Pharmacists’ Confidence in Managing Patients with Inflammatory Bowel Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Survey Development
2.2. Data Collection
2.3. Data Analysis
2.4. Ethics and Competing Interests
3. Results
3.1. Study Sample
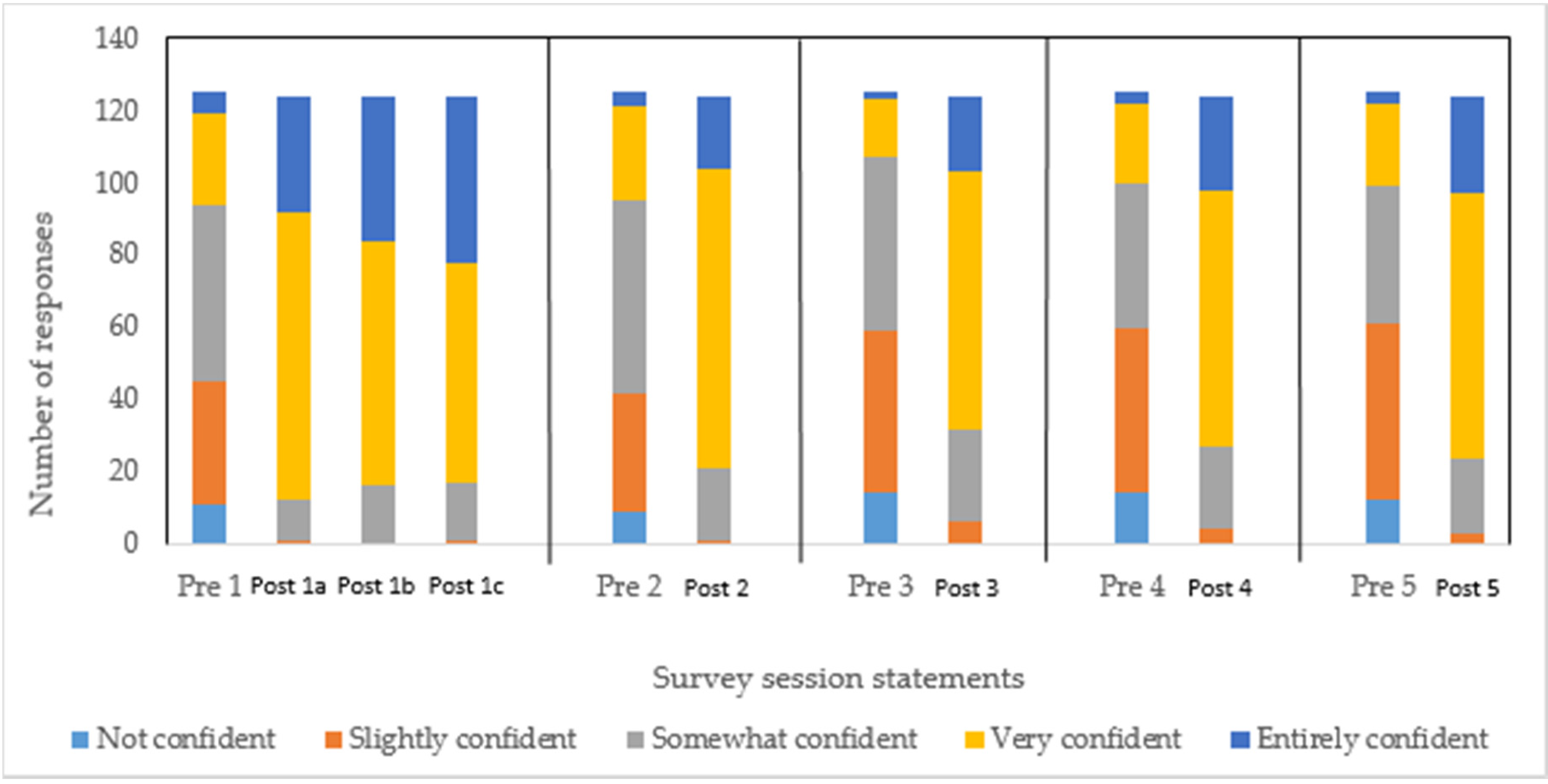
3.2. Pharmacist Confidence
3.3. Educational Opportunities
3.4. Barriers to Learning
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Disclosures
Abbreviations
| IBD | Inflammatory bowel disease |
| HCP | healthcare professionals |
| MOA | mode of action |
| CM | complementary medicines |
References
- Mowat, C.; Cole, A.; Windsor, A.; Ahmad, T.; Arnott, I.; Driscoll, R.; Mitton, S.; Orchard, T.; Rutter, M.; Younge, L.; et al. Guidelines for the management of inflammatory bowel disease in adults. Gut 2011, 60, 571–607. [Google Scholar] [CrossRef] [PubMed]
- Nasseri-Moghaddam, S. Inflammatory bowel disease. Middle East J. Digestive. Dis. 2012, 4, 77–89. [Google Scholar]
- Moss-Morris, R. Adjusting to chronic illness: Time for a unified theory. Br. J. Health Psychol. 2013, 18, 681–686. [Google Scholar] [CrossRef] [PubMed]
- Sammut, J.; Scerri, J.; Xuereb, R.B. The lived experience of adults with ulcerative colitis. J. Clin. Nurs. 2015, 24, 2659–2667. [Google Scholar] [CrossRef] [PubMed]
- Massuger, W.; Moore, G.T.C.; Andrews, J.M.; Kilkenny, M.F.; Reyneke, M.; Knowles, S.; Purcell, L.; Alex, G.; Buckton, S.; Page, A.T.; et al. Crohn’s & Colitis Australia inflammatory bowel disease audit: Measuring the quality of care in Australia. Intern. Med. J. 2019, 49, 859–866. [Google Scholar]
- Mikocka-Walus, A.; Massuger, W.; Knowles, S.R.; Moore, G.T.; Buckton, S.; Connell, W.; Pavli, P.; Raven, L.; Andrews, J.M. Quality of Care in Inflammatory Bowel Disease: Actual Health Service Experiences Fall Short of the Standards. Intern. Med. J. 2019. [Google Scholar] [CrossRef]
- Crohn’s Colitis Australia Inflammtory Bowel Disease Audit—Final Report of the First Audit of the Organisation and Provision of IBD Services in Australia. 2016. Available online: https://www.crohnsandcolitis.com.au/site/wp-content/uploads/Final_Web_Audit_17-Updated-3-Feb-2.pdf (accessed on 9 May 2019).
- Bennett, A.L.; Moore, D.; Bampton, P.A.; Bryant, R.V.; Andrews, J.M. Outcomes and patients’ perspectives of transition from paediatric to adult care in inflammatory bowel disease. World J. Gastroenterol. 2016, 22, 2611–2620. [Google Scholar] [CrossRef]
- Daniel, J.M. Young adults’ perceptions of living with chronic inflammatory bowel disease. Gastroenterol. Nurs. 2002, 25, 83–94. [Google Scholar] [CrossRef]
- Morrison, G.; Headon, B.; Gibson, P. Update in inflammatory bowel disease. Aust. Fam. Physician 2009, 38, 956–961. [Google Scholar]
- Mikocka-Walus, A.; Knowles, S.R.; Keefer, L.; Graff, L. Controversies Revisited: A Systematic Review of the Comorbidity of Depression and Anxiety with Inflammatory Bowel Diseases. Inflamm. Bowel Dis. 2016, 22, 752–762. [Google Scholar] [CrossRef]
- Regueiro, M.; Click, B.; Holder, D.; Shrank, W.; McAnallen, S.; Szigethy, E. Constructing an Inflammatory Bowel Disease Patient-Centered Medical Home. Clin. Gastroenterol. Hepatol. 2017, 15, 1148–1153. [Google Scholar] [CrossRef] [PubMed]
- Regueiro, M.; Greer, J.B.; Szigethy, E. Etiology and Treatment of Pain and Psychosocial Issues in Patients with Inflammatory Bowel Diseases. Gastroenterology 2017, 152, 430–439. [Google Scholar] [CrossRef] [PubMed]
- Prasad, S.S.; Potter, M.; Keely, S.; Talley, N.J.; Walker, M.M.; Kairuz, T. Roles of healthcare professionals in the management of chronic gastrointestinal diseases with a focus on primary care: A systematic review. JGH Open Open Access J. Gastroenterol. Hepatol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Crohn’s Colitis Australia (CCA). Australian IBD Standards: Standards of Healthcare for People with Inflammatory Bowel Disease in Australia. Available online: https://www.crohnsandcolitis.com.au/site/wp-content/uploads/IBD-Standards-Final.pdf (accessed on 9 May 2019).
- Gastroenterological Society of Australia Inflammatory Bowel Disease Clinical Update Fourth Edition Updated 2018. Available online: https://www.gesa.org.au/resources/clinical-guidelines-and-updates/inflammatory-bowel-disease/ (accessed on 8 September 2019).
- Lamb, C.A.; Kennedy, N.A.; Raine, T.; Hendy, P.A.; Smith, P.J.; Limdi, J.K.; Hayee, B.; Lomer, M.C.E.; Parkes, G.C.; Selinger, C.; et al. British Society of Gastroenterology consensus guidelines on the management of inflammatory bowel disease in adults. Gut 2019, 68 (Suppl. 3), s1–s106. [Google Scholar] [CrossRef] [PubMed]
- Royal College of Physicians UK. A Summary of the UK Inflammatory Bowel Disease Audit 2014. Available online: https://www.rcplondon.ac.uk/file/2441/download?token=aBn5fr4g (accessed on 9 May 2019).
- Ashok, K.; Mathew, A.; Thomas, A.; Mohan, D.; Gopalakrishna, R.; Reghu, R. Clinical Pharmacist’s Interventions on Medication Adherence and Knowledge of Inflammatory Bowel Disease Patients. J. Young Pharm. 2017, 9, 381–385. [Google Scholar] [CrossRef]
- Rentsch, C.; Ward, M.; Heerasing, G.; Headon, B.; Friedman, A.; Taylor, K. The role of a pharmacist in the inflammatory bowel disease clinic. J. Gastroenterol. Hepatol. 2015, 30, 176–192. [Google Scholar]
- Tiao, D.K.; Chan, W.; Jeganathan, J.; Chan, J.T.; Perry, J.; Selinger, C.P.; Leong, R.W. Inflammatory Bowel Disease Pharmacist Adherence Counseling Improves Medication Adherence in Crohn’s Disease and Ulcerative Colitis. Inflamm. Bowel Dis. 2017, 23, 1257–1261. [Google Scholar] [CrossRef]
- Andrews, J.M.; Mountifield, R.E.; Van Langenberg, D.R.; Bampton, P.A.; Holtmann, G.J. Un-promoted issues in inflammatory bowel disease: Opportunities to optimize care. Intern. Med. J. 2010, 40, 173–182. [Google Scholar] [CrossRef]
- Clement, C.; Rapport, F.; Seagrove, A.; Alrubaiy, L.; Williams, J. Healthcare professionals’ views of the use and administration of two salvage therapy drugs for acute ulcerative colitis: A nested qualitative study within the CONSTRUCT trial. BMJ Open 2017, 7, e014512. [Google Scholar] [CrossRef]
- Mikocka-Walus, A.; Andrews, J.M.; Rampton, D.; Goodhand, J.; van der Woude, J.; Bernstein, C.N. How can we improve models of care in inflammatory bowel disease? An international survey of IBD health professionals. J. Crohn’s Colitis 2014, 8, 1668–1674. [Google Scholar] [CrossRef]
- Tan, M.; Holloway, R.H.; Lange, K.; Andrews, J.M. General practitioners’ knowledge of and attitudes to inflammatory bowel disease. Intern. Med. J. 2012, 42, 801–807. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. What can “thematic analysis” offer health and wellbeing researchers? Int. J. Qual. Stud. Health Well-Being 2014, 9, 26152. [Google Scholar] [CrossRef]
- Gikas, A.; Triantafillidis, J.K. The role of primary care physicians in early diagnosis and treatment of chronic gastrointestinal diseases. Int. J. Gen. Med. 2014, 7, 159–173. [Google Scholar] [CrossRef] [PubMed]
- Bennett, A.L.; Munkholm, P.; Andrews, J.M. Tools for primary care management of inflammatory bowel disease: Do they exist? World J. Gastroenterol. 2015, 21, 4457–4465. [Google Scholar] [CrossRef] [PubMed]
- Larussa, T.; Suraci, E.; Marasco, R.; Imeneo, M.; Dumitrascu, D.L.; Abenavoli, L.; Luzza, F. Barriers And Facilitators In Conducting Clinical Trials In Inflammatory Bowel Disease: A Monocentric Italian Survey. Rev. Recent Clin. Trials 2020. [Google Scholar] [CrossRef]
- Ravikoff, J.E.; Cole, E.B.; Korzenik, J.R. Barriers to enrollment in inflammatory bowel disease randomized controlled trials: An investigation of patient perspectives. Inflamm. Bowel Dis. 2012, 18, 2092–2098. [Google Scholar] [CrossRef]
- George, P.P.; Molina, J.A.; Cheah, J.; Chan, S.C.; Lim, B.P. The evolving role of the community pharmacist in chronic disease management—A literature review. Ann. Acad. Med. Singap. 2010, 39, 861–867. [Google Scholar]
- Blouin, R.A.; Adams, M.L. The Role of the Pharmacist in Health Care: Expanding and Evolving. N. Carol. Med. J. 2017, 78, 165–167. [Google Scholar] [CrossRef]
- International Pharmaceutical Federation (FIP). Beating Non-Communicable Diseases in the Community—The Contributions of Pharmacists. Available online: https://www.fip.org/files/fip/publications/NCDs/beating-ncds-in-the-community-the-contribution-of-pharmacists.pdf (accessed on 4 June 2019).
- Tan, E.C.; Stewart, K.; Elliott, R.A.; George, J. Pharmacist services provided in general practice clinics: A systematic review and meta-analysis. Res. Soc. Adm. Pharm. 2014, 10, 608–622. [Google Scholar] [CrossRef]
- Koliani-Pace, J.L.; Haron, A.M.; Zisman-Ilani, Y.; Thompson, K.D.; Siegel, C.A. Patients’ Perceive Biologics to Be Riskier and More Dreadful Than Other IBD Medications. Inflamm. Bowel Dis. 2019. [Google Scholar] [CrossRef]
- Holt, D.Q.; Strauss, B.J.; Moore, G.T. Patients with inflammatory bowel disease and their treating clinicians have different views regarding diet. J. Hum. Nutr. Diet. 2017, 30, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Rubin, D.T.; Dubinsky, M.C.; Martino, S.; Hewett, K.A.; Panes, J. Communication between Physicians and Patients with Ulcerative Colitis: Reflections and Insights from a Qualitative Study of In-Office Patient-Physician Visits. Inflamm. Bowel Dis. 2017, 23, 494–501. [Google Scholar] [CrossRef] [PubMed]
- Freeman, C.; Rigby, D.; Aloizos, J.; Williams, I. The practice pharmacist: A natural fit in the general practice team. Aust. Prescr. 2016, 39, 211–214. [Google Scholar] [CrossRef] [PubMed]

| Description | Questions |
|---|---|
| Free-text questions | What would you like to learn more about IBD? |
| What would be barriers to your learning? | |
| Non-free text question | How likely are you to attend a similar education session on IBD in the future? |
| Confidence Statements | |
|---|---|
| Pre-session statement 1 | I am confident with my understanding of IBD and its management. |
| Post-session 1a | Identifying signs and symptoms of inflammatory bowel disease (IBD). |
| 1b | Distinguishing IBD from other gastrointestinal diseases. |
| 1c | Recognising when referral is required. |
| Pre-session statement 2 | I am able to provide relevant information about IBD and its management. |
| Post-session 2 | Providing advice to patients on the management of IBD. |
| Pre-session statement 3 | I am confident in making decisions with IBD patients about their care. |
| Post-session 3 | Reviewing/monitoring current treatments and provide guidance and tailored information on adherence and compliance. |
| Pre-session statement 4 | I am able to provide additional support in managing patients with IBD. |
| Post-session 4 | Accessing relevant resources on IBD in primary care. |
| Pre-session statement 5 | I feel confident in addressing the needs of IBD patient’s regarding their condition and treatment. |
| Post-session 5 | Addressing the needs of IBD patients regarding their condition and treatment. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Prasad, S.S.; Keely, S.; Talley, N.J.; Kairuz, T.; Walker, M.M. Pharmacists’ Confidence in Managing Patients with Inflammatory Bowel Disease. Pharmacy 2020, 8, 68. https://doi.org/10.3390/pharmacy8020068
Prasad SS, Keely S, Talley NJ, Kairuz T, Walker MM. Pharmacists’ Confidence in Managing Patients with Inflammatory Bowel Disease. Pharmacy. 2020; 8(2):68. https://doi.org/10.3390/pharmacy8020068
Chicago/Turabian StylePrasad, Sharmila S., Simon Keely, Nicholas J. Talley, Therése Kairuz, and Marjorie M. Walker. 2020. "Pharmacists’ Confidence in Managing Patients with Inflammatory Bowel Disease" Pharmacy 8, no. 2: 68. https://doi.org/10.3390/pharmacy8020068
APA StylePrasad, S. S., Keely, S., Talley, N. J., Kairuz, T., & Walker, M. M. (2020). Pharmacists’ Confidence in Managing Patients with Inflammatory Bowel Disease. Pharmacy, 8(2), 68. https://doi.org/10.3390/pharmacy8020068







