Abstract
Although opioids are the cornerstone of moderate-to-severe acute pain management they are appropriately recognised as high-risk medicines. Patient and health service delivery factors can contribute to an increased risk of death associated with excessive sedation and respiratory impairment. Despite increasing awareness of opioid-induced ventilation impairment (OIVI), no reliable method consistently identifies individual characteristics and factors that increase mortality risk due to respiratory depression events. This study assessed similarities in available coronial inquest cases reviewing opioid-related deaths in Australian hospitals from 2010 to 2020. Cases included for review were in-hospital deaths that identified patient factors, clinical errors and service delivery factors that resulted in opioid therapy contributing to the death. Of the 2879 coroner’s inquest reports reviewed across six Australian states, 15 met the criteria for inclusion. Coroner’s inquest reports were analysed qualitatively to identify common themes, contributing patient and service delivery factors and recommendations. Descriptive statistics were used to summarise shared features between cases. All cases included had at least one, but often more, service delivery factors contributing to the death, including insufficient observations, prescribing/administration error, poor escalation and reduced communication. Wider awareness of the individual characteristics that pose increased risk of OIVI, greater uptake of formal, evidence-based pain management guidelines and improved documentation and observations may reduce OIVI mortality rates.
1. Introduction
While opioid medications provide a cornerstone for the management of acute moderate-to-severe pain, their ability to depress the central nervous system is well known. There are many adverse effects linked to opioid use ranging from side effects of nausea, vomiting and confusion to excessive sedation and respiratory depression potentially leading to increased morbidity and mortality. There are many terms used interchangeably when referring to “respiratory depression” including opioid-induced respiratory depression (ORID), opioid induced ventilatory impairment (OIVI) and opioid-related adverse events [1,2,3,4,5,6,7,8,9].
The Australian and New Zealand College of Anaesthetists and Faculty of Pain Management recommends OIVI as the most appropriate description, encompassing opioid-induced central respiratory depression (decreased respiratory drive), decreased level of consciousness (sedation) and upper airway obstruction [5]. Culminating in decreased ventilation and increased arterial carbon dioxide levels. The combination of hypoxia and hypercapnia commonly results in tachycardia and hypotension, before potential cardiorespiratory arrest, hypoxic encephalopathy and death if left untreated [10].
Challenges exist when attempting to study the prevalence of OIVI with varying definitions, dependent on outcome measures compared. A systemic literature review of postoperative patients demonstrated an incidence ranging from 0.04% when naloxone use was the outcome of interest, up to 41% if assessed by presence of hypoxaemia or bradypnoea [7]. Overall, the finding was that 0.5% of 841,424 total cases met the varying criteria for rescue management [7]. In another study, Jungquist et al. reported the incidence of opioid-induced respiratory depression in sentinel events to be <2% of all patients in hospital while on opioids [8]. Ramachandran et al. reported an incidence of 0.038% when measuring sudden-onset life-threatening respiratory events by studying patients found unresponsive while on analgesic therapy [11]. This has parallels with interpreting OIVI in the context of coroners’ reports as the measurement criteria is death.
It is clear that while there are benefits to providing adequate pain management with opioid analgesia, it comes with associated risks and possible mortality. There are lessons to be learnt from the cases that progress from “respiratory depression” to death. In Australia, the state coroners inquire into unexpected deaths in hospitals, with thorough investigations involving staff, family and evidence from expert witnesses regarding the surrounding circumstances. This gives a unique opportunity to evaluate such cases in the context of collating common themes associated with mortality and assessing the recommendations made by the coroner to minimise the risk of further opioid-related deaths.
The purpose of this review was to investigate in-hospital, opioid-related deaths across Australia, utilising publicly accessible coroner’s case reports. This review aims to identify in-hospital opioid-related deaths from which to gather similarities and lessons learnt to reduce opioid-related harm.
2. Materials and Methods
In May 2020, a retrospective review of publicly available coroner’s inquest case reports for deaths in Australia between 2010 and 2020 was conducted. Deaths occurring in the Australian Capital Territory and Victoria were excluded due to lack of public access and document word search ability, respectively. NSW and WA only had published records available from 2012 to 2020.
An excel spreadsheet was constructed with four columns. The first column had the particular state, then the relevant year under that (beginning at 2020), with each name pertaining to the inquest below that. A new year was added to separate groups of names. Each name had a column space next to it, from left to right, for whether an opioid was involved, a comment on the manner of death and a highlight space to insert a colour if the case was to be “flagged” for a comprehensive review. An example of the structure is attached in the Appendix A and Appendix B with de-identified data.
The coroner’s inquest reports can be accessed via the respective state government websites, which are linked in the Appendix A and Appendix B. Cases were opened and initially assessed for opioid involvement in five areas and in the following order for any mention of “opioid”, “pain”, “analgesia” or any opioid or opioid-related drug; key-/catchwords, manner and cause of death, case background and toxicology report. If any of these phrases were identified in those subsections, it was immediately flagged for a more comprehensive review later. If within the manner or cause of death, there was reference to “respiratory depression”, “drug toxicity”, “hypoxic brain injury” or “aspiration pneumonia”, these were reviewed at the time to assess whether opioids were involved in the care.
During this primary review, cases were excluded if the coroners themselves ruled, based upon all the available evidence, that opioids administered were not directly implicated in causing, hastening or significantly contributing to death. Cases were excluded if the subject was in custody at the time or if the inquest was a part of routine investigations for those under inpatient treatment orders. Cases were also excluded where opioid information was scarce and could not be determined as an important or relevant part of their pharmacological care. The remaining cases were then reviewed under the criteria that the death must have occurred in a hospital or affiliated treatment facility, such as in drug and alcohol rehabilitation units. Cases were then excluded from further review if the opioid or other drugs considered to contribute to the death were not administered/prescribed by hospital staff (self-administered without knowledge of staff, this does not include patient-controlled analgesia).
The complete coroner’s inquest reports that met inclusion criteria were analysed qualitatively to identify common themes, contributing factors and recommendations, with a focus on patient factors, avoidable clinical errors and health service delivery factors. Data were extracted using a standardised data collection spreadsheet. Descriptive statistics were used to summarise features shared between cases.
3. Results
From 2010 to 2020, across South Australia, New South Wales, Northern Territory, Queensland, Western Australia and Tasmania, there were 2879 coroner’s inquest reports available for public view. Of these, 132 (4.58%) involved opioids. Of cases where opioids were involved, the vast majority 94 cases (71.21%) occurred in the community, 10 (7.58%) occurred under police custody and five (3.79%) in aged-care facilities, these were excluded. A further three cases were excluded as the patients had self-administered additional opioids whilst admitted in hospital and an additional case was excluded after medications were self-administered at home prior to death once admitted to hospital. Of the remaining 19 cases, 4 were reviewed and discussed by all 3 authors, with a consensus that the opioid involvement was ambiguous as a cause of death and that other factors were more important in the coroner’s consideration, leading to minimal learning points or recommendations surrounding the safe use of opioid analgesia. Thus, a total of 15 met the inclusion criteria for analysis.
A summary of the patient demographics and comorbidities for the cases included in the review is presented in Table 1. Table 2 summarises the presenting complaints and preceding events, prior to the OIVI event for each case.

Table 1.
Coroner’s inquest report date, patient demographics and comorbidities.

Table 2.
Reason for admission, details of presenting complaint, death and events prior to opioid induced ventilatory impairment (OIVI).
Across the 15 cases included for detailed review and analysis, the age range was 23—88 years old, with a mean age of 55.7 (SD: 18.2) years and a median age of 54 years. Nine (60%) cases were male, and six (40%) were female. Nine (60%) cases were situated from the public hospital sector, and six (40%) were from private hospitals or associated facilities. There was a relatively even split between medical (40%), surgical (33.33%), mental health (13.33%), drug and alcohol (6.67%) and Emergency Department/Short Stay Unit (6.66%). From medical admissions, three (50%) occurred on general medical wards, two (33.33%) being palliative and one (16.67%) being neurology. Orthopaedics comprised 80% of surgical cases, with general surgery comprising 20%.
3.1. Time of Event
Between all cases, the incidence of the event appears skewed towards the first day (33.33%). For patients undergoing a procedure, the event was most likely to occur in the first 24 hours (60%) following the operation, with the remaining occurring on day 2 after the operation (40%). The length of time to event after surgery ranged between 8 and 48 h, with a mean time to event of 23.6 h and a standard deviation of 15.7 h.
3.2. Patient Comorbidities
The patients in six (40%) cases were reported to be overweight. Of the four (26.67%) who had a BMI reported, all were in the obese range with BMI greater than 38.1. A further two more (13.33%) were described as overweight in the reports without BMI documented.
Five (33.33%) cases had confirmed (three) or suspected (two) obstructive sleep apnoea. Six (40%) had some type of heart disease (including coronary artery or ischaemic heart disease and heart failure) and four (26.67%) had confirmed diabetes mellitus. Only one case (6.67%) reported either chronic lung disease (emphysema) or chronic kidney disease.
3.3. Contributing Opioids and Other Sedatives
Morphine was involved in seven cases (46.67%), while fentanyl was implicated in four cases (26.67%).
Of these six cases, three involved parenteral administration, two involved transdermal administration and one involved both parenteral and transdermal routes, as the transdermal opioid prescribed was intended for another patient. Pethidine was involved in two cases (13.33%). Two cases (13.33%) involved oxycodone immediate release and three (20%) involved oxycodone modified release, with these cases (20%) all involving use of a combination of long- and short-acting opioids. Hydromorphone was involved in two cases (13.33%), one being given to the wrong patient and one having an incorrect dose administered.
Two (13.33%) of the cases involved patient-controlled analgesia (PCA), with a further one having PCA disconnected (indwelling venous catheter tissued) in the hours prior to the event occurring.
Methadone was implicated in three (20%) cases; in two cases, methadone was indicated for opioid substitution therapy (OST) and, in one case (6.67%), it was prescribed for the management of acute pain. A further case (6.67%) involved buprenorphine prescribed for OST. All three cases pertaining to OST involved a combination of opioids of benzodiazepines and/or antipsychotics.
Benzodiazepines were documented to have been administered in five of the cases (33.33%) with a further case reporting a benzodiazepine in the blood toxicology report. Gabapentinoids and antipsychotics were both prescribed in three cases (20%), while antihistamines and sedating antidepressants were prescribed in two cases (13.33%). Overall, eight (53.33%) of the cases had a co-prescribed sedating medication, with five (33.33%) of these cases involving a combination of one or more of the above medications.
Table 3 provides a comprehensive description of the opioids used (including route and dose) and co-prescribed sedating agents involved in the included cases.

Table 3.
Opioids involved, route of administration, dose and co-prescribed sedating agents involved in included coroners’ cases.
3.4. Health Service Delivery Factors
Four broad categories of service delivery factors contributed to the opioid-related deaths in the cases emerged upon review. These related to prescribing or administration issues, observations, escalation procedures and communication. Table 4 contains a summary of the service delivery factor subcategories and which cases had evidence of these embedded within.

Table 4.
Common health service delivery factors identified across all included coroners’ cases and grouped into subthemes.
Amongst the 15 cases, 12 (80%) had a prescribing or administration issue. Seven cases (46.67%) reported uncertainty presented by the coroner, colleagues or expert witnesses surrounding the appropriateness of the dose prescribed. Five cases (33.33%) identified local policies or procedures that required updating. Four cases (26.67%) included a scenario where there was a lack of awareness surrounding being prescribed multiple opioids together or in combination with sedative medications such as benzodiazepines or antihistamines. Two cases (13.33%) involved giving the wrong patient the wrong medication, one being prescribed incorrectly and one administered incorrectly. Two further cases (13.33%) involved a dose calculation error, one both in prescribing and administering the opioid.
Twelve cases (80%) reported issues with observations. Eight cases (53.33%) highlighted instances of insufficient monitoring or observations. Six cases (40%) reported instances of insufficient documentation of observations and vital signs. Six cases (40%) included failure to increase the level of observations once deterioration or concern was identified.
Eleven cases (73.33%) involved issues with escalation procedures. Nine cases (60%) included inadequate knowledge from hospital staff surrounding early clinical signs of deterioration. Six cases (40%) included a failure to escalate appropriately once deterioration was identified. Eight cases (53.33%) failed to involve an anaesthetist or seek out an expert pain management review when required.
Ten cases (66.67%) involved communication issues. Six cases (40%) included a lack of clear instructions to other staff. Five cases (33.33%) consisted of instances of inadequate notification of clinical deterioration or other concerns. Five cases (33.33%) consisted of poor communication amongst the health professionals working at the time. Three cases (20%) involved poor handover practices, and another three included consisted of instances of poor communication about patients’ contributing risk factors for respiratory depression.
Table 5 summarises recommendations and themes for improvement made by the coroners, stratified into categories.

Table 5.
Coroners’ recommendations and themes for improvement stratified into categories.
4. Discussion
This paper summarises the deaths of 15 individuals, in which opioid medications were implicated. These cases represent a heterogenous group of patients; however, they share similar thematic undercurrents. While this study is not powered to draw statistically significant conclusions, it can be used in conjunction with similar studies worldwide to demonstrate important factors that need to be considered when prescribing and caring for patients receiving opioid medications to improve safety [2,4,7,8,12,13].
The period immediately following surgery appears to represent a time of elevated risk for OIVI. From the literature, proximity to surgery was overwhelmingly involved with greater than 85% of all deaths occurring within 24 h of surgery [9,12]. This correlates somewhat with our data, with 60% of the events occurring within the first 24 h after the procedure and the remaining postsurgical events occurring the following day. This could be due to medical professionals’ awareness of increased mortality within 24 h after surgery and, therefore, compensating by being hypervigilant.
Studies have consistently shown statistically significant increased risk of postoperative OIVI in patients with pre-existing cardiac and pulmonary disease, as well as those with obstructive sleep apnoea (OSA) [7]. This was partially reflected in our cohort, particularly for cardiac disease and OSA, with 40% and 33.33% of all cases having these comorbidities, respectively. This increased to 60% of all surgical cases having either, with 40% of surgical cases having both OSA and cardiac disease. Only one patient, who was a postoperative case, had concurrent pulmonary disease. While only three of the five OSA cases had been formally diagnosed, they were included as the coroners had deemed them likely to have undiagnosed OSA. These patients with undiagnosed OSA had a BMI of 38 or above. In one study, 59% of chronic opioid users had evidence of previously undiagnosed OSA when undergoing polysomnography [14]. Thus, given the associated risk, timely screening and testing for OSA, particularly in cases with high a BMI could improve safety when prescribing opioids. In a study by Rao and Khanna, it has been noted that while there are assessment tools for OSA and respiratory impairment, such as the STOP-Bang questionnaire, ARISCAT and SPORC, each has its limitations, and a method to stratify all patients who may develop OIVI remains elusive [15].
The effect of OIVI is increased following co-administration of benzodiazepines [16]. Overdose deaths in patients co-prescribed opioids and benzodiazepines has been shown to be 9–10 times that of patients prescribed opioids alone [17]. The combination of opioids and gabapentinoids (gabapentin and pregabalin) have also been shown to have a lesser, but ongoing additional risk on mortality when co-prescribed with opioids [18]. Amongst our findings, benzodiazepines were involved in six (40%) of cases. Admittedly, only one of these cases listed the benzodiazepine as the only co-prescribed sedating agent, the others contained a mix of antipsychotics (three), a gabapentinoid (one) or an antihistamine (one), highlighting the need to review the total sedative load to assess and minimise the risk of OIVI.
In response to these cases, the coroners made recommendations promoting broader awareness of the inherent risk of respiratory depression in patients receiving opioid analgesia. Recommendations were made surrounding opioid prescribing as concerns relating to the prescribing process were raised in 80% of the cases. These recommendations encompassed dose, dosing intervals and routes, such as transdermal fentanyl patch prescription being limited to pain treatment specialists and not used to manage acute pain. Additionally, prescribers should be aware of previous opioid use (or naivety) and concurrent sedating medications as discussed above. Dependent on the hospital or health system, recommendations to improve safety have involved; standardising protocols for age-appropriate opioid prescribing, increased clinical education, availability of specialised acute pain teams, new acute pain charts and protocols implemented to improve monitoring and detect deterioration. A study by Lee, Caplan and Stephens found that 97% of opioid-induced respiratory depression that resulted in death or severe brain injury could be prevented by adjustments in medication administration or enhanced monitoring [12].
Concern with level of observation was noted in 80% of cases, with insufficient monitoring highlighted in 53.33%. Monitoring for OIVI can include sedation score, respiratory rate and oxygen saturation. In a study monitoring postoperative oxygen saturations continuously, it was found that not only was reduced oxygen saturation common in those receiving opioids, with 20% of all patients experiencing SpO2 <90% for >10 min per hour, but that 90% of prolonged hypoxic events (SpO2 < 90% for ≥1 h) were frequently missed on routine (4 hourly) nursing reviews [19]. This was also highlighted in another study that showed a benefit of having continuous pulse oximetry with centralised alarms [20]. In our cohort, in many cases focus was placed on lack of nursing reviews assessing these factors; however, it has been previously shown that up to a third of OIVI events occur within an hour from the last medical review [12]. Moving forward, improved techniques of monitoring could be utilised to minimise the occurrence and risks associated with OIVI. Other electronic monitoring devices for high-risk patients, such as monitoring end-tidal CO2 and minute ventilation can detect events before SpO2 falls and OIVI becomes clinically evident [4,8].
Another common theme across the cases reviewed was inadequate recognition of signs of deterioration by clinical staff (occurred in 60% of cases) and failing to escalate or increase observations when deteriorations were detected (occurred in 33.33% of cases). General communication issues were highly prevalent, identified in 76.67% of our cohort. Some of the recommendations suggest increased use of guidelines/protocols, with structured systems for patient monitoring and availability of avenues for escalation when required.
In future, novel opioid development could target the provision of potent analgesia whilst minimalising respiratory depression, utilising co-administration of respiratory stimulants potentially reducing OIVI events [21].
5. Limitations
It is important to note that the coroner’s reports are legal documents pertaining to the narratives surrounding an unsuspected death. They do not contain vivid or succinct medical notes, and itis not possible or wise to draw conclusions beyond those stated in the report. In many cases, particularly the monothematic cases such as where the incorrect doses were given, patient factors, details and other service delivery factors were absent. For instance, only one patient had documented renal disease; however, with many cases complicated by hypertension and heart disease, the incidence of this could be assumed to be much higher. Similarly, BMIs, smoking status, full medication lists and total opioid doses administered were incomplete. Another limitation of this study is its small sample size of 15 cases.
6. Conclusions
Wider awareness of the individual characteristics that pose an increased risk of OIVI, greater uptake of formal, evidence-based pain management guidelines, improved communication, observations and more appropriate escalation of care may reduce OIVI mortality rates.
Author Contributions
Conceptualisation, B.K. and J.L.J.; methodology, B.K., N.S. and J.L.J.; data extraction and analysis, B.K. and N.S.; writing—original draft preparation, B.K. and N.S.; writing—review and editing, B.K., N.S. and J.L.J. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A
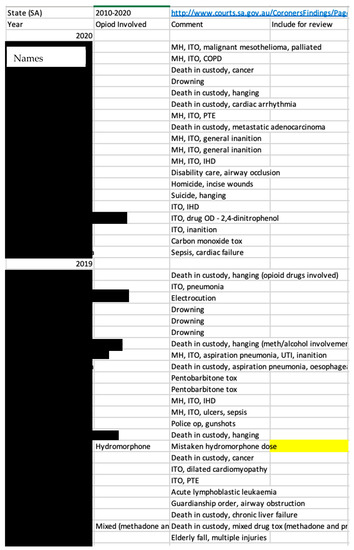
Figure A1.
Example of the excel spreadsheet design used to track coroner’s cases to include for review. Below, the URL’s for websites used to access public coroner’s reports.
Appendix B

Table A1.
References for Coroner’s Reports for each State/Territory.
Table A1.
References for Coroner’s Reports for each State/Territory.
| State/Territory | Coroner’s Reports |
|---|---|
| The State of Queensland (Queensland Courts) | https://www.courts.qld.gov.au/courts/coroners-court/findings (accessed on 15 May 2020) |
| Government of New South Wales (Coroners Court) | http://www.coroners.justice.nsw.gov.au/Pages/findings.aspx (accessed on 15 May 2020) |
| Government of Tasmania (Magistrates Court of Tasmania—Coronial Division). | https://www.magistratescourt.tas.gov.au/about_us/coroners (accessed on 15 May 2020) |
| Government of South Australia, Courts Administration Authority of South Australia (Coroners Court) | http://www.courts.sa.gov.au/CoronersFindings/Pages/default.aspx (accessed on 15 May 2020) |
| Northern Territory Government of Australia (Department of Attorney-General and Justice) | https://justice.nt.gov.au/attorney-general-and-justice/courts/coroners-findings (accessed on 15 May 2020) |
| Government of Western Australia (Coroner’s Court of Western Australia) | https://www.coronerscourt.wa.gov.au/I/inquest_findings.aspx?uid=6256-4150-5-7479 (accessed on 15 May 2020) |
References
- Lorri, A.L.; Karen, L.P.; Karen, B.D. We should focus on “when” as well as “whom” to monitor for postoperative opioid-induced ventilatory impairment. APSF Newslett. 2018, 31, 59–63. [Google Scholar]
- Overdyk, F.; Dahan, A.; Roozekrans, M.; Der Schrier, R.V.; Aarts, L.; Niesters, M. Opioid-induced respiratory depression in the acute care setting: A compendium of case reports. Pain Manag. 2014, 4, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Jungquist, R.C.; Smith, W.K.; Nicely, C.K.L.; Polomano, C.R. Monitoring hospitalized adult patients for opioid-induced sedation and respiratory depression. Am. J. Nurs. 2017, 117 (Suppl. 1), S27–S35. [Google Scholar] [CrossRef] [PubMed]
- Khanna, A.K.; Bergese, S.D.; Jungquist, C.R.; Morimatsu, H.; Uezono, S.; Lee, S.; Ti, L.K.; Urman, R.D.; McIntyre, R., Jr.; Tornero, C.; et al. Prediction of opioid-induced respiratory depression on inpatient wards using continuous capnography and oximetry: An international prospective, observational trial. Anesth. Analg. 2020, 131, 1012–1024. [Google Scholar] [CrossRef] [PubMed]
- Macintyre, P.E.; Loadsman, J.A.; Scott, D.A. Opioids, ventilation and acute pain management. Anaesth. Intensive Care 2011, 39, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Partridge, A. Predicting Risk for Opioid-induced Sedation and Respiratory Depression in Hospitalized Patients. Ph.D. Thesis, Walden University, Ann Arbor, MI, USA, 2019. [Google Scholar]
- Gupta, K.; Nagappa, M.; Prasad, A.; Abrahamyan, L.; Wong, J.; Weingarten, T.N.; Chung, F. Risk factors for opioid-induced respiratory depression in surgical patients: A systematic review and meta-analyses. BMJ Open 2018, 8, e024086. [Google Scholar] [CrossRef] [PubMed]
- Jungquist, C.R.; Chandola, V.; Spulecki, C.; Nguyen, K.V.; Crescenzi, P.; Tekeste, D.; Sayapaneni, P.R. Identifying patients experiencing opioid-induced respiratory depression during recovery from anesthesia: The Application of electronic monitoring devices. Worldviews Evid. Based Nurs. 2019, 16, 186–194. [Google Scholar] [CrossRef] [PubMed]
- Gupta, K.; Prasad, A.; Nagappa, M.; Wong, J.; Abrahamyan, L.; Chung, F.F. Risk factors for opioid-induced respiratory depression and failure to rescue: A review. Curr. Opin. Anaesthesiol. 2018, 31, 110–119. [Google Scholar] [CrossRef] [PubMed]
- Khanna, A.K.; Overdyk, F.J.; Greening, C.; Di Stefano, P.; Buhre, W.F. Respiratory depression in low acuity hospital settings–Seeking answers from the PRODIGY trial. J. Crit. Care 2018, 47, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Ramachandran, S.K.; Haider, N.; Saran, K.A.; Mathis, M.; Kim, J.; Morris, M.; O’Reilly, M. Life-threatening critical respiratory events: A retrospective study of postoperative patients found unresponsive during analgesic therapy. J. Clin. Anesth. 2011, 23, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Lee, L.; Caplan, R.; Stephens, L.; Posner, K.; Terman, G.; Voepel-Lewis, T.; Domino, K.B. Postoperative opioid-induced respiratory depression a closed claims analysis. Anesthesiology 2014, 122, 659–665. [Google Scholar] [CrossRef] [PubMed]
- Gordon, D.B.; Pellino, T.A. Incidence and characteristics of naloxone use in postoperative pain management: A critical examination of naloxone use as a potential quality measure. Pain Manag. Nurs. 2005, 6, 30–36. [Google Scholar] [CrossRef] [PubMed]
- Chung, F.; Wong, J.; Bellingham, G.; Lebovic, G.; Singh, M.; Waseem, R.; Peng, P.; George, C.F.P.; Furlan, A.; Bhatia, A.; et al. Predictive factors for sleep apnoea in patients on opioids for chronic pain. BMJ Open Respir. Res. 2019, 6, e000523. [Google Scholar] [CrossRef] [PubMed]
- Rao, V.K.; Khanna, A.K. Postoperative respiratory impairment is a real risk for our patients: The intensivist’s perspective. Anesthesiol. Res. Pract. 2018, 2018, 3215923. [Google Scholar] [CrossRef] [PubMed]
- Xu, L.; Chockalingam, A.; Stewart, S.; Shea, K.; Matta, M.K.; Narayanasamy, S.; Polli, N.R.; Volpe, D.A.; Weaver, J.; Zhu, H.; et al. Developing an animal model to detect drug–drug interactions impacting drug-induced respiratory depression. Toxicol. Rep. 2020, 7, 188–197. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, N.; Funk, M.J.; Proescholdbell, S.; Hirsch, A.; Ribisl, K.M.; Marshall, S. Cohort study of the impact of high-dose opioid analgesics on overdose mortality. Pain Med. 2015, 17, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Macleod, J.; Steer, C.; Tilling, K.; Cornish, R.; Marsden, J.; Millar, T.; Strang, J.; Hickman, M. Prescription of benzodiazepines, z-drugs, and gabapentinoids and mortality risk in people receiving opioid agonist treatment: Observational study based on the UK Clinical Practice Research Datalink and Office for National Statistics death records. PLoS Med. 2019, 16, e1002965. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Sessler, D.I.; Dalton, J.E.; Devereaux, P.; Shahinyan, A.; Naylor, A.J.; Hutcherson, M.T.; Finnegan, P.S.; Tandon, V.; Darvish-Kazem, S.; et al. Postoperative hypoxemia is common and persistent. Anesth. Analg. 2015, 121, 709–715. [Google Scholar] [CrossRef] [PubMed]
- Taenzer, A.H.; Pyke, J.B.; McGrath, S.P.; Blike, G.T. Impact of pulse oximetry surveillance on rescue events and intensive care unit transfers. Anesthesiology 2010, 112, 282–287. [Google Scholar] [CrossRef] [PubMed]
- Imam, M.Z.; Kuo, A.; Smith, M.T. Countering opioid-induced respiratory depression by non-opioids that are respiratory stimulants. F1000Research 2020, 9, 91. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).