The Role of Community Pharmacists in the Detection of Clinically Relevant Drug-Related Problems in Chronic Kidney Disease Patients
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Setting
2.2. Community Pharmacists’ Study Information
2.3. Inclusion Criteria
2.4. Exclusion Criteria
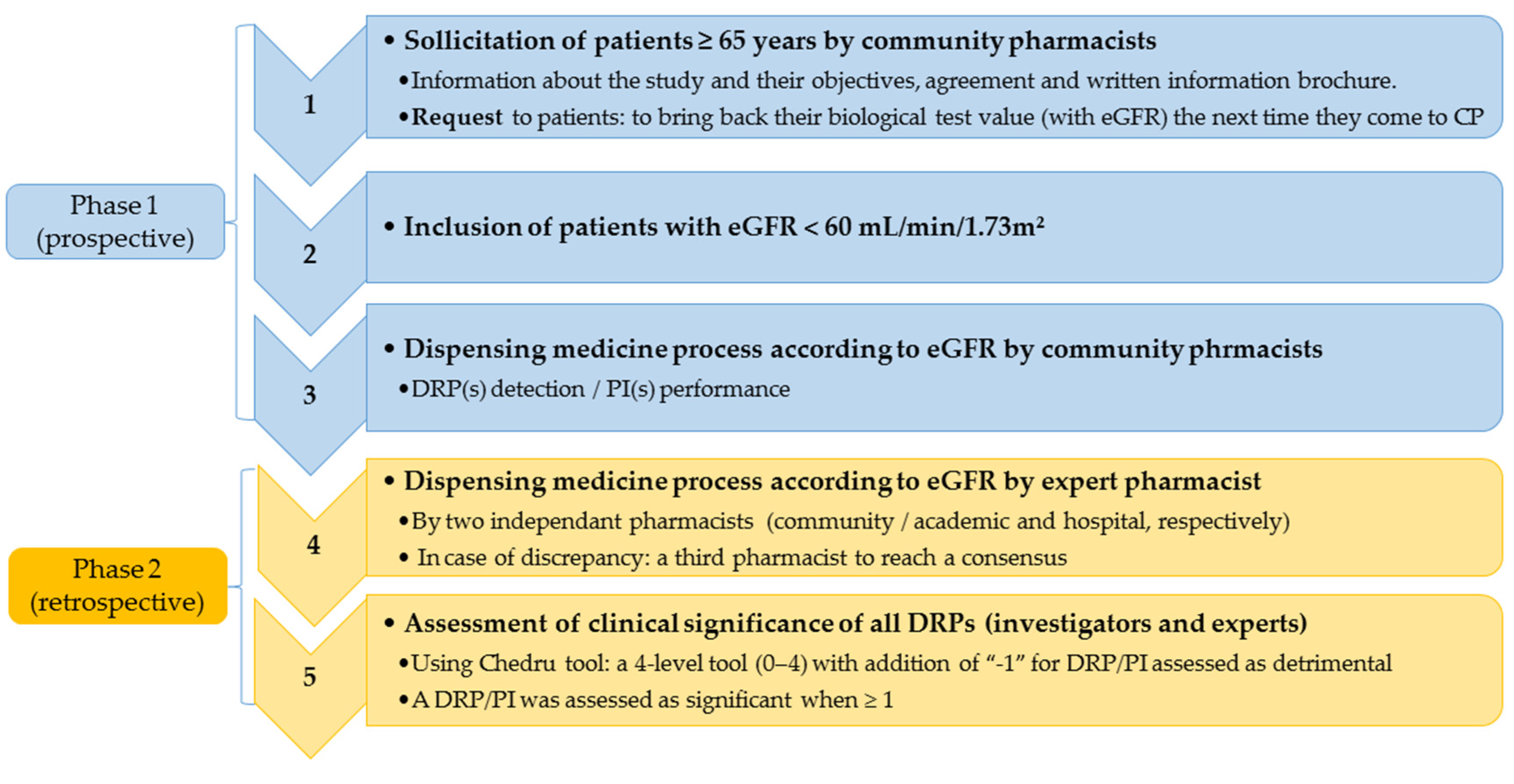
2.5. Study Design
2.6. Month Internship Period
2.7. Retrospective Dispensing Process by Expert Pharmacists and Comparison with Community Pharmacists
2.8. Comparative Clinical Assessment of Pharmacists’ DRPs
2.9. Satisfaction Form
2.10. Statistical Analysis
2.11. Ethics Approval
3. Results
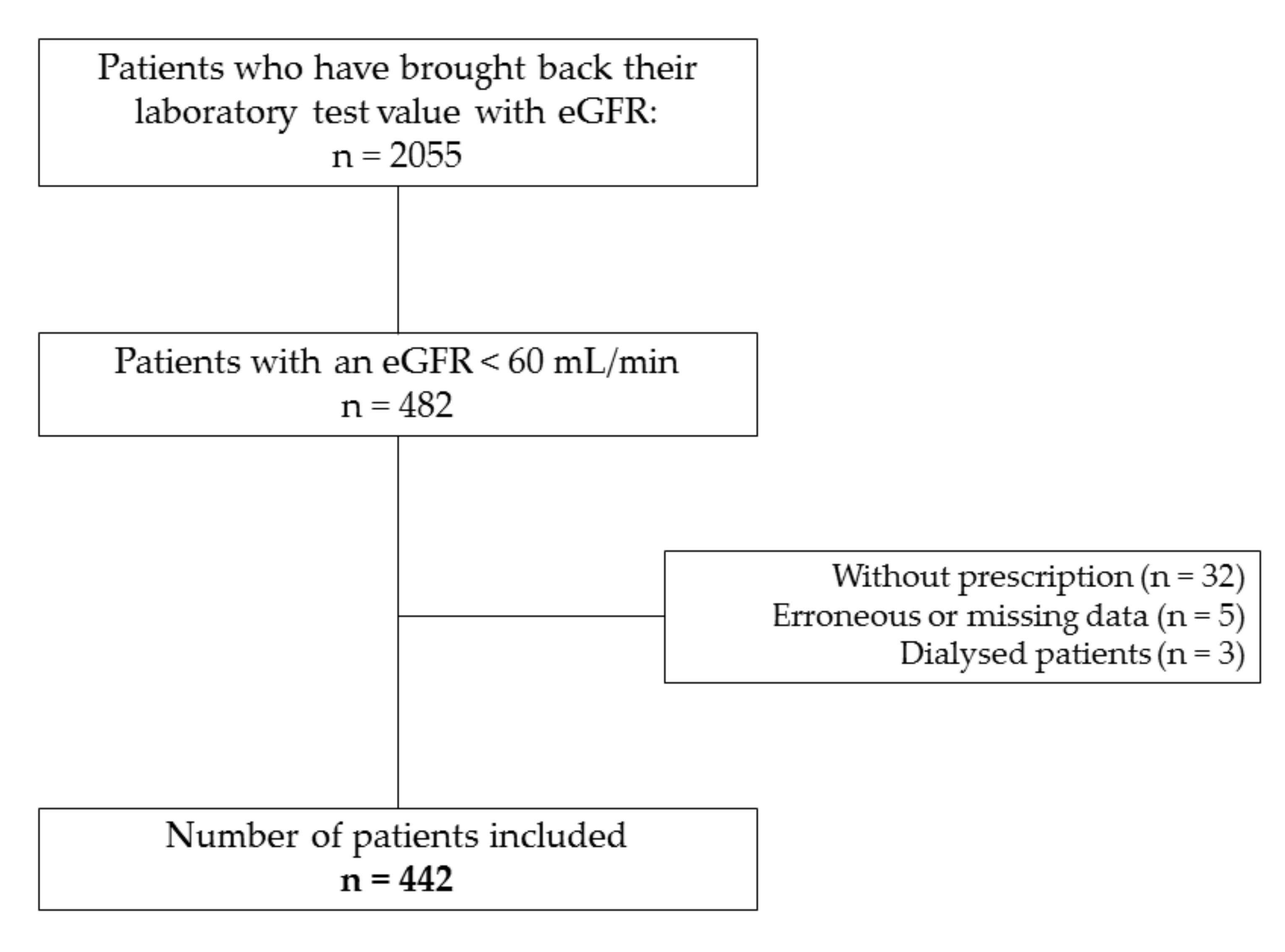
3.1. Population
3.2. Population DRP Detection by Community Pharmacists and Expert Pharmacists
3.3. Comparative Clinical Relevance Assessment of DRPs
3.4. Satisfaction Form
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Stengel, B.; Couchoud, C.; Helmer, C.; Loos-Ayav, C.; Kessler, M. Epidemiology of chronic kidney disease in France. Press Med. 2007, 36, 1811–1821. (in French). [Google Scholar] [CrossRef][Green Version]
- Lindeman, R.D.; Tobin, J.; Shock, N.W. Longitudinal studies on the rate of decline in renal function with age. J. Am. Geriatr. Soc. 1985, 33, 278–285. [Google Scholar] [CrossRef] [PubMed]
- Bitzer, M.; Wiggins, J. Aging Biology in the Kidney. Adv. Chronic Kidney Dis. 2016, 23, 12–18. [Google Scholar] [CrossRef]
- Bell, J.S.; Blacker, N.; Leblanc, V.T.; Alderman, C.P.; Philips, A.; Rowett, D.; Rossi, S.; Frank, O.; Husband, A. Prescribing for older people with chronic renal impairment. Aust. Fam. Physician. 2013, 42, 24–28. [Google Scholar] [PubMed]
- Webster, A.C.; Nagler, E.V.; Morton, R.L.; Masson, P. Chronic Kidney Disease. Lancet. 2017, 389, 1238–1252. [Google Scholar] [CrossRef]
- Koster, E.S.; Philbert, D.; Noordam, M.; Winters, N.A.; Blom, L.; Bouvy, M.L. Availability of information on renal function in Dutch community pharmacies. Int. J. Clin. Pharm. 2016, 38, 797–801. [Google Scholar] [CrossRef]
- Stemer, G.; Lemmens-Gruber, R. Clinical pharmacy activities in chronic kidney disease and end-stage renal disease patients: A systematic literature review. BMC Nephrol. 2011, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Salgado, T.M.; Moles, R.; Benrimoj, S.I.; Fernandez-Llimos, F. Pharmacists’ interventions in the management of patients with chronic kidney disease: A systematic review. Nephrol. Dial. Transplant. 2012, 27, 276–292. [Google Scholar] [CrossRef] [PubMed]
- Salgado, T.M.; Correr, C.J.; Moles, R.; Benrimoj, S.I.; Fernandez-Llimos, F. Assessing the implementability of clinical pharmacist interventions in patients with chronic kidney disease: An analysis of systematic reviews. Ann. Pharmacother. 2013, 47, 1498–1506. [Google Scholar] [CrossRef] [PubMed]
- Kondo, Y.; Ishitsuka, Y.; Shigemori, E.; Irikura, M.; Kadowaki, D.; Hirata, S.; Maemura, T.; Irie, T. Awareness and current implementation of drug dosage adjustment by pharmacists in patients with chronic kidney disease in Japan: A web-based survey. BMC Health. Serv. Res. 2014, 14, 615. [Google Scholar] [CrossRef]
- Pourrat, X.; Sipert, A.-S.; Gatault, P.; Sautenet, B.; Hay, N.; Guinard, F.; Guegan, F.; Halimi, J.-M. Community Pharmacist intervention in patients with renal impairment. Int. J. Clin. Pharm. 2015, 37, 1172–1179. [Google Scholar] [CrossRef] [PubMed]
- Bourdon, O.; Ekeland, C.; Brion, F. Pharmacy education in France. Am. J. Pharm. Educ. 2008, 72, 132. [Google Scholar] [CrossRef] [PubMed]
- Vo, T.H.; Bardet, J.-D.; Charpiat, B.; Leyrissoux, C.; Gravoulet, J.; Allenet, B.; Conort, O.; Bedouch, P. Validation of a tool for reporting pharmacists’ interventions in everyday community pharmacy. J. Clin. Pharm. Ther. 2018, 43, 240–248. [Google Scholar] [CrossRef] [PubMed]
- Dooley, M.J.; Allen, K.M.; Doecke, C.J.; Galbraith, K.J.; Taylor, G.R.; Bright, J.; Carey, D.L. A prospective multicentre study of pharmacist initiated changes to drug therapy and patient management in acute care government funded hospitals. Br. J. Clin. Pharmacol. 2004, 57, 513–521. [Google Scholar] [CrossRef]
- Levey, A.S.; Bosch, J.P.; Lewis, J.B.; Greene, T.; Rogers, N.; Roth, D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann. Intern. Med 1999, 130, 461–470. [Google Scholar] [CrossRef]
- Levey, A.S.; Stevens, L.A.; Schmid, C.H.; Zhang, Y.L.; Castro, A.F., 3rd; Feldman, H.I.; Kusek, J.W.; Eggers, P.; Van Lente, F.; Greene, T.; et al. A New Equation to Estimate Glomerular Filtration Rate. Ann. Intern. Med. 2009, 150, 604–613. [Google Scholar] [CrossRef]
- Hatoum, H.T.; Hutchinson, R.A.; Witte, K.W.; Newby, G.P. Evaluation of the contribution of clinical pharmacists: Inpatient care and cost reduction. Drug Intell. Clin. Pharm. 1988, 22, 252–259. [Google Scholar] [CrossRef]
- Chedru, V.; Juste, M. Physician assessment of the clinical impact of pharmacists’ interventions. J. Pharm. Clin. 1997, 16, 254–258. [Google Scholar]
- Sim, J.; Wright, C.C. The kappa statistic in reliability studies: Use of interpretation and sample size requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef]
- Sackett, D.L.; Haynes, R.B.; Guyatt, G.H.; Tugwell, P. Clinical Epidemiology in A Basic Science for Clinical Medicine, 2nd ed.; Little Brown & Co: Boston, MA, USA, 1985. [Google Scholar]
- Arora, P.; Vasa, P.; Brenner, D.; Iglar, K.; McFarlane, P.; Morrison, H.; Badawi, A. Prevalence estimates of chronic kidney disease in Canada: Results of a nationally representative survey. CMAJ. 2013, 185, E417–E423. [Google Scholar] [CrossRef]
- Hoerger, T.J.; Simpson, S.A.; Yarnoff, B.O.; Pavkov, M.E.; Ríos Burrows, N.; Saydah, S.H.; Williams, D.E.; Zhuo, X. The future burden of CKD in the United States: A simulation model for the CDC CKD Initiative. Am. J. Kidney Dis. 2015, 65, 403–411. [Google Scholar] [CrossRef] [PubMed]
- Breton, G.; Froissart, M.; Janus, N.; Launay-Vacher, V.; Verr, C.; Tzourio, C.; Helmer, C.; Stengel, B. Inappropriate drug use and mortality in community-dwelling elderly with impaired kidney function—the Three-City population-based study. Nephrol. Dial. Transplant. 2011, 26, 2852–2859. [Google Scholar] [CrossRef]
- Laville, S.M.; Metzger, M.; Stengel, B.; Jacquelinet, C.; Combe, C.; Fouque, D.; Laville, M.; Frimat, L.; Ayav, C.; Speyer, E.; et al. Chronic Disease-Renal Epidemiology and Information Network (CKD-REIN) Study Collaborators. Evaluation of the adequacy of drug prescriptions in patients with chronic kidney disease: Results from the CKD-REIN cohort. Br. J. Clin. Pharmacol. 2018, 84, 2811–2823. [Google Scholar] [CrossRef] [PubMed]
- Belaiche, S.; Romanet, T.; Allenet, B.; Calop, J.; Zaoui, P. Identification of drug-related problems in ambulatory chronic kidney disease patients: A 6-month prospective study. J. Nephrol. 2012, 25, 782–788. [Google Scholar] [CrossRef] [PubMed]
- De Boer, I.H.; Rue, T.C.; Hall, Y.N.; Heagerty, P.J.; Weiss, N.S.; Himmelfarb, J. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA 2011, 305, 2532–2539. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Care. Pharmacologic Approaches to Glycemic Treatment: Standard of Medical Care in Diabetes—2018. Diabetes Care. 2018, 41, S73–S85. [Google Scholar] [CrossRef]
- Calabrese, A.T.; Coley, K.C.; DaPos, S.V.; Swanson, D.; Rao, R.H. Evaluation of prescribing practices: Risk of lactic acidosis with metformin therapy. Arch. Intern. Med. 2002, 162, 434–437. [Google Scholar] [CrossRef]
- Khanal, A.; Peterson, G.M.; Castelino, R.L.; Jose, M.D. Potentially inappropriate prescribing of renally cleared drug in elderly patients in community and aged care settings. Drugs Aging. 2015, 32, 391–400. [Google Scholar] [CrossRef]
- Chang, F.; O’Hare, A.M.; Miao, Y.; Steinman, M.A. Use of Renally Inappropriate Medications in Older Veterans: A National Study. J. Am. Geriatr. Soc. 2015, 63, 2290–2297. [Google Scholar] [CrossRef]
- Charpiat, B.; Macchi-Andanson, M.; Perquin, S.; Leboucher, G.; Brandon, T. Performance assessment of pharmacy residents: Application to prescription analysis and the proper use of medicines. J. Pharm. Clin. 2003, 22, 215–220. [Google Scholar]
- Sandler, D.P.; Burr, F.R.; Weinberg, C.R. Nonsteroidal anti-inflammatory drugs and the risk for chronic renal disease. Ann. Intern. Med. 1991, 115, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Winkelmayer, W.C.; Waikar, S.S.; Mogun, H.; Solomon, D.H. Nonselective and cyclooxygenase-2-selective NSAIDs and acute kidney injury. Am. J. Med. 2008, 121, 1092–1098. [Google Scholar] [CrossRef] [PubMed]
- Weng, F.L.; Dhillon, N.; Lin, Y.; Mulgaonkar, S.; Patel, A.M. Racial differences in outcomes of the evaluation of potential live kidney donors: A retrospective cohort study. Am. J. Nephrol. 2012, 35, 409–415. [Google Scholar] [CrossRef] [PubMed]
- Prescott, L.F.; Speirs, G.C.; Critchley, J.A.; Temple, R.M.; Winney, R.J. Paracetamol disposition and metabolite kinetics in patients with chronic renal failure. Eur. J. Clin. Pharmacol. 1989, 36, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Launay-Vacher, V.; Karie, S.; Fau, J.-B.; Izzedine, H.; Deray, G. Treatment of pain in patients with renal insufficiency: The World Health Organization three-step ladder adapted. J. Pain. 2005, 6, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Verpooten, G.A.; Genissel, P.M.; Thomas, J.R.; De Broe, M.E. Single dose pharmacokinetics of perindopril and its metabolites in hypertensive patients with various degrees of renal insufficiency. Br. J. Clin. Pharmacol. 1991, 32, 187–192. [Google Scholar] [CrossRef]
- Sennesael, J.; Ali, A.; Sweny, P.; Vandenburg, M.; Slovic, D.; Dratwa, M.; Resplandy, G.; Genissel, P.; Desche, P. The pharmacokinetics of perindopril and its effects on serum angiotensin converting enzyme activity in hypertensive patients with chronic renal failure. Br. J. Clin. Pharmacol. 1992, 33, 93–99. [Google Scholar] [CrossRef]
- Chiurchiu, C.; Remuzzi, G.; Ruggenenti, P. Angiotensin-converting enzyme inhibition and renal protection in nondiabetic patients: The data of the meta-analyses. J. Am. Soc. Nephrol. 2005, 16, S58–S63. [Google Scholar] [CrossRef]
- Dreischulte, T.; Morales, D.R.; Bell, S.; Guthrie, B. Combined use of nonsteroidal anti-inflammatory drugs with diuretics and/or renin-angiotensin system inhibitors in the community increases the risk of acute kidney injury. Kidney Int. 2015, 88, 396–403. [Google Scholar] [CrossRef]
- Bryant, L.J.; Coster, G.; Gamble, G.D.; McCormick, R.N. The General Practitioner-Pharmacist Collaboration (GPPC) study: A randomised controlled trial of clinical medication reviews in community pharmacy. Int. J. Pharm. Pract. 2011, 19, 94–105. [Google Scholar] [CrossRef]
| Community Pharmacists n (%) | Expert Pharmacists n (%) | |
|---|---|---|
| Number of DRPs (categories below) | 99 | 184 |
| Dosage problem | 73 (73.7) | 133 (72.3) |
| Contraindication/non-conformity to guidelines | 26 (26.3) | 26 (14.1) |
| Monitoring | - | 14 (7.6) |
| Therapeutic redundancy | - | 5 (2.7) |
| Improper prescription: lack of information, of clarity | - | 6 (3.3) |
| Drug Classes | ||
| Antidiabetics | 20 (20.3) | 40 (21.7) |
| Anti-gout preparations | 12 (12.1) | 29 (15.8) |
| Analgesics | 5 (5.1) | 49 (26.6) |
| ACE inhibitors | 17 (17.2) | 4 (2.2) |
| Diuretics | 15 (15.2) | - |
| Others | 30 (30.3) | 62 (33.7) |
| Number of Interventions (Categories Below) | 99 | 184 * |
| Dose adjustment | 72 (72.7) | 126 (68.5) |
| Drug switch/establishment of a therapeutic alternative | 12 (12.1) | 29 (15.8) |
| Drug monitoring | 9 (9.1) | 18 (9.8) |
| Discontinuation or refusal to deliver | 6 (6.1) | 5 (2.7) |
| Optimization of the dispensing/administration modalities | - | 6 (3.3) |
| Community Pharmacists’ DRPs | Expert Pharmacists’ DRPs | |||||||
|---|---|---|---|---|---|---|---|---|
| Clinical relevance | Nephrologist | General practitioner 1 | General practitioner 2 | p | Nephrologist | General practitioner 1 | General practitioner 2 | p |
| 0 | 39 (49.4) | 38 (46.9) | 32 (41.2) | NS | 26 (17.8) | 37 (25.2) | 8 (5.4) | <0.001 |
| ≥1 | 40 (50.6) | 43 (53.1) | 46 (57.8) | 120 (82.2) | 110 (74.8) | 142 (94.6) | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mongaret, C.; Aubert, L.; Lestrille, A.; Albaut, V.; Kreit, P.; Herlem, E.; Noel, N.; Touré, F.; Lallier, F.; Slimano, F.; et al. The Role of Community Pharmacists in the Detection of Clinically Relevant Drug-Related Problems in Chronic Kidney Disease Patients. Pharmacy 2020, 8, 89. https://doi.org/10.3390/pharmacy8020089
Mongaret C, Aubert L, Lestrille A, Albaut V, Kreit P, Herlem E, Noel N, Touré F, Lallier F, Slimano F, et al. The Role of Community Pharmacists in the Detection of Clinically Relevant Drug-Related Problems in Chronic Kidney Disease Patients. Pharmacy. 2020; 8(2):89. https://doi.org/10.3390/pharmacy8020089
Chicago/Turabian StyleMongaret, Céline, Léa Aubert, Amélie Lestrille, Victorine Albaut, Pierre Kreit, Emmanuelle Herlem, Natacha Noel, Fatouma Touré, François Lallier, Florian Slimano, and et al. 2020. "The Role of Community Pharmacists in the Detection of Clinically Relevant Drug-Related Problems in Chronic Kidney Disease Patients" Pharmacy 8, no. 2: 89. https://doi.org/10.3390/pharmacy8020089
APA StyleMongaret, C., Aubert, L., Lestrille, A., Albaut, V., Kreit, P., Herlem, E., Noel, N., Touré, F., Lallier, F., Slimano, F., & MIRPhO Investigators Study, t. (2020). The Role of Community Pharmacists in the Detection of Clinically Relevant Drug-Related Problems in Chronic Kidney Disease Patients. Pharmacy, 8(2), 89. https://doi.org/10.3390/pharmacy8020089





