Diabetes and Frail Older Patients: Glycemic Control and Prescription Profile in Real Life
Abstract
:1. Introduction
2. Materials and Methods
3. Results
3.1. Characteristics of Study Population
3.2. Analysis of Glucose-Lowering Drug Prescriptions’ Appropriateness
3.3. Analysis of Glycemic Balance
3.4. Hypoglycemic Episodes
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Label | Number of Prescribed Medications (n = 151) | Average Daily Dosage |
|---|---|---|
| Insulins and analogs | 53 (35.1%) | IU |
| Rapid-acting injectable insulins and analogs | 14 (9.3%) | |
| Insulins and analogs with intermediate or long-acting action and rapid onset of action by injection | 1 (0.7%) | |
| Long-acting injectable insulins and analogs | 38 (25.2%) | |
| Insulin glargine | 28 | 20.0 |
| Insulin detemir | 10 | 21.5 |
| Glucose-loweringdrugs other than insulins | mg | |
| Biguanide | 50 (33.1%) | 1739.0 |
| Sulfonylurea drugs | 13 (8.6%) | |
| Glibenclamide | 1 | 7.5 |
| Gliclazide | 9 | 85.6 |
| Glimepiride | 3 | 1.7 |
| Alpha glucosidase inhibitors | 3 (2.0%) | 150.0 |
| Dipeptidyl Peptidase 4 (DPP-4) inhibitors | 19 (12.6%) | |
| Sitagliptin | 15 | 96.4 |
| Vildagliptin | 4 | 75.0 |
| Glucagon-Like-Peptide-1 (GLP-1) Analogs | 2 (1.3%) | |
| Liraglutide | 2 | 1.5 |
| Repaglinide | 11 | 2.6 |
| Nonfrail Patients (FRIED Score: 0 to 2) n = 22 | Frail Patients (FRIED Score: 3 to 5) n = 44 | Total | |
|---|---|---|---|
| Number of patients for whom all treatments are adjusted to kidney function | 8 (36.4%) | 25 (56.8%) | 33 (50%) |
| Number of patients with at least 1 PIMs related to renal failure | 8 a (36.4%) | 13 b (29.5%) | 21 (31.8%) |
| Metformin | 6 (27.3%) | 12 (27.3%) | 18 (27.3%) |
| Sitagliptin | 3 (13.6%) | 5 (11.4%) | 8 (12.1%) |
| Acarbose | 1 (4.5%) | 0 (0%) | 1 (1.5%) |
| Nonfrail Patients (FRIED Score: 0 to 2) | Frail Patients (FRIED Score: 3 to 5) | p Value | |
|---|---|---|---|
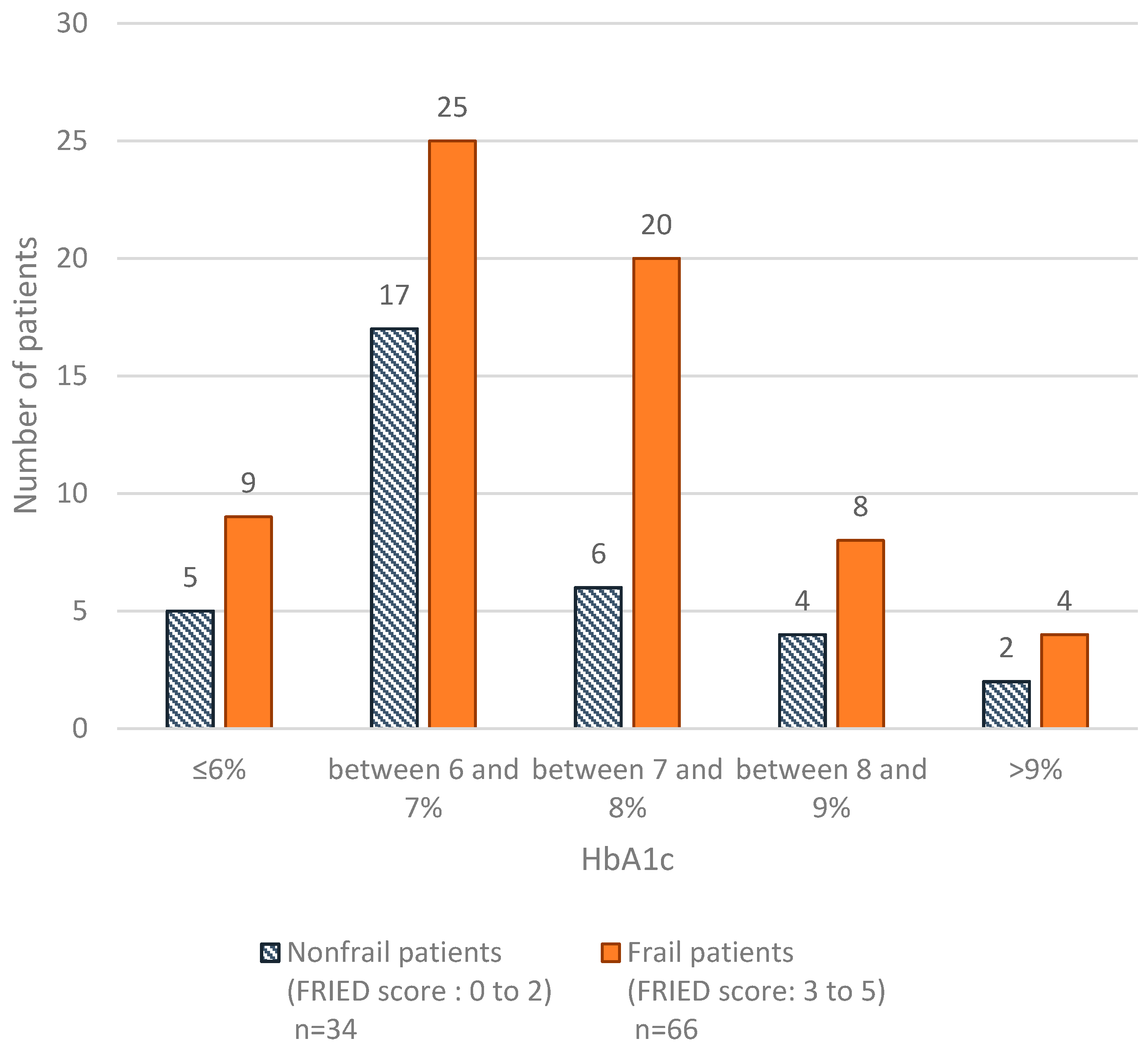
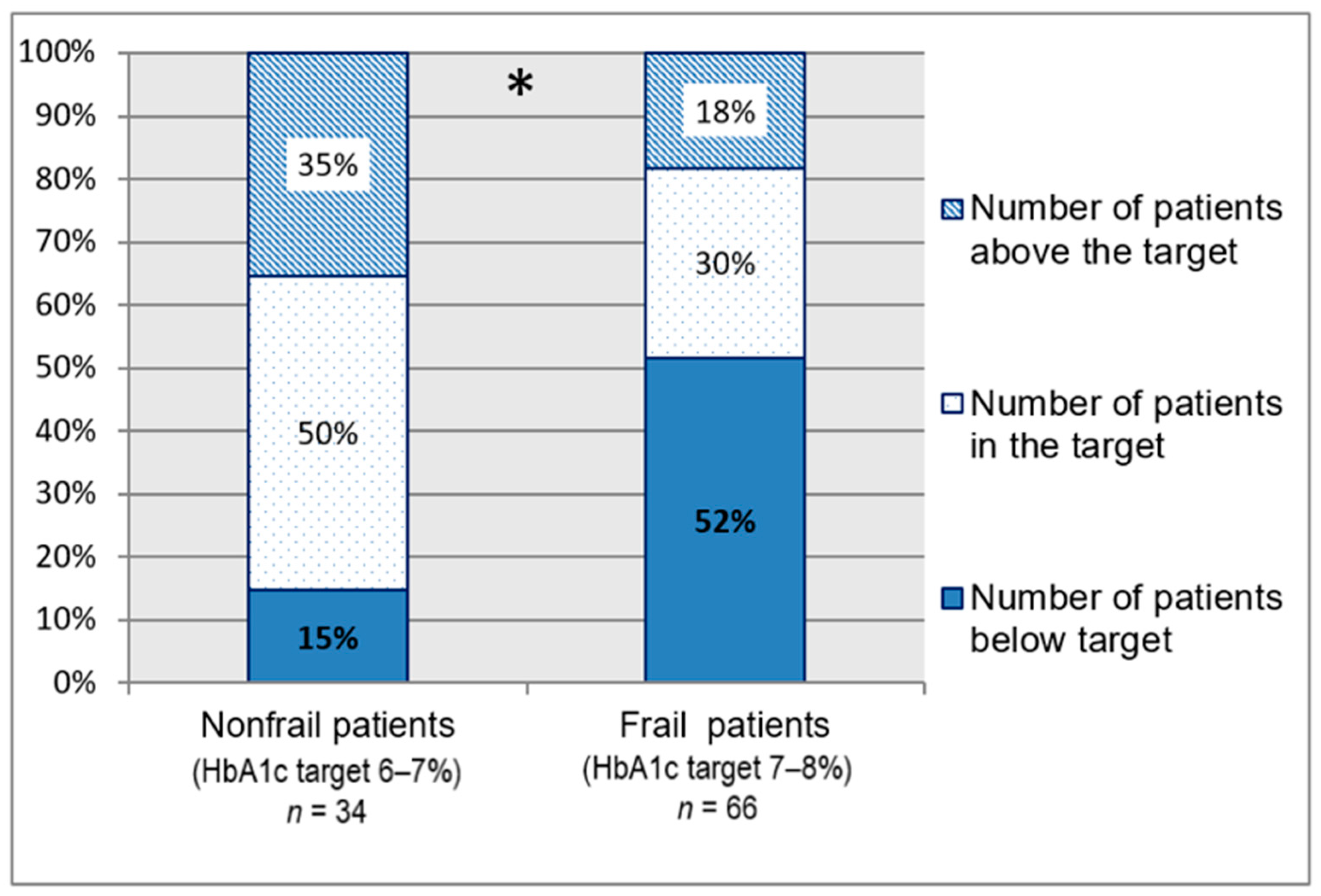
| HbA1c level | n = 34 | n = 66 | |
| ≤7% | 22 (64.7%) | 34 (51.5%) | 0.35 * |
| between 7% and 8% | 6 (17.6%) | 20 (30.3%) | |
| >8% | 6 (17.6%) | 12 (18.2%) | |
| Drugs | n = 36 | n = 74 | |
| Number of glucose-lowering drugs | 1.3 ± 1.0 | 1.4 ± 1.0 | 0.79 # |
| No drugs | 7 (19.4%) | 13 (17.6%) | 0.66 * |
| OGLDs only | 19 (52.8%) | 32 (43.2%) | |
| Insulin | 5 (13.9%) | 17 (23.0%) | |
| OGLDs + Insulin | 5 (13.9%) | 12 (16.2%) |
References
- Haute Autorité de Santé—Stratégie Médicamenteuse du Contrôle Glycémique du Diabète de Type 2. Available online: https://www.has-sante.fr/portail/jcms/c_1022476/fr/strategie-medicamenteuse-du-controle-glycemique-du-diabete-de-type-2 (accessed on 8 July 2017).
- Blacher, J.; Halimi, J.-M.; Hanon, O.; Mourad, J.-J.; Pathak, A.; Schnebert, B.; Girerd, X. Prise en charge de l’hypertension artérielle de l’adulte. Recommandations 2013 de la Société française d’hypertension artérielle. Presse Méd. 2013, 42, 819–825. [Google Scholar] [CrossRef] [PubMed]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older Adults Evidence for a Phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M157. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Young, J.; Iliffe, S.; Rikkert, M.O.; Rockwood, K. Frailty in Elderly People. Lancet 2013, 381, 752–762. [Google Scholar] [CrossRef] [Green Version]
- Lang, P.-O.; Michel, J.-P.; Zekry, D. Frailty Syndrome: A Transitional State in a Dynamic Process. Gerontology 2009, 55, 539–549. [Google Scholar] [CrossRef]
- Lee, A.K.; Rawlings, A.M.; Lee, C.J.; Gross, A.L.; Huang, E.S.; Sharrett, A.R.; Coresh, J.; Selvin, E. Severe Hypoglycaemia, Mild Cognitive Impairment, Dementia and Brain Volumes in Older Adults with Type 2 Diabetes: The Atherosclerosis Risk in Communities (ARIC) Cohort Study. Diabetologia 2018, 61, 1956–1965. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malabu, U.; Vangaveti, V.; Kennedy, L. Disease Burden Evaluation of Fall-Related Events in the Elderly Due to Hypoglycemia and Other Diabetic Complications: A Clinical Review. Clin. Epidemiol. 2014, 6, 287–294. [Google Scholar] [CrossRef] [Green Version]
- Darmon, P.; Bauduceau, B.; Bordier, L.; Charbonnel, B.; Cosson, E.; Detournay, B.; Fontaine, P.; Grimaldi, A.; Gourdy, P.; Guerci, B.; et al. Prise de position de la Société Francophone du Diabète (SFD) sur la prise en charge médicamenteuse de l’hyperglycémie du patient diabétique de type 2—2019. 121. Méd. Mal. Métabol. 2019, 13, 22. [Google Scholar] [CrossRef]
- Sinclair, A.J.; Abdelhafiz, A.; Dunning, T.; Izquierdo, M.; Rodriguez Manas, L.; Bourdel-Marchasson, I.; Morley, J.E.; Munshi, M.; Woo, J.; Vellas, B. An International Position Statement on the Management of Frailty in Diabetes Mellitus: Summary of Recommendations 2017. J. Frailty Aging 2018, 7, 10–20. [Google Scholar] [CrossRef]
- Sinclair, A.J.; Paolisso, G.; Castro, M.; Bourdel-Marchasson, I.; Gadsby, R.; Mañas, L.R. European Diabetes Working Party for Older People 2011 Clinical Guidelines for Type 2 Diabetes Mellitus. Executive Summary. Diabetes Metab. 2011, 37, S27–S38. [Google Scholar] [CrossRef]
- American Diabetes Association. 7. Diabetes Technology: Standards of Medical Care in Diabetes—2019. Diabetes Care 2021, 44, S85–S99. [Google Scholar] [CrossRef]
- Meneilly, G.S.; Knip, A.; Miller, D.B.; Sherifali, D.; Tessier, D.; Zahedi, A. Diabetes in Older People. Can. J. Diabetes 2018, 42, S283–S295. [Google Scholar] [CrossRef] [Green Version]
- Renom-Guiteras, A.; Meyer, G.; Thürmann, P.A. The EU(7)-PIM List: A List of Potentially Inappropriate Medications for Older People Consented by Experts from Seven European Countries. Eur. J. Clin. Pharmacol. 2015, 71, 861–875. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Geriatric Frailty Clinic (G.F.C) for Assessment of Frailty and Prevention of Disability Team; Tavassoli, N.; Guyonnet, S.; Abellan Van Kan, G.; Sourdet, S.; Krams, T.; Soto, M.-E.; Subra, J.; Chicoulaa, B.; Ghisolfi, A.; et al. Description of 1108 Older Patients Referred by Their Physician to the “Geriatric Frailty Clinic (G.F.C) for Assessment of Frailty and Prevention of Disability” at the Gerontopole. J. Nutr. Health Aging 2014, 18, 457–464. [Google Scholar] [CrossRef] [PubMed]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. BMJ 2007, 335, 806–808. [Google Scholar] [CrossRef] [Green Version]
- Demougeot, L.; van Kan, G.A.; Vellas, B.; de Souto Barreto, P. Frailty Detection with the Gérontopôle Frailty Screening Tool (GFST). J. Frailty Aging 2013, 2, 150–152. [Google Scholar] [CrossRef]
- Action to Control Cardiovascular Risk in Diabetes Study Group; Gerstein, H.C.; Miller, M.E.; Byington, R.P.; Goff, D.C.; Bigger, J.T.; Buse, J.B.; Cushman, W.C.; Genuth, S.; Ismail-Beigi, F.; et al. Effects of Intensive Glucose Lowering in Type 2 Diabetes. N. Engl. J. Med. 2008, 358, 2545–2559. [Google Scholar] [CrossRef] [Green Version]
- Duckworth, W.; Abraira, C.; Moritz, T.; Reda, D.; Emanuele, N.; Reaven, P.D.; Zieve, F.J.; Marks, J.; Davis, S.N.; Hayward, R.; et al. Glucose Control and Vascular Complications in Veterans with Type 2 Diabetes. N. Engl. J. Med. 2009, 360, 129–139. [Google Scholar] [CrossRef] [Green Version]
- Motter, F.R.; Fritzen, J.S.; Hilmer, S.N.; Paniz, É.V.; Paniz, V.M.V. Potentially Inappropriate Medication in the Elderly: A Systematic Review of Validated Explicit Criteria. Eur. J. Clin. Pharmacol. 2018, 74, 679–700. [Google Scholar] [CrossRef] [PubMed]
- Allenet, B.; Bedouch, P.; Rose, F.-X.; Escofier, L.; Roubille, R.; Charpiat, B.; Juste, M.; Conort, O. Validation of an Instrument for the Documentation of Clinical Pharmacists’ Interventions. Pharm. World Sci. 2006, 28, 181–188. [Google Scholar] [CrossRef]
- Lipska, K.J.; Ross, J.S.; Miao, Y.; Shah, N.D.; Lee, S.J.; Steinman, M.A. Potential Overtreatment of Diabetes Mellitus in Older Adults With Tight Glycemic Control. JAMA Intern. Med. 2015, 175, 356. [Google Scholar] [CrossRef] [PubMed]
- Dejager, S.; Penfornis, A.; Fiquet, B.; Blickle, J.F. Potential Glycemic Overtreatment in Patients >75 Years with Type 2 Diabetes Mellitus and Renal Disease: Experience from the Observational OREDIA Study. Diabetes Metab. Syndr. Obes. Targets Ther. 2015, 303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Müller, N.; Khunti, K.; Kuss, O.; Lindblad, U.; Nolan, J.J.; Rutten, G.E.; Trento, M.; Porta, M.; Roth, J.; Charpentier, G.; et al. Is There Evidence of Potential Overtreatment of Glycaemia in Elderly People with Type 2 Diabetes? Data from the GUIDANCE Study. Acta Diabetol. 2017, 54, 209–214. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- 2019 American Geriatrics Society Beers Criteria® Update Expert Panel; Fick, D.M.; Semla, T.P.; Steinman, M.; Beizer, J.; Brandt, N.; Dombrowski, R.; DuBeau, C.E.; Pezzullo, L.; Epplin, J.J. American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J. Am. Geriatr. Soc. 2019, 67, 674–694. [Google Scholar] [CrossRef]
- O’Mahony, D.; O’Sullivan, D.; Byrne, S.; O’Connor, M.N.; Ryan, C.; Gallagher, P. STOPP/START Criteria for Potentially Inappropriate Prescribing in Older People: Version 2. Age Ageing 2015, 44, 213–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schernthaner, G.; Grimaldi, A.; Di Mario, U.; Drzewoski, J.; Kempler, P.; Kvapil, M.; Novials, A.; Rottiers, R.; Rutten, G.; Shaw, K.M. GUIDE Study: Double-Blind Comparison of Once-Daily Gliclazide MR and Glimepiride in Type 2 Diabetic Patients. Eur. J. Clin. Investig. 2004, 34, 535–542. [Google Scholar] [CrossRef]
- Strain, W.D.; Lukashevich, V.; Kothny, W.; Hoellinger, M.-J.; Paldánius, P.M. Individualised Treatment Targets for Elderly Patients with Type 2 Diabetes Using Vildagliptin Add-on or Lone Therapy (INTERVAL): A 24 Week, Randomised, Double-Blind, Placebo-Controlled Study. Lancet 2013, 382, 409–416. [Google Scholar] [CrossRef]
- Bethel, M.A.; Engel, S.S.; Green, J.B.; Huang, Z.; Josse, R.G.; Kaufman, K.D.; Standl, E.; Suryawanshi, S.; Van de Werf, F.; McGuire, D.K.; et al. Assessing the Safety of Sitagliptin in Older Participants in the Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS). Diabetes Care 2017, 40, 494–501. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Currie, C.J.; Peters, J.R.; Tynan, A.; Evans, M.; Heine, R.J.; Bracco, O.L.; Zagar, T.; Poole, C.D. Survival as a Function of HbA 1c in People with Type 2 Diabetes: A Retrospective Cohort Study. Lancet 2010, 375, 481–489. [Google Scholar] [CrossRef]
- Shurraw, S.; Hemmelgarn, B.; Lin, M.; Majumdar, S.R.; Klarenbach, S.; Manns, B.; Bello, A.; James, M.; Turin, T.C.; Tonelli, M.; et al. Association between Glycemic Control and Adverse Outcomes in People with Diabetes Mellitus and Chronic Kidney Disease: A Population-Based Cohort Study. Arch. Intern. Med. 2011, 171, 1920–1927. [Google Scholar] [CrossRef] [Green Version]
- Huang, E.S.; Liu, J.Y.; Moffet, H.H.; John, P.M.; Karter, A.J. Glycemic Control, Complications, and Death in Older Diabetic Patients: The Diabetes and Aging Study. Diabetes Care 2011, 34, 1329–1336. [Google Scholar] [CrossRef] [Green Version]
- Doucet, J.A.; Bauduceau, B.; Le Floch, J.-P.; Verny, C.; The SFD/SFGG Intergroup. Medical Treatments of Elderly, French Patients with Type 2 Diabetes: Results at Inclusion in the GERODIAB Cohort. Fundam. Clin. Pharmacol. 2016, 30, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Franch-Nadal, J.; García-Gollarte, F.; Pérez Del Molino, A.; Orera-Peña, M.L.; de Miguel, M.R.; Melogno-Klinkas, M.; de Paz, H.D.; Aceituno, S.; Rodríguez-Fortúnez, P. Physicians’ and Pharmacists’ Clinical Considerations for Elderly Patients with Type 2 Diabetes Mellitus: The IMPLICA2 Study. Clin. Drug Investig. 2019, 39, 73–84. [Google Scholar] [CrossRef]
- Siaw, M.Y.L.; Ko, Y.; Malone, D.C.; Tsou, K.Y.K.; Lew, Y.-J.; Foo, D.; Tan, E.; Chan, S.C.; Chia, A.; Sinaram, S.S.; et al. Impact of Pharmacist-Involved Collaborative Care on the Clinical, Humanistic and Cost Outcomes of High-Risk Patients with Type 2 Diabetes (IMPACT): A Randomized Controlled Trial. J. Clin. Pharm. Ther. 2017, 42, 475–482. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pousinho, S.; Morgado, M.; Falcão, A.; Alves, G. Pharmacist Interventions in the Management of Type 2 Diabetes Mellitus: A Systematic Review of Randomized Controlled Trials. J. Manag. Care Spec. Pharm. 2016, 22, 493–515. [Google Scholar] [CrossRef] [PubMed]
- Van der Linden, L.; Decoutere, L.; Walgraeve, K.; Milisen, K.; Flamaing, J.; Spriet, I.; Tournoy, J. Combined Use of the Rationalization of Home Medication by an Adjusted STOPP in Older Patients (RASP) List and a Pharmacist-Led Medication Review in Very Old Inpatients: Impact on Quality of Prescribing and Clinical Outcome. Drugs Aging 2017, 34, 123–133. [Google Scholar] [CrossRef] [PubMed]
- Frier, B.M. Hypoglycaemia in Diabetes Mellitus: Epidemiology and Clinical Implications. Nat. Rev. Endocrinol. 2014, 10, 711–722. [Google Scholar] [CrossRef]
| Patient Characteristics | Statistics |
|---|---|
| Age (mean, standard deviation) | 81.7 ± 6 |
| Male (n, %) Female (n, %) | 42 (38.2%) 68 (61.8%) |
| Weight (mean, standard deviation) | 73.49 ± 14.6 |
| Kidney function (n = 108) a | |
| Serum creatinine (µmol/L) (mean, standard deviation) | 101.1 ± 78.6 |
| Creatinine clearance (mL/min) (mean, standard deviation) | 55.8 ± 20.6 |
| No CKD (n, %) | 7 (6.5%) |
| Mild CKD: creatinine clearance between 60 and 90 mL/min (n, %) | 35 (32.4%) |
| Moderate CKD: creatinine clearance between 30 and 60 mL/min (n, %) | 55 (50.9%) |
| Severe CKD: creatinine clearance < 30 mL/min (n, %) | 11 (10.2%) |
| Frailty (n = 109) b | |
| Fried score (median, (Q25, Q75)) | 3 [2; 4] |
| Fried frailty criteria b | |
| Weight loss (n, %) | 22 (20.0%) |
| Feelings of exhaustion (n, %) | 57 (52.3%) |
| Muscle weakness (n, %) | 90 (82.6%) |
| Reduced walking speed (n, %) | 64 (58.7%) |
| Sedentary lifestyle (n, %) | 87 (79.1%) |
| Falls (n = 107) c | |
| Yes (n, %) | 36 (33.6%) |
| Treatment | |
| Number of medications prescribed d (mean, standard deviation) | 8.2 ± 3.3 |
| Number of glucose-lowering medication (mean, standard deviation) | 1.4 ± 1.0 |
| Therapeutic strategy (n, %) | N (%) |
| Lifestyle changes only | 20 (18.2%) |
| Oral glucose-lowering drug only | 51 (46.4%) |
| 1 OGLD | 32 (29.1%) |
| 2 OGLDs | 17 (15.5%) |
| ≥3 OGLDs | 2 (1.8%) |
| Oral glucose-lowering drug + Insulin | 17 (15.5%) |
| 1 OGLD + Insulin | 9 (8.2%) |
| ≥ 2 OGLDs + Insulin | 8 (7.3%) |
| Insulin only | 22 (20.0%) |
| Types of Problems | n = 110 |
|---|---|
| According to EU(7) PIM List | |
| Long-acting sulphonylureas (glibenclamide, glimepiride) | 4 (3.6%) |
| Acarbose | 3 (2.7%) |
| Sliding-scale insulin | 5 (4.6%) |
| Contraindication | 2 (1.8%) |
| Overdose | |
| No adjustment to renal function | 20 (18.2%) |
| Medication used at excessively high dose | 10 (9.1%) |
| Underdose | 14 (12.7%) |
| Medication not indicated | |
| Overly tight glycemic control relative to glycemic targets | 22 (20.0%) |
| Pharmacological redundancy | 1 (0.9%) |
| Liraglutide in a patient over 75 years | 1 (0.9%) |
| Indication not treated or insufficiently treated | 4 (3.6%) |
| Hypoglycemia | 10 (9.1%) |
| Subtotal: patients with at least 1 DTP without taking into account Acarbose and Liraglutide | 66 (60.0%) |
| Total (patients with at least 1 DTP) | 67 (60.9%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mangé, A.-S.; Pagès, A.; Sourdet, S.; Cestac, P.; McCambridge, C. Diabetes and Frail Older Patients: Glycemic Control and Prescription Profile in Real Life. Pharmacy 2021, 9, 115. https://doi.org/10.3390/pharmacy9030115
Mangé A-S, Pagès A, Sourdet S, Cestac P, McCambridge C. Diabetes and Frail Older Patients: Glycemic Control and Prescription Profile in Real Life. Pharmacy. 2021; 9(3):115. https://doi.org/10.3390/pharmacy9030115
Chicago/Turabian StyleMangé, Anne-Sophie, Arnaud Pagès, Sandrine Sourdet, Philippe Cestac, and Cécile McCambridge. 2021. "Diabetes and Frail Older Patients: Glycemic Control and Prescription Profile in Real Life" Pharmacy 9, no. 3: 115. https://doi.org/10.3390/pharmacy9030115
APA StyleMangé, A.-S., Pagès, A., Sourdet, S., Cestac, P., & McCambridge, C. (2021). Diabetes and Frail Older Patients: Glycemic Control and Prescription Profile in Real Life. Pharmacy, 9(3), 115. https://doi.org/10.3390/pharmacy9030115






