Adverse Drug Reactions, Power, Harm Reduction, Regulation and the ADRe Profiles
Abstract
1. Introduction
2. Power via Prescribing
3. The Adverse Drug Reaction Problem
4. Antipsychotics, Challenging Behaviour and Older Adults in Care Homes
“… where you have somebody with behavioural or psychological problems relating to their dementia, to routinely prescribe an antipsychotic medication without looking at what is underpinning those behaviours and causing them is wrong, and it does seem to be the default position, which needs to be addressed.” Alzheimer’s Society Cymru, p. 17.
“It is quite simply unacceptable that antipsychotic medication is still being used as a primary response to ‘challenging’ behaviour across many residential care services.” Older People’s commissioner, Wales, p. 17.
“I’d like to see the circumstance whereby people are not caught in this dreadful repeat prescription mechanism, whereby it rolls on and on and on, and you could go for two years and nobody refers to it. Some GPs, some practices, are better at reviewing than others. But, theoretically, because you’re caught up in this repeat prescription mechanism, it could carry on and on and on. I’d like to see—if you’re prescribed an antipsychotic and you have a diagnosis of dementia, there should be a three-month mandatory review.” Care Forum Wales, p. 29.
What Should Be Done Differently?
5. Regulatory Interventions to Modify Prescribing and Outcomes
5.1. Actions
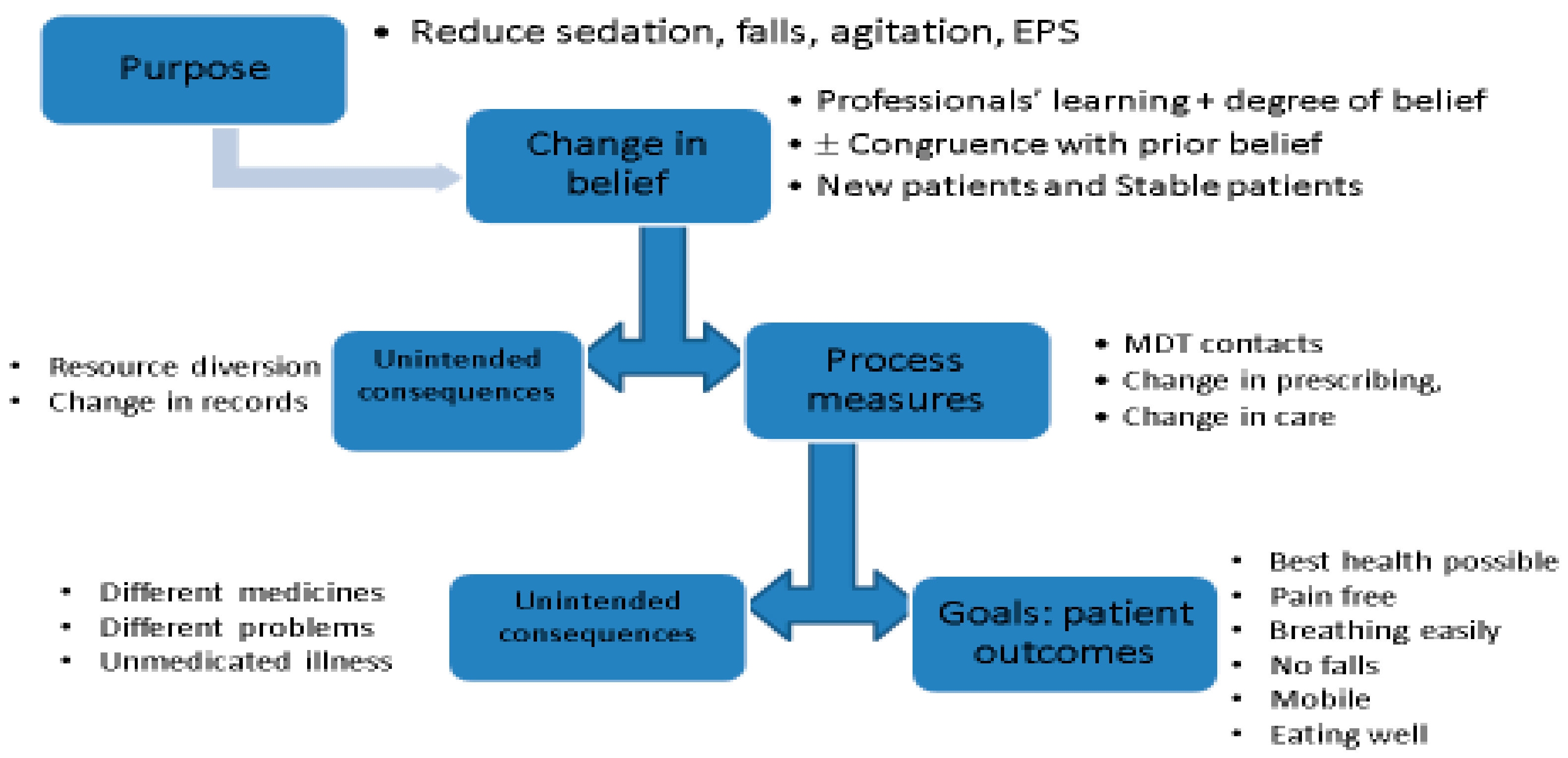
5.2. Change in Belief
Learning and Unintended Learning
5.3. Processes of Care
Unintended Processes
5.4. Outcomes of Care
Unintended Outcomes
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- McKinlay, J.B.; McKinlay, S.M. The Questionable Contribution of Medical Measures to the Decline of Mortality in the United States in the 20th Century. The Milbank Memorial Fund Quarterly. Health Soc. 1977, 55, 405–428. [Google Scholar]
- Weinshilboum, R.M. The Therapeutic Revolution. Clin. Pharmacol. Therap. 1987, 42, 481–484. [Google Scholar] [CrossRef]
- Cutler, D.M. Your Money or Your Life: Strong Medicine for America’s Health Care System; Oxford University Press: Oxford, UK, 2004. [Google Scholar]
- Lesch, J.E. The First Miracle Drugs: How the Sulfa Drugs Transformed Medicine; Oxford University Press: New York, NY, USA, 2007. [Google Scholar]
- Schuman, A.J. A Concise History of Antimicrobial Therapy (Serendipity and All). Contemp. Pediatr. 2003, 20, 66–85. [Google Scholar]
- Jayachandran, S.; Lleras-Muney, A.; Lleras-Muney, A.; Smith, K.V. Modern Medicine and the Twentieth Century Decline in Mortality: Evidence on the Impact of Sulfa Drugs. Am. Econ. J. Appl. Econ. 2010, 2, 118–146. [Google Scholar] [CrossRef]
- Leucht, S.; Tardy, M.; Komossa, K.; Heres, S.; Kissling, W.; Salanti, G.; Davis, J.M. Antipsychotic drugs versus placebo for relapse prevention in schizophrenia: A systematic review and meta-analysis. Lancet 2012, 379, 2063–2071. [Google Scholar] [CrossRef]
- Shen, W.W. A history of antipsychotic drug development. Compr. Psychiatry 1999, 40, 407–414. [Google Scholar] [PubMed]
- Zhang, J.-P. The Benefits of Antipsychotic Drugs: Symptom Control and Improved Quality of Life. In Life-Threatening Effects of Antipsychotic Drugs; Manu, P., Flanagan, R.J., Ronaldson, K.J., Eds.; Academic Press: Cambridge, MA, USA, 2016; pp. 295–309. [Google Scholar]
- D’Arcy, P.F. Iatrogenic disease: A hazard of multiple drug therapy. R. Soc. Health J. 1976, 96, 277–283. [Google Scholar] [PubMed]
- Stolley, J.M.; Buckwalter, K.C.; Fjordbak, B.; Bush, S. Iatrogenesis in the elderly: Drug-related problems. J. Gerontol. Nurs. 1991, 17, 12–17. [Google Scholar] [PubMed]
- Gardner, D.M.; Teehan, M.D. Antipsychotics and Their Side Effects; Cambridge University Press: New York, NY, USA, 2011. [Google Scholar]
- Manu, P.; Flanagan, R.J.; Ronaldson, K.J. (Eds.) Life-Threatening Effects of Antipsychotic Drugs; Academic Press: Cambridge, MA, USA, 2016. [Google Scholar]
- British Broadcasting Corporation (BBC). The New Jerusalem: Safe in Their Hands (Documentary Produced on 50th Anniversary of UK Postwar Welfare State for BBC 2). 1995. Available online: https://www.youtube.com/watch?v=fKzXcWJsesg (accessed on 13 September 2018).
- Szczepura, A.; Clay, D.; Nelson, S.; Wild, D.; Spilsbury, K. Improving Care in Residential Care Homes: A Literature Review; Joseph Rowntree Foundation: York, UK, 2008. [Google Scholar]
- Banerjee, S. The Use of Antipsychotic Medication for People with Dementia: Time for Action. A Report for the Minister of State for Care Services. An Independent Report Commissioned for the Department of Health. 2009. Available online: http://webarchive.nationalarchives.gov.uk/20130104175837/http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/documents/digitalasset/dh_108302.pdf (accessed on 20 August 2017).
- Sherlaw-Johnson, C.; Crump, H.; Curry, N.; Paddison, C.; Meaker, R. Transforming Health Care in Nursing Homes: An Evaluation of a Dedicated Primary Care Service in Outer East London; Nuffield Trust: London, UK, 2018. [Google Scholar]
- Roberts, M.L.A.; Schiavenato, M. Othering in the nursing context: A concept analysis. Nurs. Open 2017, 4, 174–181. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, T.C.; Del Mar, C. Clinicians’ Expectations of the Benefits and Harms of Treatments, Screening, and Tests: A Systematic Review. JAMA Intern. Med. 2017, 177, 407–419. [Google Scholar] [CrossRef] [PubMed]
- Schork, N.J. Personalized medicine: Time for one-person trials. Nature 2015, 520, 609–611. [Google Scholar] [CrossRef] [PubMed]
- Hakkarainen, K.M.; Andersson Sundell, K.; Petzold, M.; Hägg, S. Prevalence and perceived preventability of self-reported adverse drug events—A population-based survey of 7099 adults. PLoS ONE 2013, 8, e73166. [Google Scholar] [CrossRef] [PubMed]
- Kanagaratnam, L.; Dramé, M.; Trenque, T.; Oubaya, N.; Nazeyrollas, P.; Novella, J.L.; Jolly, D.; Mahmoudi, R. Adverse drug reactions in elderly patients with cognitive disorders: A systematic review. Maturitas 2016, 85, 56–63. [Google Scholar] [CrossRef] [PubMed]
- Alhawassi, T.M.; Krass, I.; Bajorek, B.V.; Pont, L.G. A systematic review of the prevalence and risk factors for adverse drug reactions in the elderly in the acute care setting. Clin. Interv. Aging 2014, 9, 2079–2086. [Google Scholar] [CrossRef] [PubMed]
- Bouvy, J.C.; De Bruin, M.L.; Koopmanschap, M.A. Epidemiology of adverse drug reactions in Europe: A review of recent observational studies. Drug Saf. 2015, 38, 437–453. [Google Scholar] [CrossRef] [PubMed]
- Deilkås, E.T.; Risberg, M.B.; Haugen, M.; Lindstrøm, J.C.; Nylén, U.; Rutberg, H.; Michael, S. Exploring similarities and differences in hospital adverse event rates between Norway and Sweden using Global Trigger Tool. BMJ Open 2017, 7, e012492. [Google Scholar] [CrossRef] [PubMed]
- Tangiisuran, B.; Wright, J.; Van der Cammen, T.; Rajkumar, C. Adverse drug reactions in elderly: Challenges in identification and improving preventative strategies. Age Ageing 2009, 38, 358–359. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Gabe-Walters, M.E.; Watkins, A.; Humphreys, I.; Newson, L.; Snelgrove, S.; Dennis, M.S. Nurse-Led Medicines’ Monitoring for Patients with Dementia in Care Homes: A Pragmatic Cohort Stepped Wedge Cluster Randomised Trial. PLoS ONE 2015, 10, e0140203. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Vaismoradi, M.; Griffiths, P. Adverse drug reactions, nursing and policy: A narrative review. Ann. Nurs. Pract. 2016, 3, 1050. Available online: http://www.jscimedcentral.com/Nursing/nursing-3-1050.pdf (accessed on 13 September 2018).
- Motter, F.R.; Fritzen, J.S.; Hilmer, S.N.; Paniz, E.N.; Paniz, V.M. Potentially inappropriate medication in the elderly: A systematic review of validated explicit criteria. Eur. J. Clin. Pharmacol. 2018, 74, 679–700. [Google Scholar] [CrossRef] [PubMed]
- Pirmohamed, M.; James, S.; Meakin, S.; Scott, A.K.; Walley, T.J.; Farrer, K.; Park, B.K.; Breckenridge, A.M. Adverse drug reactions as cause of admission to hospital: Prospective analysis of 18 820 patients. BMJ 2004, 329, 15–19. [Google Scholar] [CrossRef] [PubMed]
- NICE Medicines and Prescribing Centre. Medicines Optimisation: The Safe and Effective Use of Medicines to Enable the Best Possible Outcomes; NICE Guideline 5; NICE: London, UK, 2015; Available online: https://www.nice.org.uk/guidance/ng5/resources/medicines-optimisation-the-safe-and-effective-use-of-medicines-to-enable-the-best-possible-outcomes-pdf-51041805253 (accessed on 20 August 2017).
- Kongkaew, C.; Noyce, P.R.; Ashcroft, D.M. Hospital admissions associated with adverse drug reactions: A systematic review of prospective observational studies. Ann. Pharmacother. 2008, 42, 1017–1025. [Google Scholar] [CrossRef] [PubMed]
- Frontier Economic. Exploring the Costs of Unsafe Care in the NHS: A Report Prepared for the Department of Health. 2014. Available online: http://www.frontier-economics.com/documents/2014/10/exploring-the-costs-of-unsafe-care-in-the-nhs-frontier-report-2-2-2-2.pdf (accessed on 20 August 2017).
- Elliott, R.; Camacho, E.; Campbell, F.; Jankovic, D.; St. James, M.M.; Kaltenthaler, E.; Wong, R.; Sculpher, M.; Faria, R. Prevalence and Economic Burden of Medication Errors in the NHS in England. Rapid Evidence Synthesis and Economic Analysis of the Prevalence and Burden of Medication Error in the UK. Policy Research Unit in Economic Evaluation of Health and Care Interventions. Universities of Sheffield and York. 2018. Available online: http://www.eepru.org.uk/prevalence-and-economic-burden-of-medication-errors-in-the-nhs-in-england-2/ (accessed on 18 September 2018).
- Nair, P.N.; Chalmers, L.; Connolley, M.; Bereznicki, B.J.; Peterson, G.M.; Curtain, C.; Castelino, R.L.; Bereznicki, L.R. Prediction of Hospitalisation due to Adverse Drug Reactions in Elderly Community-Dwelling Patients (The PADR-EC Score). PLoS ONE 2016. [Google Scholar] [CrossRef]
- Walter, S.R.; Day, R.O.; Gallego, B.; Westbrook, J.I. The impact of serious adverse drug reactions: A population based study of a decade of hospital admissions in New South Wales, Australia. Br. J. Pharmacol. 2017, 83, 416–426. [Google Scholar] [CrossRef] [PubMed]
- WHO. Patient Safety Research: WHO. 2009. Available online: http://apps.who.int/iris/bitstream/10665/70145/1/WHO_IER_PSP_2009.10_eng.pdf (accessed on 20 August 2017).
- Roulet, L.; Ballereau, F.; Hardouin, J.B.; Chiffoleau, A.; Potel, G.; Asseray, N. Adverse drug event nonrecognition in emergency departments: An exploratory study on factors related to patients and drugs. J. Emerg. Med. 2014, 46, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Lesser, G.T.; Boockvar, K.; Polsky, I. Underestimation of adverse drug events in nursing home residents. Arch. Intern. Med. 2002, 162, 609–610. [Google Scholar] [CrossRef] [PubMed]
- Kongkaew, C.; Hann, M.; Mandal, J.; Williams, S.D.; Metcalfe, D.; Noyce, P.R.; Ashcroft, D.M. Risk factors for hospital admissions associated with adverse drug events. Pharmacotherapy 2013, 33, 827–837. [Google Scholar] [CrossRef] [PubMed]
- Rydberg, D.M.; Holm, L.; Engqvist, I.; Fryckstedt, J.; Lindh, J.D.; Stiller, C.O.; Asker-Hagelberg, C. Adverse Drug Reactions in a Tertiary Care Emergency Medicine Ward—Prevalence, Preventability and Reporting. PLoS ONE 2016, 11, e0162948. [Google Scholar] [CrossRef] [PubMed]
- Beijer, H.J.; de Blaey, C.J. Hospitalisations caused by adverse drug reactions (ADR): A meta-analysis of observational studies. Pharm. World Sci. 2002, 14, 46–54. [Google Scholar] [CrossRef]
- Gabe, M.E.; Davies, G.A.; Murphy, F.; Davies, M.; Johnstone, L.; Jordan, S. Adverse drug reactions: Treatment burdens and nurse-led medication monitoring. J. Nurs. Manag. 2011, 19, 377–392. [Google Scholar] [CrossRef] [PubMed]
- Brenner, S.; Detz, A.; Lopez, A.; Horton, C.; Sarkar, U. Signal and noise: Applying a laboratory trigger tool to identify adverse drug events among primary care patients. BMJ Qual. Saf. 2012, 21, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Forster, A.J.; Murff, H.J.; Peterson, J.F.; Gandhi, T.K.; Bates, D.W. Adverse drug events occurring following hospital discharge. J. Gen. Intern. Med. 2005, 20, 317–323. [Google Scholar] [CrossRef] [PubMed]
- Gurwitz, J.H.; Field, T.S.; Judge, J.; Rochon, P.; Harrold, L.R.; Cadoret, C.; Lee, M.; White, K.; LaPrino, J.; Erramuspe-Mainard, J.; et al. The incidence of adverse drug events in two large academic long-term care facilities. Am. J. Med. 2005, 118, 251–258. [Google Scholar] [CrossRef] [PubMed]
- Steinman, M.A.; Handler, S.M.; Gurwitz, J.H.; Schiff, G.D.; Covinsky, K.E. Beyond the prescription: Medication monitoring and adverse drug events in older adults. J. Am. Geriatr. Soc. 2011, 59, 1513–1520. [Google Scholar] [CrossRef] [PubMed]
- Aronson, J.K.; Ferner, R.E. The law of mass action and the pharmacological concentration–effect curve: Resolving the paradox of apparently non-dose-related adverse drug reactions. Br. J. Clin. Pharmacol. 2016, 81, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Stewart, R.; Hotopf, M.; Dewey, M.; Ballard, C.; Bisla, J.; Calem, M.; Fahmy, V.; Hockley, J.; Kinley, J.; Pearce, H.; et al. Current prevalence of dementia, depression and behavioural problems in the older adult care home sector: The South East London Care Home Survey. Age Ageing 2014, 43, 562–567. [Google Scholar] [CrossRef] [PubMed]
- Bradley, M.C.; Motterlini, N.; Padmanabhan, S.; Cahir, C.; Williams, T.; Fahey, T.; Hughes, C.M. Potentially inappropriate prescribing among older people in the United Kingdom. BMC Geriatr. 2014, 12, 72. [Google Scholar] [CrossRef] [PubMed]
- Sköldunger, A.; Fastbom, J.; Wimo, A.; Fratiglioni, L.; Johnell, K. Impact of Inappropriate Drug Use on Hospitalizations, Mortality, and Costs in Older Persons and Persons with Dementia: Findings from the SNAC Study. Drugs Aging 2015, 32, 671–678. [Google Scholar] [CrossRef] [PubMed]
- Storms, H.; Marquet, K.; Aertgeerts, B.; Claes, N. Prevalence of inappropriate medication use in residential long-term care facilities for the elderly: A systematic review. Eur. J. Gen. Pract. 2017, 23, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S. The Prescription Drug Guide for Nurses; Open University Press, McGraw-Hill: Maidenhead, UK, 2008. [Google Scholar]
- Masopust, J.; Protopopová, D.; Vališ, M.; Pavelek, Z.; Klímová, B. Treatment of behavioral and psychological symptoms of dementias with psychopharmaceuticals: A review. Neuropsychiatr. Dis. Treat. 2018, 14, 1211–1220. [Google Scholar] [CrossRef] [PubMed]
- Ballard, C.; Hanney, M.L.; Theodoulou, M.; Douglas, S.; McShane, R.; Kossakowski, K.; Gill, R.; Juszczak, E.; Yu, L.M.; Jacoby, R. DART-AD investigators. The dementia antipsychotic withdrawal trial (DART-AD): Long-term follow-up of a randomisedplacebo-controlled trial. Lancet Neurol. 2009, 8, 151–157. [Google Scholar] [CrossRef]
- Sacchetti, E.; Turrina, C.; Valsecchi, P. Cerebrovascular accidents in elderly people treated with antipsychotic drugs: A systematic review. Drug Saf. 2013, 33, 273–288. [Google Scholar] [CrossRef] [PubMed]
- Schneider, L.S.; Tariot, P.N.; Dagerman, K.S.; Davis, S.M.; Hsiao, J.K.; Ismail, M.S.; Lebowitz, B.D.; Lyketsos, C.G.; Ryan, J.M.; Stroup, T.S.; et al. CATIE-AD Study Group. Effectiveness of atypical antipsychotic drugs in patients with Alzheimer’s disease. N. Engl. J. Med. 2006, 355, 1525–1538. [Google Scholar] [CrossRef] [PubMed]
- Bradley, P.; Willson, A. Achieving prudent healthcare in NHS Wales Wales: Public Health Wales. 2014. Available online: http://www.1000livesplus.wales.nhs.uk/sitesplus/documents/1011/Achieving%20prudent%20healthcare%20in%20NHS%20Wales%20paper%20Revised%20version%20%28FINAL%29.pdf (accessed on 20 August 2017).
- Older People’s Commissioner for Wales. A Place to Call Home. Older People’s Commissioner for Wales. 2014. Available online: http://www.olderpeoplewales.com/Libraries/Uploads/A_Place_to_Call_Home_-_A_Review_into_the_Quality_of_Life_and_Care_of_Older_People_living_in_Care_Homes_in_Wales.sflb.ashx (accessed on 20 August 2017).
- Older People’s Commissioner for Wales. 2018. A Place to Call Home: Impact and Analysis. Older people’s Commissioner for Wales. Available online: http://www.olderpeoplewales.com/Libraries/Uploads/A_Place_to_Call_Home_-_Impact_Analysis_--_Final.sflb.ashx (accessed on 13 September 2018).
- Thomas, S.; Banner, T. Improving Medicines Use for Care Home Residents; Royal Pharmaceutical Society: Cardiff, UK, 2016; Available online: https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Policy%20statements/improving-medicines-use-for-care-home-residents-(wales).pdf?ver=2016-10-13-162139-760 (accessed on 3 April 2018).
- National Assembly for Wales (NAfW). Health, Social Care and Sport Committee 2018 Use of Antipsychotic Medication in Care Homes; National Assembly: Cardiff, UK, 2018; Available online: http://senedd.assembly.wales/documents/s75570/Report%20-%20Use%20of%20antipsychotic%20medication%20in%20care%20homes.pdf (accessed on 21 July 2018).
- Francis, R. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry; The Stationery Office: London, UK, 2013. Available online: http://webarchive.nationalarchives.gov.uk/20150407084231/http://www.midstaffspublicinquiry.com/report (accessed on 20 August 2017).
- NICE. 2014 Updated 2017 Managing Medicines in Care Homes. NICE GUIDANCE SC1. Available online: https://www.nice.org.uk/guidance/sc1# (accessed on 13 September 2018).
- Andrews, J.; Butler, M. Trusted to Care. An Independent Review of the Princess of Wales Hospital and Neath Port Talbot Hospital at Abertawe Bro Morgannwg University Health Board. Dementia Services Development Centre, The People Organisation. 2014. Available online: http://www.ambulance.wales.nhs.uk/assets/documents/2e459532-3f27-4fc6-8091-6445fb417a63635387689176252637.pdf (accessed on 20 August 2017).
- Page, A.T.; Clifford, R.M.; Potter, K.; Schwartz, D.; Etherton-Beer, C.D. The feasibility and effect of deprescribing in older adults on mortality and health: A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2016, 82, 583–623. [Google Scholar] [CrossRef] [PubMed]
- Respect Trial Team. Effectiveness of shared pharmaceutical care for older patients: RESPECT trial findings. Br. J. Gen. Pract. 2010, 60, e10–e19. [Google Scholar] [CrossRef] [PubMed]
- Forsetlund, L.; Eike, M.C.; Gjerberg, E.; Vist, G.E. Effect of interventions to reduce potentially inappropriate use of drugs in nursing homes: A systematic review of randomised controlled trials. BMC Geriatr. 2011, 11, 16. [Google Scholar] [CrossRef] [PubMed]
- Holland, R.; Desborough, J.; Goodyer, L.; Hall, S.; Wright, D.; Loke, Y.K. Does pharmacist-led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta-analysis. Br. J. Clin. Pharmacol. 2008, 65, 303–316. [Google Scholar] [CrossRef] [PubMed]
- Alldred, D.P.; Kennedy, M.C.; Hughes, C.; Chen, T.F.; Miller, P. Interventions to optimise prescribing for older people in care homes. Cochrane Database Syst. Rev. 2016, CD009095. [Google Scholar] [CrossRef]
- Viswanathan, M.; Kahwati, L.C.; Golin, C.E.; Blalock, S.J.; Coker-Schwimmer, E.; Posey, R.; Lohr, K.N. Medication therapy management interventions in outpatient settings: A systematic review and meta-analysis. JAMA Intern. Med. 2015, 175, 76–87. [Google Scholar] [CrossRef] [PubMed]
- Medicines and Healthcare products Regulatory Agency (MHRA). Antipsychotics: Initiative to Reduce Prescribing to Older People with Dementia. 2012. Available online: https://www.gov.uk/drug-safety-update/antipsychotics-initiative-to-reduce-prescribing-to-older-people-with-dementia (accessed on 13 September 2018).
- Szczepura, A.; Wild, D.; Khan, A.J.; Owen, D.W.; Palmer, T.; Muhammad, T.; Clark, M.D.; Bowman, C. Antipsychotic prescribing in care homes before and after launch of a national dementia strategy: An observational study in English institutions over a 4-year period. BMJ Open 2016, 6, e009882. [Google Scholar] [CrossRef] [PubMed]
- Marston, L.; Nazareth, I.; Petersen, I.; Walters, K.; Osborn, D.P. Prescribing of antipsychotics in UK primary care: A cohort study. BMJ Open 2014, 4, e006135. [Google Scholar] [CrossRef] [PubMed]
- Cooper, A.; Edwards, A.; Williams, H.; Evans, H.P.; Avery, A.; Hibbert, P.; Makeham, M.; Sheikh, A.; JDonaldson, L.; Carson-Stevens, A. Sources of unsafe primary care for older adults: A mixed-methods analysis of patient safety incident reports. Age Ageing 2017, 46, 833–839. [Google Scholar] [CrossRef] [PubMed]
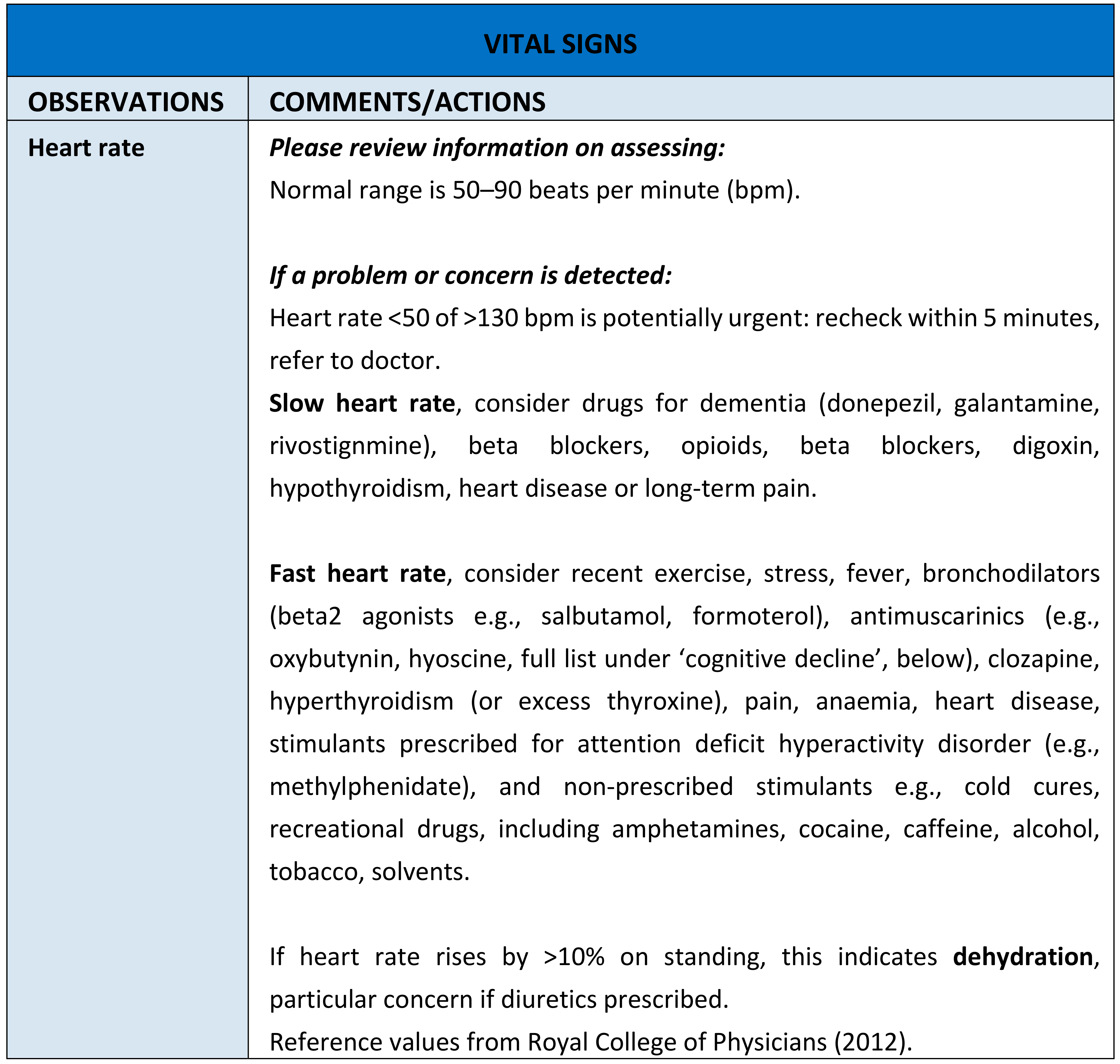
- Jordan, S.; Knight, J.; Pointon, D. Monitoring adverse drug reactions: Scales, profiles, and checklists. Int. Nurs. Rev. 2004, 51, 208–221. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Banner TGabe-Walters, M.; Mikhail, J.; Round, J.; Snelgrove, S.; Storey, M.; Wilson, D.W.; Hughes, D. Nurse-led medicines’ monitoring in care homes study protocol: A process evaluation of the impact and sustainability of the Adverse Drug Reaction (ADRe) Profile for Mental Health Medicines. BMJ 2018. [Google Scholar] [CrossRef]
- Australian Pharmaceutical Advisory Council. Guidelines for Medication Management in Residential Aged Care Facilities; Commonwealth of Australia: Canberra, Australia, 2002. Available online: http://www.health.gov.au/internet/main/publishing.nsf/Content/nmp-pdf-resguide-cnt.htm/$FILE/resguide.pdf (accessed on 13 September 2018).
- Brodaty, H.; Aerts, L.; Harrison, F.; Jessop, T.; Cations, M.; Chenoweth, L.; Shell, A.; Popovic, G.C.; Heffernan, M.; Hilmer, S.; et al. Antipsychoticm Deprescription for Older Adults in Long-term Care: The HALT Study. J. Am. Med. Dir. Assoc. 2018, 19, 592.e7–600.e7. [Google Scholar] [CrossRef] [PubMed]
- Gabe, M.; Murphy, F.; Davies, G.; Russell, I.; Jordan, S. Medication Monitoring in a Nurse-Led Respiratory Outpatient Clinic: Pragmatic Randomised Trial of the West Wales Adverse Drug Reaction Profile. PLoS ONE 2014, 9, e96682. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.; Moyle, C.; Jordan, S. Nurse-led medicines monitoring: A study examining the effects of the West Wales Adverse Drug Reaction Profile. Nurs. Stand. 2016, 31, 42–53. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Gabe, M.; Newson, L.; Snelgrove, S.; Panes, G.; Picek, A.; Russell, I.T.; Dennis, M. Medication monitoring for people with dementia in care homes: The feasibility and clinical impact of nurse-led monitoring. Sci. World J. 2014, 2014, 843621. [Google Scholar] [CrossRef] [PubMed]
- Gabe, M.E.; Jordan, S.E. Development and clinical gains of nurse-led medication monitoring profiles. J. Nurs. Manag. 2014, 22, 331–349. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Tunnicliffe, C.; Sykes, A. Minimising Side Effects: The clinical impact of nurse-administered ‘side effect’ checklists. J. Adv. Nurs. 2002, 37, 155–165. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S. Managing Adverse Drug Reactions: An Orphan Task. Developing Nurse-Administered Evaluation Checklists. J. Adv. Nurs. 2002, 38, 437–448. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Philpin, S.; Davies, S.; Andrade, M. The biological sciences in mental health nursing: stakeholders’ perspectives. J. Adv. Nurs. 2000, 32, 881–891. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Hardy, B.; Coleman, M. Medication management: An exploratory study into the role of Community Mental Health Nurses. J. Adv. Nurs. 1999, 29, 1068–1081. [Google Scholar] [CrossRef] [PubMed]
- Day, G. Divided and Dividing Wales? Explorations in Geography and Class. In Making Sense of Wales: A Sociological Perspective; Day, G., Ed.; University of Wales Press: Cardiff, UK, 2002; pp. 94–115. [Google Scholar]
- World Health Organization (WHO). 2017 WHO Launches Global Effort to Halve Medication-Related Errors in 5 Years. Geneva/Bonn. Available online: http://www.who.int/mediacentre/news/releases/2017/medication-related-errors/en/ (accessed on 20 August 2017).
- Drug and Therapeutics Bulletin 2018 What Dose of Paracetamol for Older People? Drug and Therapeutics Bulletin Vol. 56|No. 6|June 2018. pp. 68–72. Available online: https://dtb.bmj.com/content/dtb/56/6/69.full.pdf (accessed on 13 September 2018).
- Jordan, S.; Morris, J.K.; Davies, G.I.; Tucker, D.; Thayer, D.S.; Luteijn, J.M.; Morgan, M.; Garne, E.; Hansen, A.V.; Klungsøyr, K.; et al. Selective Serotonin Reuptake Inhibitor (SSRI) antidepressants in Pregnancy and Congenital Anomalies: Analysis of linked databases in Wales, Norway and Funen, Denmark. PLoS ONE 2016, 11, e0165122. [Google Scholar] [CrossRef] [PubMed]
- Willson, A. The problem with eliminating ‘low-value care’. BMJ Qual. Saf. 2015, 24, 611–614. [Google Scholar] [CrossRef] [PubMed]
- Barber, C.; Gagnon, D.; Fonda, J.; Cho, K.; Hermos, J.; Miller, M. Assessing the impact of prescribing directives on opioid prescribing practices among Veterans Health Administration providers. Pharmacoepidemiol. Drug Saf. 2017, 26, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Sackett, D.L.; Rosenberg, W.M.; Gray, J.A.; Haynes, R.B.; Richardson, W.S. Evidence based medicine: What it is and what it isn’t. BMJ 1996, 13, 71–72. [Google Scholar] [CrossRef]
- Mittal, M.; Harrison, D.L.; Miller, M.J.; Farmer, K.C.; Thompson, D.M.; Ng, Y.T. Have antiepileptic drug prescription claims changed following the FDA suicidality warning? An evaluation in a state Medicaid program. Epilepsy Behav. 2014, 34, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.Y.; Zhang, F.; Lakoma, M.D.; Butler, M.G.; Fung, V.; Larkin, E.K.; Kharbanda, E.O.; Vollmer, W.M.; Lieu, T.; Soumerai, S.B.; et al. Asthma Treatments and Mental Health Visits After a Food and Drug Administration Label Change for Leukotriene Inhibitors. Clin. Ther. 2015, 37, 1280–1291. [Google Scholar] [CrossRef] [PubMed]
- Hazell, L.; Shakir, S.A. Under-reporting of adverse drug reactions: A systematic review. Drug Saf. 2006, 29, 385–396. [Google Scholar] [CrossRef] [PubMed]
- De Boissieu, P.; Kanagaratnam, L.; Abou Taam, M.; Roux, M.P.; Dramé, M.; Trenque, T. Notoriety bias in a database of spontaneous reports: The example of osteonecrosis of the jaw under bisphosphonate therapy in the French national pharmacovigilance database. Pharmacoepidemiol. Drug Saf. 2014, 23, 989–992. [Google Scholar] [CrossRef] [PubMed]
- Pariente, A.; Gregoire, F.; Fourrier-Reglat, A.; Haramburu, F.; Moore, N. Impact of safety alerts on measures of disproportionality in spontaneous reporting databases: The notoriety bias. Drug Saf. 2007, 30, 891–898. [Google Scholar] [CrossRef] [PubMed]
- Parker, D.; Lawton, R. Judging the use of clinical protocols by fellow professionals. Soc. Sci. Med. 2000, 51, 669–677. [Google Scholar] [CrossRef]
- Roland, M. Linking physicians’ pay to the quality of care—A major experiment in the United kingdom. N. Engl. J. Med. 2004, 351, 1448–1454. [Google Scholar] [CrossRef] [PubMed]
- BMA and NHS Employers. Revisions to the GMS Contract 2006/07 Delivering Investment in General Practice; BMA: London, UK, 2009; Available online: http://www.nhsemployers.org/~/media/Employers/Documents/Primary%20care%20contracts/QOF/2006-07/Revisions%20to%20the%20GMS%20contract%20200607%20-%20Delivering%20investments%20in%20general%20practice.pdf (accessed on 13 September 2018).
- Kendrick, T.; Stuart, B.; Newell, C.; Geraghty, A.W.; Moore, M. Changes in rates of recorded depression in English primary care 2003–2013: Time trend analyses of effects of the economic recession, and the GP contract quality outcomes framework (QOF). J. Affect. Disord. 2015, 180, 68–78. [Google Scholar] [CrossRef] [PubMed]
- Barnes, G.D.; Lucas, E.; Alexander, G.C.; Goldberger, Z.D. National Trends in Ambulatory Oral Anticoagulant Use. Am. J. Med. 2015, 128, 1300.e2–1305.e2. [Google Scholar] [CrossRef] [PubMed]
- Mohammad, I.; Korkis, B.; Garwood, C.L. Incorporating Comprehensive Management of Direct Oral Anticoagulants into Anticoagulation Clinics. Pharmacotherapy 2017, 37, 1284–1297. [Google Scholar] [CrossRef] [PubMed]
- Odom, D.M.; Mladsi, D.M.; Saag, K.G.; Sherif, B.N.; Miles, L.; Ronquest, N.; Wang, J. Relationship between diclofenac dose and risk of gastrointestinal and cardiovascular events: Meta-regression based on two systematic literature reviews. Clin. Ther. 2014, 36, 906–917. [Google Scholar] [CrossRef] [PubMed]
- Sukkar, E. Risk of heart problems prompts removal of OTC diclofenac from UK pharmacy shelves. Pharm. J. 2015, 294, 7846. [Google Scholar] [CrossRef]
- Singh, R.R.; Nayak, R. Impact of FDA Black Box Warning on Psychotropic Drug Use in Noninstitutionalized Elderly Patients Diagnosed with Dementia: A Retrospective Study. J. Pharm. Pract. 2015, 29, 495–502. [Google Scholar] [CrossRef] [PubMed]
- Ryan, A.M.; Krinsky, S.; Kontopantelis, E.; Doran, T. Long-term evidence for the effect of pay-for-performance in primary care on mortality in the UK: A population study. Lancet 2016, 388, 268–274. [Google Scholar] [CrossRef]
- European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCePP). Annex 2 to the Guide on Methodological Standards in Pharmacoepidemiology. 2018. Available online: http://www.encepp.eu/standards_and_guidances (accessed on 13 September 2018).
- Hakobyan, L.; Haaijer-Ruskamp, F.M.; de Zeeuw, D.; Dobre, D.; Denig, P. A review of methods used in assessing non-serious adverse drug events in observational studies among type 2 diabetes mellitus patients. Health Qual. Life Outcomes 2011, 9, 83. [Google Scholar] [CrossRef] [PubMed]
- Schoenmakers, T.W.A.; Teichert, M.; Wensing, M.; de Smet, P.A.G.M. Evaluation of Potentially Drug-Related Patient-Reported Common Symptoms Assessed during Clinical Medication Reviews: A Cross-Sectional Observational Study. Drug Saf. 2017, 40, 419–430. [Google Scholar] [CrossRef] [PubMed]
- Talbot, J.; Keisu, M.; Stahle, L. Clinical trials—Collecting safety data and establishing the ADR Profile. In Stephens’ Detection and Evaluation of Adverse Drug Reactions, 6th ed.; Talbot, J., Aronson, J.K., Eds.; Wiley-Blackwell: Chichester, UK, 2012; pp. 215–290. [Google Scholar]
- Gandhi, T.; Burstin, H.; Cook, F.; Puopolo, A.; Haas, J.; Brennan, T.; Bates, D. Drug Complications in Outpatients. J. Gen. Intern. Med. 2000, 15, 149–154. [Google Scholar] [CrossRef]
- Weingart, S.; Gandhi, T.; Seger, A.; Seger, D.L.; Borus, J.; Burdick, E.; Leape, L.L.; Bates, D.W. Patient reported medication symptoms in primary care. Arch. Intern. Med. 2005, 165, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Lewis, G.; Cantwell, R.; Clutton-Brock, T.; Cooper, G.; Dawson, A.; Drife, J.; Garrod, D.; Harper, A.; Hulbert, D.; Lucas, S.; et al. Saving Mothers’ Lives: Reviewing maternal deaths to make motherhood safer: 2006–2008. The Eighth Report of the Confidential Enquiries into Maternal Deaths in the United Kingdom. BJOG 2011, 118 (Suppl. 1), 1–203. [Google Scholar]
- Ballard, C.; Orrell, M.; Sun, Y.; Moniz-Cook, E.; Stafford, J.; Whitaker, R.; Woods, B.; Corbett, A.; Garrod, L.; Khan, Z.; et al. Impact of antipsychotic review and nonpharmacological intervention on antipsychotic use, neuropsychiatric symptoms, and mortality in people with dementia living in nursing homes: A factorial cluster-randomized controlled trial by the well-being and health for people with dementia (WHELD) Program. Int. J. Geriatr. Psychiatry 2015, 173, 252–262. [Google Scholar] [CrossRef]
- Ballard, C.; Orrell, M.; Sun, Y.; Moniz-Cook, E.; Stafford, J.; Whitaker, R.; Woods, B.; Corbett, A.; Banerjee, S.; Testad, I.; et al. Impact of antipsychotic review and non-pharmacological intervention on health-related quality of life in people with dementia living in care homes: WHELD-a factorial cluster randomised controlled trial. Int. J. Geriatr. Psychiatry 2017, 32, 1094–1103. [Google Scholar] [CrossRef] [PubMed]
- Iyer, S.; Naganathan, V.; McLachlan, A.J.; Le Couteur, D.G. Medication withdrawal trials in people aged 64 years and older: A systematic review. Drugs Aging 2008, 25, 1021–1031. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Charlton, R.A.; Tingay, K.; Thayer, D.S.; Davies, G.I.; Morgan, M.; Tucker, D.; Watkins, A.; Gini, R.; Pierini, A.; et al. SSRI use in pregnancy: A study in 6 European databases. The International Marcé Society for Perinatal Mental Health Biennial Scientific Conference, Swansea University, Swansea, Wales, UK. Abstracts from the Marce Society Conference. Arch. Womens Ment. Health 2015, 18, 269–408. [Google Scholar] [CrossRef]
- Guthrie, B.; Makubate, B.; Hernandez-Santiago, V.; Dreischulte, T. The rising tide of polypharmacy and drug-drug interactions: Population database analysis 1995–2010. BMC Med. 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Welsh Government. Chief Medical Officer for Wales Annual Report 2015–2016. 2016. Available online: http://gov.wales/docs/dhss/publications/161110cmoreport16en.pdf (accessed on 13 September 2018).
- Hart, J.T. The inverse care law. Lancet 1971, 1, 405–412. [Google Scholar] [CrossRef]
- Pedersen, A.F.; Vedsted, P. Understanding the inverse care law: A register and survey-based study of patient deprivation and burnout in general practice. Int. J. Equity Health 2014, 13, 121. [Google Scholar] [CrossRef] [PubMed]

| Design | Clinical Area | Findings | Case Reports, Examples of ADRs Addressed without Hospitalisation | |
|---|---|---|---|---|
| Studies Using the ADRe Profiles | ||||
| Jones et al. 2016 [81] | ‘Before-and-after’ study of 20 patients | Community mental health, crisis resolution home treatment | The Profile identified previously unreported physical health problems for all participants, including two previously unreported potentially life-threatening problems (cardiac arrhythmia, and valproate-induced pancreatitis). In all, 4 participants had medicines discontinued, 3 were referred to consultant psychiatrists, 3 to general practitioners, 1 to ECG technicians, and 1 to dentists. Previously neglected health promotion issues were also recognised. | A middle-aged man, diagnosed with schizophrenia, had previously unrecorded but potentially serious cardiovascular problems (cardiac arrhythmia, intermittent acute chest pain) that worsened with exertion and radiated. He was referred immediately to his GP. The consultant determined that this case, and one other, fulfilled the criteria for a serious ADR, as it would have resulted in hospitalisation if unattended. |
| Jordan et al. 2015 [27] | Stepped wedge randomised controlled trial (RCT) over 7 months, 5 homes, 41 participants, 125 record reviews before Profile implementation and 124 after | Care home residents with permanent cognitive impairment | Profile administration increased the number of problems addressed from a mean of 6.02 [SD 2.92] to 9.86 [4.48], effect size 3.84, 95% CI 2.57–4.11, p < 0.001. For example, pain was more likely to be treated (adjusted Odds Ratio (aOR) 3.84, 1.78–8.30), and more patients attended dentists and opticians (aOR 52.76 (11.80–235.90) and 5.12 (1.45–18.03), respectively). Profile use was associated with reduction in mental health medicines (aOR 4.45, 1.15–17.22). | A lady in her late 80s, diagnosed with dementia at first administration of the Profile, was noted to be aggressive, restless, confused, sedated, and agitated. The ADRe Profile helped staff identify that hyoscine might be the cause. Hyoscine was discontinued. By the end of the study, 5 months later, aggression, restlessness, and sedation were no longer problems. |
| Jordan et al. 2014 [82] | Feasibility study, 11 patients’ records reviewed 3 times (before Profile implementation, after, and 3 months later), 3 homes. Feedback from clinicians | Care home residents with permanent cognitive impairment | The Profile took 20–25 min to implement, caused no harm, and supplemented usual care. On first use, the Profile identified previously undocumented problems for all service users: mean 12.7 [SD 4.7]. One month later, a mean of 4.9 [3.6] problems had been ameliorated. Clinical gains documented included: new prescriptions to manage pain (2 participants), psoriasis (1), Parkinsonian symptoms (1), rash (1); dose reduction of benzodiazepines for one service user; new care plans for oral hygiene, skin problems, and constipation. | A lady in her mid-60s, diagnosed with ‘Korsakoff’s syndrome’ and psoriasis, was noted to be oversedated. Benzodiazepine and antipsychotic prescribing were reduced, and sedation was no longer a problem at follow up. Itching rashes were also identified, more creams were administered, including an ‘as needed’ prescription for hydrocortisone, and symptoms were ameliorated. |
| Gabe et al. 2014 [80] | Parallel group RCT Researcher observed clinical visits before and after implementation of the Profile in the intervention arm. Feedback from patients and clinicians | Respiratory medicine, outpatient department, 54 patients recruited and followed up | The increase in numbers of problems per participant identified at follow up was significantly higher in the intervention arm where the median change was +20.5 (inter-quartile range (IQR) 13–26) while that in the control arm was −1 (−3 to +2) (Mann–Whitney U test: z = 6.28, p < 0.001). The increase in numbers of actions per participant taken at follow up was significantly higher in the intervention arm, where the median increase was +2.5 (1–4), while that in the control arm was 0 (−1.75 to +1) (Mann–Whitney U test: z = 4.40, p < 0.001). | Without the Profile, no actions were taken by nurses for a lady in her 50s, with respiratory problems sufficiently severe as to warrant oral prednisolone. Using the Profile, nurses advised her to contact her GP to seek advice regarding mood swings, depression, headaches, and immunisations. The nurse commented: “I would not have picked up on x’s depression without the Profile”. |
| Gabe & Jordan 2014 [83] | Inter-rater reliability Profiles completed in the presence of an observer | Respiratory medicine, outpatient department, 48 patients prescribed respiratory medicines | Cohen’s κ for inter-rater reliability for each item ranged 0.73–1 (good to complete agreement). The Profile identified previously unsuspected problems in all participants, including muscular weakness, skin, and mouth problems. | A lady in her 70s prescribed corticosteroids, bronchodilators, and other respiratory medicines, reported multiple oral problems, plus losing two stone in weight over the last six months, because her mouth was too sore to eat comfortably. She was advised to rinse her mouth shortly after each inhaler use, seek advice from the nurse for information on inhaler technique, and maintain routine dental check-ups. |
| Jordan et al. 2004 [76] | Comparison of instruments available to monitor antipsychotic medicines. Inter-rater reliability, 20 Profiles completed in the presence of an observer | Community mental health teams, 20 service users prescribed long-term medicines | The ADRe Profile assessed a broader range of physiological parameters and potential problems than other instruments. It is the only instrument with supporting information to prompt action in routine care. Items on the Profile had moderate-to-complete inter-rater reliability (ranging 0.44–1.00) | NA |
| Jordan et al. 2002 [84] | ‘Before-and-after’ study with 1 intervention and 1 comparator group | 3 community mental health teams in post-industrial South Wales, 40 service users prescribed long-term mental health medicines | Amongst the 20 clients in the intervention group, the Profile highlighted several problems, two of which were urgent. In the intervention group, the mean number of problems actioned per client increased from 0.35 (range = 0–4) without the Profile to 3 (range = 0–6) with (z = −3.747, 2 tailed p < 0.001). Nurses offered appropriate advice or encouraged clients to contact the relevant agencies to resolve the physical health problems identified. In the comparator group, the number of problems actioned declined from 0.85 (0–3) to 0.5 (0–2), a statistically insignificant difference (z = –1.47, p = 0.14). | Of 20 clients in the intervention group:
|
| Jordan 2002 [85] | ‘Before-and-after’ study with intervention and comparator groups, 40 patients. Interviews with professionals and service users | Community mental health teams in post-industrial South Wales | Profiles apportioned aspects of medication management between nurses and medical prescribers. Most actions taken by nurses to alleviate adverse effects concerned clients’ physical health and advice on health-promotion. Nurses’ interventions would have been more effective had they been able to supply clients with certain medicines, for example for sunblock or oral care. For some clients, ameliorating the adverse effects of medication would have involved changes to prescribed antipsychotic medication; here, decisions were more equivocal. | One client was referred to his GP with chest pain; since he was receiving 100mg fluphenazine decanoate per week, the absence of an ECG recording contravened current guidelines. Nurse: You can attach this to the notes. Show the psychiatrist a copy. If you took the time to take it to the psychiatrist—it could work. (...) By using this we’ll have more evidence to show that there are side effects and we’re concerned, to get medication reviewed. Outpatient appointments are very ‘in and out’ and things get missed. |
| Studies undertaken before the Profile was introduced | ||||
| Jordan et al. 2000 [86] | Stakeholder interviews and 3 service user focus groups | Mental health nursing: 7 service user representatives, 3 service user focus groups | Service users described serious shortfalls in professionals’ abilities to inform them of common adverse effects of medication; these problems were attributable to inadequate educational preparation. | User group representative: CPNs (Community Psychiatric Nurses) focus on the psychiatric illness, they don’t see the medical side, or want to become involved. It’s to do with their training. They wouldn’t help with the constipation or the sunburn for my daughter. This should be in their training. |
| Jordan et al. 1999 [87] | Interviews, observations, and questionnaires with 14 community mental health nurses. | Community mental health teams | Service users were experiencing ADRs, but nurses did not have a structure to record and report problems. Doctors were seeking information from nurses, rather than directly from service users. | Nurse: There should be a form of structure for it (client education). It’s down to individuals whether or not they see the importance of educating people regarding their medication, and I think that should be part and parcel of the assessment. I think it should be there, and I know that it’s not, from my own experience. To me, whoever is on medication, I will ask them if they understand their medication. People say “Oh well, that’s the GP’s role, that’s the doctor’s role”, but it isn’t. It isn’t done and I always ask them that question, “Do you understand what your medication’s doing?”, and I suppose my knowledge maybe isn’t enough either, and I think that maybe I need more training to carry that further. (...) We’ve got to be prepared to answer questions—informed answers have got to be given, then people will ask, ‘What’s this for, what’s this supposed to do to me?’ (...) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jordan, S.; Logan, P.A.; Panes, G.; Vaismoradi, M.; Hughes, D. Adverse Drug Reactions, Power, Harm Reduction, Regulation and the ADRe Profiles. Pharmacy 2018, 6, 102. https://doi.org/10.3390/pharmacy6030102
Jordan S, Logan PA, Panes G, Vaismoradi M, Hughes D. Adverse Drug Reactions, Power, Harm Reduction, Regulation and the ADRe Profiles. Pharmacy. 2018; 6(3):102. https://doi.org/10.3390/pharmacy6030102
Chicago/Turabian StyleJordan, Sue, Patricia A. Logan, Gerwyn Panes, Mojtaba Vaismoradi, and David Hughes. 2018. "Adverse Drug Reactions, Power, Harm Reduction, Regulation and the ADRe Profiles" Pharmacy 6, no. 3: 102. https://doi.org/10.3390/pharmacy6030102
APA StyleJordan, S., Logan, P. A., Panes, G., Vaismoradi, M., & Hughes, D. (2018). Adverse Drug Reactions, Power, Harm Reduction, Regulation and the ADRe Profiles. Pharmacy, 6(3), 102. https://doi.org/10.3390/pharmacy6030102








