Antibiotic Stewardship in Community Pharmacies: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Step 1: Identification and Development of Research Question
- (a)
- What are the perceptions of community pharmacists towards antibiotic dispensing?
- (b)
- What are the attitudes of community pharmacists towards antibiotic dispensing?
- (c)
- How frequently did community pharmacists sell antibiotics in community pharmacies?
- (d)
- How often did customers demand antibiotics in community pharmacies?
- (e)
- What is the suitability of antibiotics that were dispensed from community pharmacies?
2.2. Step 2: Relevant Literature Identification
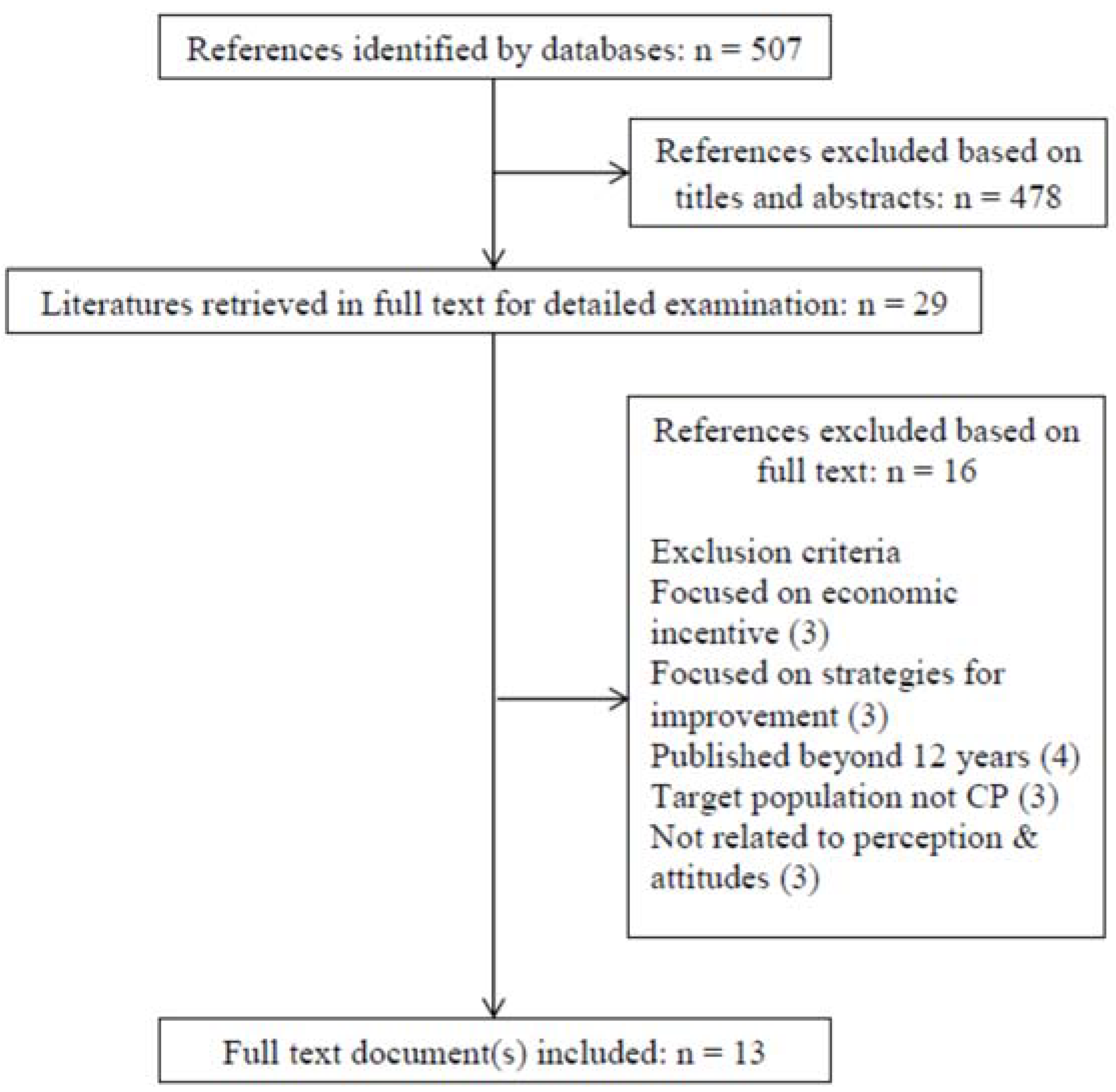
2.3. Step 3: Screening and Selection of Relevant Literature
2.4. Step 4: Data Charting
2.5. Step 5: Analyzing, Summarizing, and Reporting Results
3. Results
3.1. Awareness and Perception towards Antibiotic Dispensing
3.2. Attitudes of Pharmacists towards Antibiotic Dispensing
3.2.1. Patient/Customer Demand
3.2.2. Revenue/Profit/Sales/Business Reasons
3.2.3. Doctor/Health Facility Prescription
3.3. Commonly Dispensed Antibiotics
3.4. Simulated Patients/Simulated Clients/Voluntary Collaborators
4. Discussion
5. Conclusions
Funding
Author Contributions
Acknowledgments
Conflicts of Interest
References
- De Kraker, M.E.A.; Davey, P.G.; Grundmann, H.; BURDEN Study Group. Mortality and hospital stay associated with resistant Staphylococcus aureus and Escherichia coli bacteremia: Estimating the burden of antibiotic resistance in Europe. PLoS Med. 2011, 8, e1001104. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States, 2013. Available online: https://www.cdc.gov/drugresistance/threat-report-2013/pdf/ar-threats-2013-508.pdf#page=11 (accessed on 29 May 2018).
- World Health Organization. Antimicrobial Resistance: Global Report on Surveillance 2014. Available online: http://www.who.int/drugresistance/documents/surveillancereport/en/ (accessed on 29 May 2018).
- World Health Organization. Global Tuberculosis Report 2015. Available online: www.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf (accessed on 29 May 2018).
- Centers for Disease Dynamics Economics and Policy. The State of the World’s Antibiotics 2015. Available online: https://www.cddep.org/wp-content/uploads/2017/06/swa_executive_summary_edits_2016.pdf (accessed on 29 May 2018).
- European Antimicrobial Resistance Surveillance Network (EARSNet). EARS-Net Report Quarters 1–4 Dublin 2014. Available online: https://www.hpsc.ie/a-z/microbiologyantimicrobialresistance/europeanantimicrobialresistancesurveillancesystemearss/earsssurveillancereports/2014reports/File,14686,en.pdf (accessed on 29 May 2018).
- Public Health Agency of Canada. Canadian Antimicrobial Resistance Surveillance System Report 2015 Ottawa. Available online: https://www.researchid.com/wp-content/uploads/2018/02/2015_antimicrobial-surveillance-antimicrobioresistance-eng.pdf (accessed on 29 May 2018).
- Kariuki, S.; Dougan, G. Antibacterial resistance in sub-Saharan Africa: An underestimated emergency. Ann. N. Y. Acad. Sci. 2014, 1323, 43–55. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization (PAHO). Forthcoming. Informe Anual de la Red de Monitoreo/Vigilancia de la Resistencia a los Antibióticos y de Infecciones Asociadas a la Atención de la Salud 2014. Washington. Available online: https://www.paho.org/hq/index.php?option=com_topics&view=article&id=7&Itemid=40740&lang=en (accessed on 25 May 2018).
- Lu, P.-L.; Liu, Y.-C.; Toh, H.-S.; Lee, Y.-L.; Liu, Y.-M.; Ho, C.-M.; Huang, C.-C.; Liu, C.-E.; Ko, W.-C.; Wang, J.-H.; et al. Epidemiology and antimicrobial susceptibility profiles of Gram-negative bacteria causing urinary tract infections in the Asia-Pacific region: 2009–2010 results from the Study for Monitoring Antimicrobial Resistance Trends (SMART). Int. J. Antimicrob. Agents 2012, 40, S37–S43. [Google Scholar] [CrossRef]
- Ventola, C.L. The antibiotic resistance crisis: Part 1: Causes and threats. Pharm. Ther. 2015, 40, 277–283. [Google Scholar]
- Morgan, D.J.; Okeke, I.N.; Laxminarayan, R.; Perencevich, E.N.; Weisenberg, S. Nonprescription antimicrobial use worldwide: A systematic review. Lancet Infect. Dis. 2011, 11, 692–701. [Google Scholar] [CrossRef]
- Okeke, I.N.; Laxminarayan, R.; Bhutta, Z.A.; Duse, A.G.; Jenkins, P.; O’Brien, T.F.; Pablos-Mendez, A.; Klugman, K.P. Antimicrobial resistance in developing countries. Part I: Recent trends and current status. Lancet Infect. Dis. 2005, 5, 481–493. [Google Scholar] [CrossRef]
- Zoorob, R.; Grigoryan, L.; Nash, S.; Trautner, B.W. Nonprescription Antimicrobial Use in a Primary Care Population in the United States. Antimicrob. Agents Chemother. 2016, 60, 5527–5532. [Google Scholar] [CrossRef] [PubMed]
- The Alliance for the Prudent Use of Antibiotics. Executive summary: Select findings, conclusions, and policy recommendations. Clin. Infect. Dis. 2005, 41, S224–S227. [Google Scholar] [CrossRef] [PubMed]
- Gebretekle, G.B.; Serbessa, M.K. Exploration of over the counter sales of antibiotics in community pharmacies of Addis Ababa, Ethiopia: Pharmacy professionals’ perspective. Antimicrob. Resist. Infect. Control 2016, 5, 2. [Google Scholar] [CrossRef] [PubMed]
- Dillip, A.; Embrey, M.; Shekalaghe, E.; Ross-Degnan, D.; Vialle-Valentin, C.; Kimatta, S.; Liana, J.; Rutta, E.; Valimba, R.; Chalker, J. What motivates antibiotic dispensing in accredited drug dispensing outlets in Tanzania? A qualitative study. Antimicrob. Resist. Infect. Control 2015, 4, 30. [Google Scholar] [CrossRef] [PubMed]
- Hadi, M.A.; Karami, N.A.; Al-Muwalid, A.S.; Al-Otabi, A.; Al-Subahi, E.; Bamomen, A.; Mohamed, M.M.A.; Elrggal, M.E. Community pharmacists’ knowledge, attitude, and practices towards dispensing antibiotics without prescription (DAwP): A cross-sectional survey in Makkah Province, Saudi Arabia. Int. J. Infect. Dis. 2016, 47, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Zapata-Cachafeiro, M.; González-González, C.; Váquez-Lago, J.M.; López-Vázquez, P.; López-Durán, A.; Smyth, E.; Figueiras, A. Determinants of antibiotic dispensing without a medical prescription: A cross-sectional study in the north of Spain. J. Antimicrob. Chemother. 2014, 69, 3156–3160. [Google Scholar] [CrossRef] [PubMed]
- Almaaytah, A.; Mukattash, T.L.; Hajaj, J. Dispensing of non-prescribed antibiotics in Jordan. Patient Prefer. Adherence 2015, 9, 1389–1395. [Google Scholar] [CrossRef] [PubMed]
- Llor, C.; Cots, J.M. The Sale of antibiotics without prescription in pharmacies in Catalonia, Spain. Clin. Infect. Dis. 2009, 48, 1345–1349. [Google Scholar] [CrossRef] [PubMed]
- Plachouras, D.; Kavatha, D.; Antoniadou, A.; Giannitsioti, E.; Poulakou, G.; Kanellakopoulou, K.; Giamarellou, H. Dispensing of antibiotics without prescription in Greece, 2008: Another link in the antibiotic resistance chain. Eurosurveillance 2010, 15, 19488. [Google Scholar] [CrossRef] [PubMed]
- Bin Abdulhak, A.A.; Al Tannir, M.A.; Almansor, M.A.; Almohaya, M.S.; Onazi, A.S.; Marei, M.A.; Aldossary, O.F.; Obeidat, S.A.; Obeidat, M.A.; Riaz, M.S.; et al. Non prescribed sale of antibiotics in Riyadh, Saudi Arabia: A Cross sectional study. BMC Public Health 2011, 11, 538. [Google Scholar] [CrossRef] [PubMed]
- Diwan, V.; Sabde, Y.D.; Byström, E.; Costa, A.D. Treatment of pediatric diarrhea: A simulated client study at private pharmacies of Ujjain, Madhya Pradesh, India. J. Infect. Dev. Ctries. 2015, 9, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Roque, F.; Soares, S.; Breitenfeld, L.; López-Durán, A.; Figueiras, A.; Herdeiro, M.T. Attitudes of community pharmacists to antibiotic dispensing and microbial resistance: A qualitative study in Portugal. Int. J. Clin. Pharm. 2013, 35, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Shet, A.; Sundaresan, S.; Forsberg, B.C. Pharmacy-based dispensing of antimicrobial agents without prescription in India: Appropriateness and cost burden in the private sector. Antimicrob. Resist. Infect. Control 2015, 4, 55. [Google Scholar] [CrossRef] [PubMed]
- Alabid, A.H.M.A.; Ibrahim, M.I.M.; Hassali, M.A. Antibiotics Dispensing for URTIs by Community Pharmacists (CPs) and General Medical Practitioners in Penang, Malaysia: A Comparative Study using Simulated Patients (SPs). J. Clin. Diagn. Res. 2014, 8, 119–123. [Google Scholar] [CrossRef] [PubMed]
- Roque, F.; Soares, S.; Breitenfeld, L.; Figueiras, A.; Herdeiro, M.T. Influence of Community Pharmacists’ Attitudes on Antibiotic Dispensing Behavior: A Cross-sectional Study in Portugal. Clin. Ther. 2015, 37, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Society for Healthcare Epidemiology of America; Infectious Diseases Society of America; Pediatric Infectious Diseases Society. Policy Statement on antimicrobial stewardship by the Society for Healthcare Epidemiology of America (SHEA), the Infectious Diseases Society of America (IDSA), and the Pediatric Infectious Diseases Society (PIDS). Infect. Control Hosp. Epidemiol. 2012, 33, 322–327. [Google Scholar] [CrossRef] [PubMed]
- American Society of Health-System Pharmacists. ASHP Statement on the pharmacist’s role in antimicrobial stewardship and infection prevention and control. Am. J. Health Syst. Pharm. 2010, 67, 575–577. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Levac, D.; Colquhoun, H.; O’Brien, K.K. Scoping studies: Advancing the methodology. Implement. Sci. 2010, 5, 69. [Google Scholar] [CrossRef] [PubMed]
- Madden, J.M.; Quick, J.D.; Ross-Degnan, D.; Kafle, K.K. Undercover careseekers: Simulated clients in the study of health provider behavior in developing countries. Soc. Sci. Med. 1997, 45, 1465–1482. [Google Scholar] [CrossRef]
- Muñoz, E.B.; Dorado, M.F.; Guerrero, J.E.; Martínez, F.M. The effect of an educational intervention to improve patient antibiotic adherence during dispensing in a community pharmacy. Aten. Primaria 2014, 46, 367–375. [Google Scholar] [CrossRef] [PubMed]
- Sá Del Fiol, F.; Sá Del Fiol, F.; Gerenutti, M.; Groppo, F.C. Antibiotics and pregnancy. Die Pharm. Int. J. Pharm. Sci. 2005, 60, 483–493. [Google Scholar] [CrossRef]
- Rettig, E.; Tunkel, D.E. Contemporary concepts in management of acute otitis media in children. Otolaryngol. Clin. N. Am. 2014, 47, 651–672. [Google Scholar] [CrossRef] [PubMed]
- Essack, S.; Bell, J.; Shephard, A. Community pharmacists—Leaders for antibiotic stewardship in respiratory tract infection. J. Clin. Pharm. Ther. 2018, 43, 302–307. [Google Scholar] [CrossRef] [PubMed]
- McCullough, A.R.; Rathbone, J.; Parekh, S.; Hoffmann, T.C.; Del Mar, C.B. Not in my backyard: A systematic review of clinicians’ knowledge and beliefs about antibiotic resistance. J. Antimicrob. Chemother. 2015, 70, 2465–2473. [Google Scholar] [CrossRef] [PubMed]
| Author, Year, [Ref.] | Study Type Study Tool | Study Participants Study Site Sampling | Aims/Objectives | Study Findings | Conclusion Limitation |
|---|---|---|---|---|---|
| Dillip, 2015, [17] | Qualitative; In-depth interviews | Accredited drug dispensing outlet (ADDO) owners and dispensers; Tanga and Ruvuma; Tanzania purposive interviews (7) | Exploring attitudes towards antibiotic dispensing; Accreditation influence on dispensing | Good knowledge but low implementation; Customer demand Profit margin; Habit to follow doctors’ prescriptions | Positive influence of ADDO Program but absence of translation into practice; Nongeneralizable sample Social desirability bias |
| Zapata, 2014, [19] | Cross-sectional Self-administered questionnaire | 286 Community pharmacists (CPs) Spain Exhaustive sampling | Interpretation of knowledge and attitudes for DAwMP | Positive relationship with DAwMP; Indifferent attitude, complacency; Insufficient knowledge | Strong relationship with DAwMP; Nonresponse bias; Inappropriate validity criterion |
| Gebretekle, 2016, [16] | Phenomenological qualitative; In-depth interviews Observation | Five CPs Ethiopia | Exploring reasons—OTC antibiotics sales | Frequent DAwMP; Weak enforcement regulation; Customer demand, profit margin | OTC antibiotic sales-common practice; Strict regulatory enforcement; Educational campaigns; Non-generalizable sample |
| Hadi, 2015, [18] | Cross-sectional; Self-administered questionnaire | 189 CPs Makkah, Saudi Arabia | Exploring knowledge, attitude, practices towards DAwMP | Insufficient knowledge of legality; Knowledgeable of consequences of DAwMP Patient unwillingness to consult doctors; Unaffordability of doctors’ consultations | Ignorant of DAwMP as illegal Educational interventions; Single study setting (Makkah); Non-generalizable; Social desirability bias |
| Almaytah, 2015, [20] | Prospective design; Five clinical scenarios (SPs) | 202 pharmacies Jordan | Assessing knowledge of viral symptoms; DAwMP | Unnecessary dispensing for sore throat and UTI; Insufficient knowledge of duration of treatment; Antibiotic dispensing refusal | Absence of abidance of national regulation |
| Llor, 2009, [21] | Prospective design; Three clinical scenarios (SPs) | 197 pharmacies Spain | Exploring the attitude for DAwMP; Quantifying the extent of DAwMP | Unnecessary dispensing for sore throat and acute bronchitis; Recommended consultation | Though illegal DAwMP observed; Not confirmed whether community pharmacist dispensing |
| Plachouras, 2010, [22] | Prospective design; 21 voluntary collaborators | 174 pharmacies Greece | Quantifying the extent of DAwMP | Huge and easy dispensing Amoxicillin/clavulanate and ciprofloxacin largely requested | Despite implementation of restriction ciprofloxacin dispensed; Educational strategies for pharmacists; Need of strong regulation enforcement |
| Abdulhak, 2011, [23] | Cross-sectional; SPs | 327 pharmacies Saudi Arabia Quasi-random | Exploring DAwMP; Exploring associated risks | DAwMP observed without patients’ requests for sore throat and diarrhea; Improper history-taking | DAwMP routinely observed; Requirement of stringent enforcement and compliance to regulations |
| Alabid, 2014, [27] | Cross-sectional; SPs | 50 pharmacies Malaysia Convenient | Investigating antibiotic dispensing for (upper respiratory tract infections) URTIs | Noncompliance rational use of drug concept (RUD) by WHO | Irrational antibiotic dispensing; Polypharmacy; Nonrepresentative sample |
| Diwan, 2015, [24] | Cross-sectional; Simulated clients (SCs) | 164 pharmacies India | Investigating treatment of childhood diarrhea | DAwMP with antimotility agents and probiotics; Actual treatment (oral rehydration salt) | Highly inappropriate treatment; Actual treatment under-dispensed; Not confirmed whether community pharmacist dispensing |
| Shet, 2015, [26] | Cross-sectional; Two clinical scenarios (SPs) | 261 pharmacies India | Exploring frequency of DAwMP | Frequent DAwMP; Inappropriate management for URTI and self-limiting illnesses | Highly undesirable DAwMP; Not confirmed whether community pharmacist dispensing |
| Roque, 2013, [25] | Exploratory qualitative; Semi-structured interviews (six focus groups) | 32 CPs Portugal | Exploring the knowledge, perception and attitude | Knowledgeable about rational dispensing and antibiotic resistance; Factors: Physicians and patients and veterinary consumption for antibiotic resistance | Fair improvement chances; Behavioral intention for expected change; Non-generalizable sample; Chances of bias in FGD |
| Roque, 2015, [28] | Cross-sectional; Self-administered questionnaire | 770 CPs Portugal | Evaluating DAwMP; Attitude towards DAwMP | Frequent DAwMP-dental ailments and UTIs; Factors: Patient satisfaction, precaution, and fear for DAwMP | Attitudes promotes DAwMP; Educational interventions; Nonresponse bias; Social desirability |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jamshed, S.; Padzil, F.; Shamsudin, S.H.; Bux, S.H.; Jamaluddin, A.A.; Bhagavathula, A.S.; Azhar, S.; Hassali, M.A. Antibiotic Stewardship in Community Pharmacies: A Scoping Review. Pharmacy 2018, 6, 92. https://doi.org/10.3390/pharmacy6030092
Jamshed S, Padzil F, Shamsudin SH, Bux SH, Jamaluddin AA, Bhagavathula AS, Azhar S, Hassali MA. Antibiotic Stewardship in Community Pharmacies: A Scoping Review. Pharmacy. 2018; 6(3):92. https://doi.org/10.3390/pharmacy6030092
Chicago/Turabian StyleJamshed, Shazia, Fadzlan Padzil, Siti Hadijah Shamsudin, Siti Halimah Bux, Abdul Aziz Jamaluddin, Akshaya Srikanth Bhagavathula, Saira Azhar, and Mohamed Azmi Hassali. 2018. "Antibiotic Stewardship in Community Pharmacies: A Scoping Review" Pharmacy 6, no. 3: 92. https://doi.org/10.3390/pharmacy6030092
APA StyleJamshed, S., Padzil, F., Shamsudin, S. H., Bux, S. H., Jamaluddin, A. A., Bhagavathula, A. S., Azhar, S., & Hassali, M. A. (2018). Antibiotic Stewardship in Community Pharmacies: A Scoping Review. Pharmacy, 6(3), 92. https://doi.org/10.3390/pharmacy6030092






