ needs. Am. J. Health Syst. Pharm. 2020, 77, 1822–1824. [Google Scholar] [CrossRef] [PubMed]
- Paola, S. Telehealth: Conducting medication reviews during COVID-19. Aust. J. Pharm. 2020, 101, 22–25. [Google Scholar] [CrossRef]
- Segal, E.M.; Alwan, L.; Pitney, C.; Taketa, C.; Indorf, A.; Held, L.; Lee, K.S.; Son, M.; Chi, M.; Diamantides, E.; et al. Establishing clinical pharmacist telehealth services during the COVID-19 pandemic. Am. J. Health Syst. Pharm. 2020, 77, 1403–1408. [Google Scholar] [CrossRef]
- Yemm, K.E.; Arnall, J.R.; Cowgill, N.A. Necessity of pharmacist-driven nonprescription telehealth consult services in the era of COVID-19. Am. J. Health Syst. Pharm. 2020, 77, 1188. [Google Scholar] [CrossRef]
- Li, H.; Zheng, S.; Liu, F.; Liu, W.; Zhao, R. Fighting against COVID-19: Innovative strategies for clinical pharmacists. Res. Social Adm. Pharm. 2021, 17, 1813–1818. [Google Scholar] [CrossRef]
- Margusino-Framinan, L.; Illarro-Uranga, A.; Lorenzo-Lorenzo, K.; Monte-Boquet, E.; Marquez-Saavedra, E.; Fernandez-Bargiela, N.; Gomez-Gomez, D.; Lago-Rivero, N.; Poveda-Andres, J.L.; Diaz-Acedo, R.; et al. Pharmaceutical care to hospital outpatients during the COVID-19 pandemic: Telepharmacy. Farm. Hosp. 2020, 44, 61–65. [Google Scholar] [CrossRef] [PubMed]
- Tortajada-Goitia, B.; Morillo-Verdugo, R.; Margusino-Framinan, L.; Marcos, J.A.; Fernandez-Llamazares, C.M. Survey on the situation of telepharmacy as applied to the outpatient care in hospital pharmacy departments in Spain during the COVID-19 pandemic. Farm. Hosp. 2020, 44, 135–140. [Google Scholar] [CrossRef]
- Asseri, A.A.; Manna, M.M.; Yasin, I.M.; Moustafa, M.M.; Roubie, G.M.; El-Anssay, S.M.; Baqawie, S.K.; Alsaeed, M.A. Implementation and evaluation of telepharmacy during COVID-19 pandemic in an academic medical city in the Kingdom of Saudi Arabia: Paving the way for telepharmacy. World J. Adv. Res. Rev. 2020, 7, 218–226. [Google Scholar] [CrossRef]
- Elson, E.C.; Oermann, C.; Duehlmeyer, S.; Bledsoe, S. Use of telemedicine to provide clinical pharmacy services during the SARS-CoV-2 pandemic. Am. J. Health Syst. Pharm. 2020, 77, 1005–1006. [Google Scholar] [CrossRef] [PubMed]
- Hua, X.; Gu, M.; Zeng, F.; Hu, H.; Zhou, T.; Zhang, Y.; Shi, C. Pharmacy administration and pharmaceutical care practice in a module hospital during the COVID-19 epidemic. J. Am. Pharm. Assoc. 2020, 60, 431–438. [Google Scholar] [CrossRef]
- Ashiru-Oredope, D.; Chan, A.; Olaoye, O.; Rutter, V.; Babar, Z.-U.-D.; Anderson, C.; Matuluko, A.; Tuck, C.; Halai, M.; Wickens, H.; et al. COVID-19: Needs assessment of the pharmacy profession and contributions so far across the Commonwealth. Res. Sqaure 2020. [Google Scholar] [CrossRef]
- Peláez Bejarano, A.; Villar Santos, P.; Robustillo-Cortés, M.d.l.A.; Sánchez Gómez, E.; Santos Rubio, M.D. Implementation of a novel home delivery service during pandemic. Eur. J. Hosp. Pharm. 2020, 28, s120–s123. [Google Scholar] [CrossRef]
- Mohamed Ibrahim, O.; Ibrahim, R.M.; Abdel-Qader, D.H.; Al Meslamani, A.Z.; Al Mazrouei, N. Evaluation of telepharmacy services in light of COVID-19. Telemed J. E Health 2020, 27, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Koster, E.S.; Philbert, D.; Bouvy, M.L. Impact of the COVID-19 epidemic on the provision of pharmaceutical care in community pharmacies. Res. Soc. Adm. Pharm. 2021, 17, 2002–2004. [Google Scholar] [CrossRef] [PubMed]
- Kulatunga, G.G.; Hewapathirana, R.; Marasinghe, I.R.B.; Dissanayake, V.H.W. A review of telehealth practices in Sri Lanka in the context of the COVID-19 pandemic. Sri Lanka J. Biomed. Inform. 2020, 11, 8–19. [Google Scholar] [CrossRef]
- Mallhi, T.H.; Liaqat, A.; Abid, A.; Khan, Y.H.; Alotaibi, N.H.; Alzarea, A.I.; Tanveer, N.; Khan, T.M. Multilevel engagements of pharmacists during the COVID-19 pandemic: The way forward. Front. Public Health 2020, 8, 561924. [Google Scholar] [CrossRef]
- Saghir, S.; Hashmi, F.K.; Khadka, S.; Rizvi, M. Paradigm shift in practice: The role of pharmacists in COVID-19 management. EJMS 2020, 2, 111–115. [Google Scholar] [CrossRef]
- Mohiuddin, A.K. Prospect of tele-pharmacists in COVID-19 pandemic situation in Bangladesh. J. Biosci. Biomed. Eng. 2020, 1. [Google Scholar] [CrossRef]
- Mohiuddin, A.; Nasirullah, M. Scope of tele-pharmacists in pandemic situations of Bangladesh. Curr. Tr. Clin. Med. Sci. 2020, 1. [Google Scholar] [CrossRef]
- Crilly, P.; Kayyali, R. A systematic review of randomized controlled trials of telehealth and digital technology use by community pharmacists to improve public health. Pharmacy 2020, 8, 137. [Google Scholar] [CrossRef] [PubMed]
- Muflih, S.M.; Al-Azzam, S.; Abuhammad, S.; Jaradat, S.K.; Karasneh, R.; Shawaqfeh, M.S. Pharmacists’ experience, competence and perception of telepharmacy technology in response to COVID-19. Int. J. Clin. Pract. 2021, 75, e14209. [Google Scholar] [CrossRef] [PubMed]
- Plantado, A.N.R.; de Guzman, H.J.D.; Mariano, J.E.C.; Salvan, M.; Benosa, C.A.C.; Robles, Y.R. Development of an online telepharmacy service in the Philippines and analysis of its usage during the COVID-19 pandemic. J. Pharm. Pract. 2021, 8971900211033120. [Google Scholar] [CrossRef]
- Hedima, E.W.; Okoro, R.N. Telepharmacy: An opportunity for community pharmacists during the COVID-19 pandemic in Sub Saharan Africa. Health Policy Technol. 2021, 10, 23–24. [Google Scholar] [CrossRef]
| Article Reference, Title, and Country | Key Points | |
|---|---|---|
| Expert Opinion | ||
| [20] | Pharmacist intervention amid the coronavirus disease 2019 (COVID-19) pandemic: from direct patient care to telemedicine. Canada | Increased demand for telepharmacy; Privacy and confidentiality concerns; Patient consent; Building trust with the patient; GeriMedRisk app |
| [21] | Opportunities of information communication technologies for providing pharmaceutical care in the COVID-19 pandemic. Bulgaria | Mobile applications such as APOmondo; Quality, reliability, and security requirements for healthcare system |
| [22] | Leveraging telecommuting pharmacists in the post-COVID-19 world. USA | HIPAA-compliant communication platforms; Ensuring efficiency of the telepharmacists working remotely; Telecommuting models |
| [23] | The shifting landscape of pharmaceutical care–during and beyond the COVID-19 pandemic. Iran | Digital information and communication technologies that are affordable and user friendly; patient confidentiality, Electronic prescriptions and online ordering |
| [24] | Pharmacists at the frontline beating the COVID-19 pandemic. New Zealand | New Zealand–Hotline numbers for phone consultations and prescription orders Australia–Remote dispensing China and Columbia–Home delivery Pakistan–Triaging patients for consultation |
| [25] | An expert shares pharmacy’s biggest COVID-19 lessons-so far. USA | Video/Phone consultations, Ease of requirements to Facetime or Zoom, fair and equitable access to telepharmacy programs should be advocated for after the pandemic. |
| [26] | Undertaking medication review by telehealth. Australia | Need of additional time and resources for telepharmacy-appropriate equipment, location, audio vs. audiovisual technology; Resources for pharmacists to conduct televisits by professional associations, regulatory bodies and universities |
| [27] | Providing pharmacy services during the coronavirus pandemic. China | WeChat, online remote pharmacy service |
| [28] | Innovations in practice: telepharmacy’s time has arrived. Canada | Reduced digital literacy; Risk of privacy and security; Disclaimer statement for all televisits, Record patient satisfaction to determine further use |
| [29] | Ambulatory care practice in the COVID-19 era: redesigning clinical services and experiential learning. USA | Telepharmacy for medication management using Facetime and Skype; Expanded approvals for telehealth, billing codes |
| [30] | Pharmacists turn to telehealth to meet patients’ needs. USA | Reimbursement for televisits; ASHP advocating for telepharmacy; Co-visit model with PCP |
| [31] | Telehealth: conducting medication reviews during COVID-19. Australia | Telehealth if patient meets eligibility criteria; Risk-benefit assessment to ensure suitability for patient; Informed consent; Ensuring insurance coverage |
| Case Studies/Original Research | ||
| [32] | Establishing clinical pharmacist telehealth services during the COVID-19 pandemic. USA | Coronavirus Preparedness and Response Supplemental Appropriations Act, credentialing pharmacists for telehealth; Additional time and resources needed for telepharmacy; HIPPA-compliant platform |
| [33] | Necessity of pharmacist-driven nonprescription telehealth consult services in the era of COVID-19. USA | Telehealth for at-risk populations; Adaptation of clinical assessment tools |
| [34] | Fighting against COVID-19: innovative strategies for clinical pharmacists. China | Cloud pharmacy care for patients to text and call pharmacists; WeChat App for online Pharmaceutical monitoring; multimedia health education |
| [35] | Pharmaceutical care to hospital outpatients during the COVID-19 pandemic: telepharmacy. Spain | Outpatient consultation services, home drug deliver using geolocation; increased need for resources |
| [36] | Survey on the situation of telepharmacy as applied to the outpatient care in hospital pharmacy departments in Spain during the COVID-19 pandemic. Spain | Strategic Outpatient Pharmaceutical Care Map for gradual implementation of telepharmacy throughout Spain; Has the capacity for nationwide implementation |
| [37] | Implementation and evaluation of telepharmacy during COVID-19 pandemic in an academic medical city in the Kingdom of Saudi Arabia: paving the way for telepharmacy. Saudi Arabia | Adopted institutional pandemic response model, Home delivery of medications followed by remote counseling using HIPPA-compliant video; Business WhatsApp; SEHA App for visual media consultations; National policy |
| [38] | Use of telemedicine to provide clinical pharmacy services during the SARS-CoV-2 pandemic. USA | Exercise enforcement discretion to use videoconferencing not fully compliant with HIPAA; Use of Telephones, Microsoft Teams and EMR for profile reviews, inpatient rounds, and patient education |
| [39] | Pharmacy administration and pharmaceutical care practice in a module hospital during the COVID-19 epidemic. China | Zero contact pharmaceutical care model for virtual consultation; WeChat App; Radio station to relieve panic and tension among public |
| [40] | COVID-19: needs assessment of the pharmacy profession and contributions so far across the Commonwealth. The Commonwealth | COVID-19 resources, CwPAMS app; Webinars to train pharmacists; challenges to remote working such as isolation |
| [41] | Implementation of a novel home delivery service during pandemic. Spain | Identifying patients who require onsite pharmaceutical care and telepharmacy; Medication delivery service; Telephone survey of patient satisfaction |
| [42] | . Evaluation of telepharmacy services in light of COVID-19. United Arab Emirates | Videoconferencing; Home delivery of meds; More dispensing errors; Effectiveness of telepharmacy was evaluated |
| [43] | Impact of the COVID-19 epidemic on the provision of pharmaceutical care in community pharmacies. Netherlands | Online education and counseling; Concerns about privacy; Webinars and educational sessions to reduce telepharmacy skepticism |
| Review Articles | ||
| [44] | A review of telehealth practices in Sri Lanka in the context of the COVID-19 pandemic. Sri Lanka | Videoconferencing and e-prescriptions; Reduced standard of care and patient–physician relationship; Poor control of controlled prescriptions; Privacy and cybersecurity, Deficient reimbursement; Need for national framework |
| [45] | Multilevel engagements of pharmacists during the COVID-19 pandemic: the way forward. Saudi Arabia, Pakistan | Webpages, message services and social networking links to respond to patient queries |
| [46] | Paradigm shift in practice: the role of pharmacists in COVID-19 management. Pakistan | Multimedia health education; Multidisciplinary treatments; Need for training and curriculum for disaster management practice for pharmacists |
| [47] | Prospect of tele-pharmacists in COVID-19 pandemic situation in Bangladesh. Bangladesh | Physician-led responsive model and telehealthcare by pharmacists |
| [48] | Scope of tele-pharmacists in pandemic situations of Bangladesh. Bangladesh | Responsive model, policy makers, appropriate and quality information |
| [49] | A systematic review of randomized controlled trials of telehealth and digital technology use by community pharmacists to improve public health. USA | Social media, smartphone mobile application, health and digital literacy, blueprint, public awareness |
| [50] | Pharmacists’ experience, competence and perception of telepharmacy technology in response to COVID-19. Jordan | Social media platforms, web-based survey, quality of pharmaceutical care |
| [51] | Development of an Online Telepharmacy Service in the Philippines and Analysis of Its Usage During the COVID-19 Pandemic. Philippines | Online telepharmacy service, alleviate fear, counseling services, Google Form |
| [52] | Telepharmacy: An opportunity for community pharmacists during the COVID-19 pandemic in Sub Saharan Africa. Africa | Telepharmacy models, videoconferencing, medication delivery, medication adherence |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Unni, E.J.; Patel, K.; Beazer, I.R.; Hung, M. Telepharmacy during COVID-19: A Scoping Review. Pharmacy 2021, 9, 183. https://doi.org/10.3390/pharmacy9040183
Unni EJ, Patel K, Beazer IR, Hung M. Telepharmacy during COVID-19: A Scoping Review. Pharmacy. 2021; 9(4):183. https://doi.org/10.3390/pharmacy9040183
Chicago/Turabian StyleUnni, Elizabeth J., Kanchita Patel, Isaac Rex Beazer, and Man Hung. 2021. "Telepharmacy during COVID-19: A Scoping Review" Pharmacy 9, no. 4: 183. https://doi.org/10.3390/pharmacy9040183
APA StyleUnni, E. J., Patel, K., Beazer, I. R., & Hung, M. (2021). Telepharmacy during COVID-19: A Scoping Review. Pharmacy, 9(4), 183. https://doi.org/10.3390/pharmacy9040183







