The Association between Medication Experiences and Beliefs and Low Medication Adherence in Patients with Chronic Disease from Two Different Societies: The USA and the Sultanate of Oman
Abstract
1. Introduction
1.1. Significance
1.2. Innovation
1.3. Study Objective
- Do medication experiences and beliefs affect medication adherence?
- Do relationships between medication adherence and medication experiences and beliefs vary from one nation to another?
2. Methodology
2.1. Overview
2.2. Design and Sample
- A.
- Secondary data analysis: The United States
- B.
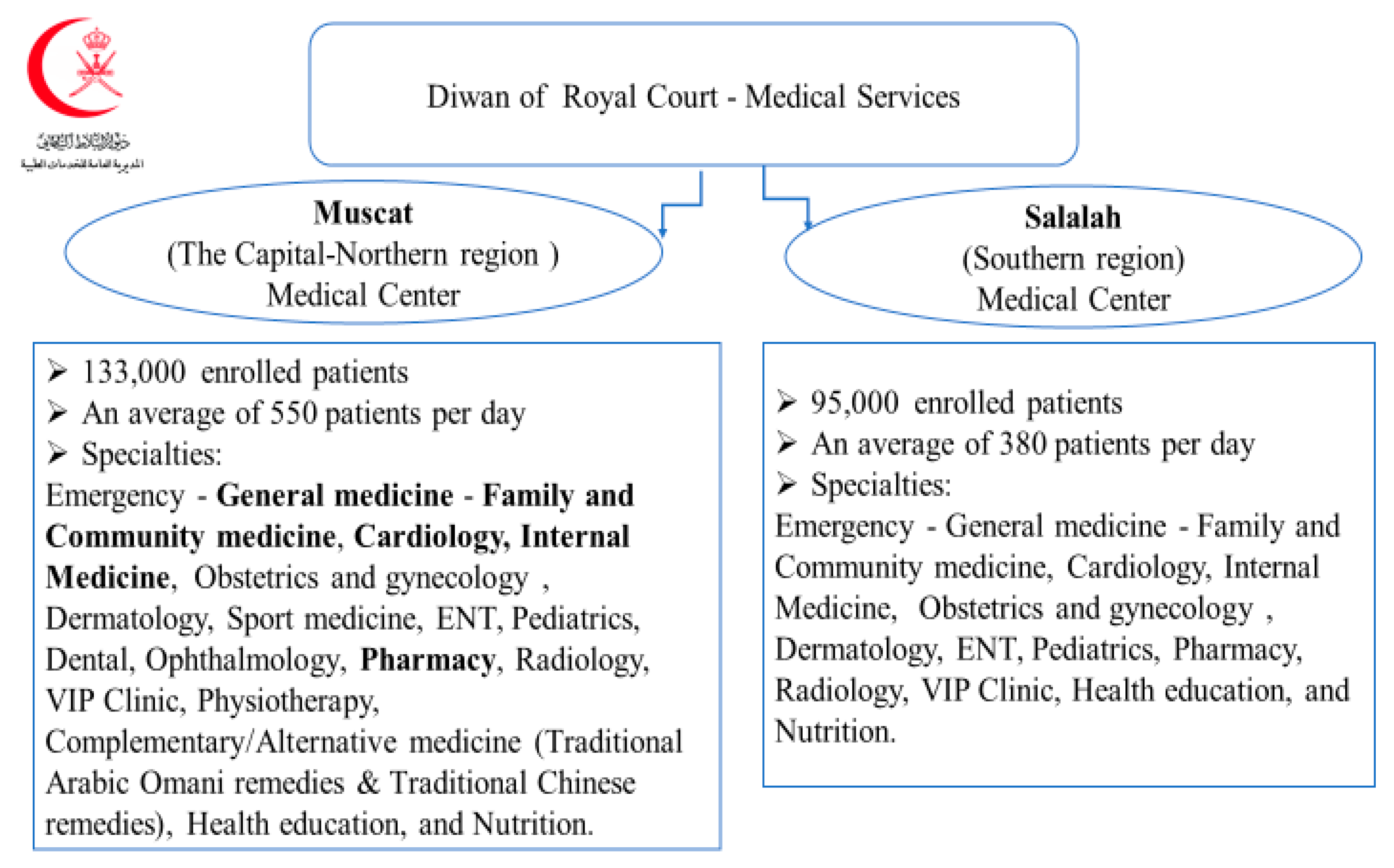
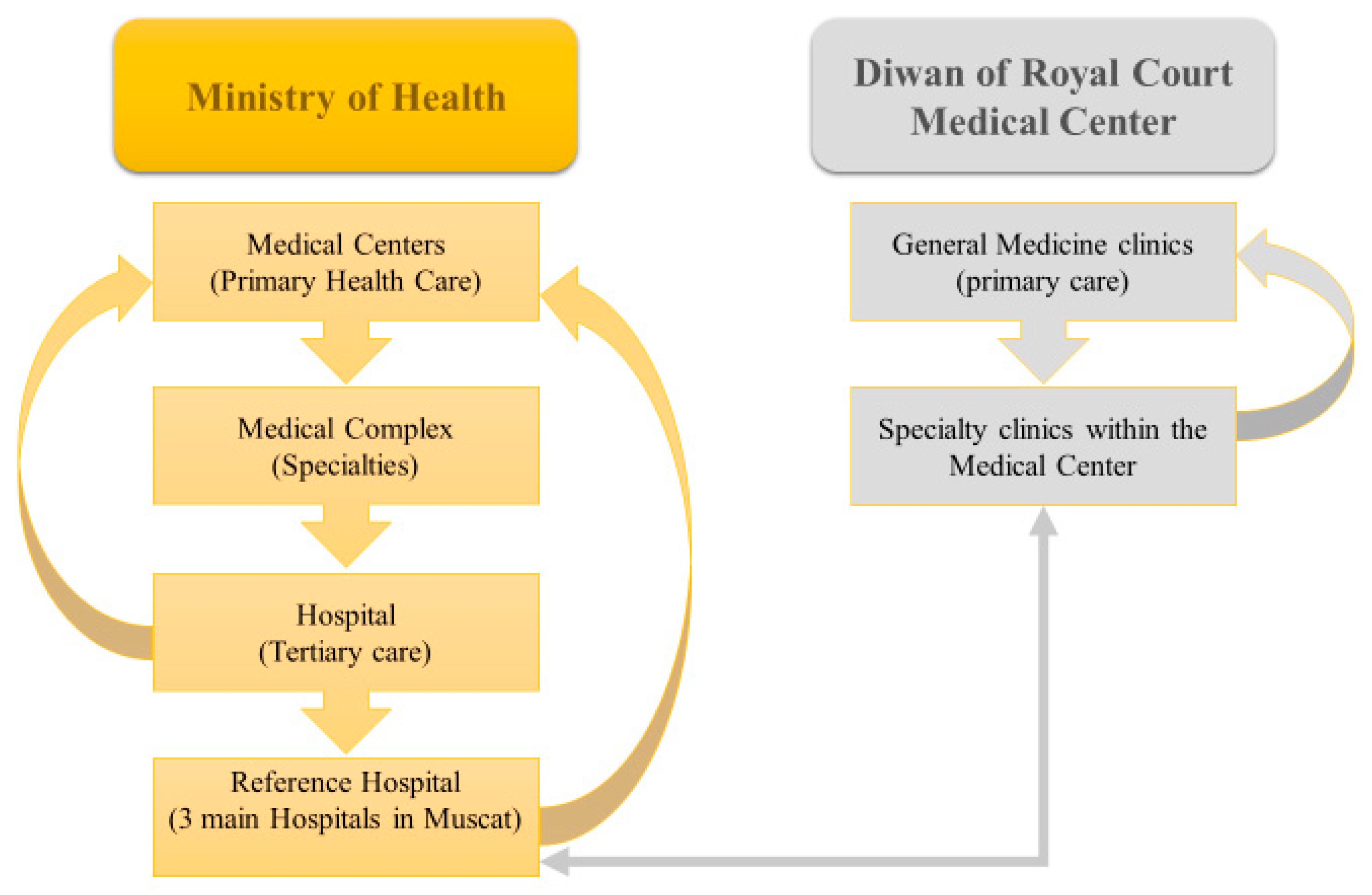
- Data collection from a different population: The Sultanate of Oman
- I.
- Sampling Frame
- II.
- Sampling Method
- III.
- Sample Size
- IV.
- Inclusion Criteria
- V.
- Exclusion Criteria
- VI.
- Process for Survey Development, Translation, and Data Collection
- (a)
- Survey development process (Supplementary Material 1: Developed Survey)
- The same variables (see Study Measures section) used in the secondary analysis were selected and a new survey was developed.
- Element writing guidelines [43] and social exchange theory were applied to reduce the social desirability bias, reduce the measurement error, and increase the response rate.
- The survey was reviewed by measurement expert Dr. Michael C. Rodriguez, a Professor of Quantitative Methods in Education, Campbell Leadership Chair in Education and Human Development, and Co-Director of the Educational Equity Resource Center at the Educational Psychology University of Minnesota. The measurement expert review aimed to ensure that the survey was well presented, increasing the response rate and reducing measurement errors.
- The following copyright footnote was added in Arabic at the end of each page of the survey:
- (b)
- Arabic translation process
- The translation was done through a forward–backward translation process to ensure the questions were translated correctly. This process was performed by three individuals who speak Arabic from the Sultanate of Oman and who obtained their bachelor’s and master’s degrees from Western universities in English. The first person did the forward translation and then sent it to the second person who did the back translation. The third person was the investigator who modified the final version of the translation.
- Finally, the “think aloud” process was applied by two Arabic speakers to ensure that questions were answered correctly and that participants could understand and follow the instructions correctly (Supplementary Material 2: Arabic Translated Survey).
- A pilot study of the first 80 paper survey sets was distributed at the three clinics and in the pharmacy waiting area. Some adjustments were made to the formatting and language of the questions. These adjustments reduced the number of unanswered questions and increased the overall response rate (for more details, see Data Collection Process).
- (c)
- Oman approval process
- (d)
- Data Collection process
- The first 80 paper survey sets were distributed at the three clinics and the pharmacy waiting area as a pilot project. The nurse in charge of each clinic distributed paper scanning kits with pens to patients in the waiting area after completing the screening. In this pilot survey, 68 responders only answered the first few questions, and many others did not answer any questions at all. Therefore, each clinic’s nurses were asked to verify that the patient upon delivery answered all survey questions;
- Many participants could not write or read, resulting in a lower response rate at the beginning of the data collection process. Therefore, three pharmacists and three nurses were appointed to assist any illiterate patient who was not accompanied by educated relatives. One pharmacist and one nurse were assigned to the Internal Medicine Clinic and the same in the General Medicine Clinic. Only one nurse was assigned to the Cardiology Clinic, as few patients were attending this clinic and it was open only twice a week. One pharmacist was also assigned in the pharmacy waiting area for any patient who may have missed the clinic’s questionnaire;
- In the first week of the process, about 74 responses were discarded because participants missed many questions of the MMAS-8 questions. The investigator made some adjustments to the formatting and language of the questions. These adjustments reduced the number of unanswered questions and increased the overall response rate;
- To ensure that the required sample size (500 or more) was obtained, the researcher examined daily the number of responses collected and how many were actually valid during the data collection period;
- Finally, 776 responses were collected between 16 June and 16 August 2019. However, 714 responses were accepted and entered into the SPSS software program. Sixty-two responses were excluded because: 28 questions relating to the “MMAS-8” were not answered, twenty-three responses did not have a chronic disease, and eleven participants did not respond to half of the survey. The missing data were excluded from the study.
- (e)
- Data Quality Control
2.3. IRB Approval (Exemption/Non-Human Subject Criteria)
2.4. Study Measures (Variables)
- (a)
- Chronic Diseases
- Have you ever had any of the following chronic diseases, either now or in the past?
| NO | Yes | |
| Heart disease? | ||
| Diabetes? | ||
| Breathing problems? | ||
| Arthritis? | ||
| Cancer? | ||
| Stroke? | ||
| Obesity? | ||
| Hypothyroidism? | ||
| High Cholesterols Level | ||
| Others? |
- Please list, if any, other chronic diseases you may have and not mentioned above:
- (b)
- Medication Adherence
| Medication Adherence | Score |
| Low adherence | 0 to less than 6 |
| Moderate adherence | 6 to less than 8 |
| High adherence | 8 |
| 1. | Do you sometimes forget to take your pills? | Yes | No |
| 2. | People sometimes miss taking their medications for reasons other than forgetting. Thinking over the past two weeks, were there any days when you did not take your medicine? | ||
| 3. | Have you ever cut back or stopped taking your medicine without telling your doctor because you felt worse when you took it? | ||
| 4. | When you travel or leave home, do you sometimes forget to bring along your medicine? | ||
| 5. | Did you take all your medicine yesterday? | ||
| 6. | When you feel like your symptoms are under control, do you sometimes stop taking your medicine? | ||
| 7. | Taking medicine every day is a real inconvenience for some people. Do you ever feel hassled about sticking to your treatment plan? | ||
| 8. | How often do you have difficulty remembering to take all your medicine? |
- (c)
- (d)
- Demography and other factors (age, gender, ethnicity or race, and education). Each factor was analyzed separately to measure its effect on medication adherence:
2.5. Data Analysis Plan
2.5.1. Descriptive Statistics
2.5.2. Addressing Major Research Questions
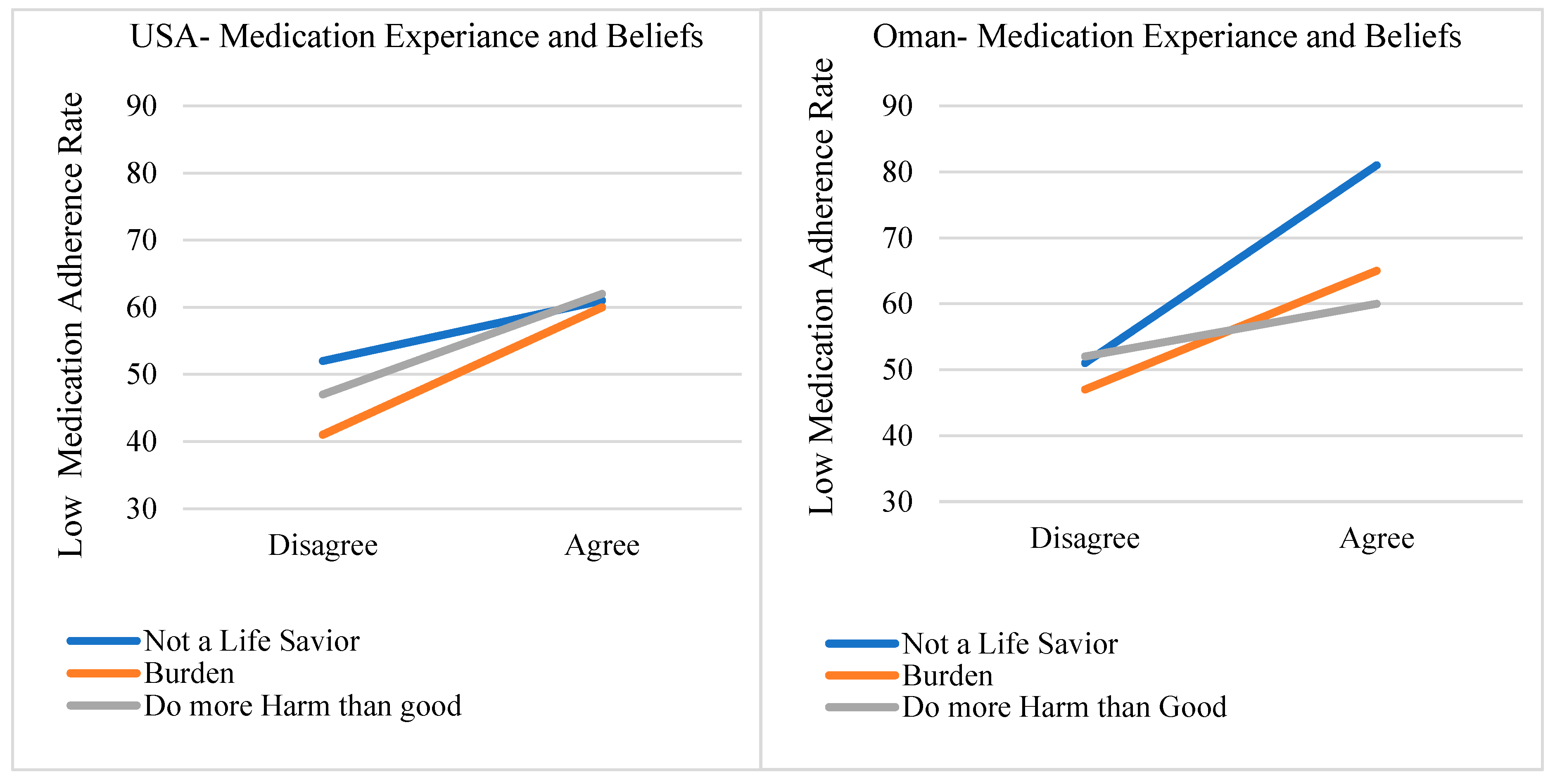
- Do medication experiences and beliefs affect medication adherence? The three variables were used to measure medication experiences and the mean Morisky Medication Adherence Scale (MMAS-8) score was used to measured medication adherence.Chi-square analysis with p-values of less than 0.05 was also conducted to describe the relationship between the medication experiences and beliefs and the outcome of interest (low medication adherence (MMAS-8 < 6)) in chronic disease participants.Note: The participants’ opinions varied for each statement, between agreeing or disagreeing, whether their medication adherence was low or high. This study focused on the low medication adherence participants (MMAS-8 scores from 0 to less than 6).
- Do relationships between medication adherence and medication experiences and beliefs vary from one nation to another? A simple comparison between the percentages of the Omani and U.S. populations’ medication adherence based each country’s medication experiences and beliefs statement.
3. Results
3.1. Descriptive Findings
3.2. The Association of Medication Experiences and Beliefs with Low Medication Adherence
4. Discussion
Study Limitations
5. Conclusions
5.1. Study Implications
5.2. Future Research
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adherence to Long-Term Therapies: Evidence for Action, Section I. Available online: https://www.who.int/chp/knowledge/publications/adherence_Section1.pdf (accessed on 27 January 2021).
- Aronson, J.K. Compliance, Concordance, Adherence. Br. J. Clin. Pharmacol. 2007, 63, 383–384. [Google Scholar] [CrossRef] [PubMed]
- Osterberg, L.; Blaschke, T. Adherence to Medication. N. Engl. J. Med. 2005, 353, 487–497. [Google Scholar] [CrossRef] [PubMed]
- Definitions, Meanings, Synonyms, and Grammar by Oxford Dictionary on Lexico.Com. Available online: https://en.oxforddictionaries.com/definition/adherence (accessed on 15 January 2021).
- McGuire, M.; Iuga, A.O. Adherence and Healthcare Costs. Risk Manag. Healthc. Policy 2014, 7, 35–44. [Google Scholar] [CrossRef] [PubMed]
- National Health Council. About Chronic Disease. Available online: https://nationalhealthcouncil.org/wp-content/uploads/2019/12/AboutChronicDisease.pdf (accessed on 15 January 2021).
- Centers for Disease Control and Prevention. National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), Chronic Disease in America. Available online: https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm (accessed on 15 January 2021).
- Raghupathi, W.; Raghupathi, V. An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach to Public Health. Int. J. Environ. Res. Public Health 2018, 15, 431. [Google Scholar] [CrossRef]
- Prescription Drug Spending in the, U.S. Healthcare System. Available online: https://www.actuary.org/content/prescription-drug-spending-us-health-care-system (accessed on 15 January 2021).
- Lam, W.Y.; Fresco, P. Medication Adherence Measures: An Overview. Biomed. Res. Int. 2015, 2015, 217047. [Google Scholar] [CrossRef]
- Briesacher, B.A.; Andrade, S.E.; Fouayzi, H.; Chan, K.A. Comparison of Drug Adherence Rates among Patients with Seven Different Medical Conditions. Pharmacotherapy 2008, 28, 437–443. [Google Scholar] [CrossRef]
- Haynes, R.B.; McDonald, H.P.; Garg, A.X. Helping Patients Follow Prescribed Treatment: Clinical Applications. JAMA 2002, 288, 2880–2883. [Google Scholar] [CrossRef]
- Cramer, J.A.; Spilker, B. Patient Compliance in Medical Practice and Clinical Trials; Raven Press: New York, NY, USA, 1991. [Google Scholar]
- Reed, M.; Brand, R.; Newhouse, J.P.; Selby, J.V.; Hsu, J. Coping with Prescription Drug Cost Sharing: Knowledge, Adherence, and Financial Burden. Health Serv. Res. 2008, 43, 785–797. [Google Scholar] [CrossRef]
- Schommer, J. National Consumer Survey on the Medication Experience and Pharmacists. Roles 2016, 102. Available online: https://www.pharmacy.umn.edu/sites/pharmacy.umn.edu/files/the-2015-national-consumer-survey-on-the-medication-experience-and-pharmacists-roles.pdf (accessed on 3 February 2021).
- Schommer, J.C.; Worley, M.M.; Kjos, A.L. Decision-Making during Initiation of Medication Therapy. Res. Social Adm. Pharm. 2014, 10, 313–327. [Google Scholar] [CrossRef]
- Shoemaker, S.J.; Ramalho de Oliveira, D.; Alves, M.; Ekstrand, M. The Medication Experience: Preliminary Evidence of Its Value for Patient Education and Counseling on Chronic Medications. Patient Educ. Couns. 2011, 83, 443–450. [Google Scholar] [CrossRef] [PubMed]
- Collins, F.S.; Varmus, H. A New Initiative on Precision Medicine. N. Engl. J. Med. 2015, 372, 793–795. [Google Scholar] [CrossRef] [PubMed]
- Shoemaker, S.J.; Ramalho de Oliveira, D. Understanding the Meaning of Medications for Patients: The Medication Experience. Pharm. World Sci. 2008, 30, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Al-Noumani, H.; Wu, J.-R.; Barksdale, D.; Alkhasawneh, E.; Knafl, G.; Sherwood, G. Relationship between Medication Adherence and Health Beliefs among Patients with Hypertension in Oman: Pilot Study. Sultan Qaboos Univ. Med. J. 2017, 17, e329. [Google Scholar] [CrossRef]
- Al-Noumani, H.; Wu, J.-R.; Barksdale, D.; Knafl, G.; AlKhasawneh, E.; Sherwood, G. Health Beliefs and Medication Adherence in Omanis with Hypertension. J. Cardiovasc. Nurs. 2018, 33, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Travers, R.; Huth, E.J.; Murray, T.J. Medicine in Quotations: Views of Health and Disease through the Ages. Health Hist. 2006, 8, 183. [Google Scholar] [CrossRef]
- Cramer, J.; Rosenheck, R.; Kirk, G.; Krol, W.; Krystal, J.; VA Nalterxone Study Group 425. Medication Compliance Feedback and Monitoring in a Clinical Trial: Predictors and Outcomes. Value Health 2003, 6, 566–573. [Google Scholar] [CrossRef]
- Benner, J.S.; Glynn, R.J.; Mogun, H.; Neumann, P.J.; Weinstein, M.C.; Avorn, J. Long-Term Persistence in Use of Statin Therapy in Elderly Patients. JAMA 2002, 288, 455–461. [Google Scholar] [CrossRef]
- MedicineNet. Definition of Chronic Disease. Available online: https://www.medicinenet.com/chronic_disease/definition.htm (accessed on 15 January 2021).
- Schlenk, E.A.; Burke, L.E.; Rand, C. Behavioral Strategies to Improve Medication-Taking Compliance; Futura Publishing Co: Armonk, NY, USA, 2001; pp. 57–70. [Google Scholar]
- Coleman, C.I.; Limone, B.; Sobieraj, D.M.; Lee, S.; Roberts, M.S.; Kaur, R.; Alam, T. Dosing Frequency and Medication Adherence in Chronic Disease. J. Manag. Care Pharm. 2012, 18, 527–539. [Google Scholar] [CrossRef]
- Denollet, J.; Sys, S.U.; Stroobant, N.; Rombouts, H.; Gillebert, T.C.; Brutsaert, D.L. Personality as Independent Predictor of Long-Term Mortality in Patients with Coronary Heart Disease. Lancet 1996, 347, 417–421. [Google Scholar] [CrossRef]
- Tedla, Y.G.; Bautista, L.E. Drug Side Effect Symptoms and Adherence to Antihypertensive Medication. Am. J. Hypertens. 2016, 29, 772–779. [Google Scholar] [CrossRef]
- Zachariae, R.; Pedersen, C.G.; Jensen, A.B.; Ehrnrooth, E.; Rossen, P.B.; von der Maase, H. Association of Perceived Physician Communication Style with Patient Satisfaction, Distress, Cancer-Related Self-Efficacy, and Perceived Control over the Disease. Br. J. Cancer 2003, 88, 658–665. [Google Scholar] [CrossRef] [PubMed]
- Sokol, M.C.; McGuigan, K.A.; Verbrugge, R.R.; Epstein, R.S. Impact of Medication Adherence on Hospitalization Risk and Healthcare Cost. Med. Care 2005, 43, 521–530. [Google Scholar] [CrossRef] [PubMed]
- Abdo-Rabbo, A.; Al-Ansari, M.; Gunn, B.C.; Suleiman, B.J. The Use of Medicines in Oman: Public Knowledge, Attitudes and Practices. Sultan Qaboos Univ. Med. J. 2009, 9, 124–131. [Google Scholar] [PubMed]
- Jimmy, B.; Jose, J.; Al-Hinai, Z.A.; Wadair, I.K.; Al-Amri, G.H. Adherence to Medications among Type 2 Diabetes Mellitus Patients in Three Districts of Al Dakhliyah Governorate, Oman: A Cross-Sectional Pilot Study. Sultan Qaboos Univ. Med. J. 2014, 14, e231–e235. [Google Scholar] [PubMed]
- Al-Rawas, O.A.; Jayakrishnan, B.; Ben Abid, F.; George, J.; Baddar, S.A.; Al-Riyami, B.M. Management and Control of Asthma in Patients Attending a Specialist Centre in Oman. Sultan Qaboos Univ. Med. J. 2009, 9, 132–139. [Google Scholar]
- Cheng, H.G.; Phillips, M.R. Secondary Analysis of Existing Data: Opportunities and Implementation. Heal. Shanghai Arch. Psychiatry 2014, 26, 371–375. [Google Scholar]
- Schommer, J.C. Final-Report-on-2013-National-Consumer-Survey-on-the-Medication-Experiances. Available online: https://www.pharmacy.umn.edu/sites/pharmacy.umn.edu/files/final-report-on-2013-national-consumer-survey-on-the-medication-experience.pdf (accessed on 15 January 2021).
- Jon Schommer 2015–2016. Available online: https://www.pharmacy.umn.edu/departments/pharmaceutical-care-health-systems/peters-chair-pharmacy-practice-innovation/chair-jon-schommer (accessed on 15 January 2021).
- Al Abri, M.; Observer, O.; al Raisi, R.; Yousuf, K.; Nair, V.; Ebuen, Y. NCDs to Blame for 70% of Deaths in Sultanate. Available online: http://www.omanobserver.om/ncds-to-blame-for-70-of-deaths-in-sultanate/ (accessed on 15 January 2021).
- National Centre for Statistics and Information. Available online: https://www.ncsi.gov.om/Pages/AllIndicators.aspx (accessed on 15 January 2021).
- The Diwan Royal Court Medical Services. المديرية العامة للخدمات الطبية—ديوان البلاط السلطاني. Available online: https://msd.gov.om/ (accessed on 15 January 2021).
- Barton, P.L. Understanding the U.S. Health Services System; Health Administration Press: Chicago, IL, USA, 2010. [Google Scholar]
- Raosoft, I. Raosoft Sample Size Calculator. Available online: http://www.raosoft.com/samplesize.html (accessed on 15 January 2021).
- Dillman, D.A.; Smyth, J.D.; Christian, L.M. Internet, Phone, Mail, and Mixed-Mode Surveys: The Tailored Design Method; John Wiley & Sons: Hoboken, NJ, USA, 2014. [Google Scholar]
- Morisky, D.E.; Green, L.W.; Levine, D.M. Concurrent and Predictive Validity of a Self-Reported Measure of Medication Adherence. Med. Care 1986, 24, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Morisky, D.E.; Ang, A.; Krousel-Wood, M.; Ward, H.J. Predictive Validity of a Medication Adherence Measure in an Out-patient Setting. J. Clin. Hypertens. (Greenwich) 2008, 10, 348–354. [Google Scholar] [CrossRef]
- Berlowitz, D.R.; Foy, C.G.; Kazis, L.E.; Bolin, L.P.; Conroy, M.B.; Fitzpatrick, P.; Gure, T.R.; Kimmel, P.L.; Kirchner, K.; Morisky, D.E.; et al. SPRINT Research Group. Effect of Intensive Blood-Pressure Treatment on Patient-Reported Outcomes. N. Engl. J. Med. 2017, 377, 733–744. [Google Scholar] [CrossRef]
- Bress, A.P.; Bellows, B.K.; King, J.B.; Hess, R.; Beddhu, S.; Zhang, Z.; Berlowitz, D.R.; Conroy, M.B.; Fine, L.; Oparil, S.; et al. SPRINT Research Group. Cost-Effectiveness of Intensive versus Standard Blood-Pressure Control. N. Engl. J. Med. 2017, 377, 745–755. [Google Scholar] [CrossRef]
- N.I.H. Meets the Definition of Human Subjects Research. Available online: https://grants.nih.gov/sites/default/files/exemption_infographic_v8_508c_1-15-2020.pdf (accessed on 15 January 2021).
- Investigator Manual. Institutional Review Board (IRB). Available online: https://assets.campbell.edu/wp-content/uploads/2018/09/CUIRB-Investigator-Manual-2020.pdf (accessed on 15 January 2021).
- Horne, R.; Weinman, J.; Hankins, M. The Beliefs about Medicines Questionnaire: The Development and Evaluation of a New Method for Assessing the Cognitive Representation of Medication. Psychol. Health 1999, 14, 1–24. [Google Scholar] [CrossRef]
- Alves, M.R. The Medication Experience of People Living with HIV: From the Understanding of the Meanings of Medication to the Development of a Conceptual Framework of Medication Experience. Ph.D. Thesis, University of Minnesota, Minneapolis, MN, USA, 2012. [Google Scholar]
- Horne, R. Patients’ Beliefs about Treatment: The Hidden Determinant of Treatment Outcome? J. Psychosom. Res. 1999, 47, 491–495. [Google Scholar] [CrossRef]
- Horne, R.; Weinman, J. Patients’ Beliefs about Prescribed Medicines and Their Role in Adherence to Treatment in Chronic Physical Illness. J. Psychosom. Res. 1999, 47, 555–567. [Google Scholar] [CrossRef]
- Pound, P.; Britten, N.; Morgan, M.; Yardley, L.; Pope, C.; Daker-White, G.; Campbell, R. Resisting Medicines: A Synthesis of Qualitative Studies of Medicine Taking. Soc. Sci. Med. 2005, 61, 133–155. [Google Scholar] [CrossRef]
- Porteous, T.; Francis, J.; Bond, C.; Hannaford, P. Temporal Stability of Beliefs about Medicines: Implications for Optimising Adherence. Patient Educ. Couns. 2010, 79, 225–230. [Google Scholar] [CrossRef] [PubMed]
- Clifford, S.; Barber, N.; Horne, R. Understanding Different Beliefs Held by Adherers, Unintentional Nonadherers, and Intentional Nonadherers: Application of the Necessity-Concerns Framework. J. Psychosom. Res. 2008, 64, 41–46. [Google Scholar] [CrossRef] [PubMed]
- Tibaldi, G.; Clatworthy, J.; Torchio, E.; Argentero, P.; Munizza, C.; Horne, R. The Utility of the Necessity—Concerns Framework in Explaining Treatment Non-Adherence in Four Chronic Illness Groups in Italy. Chronic Illn. 2009, 5, 129–133. [Google Scholar] [CrossRef]
- Neame, R.; Hammond, A. Beliefs about Medications: A Questionnaire Survey of People with Rheumatoid Arthritis. Rheumatology (Oxford) 2005, 44, 762–767. [Google Scholar] [CrossRef] [PubMed]
- Foot, H.; Caze, A.L.; Gujral, G.; Cottrell, N. The Necessity—Concerns Framework Predicts Adherence to Medication in Multiple Illness Conditions: A Meta-Analysis. Patient Educ. Couns. 2016, 99, 706–717. [Google Scholar] [CrossRef] [PubMed]
- Bane, C.; Hughes, C.M.; McElnay, J.C. The Impact of Depressive Symptoms and Psychosocial Factors on Medication Adherence in Cardiovascular Disease. Patient Educ. Couns. 2006, 60, 187–193. [Google Scholar] [CrossRef] [PubMed]
- Treharne, G.J.; Lyons, A.C.; Kitas, G.D. Medication Adherence in Rheumatoid Arthritis: Effects of Psychosocial Factors. Psychol. Health Med. 2004, 9, 337–349. [Google Scholar] [CrossRef]
- Hoogen, F.H.J.; Benraad, B.; Hekster, Y.A.; Lankveld, W.I.M. Adherence Rates and Associations with Non-Adherence in Patients with Rheumatoid Arthritis Using Disease Modifying Antirheumatic Drugs. J. Rheumatol 2009, 36, 2164–2170. [Google Scholar]
- Thurah, A.; Nørgaard, M.; Harder, I.; Stengaard-Pedersen, K. Compliance with Methotrexate Treatment in Patients with Rheumatoid Arthritis: Influence of Patients’ Beliefs about the Medicine. A Prospective Cohort Study. Rheumatol. Int. 2010, 30, 1441–1448. [Google Scholar] [CrossRef][Green Version]
- Horne, R.; Parham, R.; Driscoll, R.; Robinson, A. Patients’ Attitudes to Medicines and Adherence to Maintenance Treatment in Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2009, 15, 837–844. [Google Scholar] [CrossRef] [PubMed]
- Zullig, L.L.; Peppercorn, J.M.; Schrag, D.; Taylor, D.H., Jr.; Lu, Y.; Samsa, G.; Abernethy, A.P.; Zafar, S.Y. Financial Distress, Use of Cost-Coping Strategies, and Adherence to Prescription Medication among Patients with Cancer. J. Oncol. Pract. 2013, 9, 60s–63s. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Description | USA (n = 13,731) | Oman (n = 687) |
|---|---|---|---|
| n (%) | n (%) | ||
| Chronic Disease Types | Heart disease | 1780 (13%) | 445 (65%) |
| Diabetes | 3051 (22%) | 405 (59%) | |
| Arthritis | 6956 (51%) | 172 (25%) | |
| Breathing problems | 6241 (46%) | 87 (13%) | |
| Obesity | 7546 (55%) | 144 (21%) | |
| Stroke | 618 (5%) | 16 (2%) | |
| Cancer | 1740 (13%) | 20 (3%) | |
| Hypothyroidism | ------- | 114 (17%) | |
| Other chronic diseases | ------- | 97 (14%) | |
| Medication Adherence | Low Adherence | 6129 (52%) | 351 (55%) |
| Medium to High Adherence | 5625 (48%) | 290(45%) | |
| Medication Experiences and beliefs | |||
| a. Medicines are a life-saver | Disagree | 1133 (8%) | 75 (11%) |
| Agree | (92%) | 615 (89%) | |
| b. Medicines are burden | Disagree | 5570 (41%) | 477 (71%) |
| Agree | 8161 (59%) | 195 (29%) | |
| c. Medicines do harm more than good | Disagree | 8599 (63%) | 552 (83%) |
| Agree | 5132 (37%) | 116 (17%) | |
| Age | 20s | 2056 (14.9%) | 42 (6.5%) |
| 30s | 2373 (17.3%) | 120 (18.5%) | |
| 40s | 2293 (16.7%) | 167 (25.8%) | |
| 50s | 2806 (20.4%) | 176 (27.2%) | |
| 60s | 2805 (20.4%) | 102 (15.8%) | |
| 70s | 1173 (8.5%) | 35 (5.4%) | |
| 80s | 212 (1.5%) | 5 (0.8%) | |
| 90s | 13 (0.1%) | ------ | |
| Gender | Male | 3839 (28%) | 331 (50%) |
| Female | 9892 (72%) | 329 (50%) | |
| Educational Level | Less than a High School Graduate | 336 (2%) | 404 (61%) |
| High School Graduate and Higher | (98%) | 258 (39%) | |
| Low Medication Adherence | ||||
|---|---|---|---|---|
| USA (Total n = 11,754) Oman (Total n = 561) | USA (Total n = 11,754) Oman (Total n = 547) | USA (Total n = 11,754) Oman (Total n = 542) | ||
| Not a life-saver n (%) | Burden n (%) | Does more harm than good n (%) | ||
| USA | Disagree | 5655/10974 (52%) | 2001/4914 (41%) | 3590/7629 (47%) |
| Agree | 474/780 (61%) | 4128/6840 (60%) | 2539/4125 (62%) | |
| Oman | Disagree | 256/504 (51%) | 184/388 (47%) | 237/459 (52%) |
| Agree | 46/57 (81%) | 104/159 (65%) | 50/83 (60%) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ibrahim, K.M.; Schommer, J.C.; Morisky, D.E.; Rodriguez, R.; Gaither, C.; Snyder, M. The Association between Medication Experiences and Beliefs and Low Medication Adherence in Patients with Chronic Disease from Two Different Societies: The USA and the Sultanate of Oman. Pharmacy 2021, 9, 31. https://doi.org/10.3390/pharmacy9010031
Ibrahim KM, Schommer JC, Morisky DE, Rodriguez R, Gaither C, Snyder M. The Association between Medication Experiences and Beliefs and Low Medication Adherence in Patients with Chronic Disease from Two Different Societies: The USA and the Sultanate of Oman. Pharmacy. 2021; 9(1):31. https://doi.org/10.3390/pharmacy9010031
Chicago/Turabian StyleIbrahim, Kamla M., Jon C. Schommer, Donald E. Morisky, Raquel Rodriguez, Caroline Gaither, and Mark Snyder. 2021. "The Association between Medication Experiences and Beliefs and Low Medication Adherence in Patients with Chronic Disease from Two Different Societies: The USA and the Sultanate of Oman" Pharmacy 9, no. 1: 31. https://doi.org/10.3390/pharmacy9010031
APA StyleIbrahim, K. M., Schommer, J. C., Morisky, D. E., Rodriguez, R., Gaither, C., & Snyder, M. (2021). The Association between Medication Experiences and Beliefs and Low Medication Adherence in Patients with Chronic Disease from Two Different Societies: The USA and the Sultanate of Oman. Pharmacy, 9(1), 31. https://doi.org/10.3390/pharmacy9010031






