Accessing Mole-Scanning through Community Pharmacy: A Pilot Service in Collaboration with Dermatology Specialists
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Overview
2.2. Intervention
2.3. Data Collection and Analysis
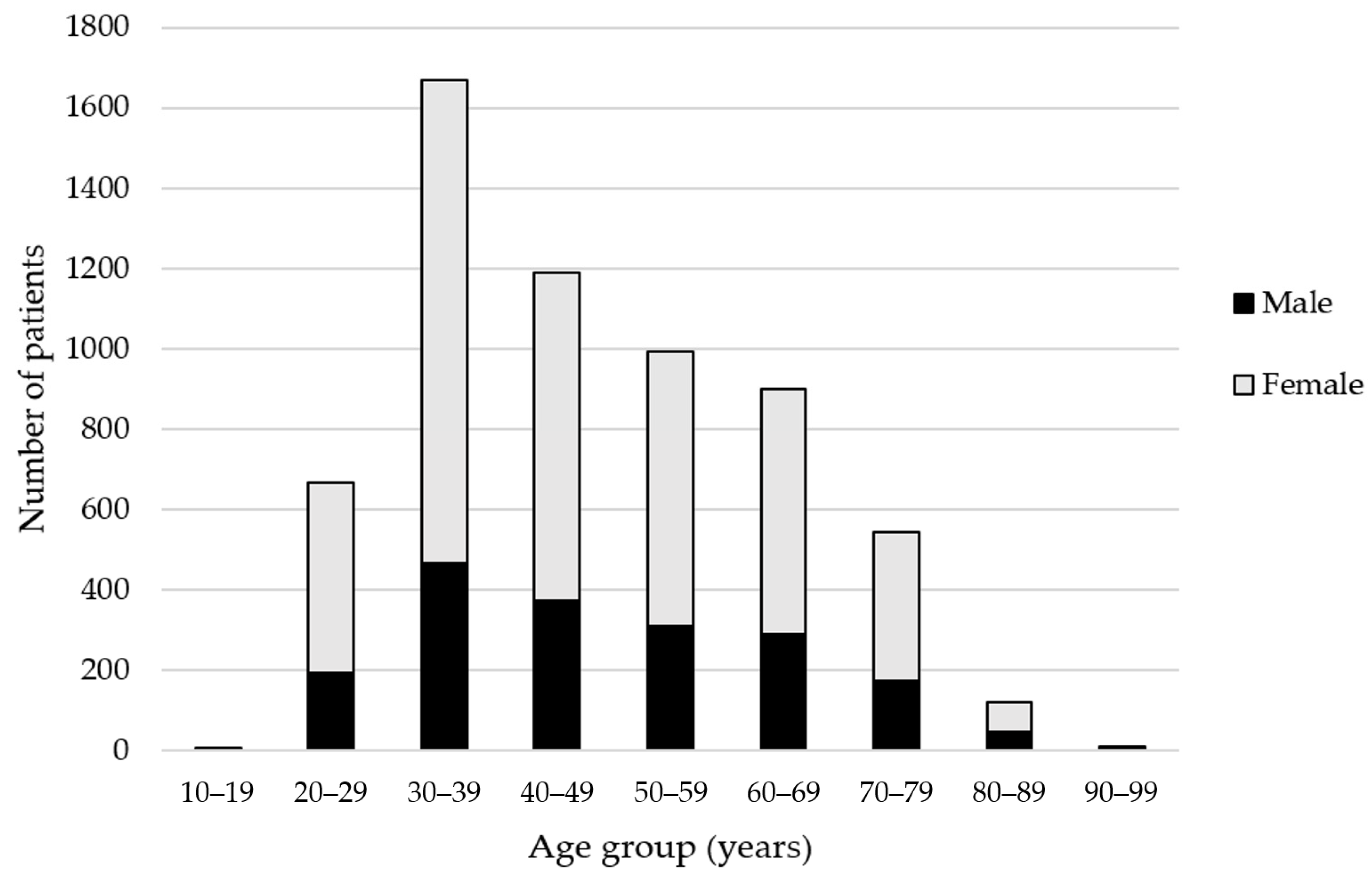
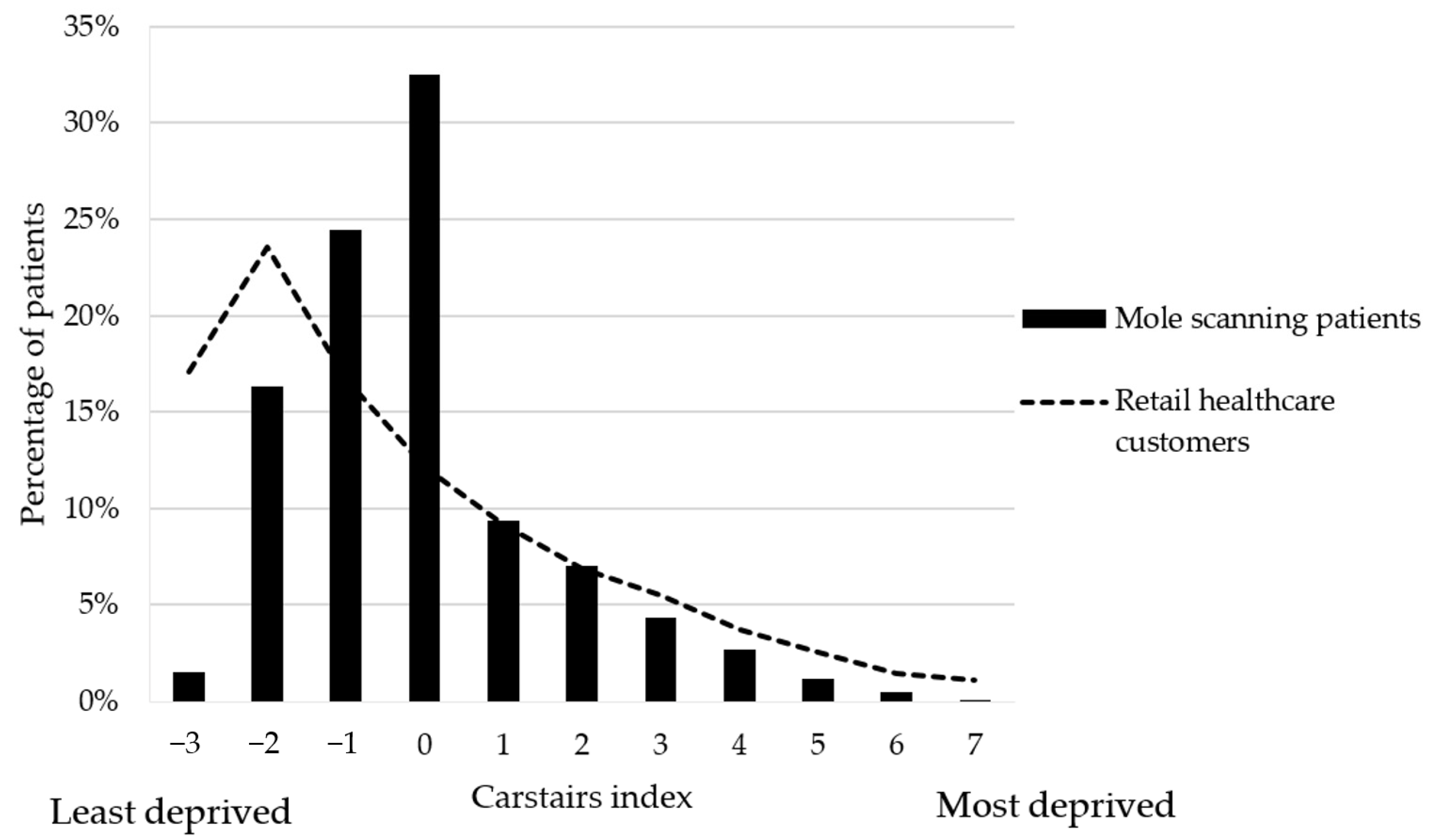
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Seventh World Health Assembly Agenda Item 15.6: Cancer Prevention and Control in the Context of an Integrated Approach (WHA70.12). Available online: https://apps.who.int/iris/rest/bitstreams/1159429/retrieve (accessed on 2 October 2020).
- Cancer Research UK Melanoma Skin Cancer Statistics. Available online: www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/melanoma-skin-cancer#heading-Zero (accessed on 2 October 2020).
- Johnson, M.M.; Leachman, S.A.; Aspinwall, L.G.; Cranmer, L.D.; Curiel-Lewandrowski, C.; Sondak, V.K.; Stemwedel, C.E.; Swetter, S.M.; Vetto, J.; Bowles, T.; et al. Skin cancer screening: Recommendations for data-driven screening guidelines and a review of the US Preventive Services Task Force controversy. Melanoma Manag. 2017, 4, 13–37. [Google Scholar] [CrossRef] [PubMed]
- Katalinic, A.; Eisemann, N.; Waldmann, A. Skin Cancer Screening in Germany. Documenting Melanoma Incidence and Mortality from 2008 to 2013. Dtsch. Arztebl. Int. 2015, 112, 629–634. [Google Scholar] [PubMed]
- Waldmann, A.; Nolte, S.; Weinstock, M.A.; Breitbart, E.W.; Eisemann, N.; Geller, A.C.; Greinert, R.; Volkmer, B.; Katalinic, A. Skin cancer screening participation and impact on melanoma incidence in Germany—An observational study on incidence trends in regions with and without population-based screening. Br. J. Cancer 2012, 106, 970–974. [Google Scholar] [CrossRef] [PubMed]
- Johansson, M.; Brodersen, J.; Gøtzsche, P.C.; Jørgensen, K.J. Screening for reducing morbidity and mortality in malignant melanoma. Cochrane Database Syst. Rev. 2019, 6, Cd012352. [Google Scholar] [CrossRef] [PubMed]
- Voss, R.K.; Woods, T.N.; Cromwell, K.D.; Nelson, K.C.; Cormier, J.N. Improving outcomes in patients with melanoma: Strategies to ensure an early diagnosis. Patient Relat. Outcome Meas. 2015, 6, 229–242. [Google Scholar] [PubMed]
- Alexandrescu, D.T. Melanoma costs: A dynamic model comparing estimated overall costs of various clinical stages. Derm. Online J. 2009, 15, 1. [Google Scholar]
- Kakushadze, Z.; Raghubanshi, R.; Yu, W. Estimating Cost Savings from Early Cancer Diagnosis. Data 2017, 2, 30. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence (NICE) Skin Cancers—Recognition and Referral. Available online: https://cks.nice.org.uk/skin-cancers-recognition-and-referral#!scenario (accessed on 2 October 2020).
- NHS England Transforming Elective Care Services Dermatology. Available online: www.england.nhs.uk/publication/transforming-elective-care-services-dermatology/ (accessed on 2 October 2020).
- Dermatology Council for England 2017 Audit of Undergraduate Education. Available online: www.appgs.co.uk/publication/view/2017-audit-of-undergraduate-education/ (accessed on 2 October 2020).
- Greenfield, G.; Foley, K.; Majeed, A. Rethinking primary care’s gatekeeper role. BMJ 2016, 354, i4803. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.C.; Bravata, D.M.; Weil, E.; Olkin, I. A comparison of dermatologists’ and primary care physicians’ accuracy in diagnosing melanoma: A systematic review. Arch. Derm. 2001, 137, 1627–1634. [Google Scholar] [CrossRef] [PubMed]
- Berk-Krauss, J.; Polsky, D.; Stein, J.A. Mole Mapping for Management of Pigmented Skin Lesions. Derm. Clin. 2017, 35, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Argenziano, G.; Puig, S.; Zalaudek, I.; Sera, F.; Corona, R.; Alsina, M.; Barbato, F.; Carrera, C.; Ferrara, G.; Guilabert, A.; et al. Dermoscopy improves accuracy of primary care physicians to triage lesions suggestive of skin cancer. J. Clin. Oncol. 2006, 24, 1877–1882. [Google Scholar] [CrossRef] [PubMed]
- Koelink, C.J.; Vermeulen, K.M.; Kollen, B.J.; de Bock, G.H.; Dekker, J.H.; Jonkman, M.F.; van der Heide, W.K. Diagnostic accuracy and cost-effectiveness of dermoscopy in primary care: A cluster randomized clinical trial. J. Eur. Acad. Derm. Venereol 2014, 28, 1442–1449. [Google Scholar] [CrossRef] [PubMed]
- Todd, A.; Copeland, A.; Husband, A.; Kasim, A.; Bambra, C. The positive pharmacy care law: An area-level analysis of the relationship between community pharmacy distribution, urbanity and social deprivation in England. BMJ Open 2014, 4, e005764. [Google Scholar] [CrossRef] [PubMed]
- Pharmaceutical Services Negotiating Committee (PSNC) PSNC Services Database. Available online: https://psnc.org.uk/services-commissioning/services-database/ (accessed on 2 October 2020).
- National Health Service (NHS) Interim NHS People Plan. Available online: www.longtermplan.nhs.uk/wp-content/uploads/2019/06/ipp-p-future-workforce.pdf (accessed on 2 October 2020).
- Kjome, R.L.S.; Wright, D.J.; Bjaaen, A.B.; Garstad, K.W.; Valeur, M. Dermatological cancer screening: Evaluation of a new community pharmacy service. Res. Soc. Adm. Pharm. 2017, 13, 1214–1217. [Google Scholar] [CrossRef] [PubMed]
- National Health Service (NHS) Overview Skin Cancer (Melanoma). Available online: www.nhs.uk/conditions/melanoma-skin-cancer/ (accessed on 2 October 2020).
- Emery, J.D.; Hunter, J.; Hall, P.N.; Watson, A.J.; Moncrieff, M.; Walter, F.M. Accuracy of SIAscopy for pigmented skin lesions encountered in primary care: Development and validation of a new diagnostic algorithm. BMC Derm. 2010, 10, 9. [Google Scholar] [CrossRef] [PubMed]
- Morgan, O.; Baker, A. Measuring deprivation in England and Wales using 2001 Carstairs scores. Health Stat. Q. 2006, 31, 28–33. [Google Scholar]
- Curtis, L.; Burns, A. PSSRU Unit Costs of Health & Social Care 2019. Available online: www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2019/ (accessed on 2 October 2020).
- Office for National Statistics. Cancer Registration Statistics, England. Available online: www.ons.gov.uk/peoplepopulationandcommunity/healthandsocialcare/conditionsanddiseases/datasets/cancerregistrationstatisticscancerregistrationstatisticsengland (accessed on 2 October 2020).
- Boardman, H.; Lewis, M.; Croft, P.; Trinder, P.; Rajaratnam, G. Use of community pharmacies: A population-based survey. J. Public Health 2005, 27, 254–262. [Google Scholar] [CrossRef] [PubMed]
- Amaro-Ortiz, A.; Yan, B.; D’Orazio, J.A. Ultraviolet radiation, aging and the skin: Prevention of damage by topical cAMP manipulation. Molecules 2014, 19, 6202–6219. [Google Scholar] [CrossRef] [PubMed]
- NHS England A&E Attendances and Emergency Admissions 2019–2020. Available online: www.england.nhs.uk/statistics/statistical-work-areas/ae-waiting-times-and-activity/ae-attendances-and-emergency-admissions-2019-20/ (accessed on 2 October 2020).
- Earnshaw, C.H.; Hunter, H.J.A.; McMullen, E.; Griffiths, C.E.M.; Warren, R.B. Reduction in skin cancer diagnosis, and overall cancer referrals, during the COVID-19 pandemic. Br. J. Derm. 2020, 183, 792–794. [Google Scholar] [CrossRef] [PubMed]
| Outcome of Scan Analysis | n (% of Total) | |
|---|---|---|
| No follow up required | Normal | 5667 (57.4%) |
| Non suspicious seborrhoeic keratosis | 2217 (22.4%) | |
| Potential sun damage | 603 (6.1%) | |
| Other skin lesion (normal) | 169 (1.7%) | |
| Normal with atypical characteristics | 106 (1.1%) | |
| Total–no follow up required | 8762 (88.7%) | |
| Follow up required | Suspicious | 452 (4.6%) |
| Other skin lesion to follow up | 296 (3.0%) | |
| Sun damage | 193 (2.0%) | |
| Basal cell carcinoma cannot be excluded | 173 (1.8%) | |
| Inadequate scan/more information required | 4 (0.0%) | |
| Total–follow up required | 1118 (11.3%) | |
| Total | 9880 | |
| Confirmed Diagnosis | n (%) |
|---|---|
| Normal | 335 (44.3%) |
| Sun damage | 197 (26.0%) |
| Basal cell carcinoma | 83 (11.0%) |
| Other skin condition | 50 (6.6%) |
| Malignant melanoma | 47 (6.2%) |
| Seborrhoeic keratosis | 23 (3.0%) |
| Atypical | 19 (2.5%) |
| Squamous cell carcinoma | 3 (0.4%) |
| Total | 757 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kirkdale, C.L.; Archer, Z.; Thornley, T.; Wright, D.; Valeur, M.; Gourlay, N.; Ayerst, K. Accessing Mole-Scanning through Community Pharmacy: A Pilot Service in Collaboration with Dermatology Specialists. Pharmacy 2020, 8, 231. https://doi.org/10.3390/pharmacy8040231
Kirkdale CL, Archer Z, Thornley T, Wright D, Valeur M, Gourlay N, Ayerst K. Accessing Mole-Scanning through Community Pharmacy: A Pilot Service in Collaboration with Dermatology Specialists. Pharmacy. 2020; 8(4):231. https://doi.org/10.3390/pharmacy8040231
Chicago/Turabian StyleKirkdale, Charlotte L., Zoe Archer, Tracey Thornley, David Wright, Mette Valeur, Nicola Gourlay, and Kurt Ayerst. 2020. "Accessing Mole-Scanning through Community Pharmacy: A Pilot Service in Collaboration with Dermatology Specialists" Pharmacy 8, no. 4: 231. https://doi.org/10.3390/pharmacy8040231
APA StyleKirkdale, C. L., Archer, Z., Thornley, T., Wright, D., Valeur, M., Gourlay, N., & Ayerst, K. (2020). Accessing Mole-Scanning through Community Pharmacy: A Pilot Service in Collaboration with Dermatology Specialists. Pharmacy, 8(4), 231. https://doi.org/10.3390/pharmacy8040231






