Using Numbers Creates Value for Health Professionals: A Quantitative Study of Pain Management in Palliative Care
Abstract
:1. Introduction
2. Experimental Section
2.1. Design
2.2. Setting
| Profession | Numbers (Team South) | Numbers (team North) |
|---|---|---|
| Physician | 2 | 2 |
| Physiotherapist | 1 | 1 |
| Occupational therapist | 0.5 (shared between the two teams) | 0.5 (shared between the two teams) |
| Social worker | 0.5 (shared between the two teams) | 0.5 (shared between the two teams) |
| Nurse | 6 | 8 |
| Total | 10 | 12 |
|
2.3. Data Collection
- What do we want toaccomplish? Goals?
- How will we knowthat achange isanimprovement? Measurements?
- What changes can lead toimprovements in accordance with the ideas?
2.4. Data Analysis
2.5. Ethical Considerations
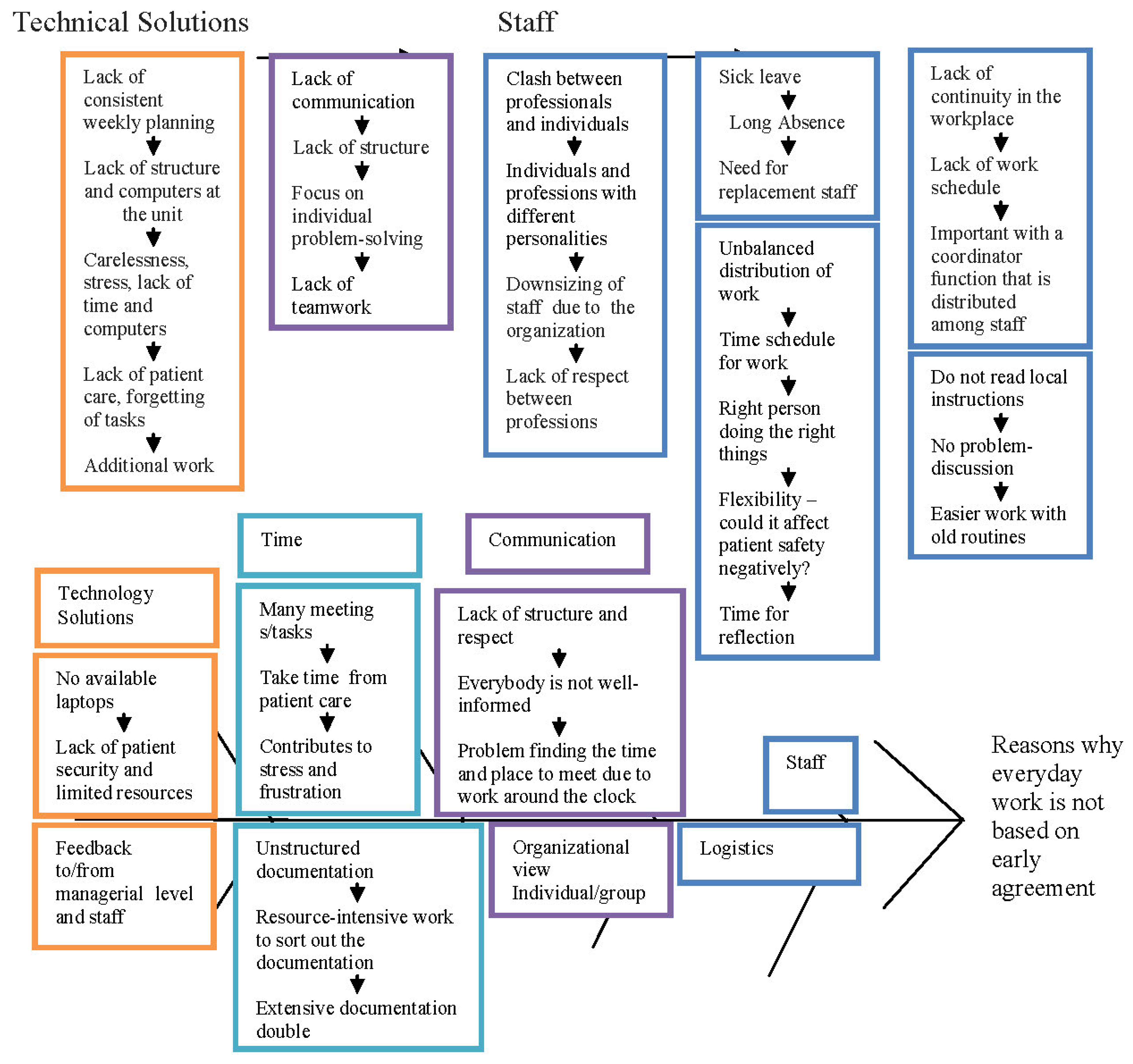
3. Results and Discussion
3.1. Results
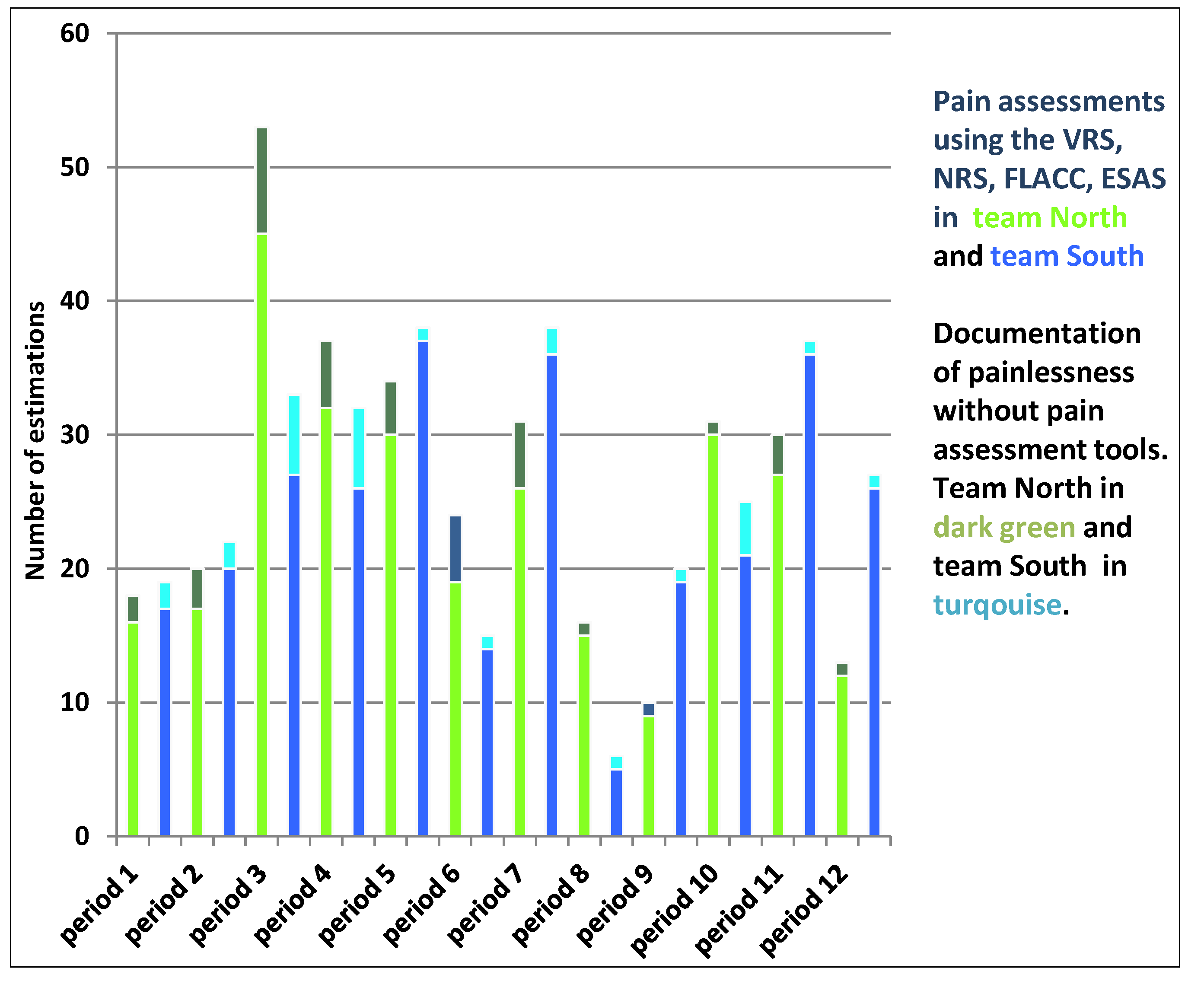
3.1.1. Documentation of Pain Management
| Pain management | North T1 | % | South | % | NorthT2 | % | South | % | NorthT3 | % | South | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of patients with pain | 7(41) | 17 | 7(39) | 18 | 19(24) | 79 | 11(28) | 39 | 2(28) | 7 | 27(53) | 51 |
| Number of pain assessments | 12(41) | 29 | 14(39) | 36 | 17(24) | 71 | 11(28) | 39 | 23(28) | 82 | 28(53) | 53 |
| Estimated pain > 4 | 1(41) | 2 | 5(39) | 13 | 5(24) | 21 | 3(28) | 11 | 5(28) | 18 | 5(53) | 9 |
| Number of pain analyses | 2(41) | 5 | 3(39) | 8 | 8(24) | 33 | 2(28) | 7 | 3(28) | 11 | 2(53) | 4 |
| Pain Estimation | Number of Pain Estimates | Percentage of Total Number of Pain Estimates (%) |
|---|---|---|
| 0 | 224 | 40% |
| 1 | 35 | 6% |
| 2 | 55 | 10% |
| 3 | 71 | 13% |
| 4 | 42 | 8% |
| 5 | 40 | 7% |
| 6 | 23 | 4% |
| 7 | 29 | 5% |
| 8 | 29 | 5% |
| 9 | 5 | 1% |
| 10 | 8 | 1% |
| Total | 561 | 100% |
| 14 days | Number of Patients with Documentation of Pain | Percentage of Total Number of Patients with Documentation of Pain (%) |
|---|---|---|
| 10–23 October 2012 | 10/14 patients (North) | 71 |
| 12/16 patients (South) | 75 | |
| 24 October–6 November 2012 | 16/20 patients (North) | 80 |
| 9/14 patients (South) | 64 | |
| 7–20 November 2012 | 18/21 patients (North) | 86 |
| 10/12 patients (South) | 83 | |
| 21 November–4 December 2012 | 11/14 patients (North) | 78 |
| 9/12 patients (South) | 75 | |
| 5–18 December 2012 | 10/14 patients (North) | 71 |
| 9/12 patients (South) | 75 | |
| 19 December 2012–1 January 2013 | 10/12 patients (North) | 83 |
| 11/12 patients (South) | 92 | |
| 2–15 January 2013 | 13/15 patients (North) | 87 |
| 16/16 patients (South) | 100 | |
| 31 January–13 February 2013 | 7/11 patients (North) | 64 |
| 10/11 patients (South) | 91 | |
| 14–27 February 2013 | 8/11 patients (North) | 73 |
| 13/13 patients (South) | 100 | |
| 28 February–13 March 2013 | 11/12 patients (North) | 92 |
| 13/15 patients (South) | 87 | |
| 14–27 March 2013 | 10/12 patients (North) | 83 |
| 10/12 patients (South) | 83 | |
| 28 March–10 April 2013 | 9/9 patients (North) | 100 |
| 6/8 patients (South) | 75 |
3.1.2. Pain Management Activities
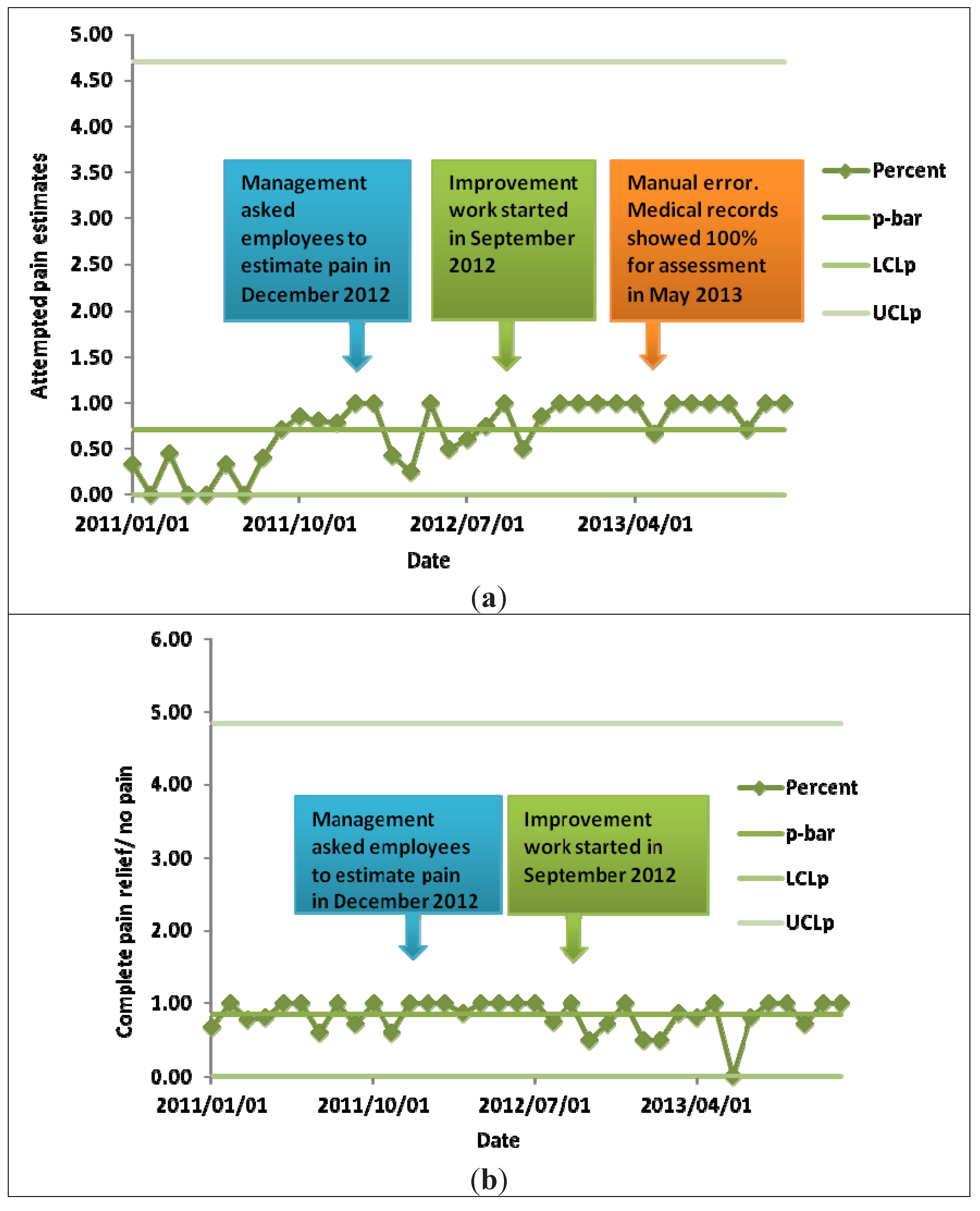
3.2. Discussion
|
3.3. Limitations
4. Conclusions
Author Contributions
Conflicts of Interest
References
- Batalden, P.; Davidoff, F. What is “quality improvement” and how can it transform healthcare? Qual. Saf. Health Care 2007, 16, 2–3. [Google Scholar] [CrossRef]
- Larsen, D. Using real time patient feedback to introduce safety changes. Nurs. Manag. 2011, 18, 27–31. [Google Scholar] [CrossRef]
- National Board of Health and Welfare. Nationellt. kunskapsstöd för god palliativ vård i livets slutskede. Vägledning, rekommendationer och indikatorer, Stöd. för styrning och ledning; National Board of Health and Welfare: Stockholm, Sweden, 2013. (In Swedish) [Google Scholar]
- Hilarius, D.L.; Kloeg, P.H.; van der Wall, E.; Komen, M.; Gundy, M.C.; Aaronson, N.K. Cancer-related fatigue: Clinical practice versus practice guidelines. Support. Care Cancer 2011, 19, 531–538. [Google Scholar] [CrossRef]
- Crites, G.E.; McNamara, M.C.; Akl, E.A.; Richardson, W.S.; Umscheid, C.A.; Nishikawa, J. Evidence in the learning organisation. Health Res. Policy Syst. 2009, 7, 1–13. [Google Scholar] [CrossRef]
- Grol, R.; Grimshaw, J. From best evidence to best practice: Effective implementation of change in patients’ care. Lancet 2003, 36, 1225–1230. [Google Scholar] [CrossRef]
- Håkonsen, G.; Strelec, P.; Campbell, D.; Hudson, S.; Loennechen, T. Adherence to Medication Guideline Criteria in Cancer Pain Management. J. Pain Symp. Manag. 2008, 37, 1006–1018. [Google Scholar]
- National Board of Health and Welfare. Nationellt. vårdprogram för palliativ vård; National Board of Health and Welfare: Stockholm, Sweden, 2012. (In Swedish) [Google Scholar]
- Batalden, P. The leader’s work in the improvement of healthcare. Qual. Saf. Health Care 2010, 19, 367–368. [Google Scholar]
- Lugtenberg, M.; Burgers, J.S.; Besters, C.F.; Han, D.; Westert, G.P. Perceived barriers to guideline adherence: A survey among general practitioners. BMC Fam. Pract. 2011, 12, 1–9. [Google Scholar]
- Argyris, C.; Schön, D. Theory in Practice: Increasing Professional Effectiveness; Jossey-Bass: San-Francisco, CA, USA, 1974. [Google Scholar]
- Argyris, C.; Schön, D. Organizational Learning: A Theory of Action Perspective; Addison-Wesley: New York, NY, USA, 1995. [Google Scholar]
- Garcia-Morales, V.J.; Verdú-Jover, A.; Lloréns, F.J. The influence of CEO perceptions on the level of organizational learning: Single-loop and double-loop learning. Int. J. Manpower 2009, 30, 567–590. [Google Scholar] [CrossRef]
- Langley, G.J.; Moen, R.D.; Nolan, K.M.; Nolan, T.W.; Norman, C.L.; Provost, L.P. The Improvement Guide. In A Practical Approach to Enhancing Organizational Performance; Jossey-Bass: San Francisco, CA, USA, 2009. [Google Scholar]
- Bradely, E.H.; Holmboe, E.S.; Mattera, S.A.; Roumanis, S.A.; Radford, M.J.; Krumholz, H.M. Data feedback efforts in quality improvement: Lessons learned from US hospitals. Qual. Saf. Health Care 2004, 13, 26–31. [Google Scholar]
- Preheim, G.J.; Armstrong, G.E.; Barton, A.J. The New Fundamentals in Nursing: Introducing Beginning Quality and Safety Education for Nurses’ Competencies. J. Nurs. Educ. 2009, 48, 694–697. [Google Scholar] [CrossRef]
- Gilbert, J.E.; Howell, D.; King, S.; Sawka, C.; Hughes, E.; Angus, H.; Dudgeon, D. Quality Improvement in Cancer Symptom Assessment and Control: The Provincial Palliative Care Integration Project (PPCIP). J. Pain Symp. Manag. 2012, 43, 663–678. [Google Scholar] [CrossRef]
- Rushmer, R.; Voigt, D. MEASURE IT, IMPROVE IT: The Safer Patients Initiative and quality improvement in subcutaneous insulin therapy for hospital in-patients. Diabet. Med. 2008, 25, 960–967. [Google Scholar] [CrossRef]
- Thakkar, K.; Gilchrist, M.; Dickinson, E.; Benn, J.; Franklin, B.D.; Jacklin, A. A quality improvement program to increase compliance with an anti-infective prescribing policy. J. Antimicrob. Chemother. 2011, 66, 1916–1920. [Google Scholar] [CrossRef]
- Van Tiel, F.H.; Elenbaas, T.W.; Voskuilen, B.M.; Herczeg, J.; Verheggen, F.W.; Mochtar, B.; Stobberingh, E.E. Plan-do-study-act cycles as an instrument for improvement of compliance after cardiothoracic surgery. J. Hosp. Infect. 2006, 62, 64–70. [Google Scholar]
- Nelson, E.; Godfrey, M.; Batalden, P.; Berry, S.A.; Bothe, A.E.; McKinley, K.E.; Melin, C.N.; Muethin, S.E.; Moore, G.; Wasson, J.H.; et al. Clinical Microsystem, Part 1. The Building Blocks of Health Systems. Joint Comm. J. Qual. Patient Saf. 2008, 34, 367–378. [Google Scholar]
- Rosengren, K.; Kullén Engström, A.; Axelsson, L. The staff’s experience of structural changes in the health and medical service in western Sweden. J. Nurs. Manag. 1999, 7, 289–298. [Google Scholar]
- Kullén Engström, A.; Rosengren, K.; Hallberg, L. Balancing involvement: Employees’ experiences of merging hospitals in Sweden. J. Adv. Nurs. 2002, 38, 11–18. [Google Scholar] [CrossRef]
- Kaplan, H.C.; Provost, L.P.; Froehle, C.M.; Margolis, P.A. The Model for Understanding Success in Quality (MUSIQ): Building a theory of context in healthcare quality improvement. BMJ Qual. Saf. 2012, 21, 13–20. [Google Scholar] [CrossRef]
- Clarke, J.R.; Lerner, J.C.; Marella, W. The Role for Leaders of Health Care Organizations in Patient Safety. Am. J. Med. Qual. 2007, 22, 311–318. [Google Scholar] [CrossRef]
- Arnold, J.; Randall, R. Work Psychology: Understanding Human Behavior in the Workplace; Pearson Education Limited: Essex, UK, 2010. [Google Scholar]
- Decuyper, S.; Dochy, F.; van den Bossche, P. Grasping the dynamic complexity of team learning: An integrative model for effective team learning in organisations. Educ. Res. Rev. 2010, 5, 111–113. [Google Scholar]
- Porter, M.E. Value in Health Care. Appendix 1. Value in Health Care. N. Engl. J. Med. 2010, 363, 2477–2481. [Google Scholar] [CrossRef]
- Rosengren, K.; Athlin, E.; Segesten, K. Presence and availability: Staff conceptions of nursing leadership on an intensive care unit. J. Nurs. Manag. 2007, 15, 522–529. [Google Scholar] [CrossRef]
- Rosengren, K.; Höglund, P.; Hedberg, B. Quality register: A tool for patient advantages—From a caring perspective. J. Nurs. Manag. 2012, 20, 196–205. [Google Scholar] [CrossRef]
- Senge, P. The Fifth Discipline: The art and Practice of the Learning Organization; Currency Doubleday: London, UK, 2006. [Google Scholar]
- International Association for Study of Pain (IASP). Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definitions of Pain Terms/Prepared by the Task Force on Taxonomy of the International Association for the Study of Pain; IASP Press: Seattle, DC, USA, 1994; pp. 209–214. [Google Scholar]
- Patrick, D.L.; Ferketich, S.L.; Frame, P.S.; Harris, J.J.; Hendricks, C.B.; Levin, B. National Institutes of Health State-of-the-Science Conference Statement: Symptom management in cancer: Pain, depression, and fatigue, 15–17 July 2002. J. Nat. Cancer Inst. Monogr. 2004, 32, 9–16. [Google Scholar]
- Raphael, J.; Ahmedzai, S.; Hester, J.; Urch, C.; Barrie, J.; Williams, J. Cancer pain: Part 1: Pathophysiology; oncological, pharmacological, and psychological treatments: A perspective from the British Pain Society endorsed by the UK Association of Palliative Medicine and the Royal College of General Practitioners. Pain Med. 2010, 11, 742–764. [Google Scholar]
- Chang, V.T.; Sorger, B.; Rosenfeld, K.E.; Lorenz, K.A.; Bailey, A.F.; Pharm, T.B.; Weinberger, L.; Montagnini, M. Pain and palliative medicine. J. Rehabil. Res. Dev. 2007, 44, 279–294. [Google Scholar] [CrossRef]
- Melzack, R.; Katz, J. Pain measurement in persons in pain. In Textbook of Pain; Wall, P.D., Melzack, R., Eds.; Churchill Livingstone: London, UK, 1999; pp. 1341–1352. [Google Scholar]
- Voepel-Lewis, T.; Merkel, S.; Tait, A.R.; Trzcinka, A.; Malviya, S. The reliability and validity of the Face, Legs, Activity, Cry, Consolability observational tool as a measure of pain in children with cognitive impairment. Anasth. Analg. 2002, 95, 1224–1229. [Google Scholar]
- Bruera, E.; Khuen, N.; Miller, M.J.; Selmser, P.; Macmillan, K. The Edmonton Symptom Assessment System (ESAS). A simple method for the assessment of palliative care patients. J. Palliat. Care 1991, 7, 6–9. [Google Scholar]
- Polit, D.; Beck, C.T. Nursing Research: Generating and Assessing Evidence for Nursing Practice; Wolters Kluwer Health/Lippincott Williams & Wilkins cop.: Philadelphia, PA, USA, 2012. [Google Scholar]
- Eriksson, M.; Appelros, P.; Norrving, B.; Tere’nt, A.; Stegmayr, B. Assessment of functional outcome in a national quality register for acute stroke: Can simple self-reported items be transformed into the modified ranking scale? Stroke 38, 1384–1386. [Google Scholar]
- Swedish Palliative Registry. Svenska. Palliativregistret. Available online: http://palliativ.se/?page_id=99/ (accessed on 15 April 2014).
- Nilsson, K. Dokumentation. av symtom i avancerad palliativ vård. En journalgranskningsstudie. Thesis Master i Nursing, Department for Health and Society, University College of Kristianstad, Kristianstad, Sweden, 2012. [Google Scholar]
- Thor, J.; Herrlin, B.; Wittlöv, K.; Övretvieit, J.; Brommels, M. Evolution and outcomes of a quality improvement program. Int. J. Health Care 2010, 23, 312–327. [Google Scholar]
- Bryman, A. Social Research Methods; Oxford University Press: Oxford, UK, 2008. [Google Scholar]
- Carey, R.G. Improving Healthcare with Control Charts Basic and Advanced SPC Methods and Case Studies; American Society for Quality (ASQ): Milwaukee, WI, USA, 2003. [Google Scholar]
- Codex. Rules & Guidelines for Research. The Humanities and Social Sciences. Available online: http://www.codex.vr.se/en/forskninghumsam.shtml/ (accessed on 15 April 2014).
- Swedish Code of Statutes. Hälso-och sjukvårdslagen. 1982:763. Available online: http://www.socialstyrelsen.se/regelverk/lagarochforordningar (accessed on 10 June 2014). (In Swedish)
- Antonovsky, A. The Salutogenic Model as a theory to guide Health Promotion. Health Promot. Int. 1996, 11, 11–18. [Google Scholar]
- Unné, A.; Rosengren, K. Staffs Experience of Pain Management—An Improvement in Palliative Care. Pharmacy 2013, 1, 119–136. [Google Scholar]
- Baszanger, I. Inventing Pain Medicine: From the Laboratory to the Clinic; Rutgers University Press: London, UK, 1998. [Google Scholar]
- Baszanger, I. Deciphering chronic pain. Sociol. Health Illn. 1992, 14, 181–215. [Google Scholar]
- Ekman, I.; Wolf, A.; Olsson, L.-E.; Taft, C.; Dudas, K.; Schaufelberger, M.; Swedberg, K. Effects of person-centered care in patients with chronic heart failure: The PCC-HF study. Eur. Heart J. 2012, 33, 1112–1119. [Google Scholar]
- Politi, M.; Clark, M.; Ombao, H.; Dizon, D.; Elwyn, G. Communicating uncertainty can lead to less decision satisfaction: a necessary cost of involving patients in shared decision making? Health Expect. 2011, 14, 84–91. [Google Scholar]
- Abernethy, A.; Wheeler, J.; Bull, J. Development of a Health Information Technology-Based Data System in Community-Based Hospice and Palliative Care. Am. J. Prev. Med. 2011, 40, S217–S224. [Google Scholar] [CrossRef]
- Bull, J.H.; Whitten, E.; Morris, J.; Hooper, R.N.; Wheeler, J.; Kamal, A.; Abernethy, A.P. Demonstration of a Sustainable Community-Based Model of Care across the Palliative Care Continuum. J. Pain Symtom. Manag. 2012, 44, 797–806. [Google Scholar] [CrossRef]
- Caines, A.; Samadi, N.; Ouimet, G.; Thompson, A.; Pope, J. The sensitivity and specificity of pain diagrams in rheumatic disease referrals. Rheumatology 2012, 51, 1093–1098. [Google Scholar] [CrossRef]
- Ripamonti, C.I. Pain management. Ann. Oncol. 2012, 23, x294–x301. [Google Scholar]
- Keogh, E.; Rosser, B.; Eccleston, C. e-Health and chronic pain management: Current status and developments. Pain 2010, 151, 18–21. [Google Scholar]
- Wantland, D.J.; Portillo, C.J.; Holzemer, W.L.; Slaughter, R.; McGhee, E.M. The effectiveness of Web-based vs. non-Web-based interventions: A meta-analysis of behavioral change outcomes. J. Med. Internet Res. 2004, 6, e40. [Google Scholar]
- SCB. Privatpersoners. användning av datorer och internet 2011. Available online: http://www.scb.se/statistik/_publikationer/LE0108_2011A02_BR_IT01BR1201.pdf (accessed on 18 March 2014). (In Swedish)
- Ullrich, P.F.; Vaccaro, A.R. Patient education on the internet: Opportunities and pitfalls. Spine 2002, 27, E185–E188. [Google Scholar] [CrossRef]
- Center för eHälsa i samverkan. Handlingsplan 2012–2018. Landsting, regioners och kommuners samarbetet inom eHälsoområdet. Available online: http://www.cehis.se/en (accessed on 30 December 2013).
- Swedish eHealth Agency (2014). Available online: http://www.ehalsomyndigheten.se/Om-oss-/Uppdrag-och-verksamhet/Other-languages1/Swedish-eHealth-Agency/ (accessed on 20 January 2014).
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Unné, A.; Rosengren, K. Using Numbers Creates Value for Health Professionals: A Quantitative Study of Pain Management in Palliative Care. Pharmacy 2014, 2, 205-221. https://doi.org/10.3390/pharmacy2030205
Unné A, Rosengren K. Using Numbers Creates Value for Health Professionals: A Quantitative Study of Pain Management in Palliative Care. Pharmacy. 2014; 2(3):205-221. https://doi.org/10.3390/pharmacy2030205
Chicago/Turabian StyleUnné, Anna, and Kristina Rosengren. 2014. "Using Numbers Creates Value for Health Professionals: A Quantitative Study of Pain Management in Palliative Care" Pharmacy 2, no. 3: 205-221. https://doi.org/10.3390/pharmacy2030205
APA StyleUnné, A., & Rosengren, K. (2014). Using Numbers Creates Value for Health Professionals: A Quantitative Study of Pain Management in Palliative Care. Pharmacy, 2(3), 205-221. https://doi.org/10.3390/pharmacy2030205




