Polypharmacy and Medication-Related Problems in Hemodialysis Patients: A Call for Deprescribing
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Setting
2.2. Study Population
2.3. Methods
- (1)
- Minor: Limited clinical effects and does not require therapy modification
- (2)
- Moderate: The interaction may result in the exacerbation of the patient’s condition and/or requires therapy modification
- (3)
- Major: The interaction may be life-threatening and/or requires medical intervention to minimize or prevent serious adverse events
- (4)
- Contraindicated: The drugs are contraindicated for current use
2.4. Study Outcomes
2.5. Sample Size
2.6. Statistical Analysis
2.7. Ethics
3. Results
3.1. Population
3.2. Baseline Characteristics
3.3. Study Outcomes
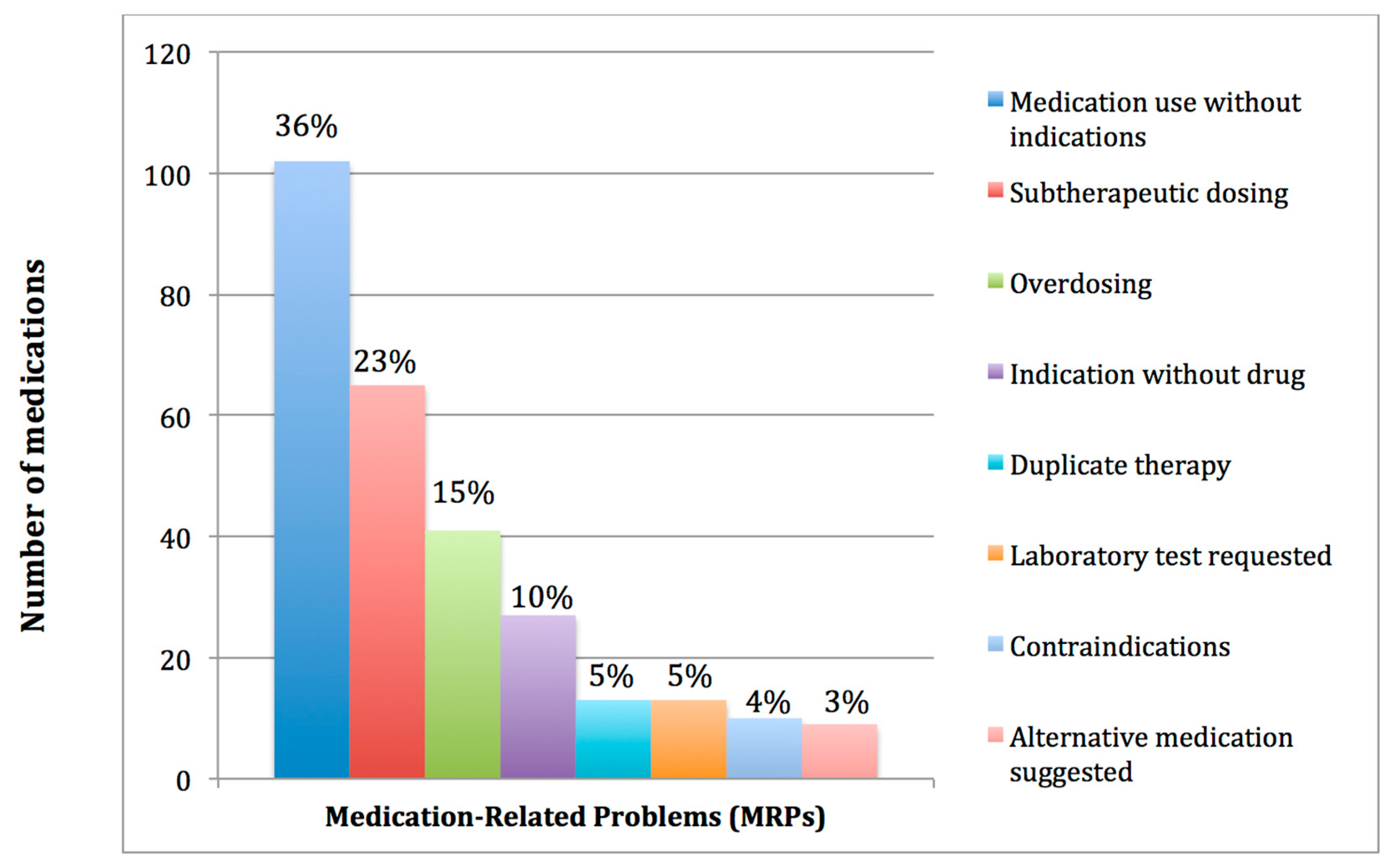
3.3.1. Primary Endpoint
3.3.2. Secondary Endpoints
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Central for Disease Control and Prevention, Chronic kidney Disease Survillence System. Available online: https://nccd.cdc.gov/ckd/ (accessed on 25 November 2017).
- Health indicators for renal replacement therapy in Saudi Arabia. Available online: http://www.sjkdt.org/article.asp?issn=1319-2442;year=2018;volume=29;issue=1;spage=225;epage=231;aulast= (accessed on 24 July 2018).
- Dialysis in the kingdom of Saudi Arabia. Saudi J. Kidney Dis. Transplant. 2017, 28, 949–957.
- Fink, J.C.; Chertow, G.M. Medication errors in chronic kidney disease: One piece in the patient safety puzzle. Kidney Int. 2009, 76, 1123–1125. [Google Scholar] [CrossRef] [PubMed]
- Al-Sayyari, A.A.; Shaheen, F.A. End stage chronic kidney disease in saudi arabia. A rapidly changing scene. Saudi Med. J. 2011, 32, 339–346. [Google Scholar] [PubMed]
- Rifkin, D.E.; Laws, M.B.; Rao, M.; Balakrishnan, V.S.; Sarnak, M.J.; Wilson, I.B. Medication adherence behavior and priorities among older adults with ckd: A semistructured interview study. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2010, 56, 439–446. [Google Scholar] [CrossRef] [PubMed]
- Chapin, E.; Zhan, M.; Hsu, V.D.; Seliger, S.L.; Walker, L.D.; Fink, J.C. Adverse safety events in chronic kidney disease: The frequency of “multiple hits”. Clin. J. Am. Soc. Nephrol. 2010, 5, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Milton, J.C.; Jackson, S.H. Inappropriate polypharmacy: Reducing the burden of multiple medication. Clin. Med. 2007, 7, 514–517. [Google Scholar] [CrossRef]
- Weir, M.R.; Fink, J.C. Safety of medical therapy in patients with chronic kidney disease and end-stage renal disease. Curr. Opin. Nephrol. Hypertens. 2014, 23, 306–313. [Google Scholar] [CrossRef] [PubMed]
- Cardone, K.E.; Bacchus, S.; Assimon, M.M.; Pai, A.B.; Manley, H.J. Medication-related problems in CKD. Adv. Chronic Kidney Dis. 2010, 17, 404–412. [Google Scholar] [CrossRef] [PubMed]
- Multidisciplinary team care for CKD-MBD. Achieving KDIGO guideline recommendations in the bundling era. Available online: https://www.ncbi.nlm.nih.gov/pubmed/24960985 (accessed on 24 July 2018).
- Mair, A.; Fernandez-Llimos, F. Polypharmacy management programmes: The SIMPATHY project. Eur. J. Hosp. Pharm. 2017, 24, 5–6. [Google Scholar] [CrossRef]
- Alkatheri, A.M. Pharmacist effectiveness in reducing medication-related problems in dialysis patients. Saudi Pharm. J. 2004, 12, 54–59. [Google Scholar]
- Abrahams, R. Role of a pharmacist on the dialysis unit. Am. J. Health-Syst. Pharm. 2008, 65, 1218–1219. [Google Scholar] [CrossRef] [PubMed]
- Mason, N.A.; Bakus, J.L. Strategies for reducing polypharmacy and other medication-related problems in chronic kidney disease. Semin. Dial. 2010, 23, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Mason, N.A. Polypharmacy and medication-related complications in the chronic kidney disease patient. Curr. Opin. Nephrol. Hypertens. 2011, 20, 492–497. [Google Scholar] [CrossRef] [PubMed]
- Gheewala, P.; Peterson, G.; Curtain, C.; Nishtala, P.; Hannan, P.; Castelino, R. Impact of the pharmacist medication review services on drug-related problems and potentially inappropriate prescribing of renally cleared medications in residents of aged care facilities. Drugs Aging 2014, 31, 825–835. [Google Scholar] [CrossRef] [PubMed]
- Traynor, K. Pharmacists find satisfaction in dialysis clinics. Am. J. Health-Syst. Pharm. 2010, 67, 422–426. [Google Scholar] [CrossRef] [PubMed]
- Erickson, A.L.; Szumita, P.M.; Cotugno, M.C. Implementation of clinical pharmacy services in a dialysis unit. Am. J. Health-Syst. Pharm. 2008, 65, 2011–2013. [Google Scholar] [CrossRef] [PubMed]
- Manley, H.J.; Drayer, D.K.; Muther, R.S. Medication-related problem type and appearance rate in ambulatory hemodialysis patients. BMC Nephrol. 2003, 4, 10. [Google Scholar] [CrossRef] [PubMed]
- Manley, H.J.; Cannella, C.A.; Bailie, G.R.; St Peter, W.L. Medication-related problems in ambulatory hemodialysis patients: A pooled analysis. Am. J. Kidney Dis. 2005, 46, 669–680. [Google Scholar] [CrossRef] [PubMed]
- St Peter, W.L. Management of polypharmacy in dialysis patients. Semin. Dial. 2015, 28, 427–432. [Google Scholar] [CrossRef] [PubMed]
- Mirkov, S. Implementation of a pharmacist medication review clinic for haemodialysis patients. N. Z. Med. J. 2009, 122, 25–37. [Google Scholar] [PubMed]
- Belaiche, S.; Romanet, T.; Allenet, B.; Calop, J.; Zaoui, P. Identification of drug-related problems in ambulatory chronic kidney disease patients: A 6-month prospective study. J. Nephrol. 2012, 25, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Payne, R.A.; Avery, A.J.; Duerden, M.; Saunders, C.L.; Simpson, C.R.; Abel, G.A. Prevalence of polypharmacy in a Scottish primary care population. Eur. J. Clin. Pharmacol. 2014, 70, 575–581. [Google Scholar] [CrossRef] [PubMed]
- Al-Dadah, A.; Omran, J.; Nusair, M.B.; Dellsperger, K.C. Cardiovascular mortality in dialysis patients. Adv. Perit. Dial. 2012, 28, 56–59. [Google Scholar] [PubMed]
- Collins, A.J. Cardiovascular mortality in end-stage renal disease. Am. J. Med. Sci. 2003, 325, 163–167. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, C.; McQuillan, R.; Bell, C.; Battistella, M. Targeted deprescribing in an outpatient hemodialysis unit: A quality improvement study to decrease polypharmacy. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2017, 70, 611–618. [Google Scholar] [CrossRef] [PubMed]
- Pai, A.B.; Cardone, K.E.; Manley, H.J.; St Peter, W.L.; Shaffer, R.; Somers, M.; Mehrotra, R. Medication reconciliation and therapy management in dialysis-dependent patients: Need for a systematic approach. Clin. J. Am. Soc. Nephrol. 2013, 8, 1988–1999. [Google Scholar] [CrossRef] [PubMed]
- Ledger, S.; Choma, G. Medication reconciliation in hemodialysis patients. CANNT J. 2008, 18, 41–43. [Google Scholar] [PubMed]
| Baseline Characteristics | N = 83 a |
|---|---|
| Age, median (IQR) b | 63 (49–71) |
| Gender (Males) | 42 (51%) |
| Body mass index (kg/m2) c, median (IQR) | 23.87 (28.3–21.5) |
| Underlying cause of end stage kidney disease | |
| Hypertension | 17 (21%) |
| Diabetes | 11 (13%) |
| Diabetes and hypertension | 20 (24%) |
| Glomerular diseases | 2 (2%) |
| Other | 11 (13%) |
| Unknown | 22 (27%) |
| Number of comorbid conditions per patient, mean ± SD d | 3.14 ± 1.64 |
| Comorbidities e | |
| Hypertension | 77 (93%) |
| Diabetes Mellitus | 45 (54%) |
| Ischemic heart disease | 31 (37%) |
| Dyslipidemia | 21 (25%) |
| Cerebrovascular accident | 12 (15%) |
| Respiratory diseases | 11 (13%) |
| Thyroid disorders | 6 (7%) |
| Epilepsy | 6 (7%) |
| Hepatitis C virus infection | 5 (6%) |
| Heart failure | 5 (6%) |
| Gastrointestinal diseases | 5 (6%) |
| Atrial fibrillation | 4 (5%) |
| Peripheral vascular disease | 3 (4%) |
| Depression | 3 (4%) |
| Hepatitis B virus infection | 1 (1%) |
| Variable | Β b | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Age | 0.03 | −0.02, 0.08 | 0.278 |
| Gender | |||
| Female | Reference | - | - |
| Male | −1.39 | −2.90, −0.12 | 0.070 |
| Cause of hemodialysis | |||
| Unknown | Reference | - | - |
| Hypertension | 0.06 | −2.19, 2.06 | 0.952 |
| Diabetes | 2.00 | −0.72, 4.71 | 0.147 |
| Hypertension and Diabetes | 1.65 | −0.63, 3.93 | 0.152 |
| Glomerular disease | −0.91 | −5.78, 3.95 | 0.709 |
| Other | 0.06 | −2.45, 2.33 | 0.961 |
| Number of comorbid conditions | 1.16 | 0.45, 1.87 | 0.002 c |
| Hypertension | 0.12 | −3.06, 3.30 | 0.941 |
| Diabetes mellitus | −0.44 | −2.57, 1.69 | 0.680 |
| Ischemic heart disease | 3.03 | 1.27, 4.97 | 0.001 c |
| Cerebrovascular stroke | −0.33 | −2.68, 2.03 | 0.782 |
| Dyslipidemia | 0.00 | −2.02, 2.03 | 0.996 |
| Respiratory disease | 3.50 | 1.18, 5.84 | 0.004 c |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alshamrani, M.; Almalki, A.; Qureshi, M.; Yusuf, O.; Ismail, S. Polypharmacy and Medication-Related Problems in Hemodialysis Patients: A Call for Deprescribing. Pharmacy 2018, 6, 76. https://doi.org/10.3390/pharmacy6030076
Alshamrani M, Almalki A, Qureshi M, Yusuf O, Ismail S. Polypharmacy and Medication-Related Problems in Hemodialysis Patients: A Call for Deprescribing. Pharmacy. 2018; 6(3):76. https://doi.org/10.3390/pharmacy6030076
Chicago/Turabian StyleAlshamrani, Majed, Abdullah Almalki, Mohamed Qureshi, Oyindamola Yusuf, and Sherine Ismail. 2018. "Polypharmacy and Medication-Related Problems in Hemodialysis Patients: A Call for Deprescribing" Pharmacy 6, no. 3: 76. https://doi.org/10.3390/pharmacy6030076
APA StyleAlshamrani, M., Almalki, A., Qureshi, M., Yusuf, O., & Ismail, S. (2018). Polypharmacy and Medication-Related Problems in Hemodialysis Patients: A Call for Deprescribing. Pharmacy, 6(3), 76. https://doi.org/10.3390/pharmacy6030076






