Clinical Outcomes of Pharmacist Involvement in Cardiac Arrest and Trauma Resuscitations: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Study ID | Design | Sample Size | Country | Event | Primary Outcomes |
|---|---|---|---|---|---|
| Amini, 2013 [19] | Retrospective Cohort | 100 | USA | Trauma | PP decreased overall length of stay in the ED |
| Bolt, 2015 [7] | Survey | 43 | CAN | Cardiac | Institutions with PP on the CPR team saw increased ACLS guideline—medication compliance |
| Bond, 1999 [20] | Statistical Analyses | 1029 | USA | Cardiac | PP clinical services decreased mortality (40,478 fewer deaths/year) |
| Cooper, 2007 [21] | Chart Review | 46 | USA | Cardiac | PP increased ACLS medication compliance (therapy recommendation and drug dosage adjustment) |
| Currey, 2024 [14] | Systematic Review | 30 Full-Texts | AUS | Cardiac Trauma | PP increased compliance with ACLS guidelines and reduced medication errors |
| Draper, 2008 [8] | Retrospective Analysis | 74 | USA | Cardiac | PP improved medication compliance and reduced MI- related medication errors—significant PP improved survival to hospital discharge and decreased mortality |
| Ernst, 2012 [22] | Cross- Sectional Cohort Study | 694 | USA | Cardiac Trauma | PP reduced medication errors |
| Fairbanks, 2008 [23] | Quality Improvement | 72 | USA | ED | PP reduced rate of medication errors |
| Felh, 2017 [24] | Retrospective Quasi- Experimental | Pre: 234 Post: 157 | USA | Cardiac | PP did not cause significant difference in time to hospital discharge |
| Groth, 2016 [25] | Evaluation of Pilot Program Study | 32 | USA | Cardiac | PP increased ACLS medication compliance (therapy addition) PP decreased patient escalation of care |
| Hashemipour, 2013 [26] | Quality Improvement | Pre: 54 Post: 32 | USA | Cardiac | PP increased ACLS medication compliance (not significant) PP decreased number of cardiac arrests |
| Heavner, 2018 [27] | Retrospective Chart Review | Pre: 26 CA Post: 54 CA | USA | Cardiac | PP increased ACLS compliance—significant PP improved acute event survival to hospital admission—significant |
| Lada, 2007 [28] | Quality Improvement | 34 | USA | N/A | PP prevented medication errors |
| Lamkin, 2019 [29] | Retrospective: Cohort Chart Review | 1082 Study PP: 782 Control PA: 300 | USA | Trauma | PP increased proper use of Lidocaine and decreased medication errors—significant |
| McAllister, 2017 [30] | Retrospective Analysis | PP: 20 PA: 45 | USA | Cardiac | PP increased ACLS medication compliance—significant PP increased survival to hospital admission and discharge—significant |
| McGinnis, 2022 [13] | Quality Improvement | 19-RRT Activations 104 Interventions | USA | Cardiac | PP decreased medication errors |
| Ray, 2024 [31] | Survey | 184 | USA | Cardiac | PP optimized preparation, administration of resuscitative medication |
| Robb, 2003 [32] | Questionnaire | 164 | UK | Cardiac | PP optimized medication preparation and simplified ACLS algorithm |
| Roman 2024 [15] | Unblinded Randomized Control Trial | Control: 37 Study: 43 | AUS | Trauma | PP reduced medication errors (able to prescribe medications) PP did not cause significant difference in length of stay in ED or hospital |
| Study ID | Country | Event | Secondary Outcomes |
|---|---|---|---|
| Al Harbi, 2006 [33] | USA | Cardiac | Majority of pharmacists were BLS-certified (n = 30) Fewer pharmacists were ACLS-certified (n = 20) ACLS-trained pharmacists (n = 16/20) were confident in providing drug information in a CPR situation vs. non-ACLS-trained pharmacists (n = 4/27) ACLS-trained pharmacists (n = 14/20) were confident in recommending a drug during a CPR situation vs. non-ACLS-trained pharmacists (n = 4/27) |
| Bolt, 2015 [7] | CAN | Cardiac | Majority (n = 30/43) of organizations had less than 25 FTE pharmacists Majority (n = 27/43) of organizations had less than 50% of pharmacists who completed residency Several (n = 8/43) organizations cited staff coverage issues as barriers to further pharmacist integration on code teams |
| Bond, 1999 [20] | USA | Cardiac | Pharmacists’ services in 4 key areas were associated with cost avoidance through mortality prevention
|
| Cooper, 2007 [21] | USA | Cardiac | There were 17 FTE pharmacists and 4 clinical specialist FTEs All pharmacists were either certified in ACLS or passed a certification test to participate oin CPR teams |
| Ernst, 2012 [22] | USA | Cardiac Trauma | Clinical pharmacists are available 10 h/day on a non- on-call basis, allowing for comparison of PA vs. PP |
| Felh, 2017 [24] | USA | Cardiac | 20 pharmacists comprised of staff pharmacists, pharmacy residents |
| Groth, 2016 [25] | USA | Cardiac | Program was developed by 2 ACLS pharmacists trained in clinical care and emergency medicine |
| Hale, 2009 [34] | USA | Trauma | 27/161 trauma centers (17%) that did not consider integration of pharmacists into trauma team cited staffing difficulties 19/161 trauma centers (12%) that did not consider integration of pharmacists into trauma team cited cost concerns |
| Hashemipour, 2013 [26] | USA | Cardiac | 75.6% of institution pharmacists were in practice for 5+ years—ACLS- and BLS-certified Pharmacists reported increased confidence following training program completion Pharmacists are rotated to cover for code pharmacists’ absence |
| Heavner, 2018 [27] | USA | Cardiac | Lead pharmacist, PGY2 pharmacy residents acquired ACLS training |
| Lada, 2007 [28] | USA | N/A | The extrapolated cost avoidance for a one-year period = USD $3,089,328. |
| Machado, 2003 [35] | USA | Cardiac | Most participating institutions (n = 90/149) had 5 FTE pharmacists Most non-participating institutions (n = 191/286) had 5 FTE pharmacists Majority of pharmacists (n = 301/381) pharmacists were CPR-trained Fewer participant pharmacists (n = 140/380) were ACLS-trained Fewer non-participant pharmacists (n = 118/723) were ACLS-trained 78% of routine CPR participant emergency pharmacists felt they were adequately trained to respond to codes (p < 0.001) 25.4% of non-participants felt adequately trained (p < 0.001) |
| Marlowe, 2005 [36] | USA | Cardiac | Pharmacists reported increased confidence on a scale (0–5) in regards to various code team responsibilities (pre- vs. post-program) Calculate doses of resuscitation medications to be drawn up 3.54 ± 0.43 vs. 3.96 ± 0.2; p = 0.015 |
| McAllister, 2017 [30] | USA | Cardiac | Annual cost avoidance provided by a single full-time pharmacist = USD$ 321,308 per year |
| Ray, 2024 [31] | USA | Cardiac | Most participants (38%) had 4–7 years of practical experience Majority of participants (61%) reported 19–24 h of dedicated EMP coverage |
| Robb, 2003 [32] | UK | Cardiac | All pharmacists who attended cardiac arrest events received 4H training in BLS and 8H training in ACLS Resident pharmacists attended arrests overnight, on weekends; enabled 24H coverage |
| Roman 2024 [15] | AUS | Trauma | EM Pharmacists have at least 2 years of clinical experience in hospital pharmacy practice EM pharmacists responded to trauma callouts from Monday to Friday (07:00–21:00 h) |
| Shimp, 1995 [37] | USA | Cardiac | BLS = 66/160 pharmacy graduates who responded (41%) On a 5-point scale, all pharmacists ranked their confidence as 3.2 ± 1.2 in their ability to perform CPR-BLS
|
| Toma, 2007 [38] | USA Puerto Rico | Cardiac | Majority of staff pharmacists were BLS-trained (n = 62) but fewer were ACLS-trained (n = 46) Majority of clinical pharmacists were BLS-trained (n = 67) and a similar number were ACLS-trained (n = 55) Majority of PGY1 pharmacists were BLS-trained (n = 91) but fewer were ACLS-trained (n = 77)—highest proportion Majority of staff pharmacists were BLS-trained (n = 48) and a similar number were ACLS-trained (n = 41) |
| Wanbon, 2015 [39] | CAN | N/A | Many pharmacists (n = 27/56) had completed hospital residency Majority of pharmacists (n = 30/52) were CPR-certified but a lesser amount (n = 17/52) were ACLS- certified |
| Selection | Comparability | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|
| Reference | D1 | D2 | D3 | D4 | D5 | D6 | D7 | D8 |
| Amini, 2013 [19] |  |  |  |  |  |  |  |  |
| Bolt, 2015 [7] |  |  |  |  |  |  |  |  |
| Bond, 1999 [20] |  |  |  |  |  |  |  |  |
| Cooper, 2007 [21] |  |  |  |  |  |  |  |  |
| Currey, 2024 [14] |  |  |  |  |  |  |  |  |
| Draper, 2008 [8] |  |  |  |  |  |  |  |  |
| Ernst, 2012 [22] |  |  |  |  |  |  |  |  |
| Fairbanks, 2008 [23] |  |  |  |  |  |  |  |  |
| Feih, 2017 [24] |  |  |  |  |  |  |  |  |
| Groth, 2016 [25] |  |  |  |  |  |  |  |  |
| Heavner, 2018 [27] |  |  |  |  |  |  |  |  |
| Lada, 2007 [28] |  |  |  |  |  |  |  |  |
| Lamkin, 2019 [29] |  |  |  |  |  |  |  |  |
| McAllister, 2017 [30] |  |  |  |  |  |  |  |  |
| McGinnis, 2022 [13] |  |  |  |  |  |  |  |  |
| Ray, 2024 [31] |  |  |  |  |  |  |  |  |
| Robb, 2003 [32] |  |  |  |  |  |  |  |  |
| Roman, 2024 [15] |  |  |  |  |  |  |  |  |
| Wanbon, 2015 [39] |  |  |  |  |  |  |  |  |
Judgement
D2: How was the non-exposed group selected? (Selection bias.) D3: How was the exposure ascertained? (Selection bias.) D4: Did the study demonstrate that the outcome of interest was not present at the start of the study? (Selection bias.) D5: Comparability of groups on the basis of the design or analysis controlled for confounders (Comparability bias.) D6: How was the outcome assessed? (Outcome bias.)D7: Was follow-up long enough for outcomes to occur? (Outcome bias.)D8: Was the follow-up of subjects adequate? (Outcome bias.) | ||||||||
3. Results
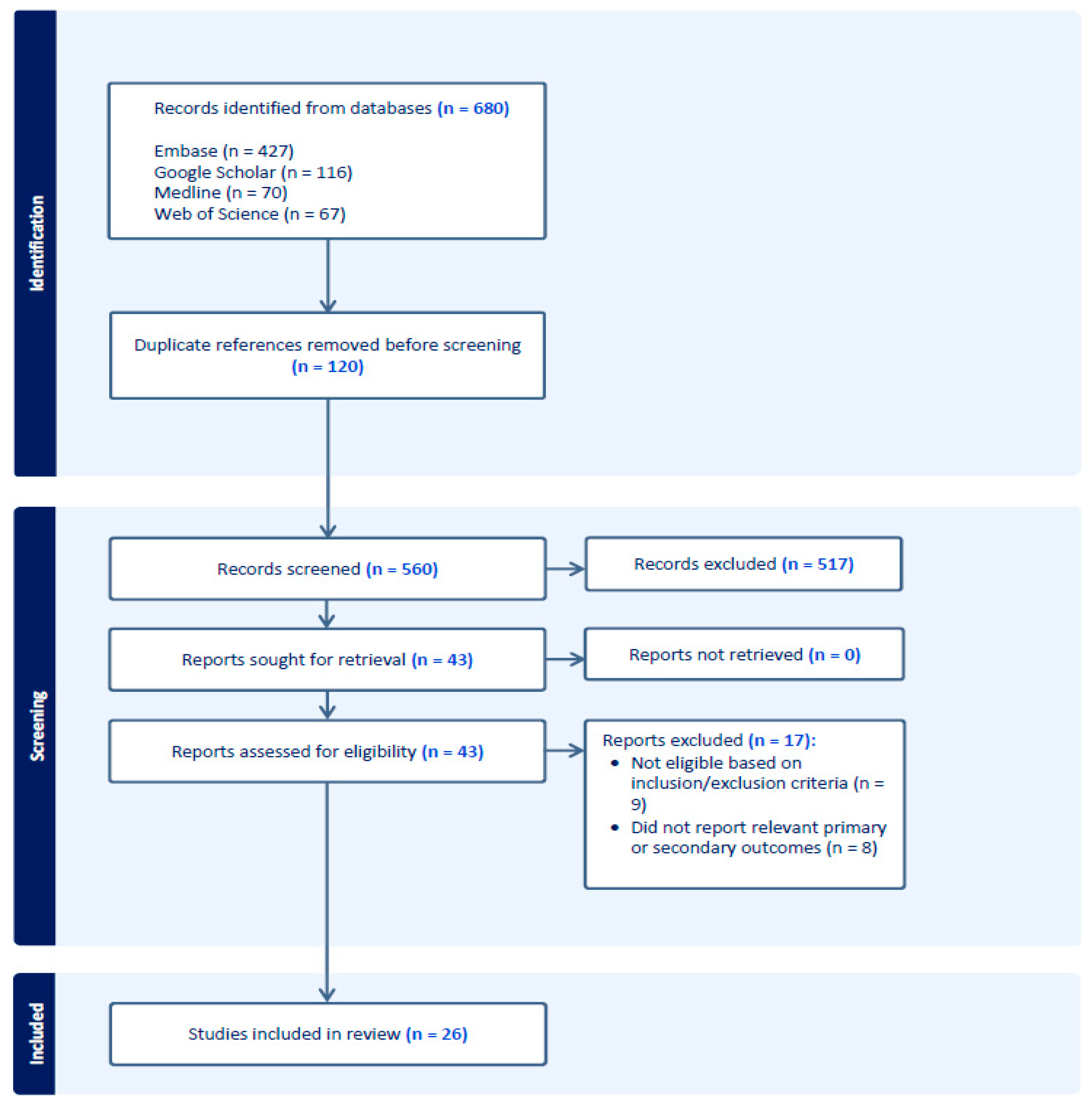
3.1. Study Selection
3.2. Study Characteristics
3.3. Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ACLS | Advanced cardiac life support |
| AUS | Australia |
| BLS | Basic life support |
| CA | Cardiac arrest |
| CAN | Canada |
| CPR | Cardiopulmonary resuscitation |
| ED | Emergency department |
| EM | Emergency medicine |
| EMP | Emergency medicine pharmacists |
| MI | Myocardial infarction |
| PA | Pharmacist absent |
| PGY1 | Post-graduate year 1 |
| PGY2 | Post-graduate year 2 |
| PP | Pharmacist present |
| RRT | Rapid response team |
| USA | United States of America |
| UK | United Kingdom |
Appendix A
| # | Query | Results from September 2024 |
|---|---|---|
| 1 | (clinical pharmacist or pharmacist).mp. [mp = title, book title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms, population supplementary concept word, anatomy supplementary concept word] | 105, 162 |
| 2 | exp Heart Arrest/ | 134, 089 |
| 3 | exp cardiopulmonary resuscitation/or exp advanced cardiac life support/ | 135, 798 |
| 4 | exp resuscitation/ | 141, 227 |
| 5 | (cardiac resuscitation or trauma resuscitation or cardiac arrest* or advanced cardiac life support or ACLS or CPR or code blue or trauma response team).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword heading word, floating subheading word, candidate term word] | 101, 636 |
| 6 | exp advanced cardiac life support/ | 836 |
| 7 | exp emergency ward/ | 234, 541 |
| 8 | exp emergency health service/ | 354, 546 |
| 9 | exp emergency medicine/ | 49, 973 |
| 10 | (emergency department or emergency ward or emergency medicine or trauma cent*).mp. [mp = title, abstract, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword heading word, floating subheading word, candidate term word] | 365, 707 |
| 11 | 1 or 2 | 134, 089 |
| 12 | 3 or 4 or 5 or 6 | 254, 491 |
| 13 | 7 or 8 or 9 or 10 | 449, 850 |
| 14 | 11 and 12 and 13 | 194 |
| 15 | 11 amd 12 | 661 |
| 16 | Limit 15 to Embase | 425 |
| # | Query | Results from September 2024 |
|---|---|---|
| 1 | ((clinical pharmacist or pharmacist).mp. [mp = title, book title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms, population supplementary concept word, anatomy supplementary concept word] | 23, 024 |
| 2 | exp Heart Arrest/ | 58, 590 |
| 3 | exp cardiopulmonary resuscitation/or exp advanced cardiac life support/ | 23, 543 |
| 4 | (cardiac arrest* or trauma resuscitation or cardiac resuscitation or ACLS or CPR or code blue or trauma response team).mp. [mp = title, book title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms, population supplementary concept word, anatomy supplementary concept word] | 61, 585 |
| 5 | exp emergency service, hospital/or exp trauma centers/ | 104, 613 |
| 6 | (emergency medicine or emergency department or emergency ward or trauma cent*).mp. [mp = title, book title, abstract, original title, name of substance word, subject heading word, floating sub-heading word, keyword heading word, organism supplementary concept word, protocol supplementary concept word, rare disease supplementary concept word, unique identifier, synonyms, population supplementary concept word, anatomy supplementary concept word] | 176, 604 |
| 7 | 2 and 5 | 1, 179 |
| 8 | exp Pharmacists/ | 23, 136 |
| 9 | 1 or 8 | 35, 346 |
| 10 | 2 or 3 or 4 | 96, 620 |
| 11 | 5 or 6 | 211, 697 |
| 12 | 9 and 10 | 70 |
| 13 | 9 and 10 and 11 | 25 |
| # | Query | Results from September 2024 |
|---|---|---|
| 1 | (“clinical pharmacists” OR “hospital pharmacists”) AND (“emergency department”) AND (“cardiac arrest” OR “trauma resuscitation”) AND (“advanced cardiac life support” OR “ACLS”) | 116 |
References
- Clinical Pharmacist Services in the Emergency Department. Ann. Emerg. Med. 2021, 77, e127–e133. [CrossRef] [PubMed]
- American College of Medical Toxicology. The Role of Clinical Pharmacists in the Emergency Department [Internet]; ACMT: Phoenix, AZ, USA, 2017; Available online: https://www.acmt.net/wp-content/uploads/2022/06/PRS_170804_The-Role-of-Clinical-Pharmacists-in-the-Emergency-Department.pdf (accessed on 5 June 2025).
- Eppert, H.D.; Reznek, A.J.; American Society of Health-System Pharmacists. ASHP guidelines on emergency medicine pharmacist services. Am. J. Health Syst. Pharm. 2011, 68, e81–e95. [Google Scholar] [CrossRef] [PubMed]
- Farmer, B.M.; Hayes, B.D.; Rao, R.; Farrell, N.; Nelson, L. The Role of Clinical Pharmacists in the Emergency Department. J. Med. Toxicol. 2018, 14, 114–116. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Morgan, S.R.; Acquisto, N.M.; Coralic, Z.; Basalyga, V.; Campbell, M.; Kelly, J.J.; Langkiet, K.; Pearson, C.; Sokn, E.; Phelan, M. Clinical pharmacy services in the emergency department. Am. J. Emerg. Med. 2018, 36, 1727–1732. [Google Scholar] [CrossRef]
- Punj, E.; Collins, A.; Agravedi, N.; Marriott, J.; Sapey, E. What is the evidence that a pharmacy team working in an acute or emergency medicine department improves outcomes for patients: A systematic review. Pharmacol. Res. Perspect. 2022, 10, e01007. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Bolt, J.; Semchuk, W.; Loewen, P.; Bell, A.; Strugari, C. A Canadian Survey of Pharmacist Participation during Cardiopulmonary Resuscitation. Can. J. Hosp. Pharm. 2015, 68, 290. [Google Scholar] [CrossRef]
- Draper, H.M.; Eppert, J.A. Association of Pharmacist Presence on Compliance with Advanced Cardiac Life Support Guidelines During In-Hospital Cardiac Arrest. Ann. Pharmacother. 2008, 42, 469–474. [Google Scholar] [CrossRef]
- Bingham, A.L.; Kavelak, H.L.; Hollands, J.M.; Finn, L.A.; Delic, J.J.; Schroeder, N.; Cawley, M.J. Advanced cardiac life support certification for student pharmacists improves simulated patient survival. Curr. Pharm. Teach. Learn. 2020, 12, 975–980. [Google Scholar] [CrossRef]
- Scarponcini, T.R.; Edwards, C.J.; Rudis, M.I.; Jasiak, K.D.; Hays, D.P. The role of the emergency pharmacist in trauma resuscitation. J. Pharm. Pract. 2011, 24, 146–159. [Google Scholar] [CrossRef] [PubMed]
- Patanwala, A.E.; Hays, D.P. Pharmacist’s activities on a trauma response team in the emergency department. Am. J Health Syst. Pharm. 2010, 67, 1536–1538. [Google Scholar] [CrossRef] [PubMed]
- Montgomery, K.; Hall, A.B.; Keriazes, G. Pharmacist’s impact on acute pain management during trauma resuscitation. J. Trauma Nurs. 2015, 22, 87–90. [Google Scholar] [CrossRef] [PubMed]
- McGinnis, C.; Kim, C.; Qureshi, A.; Scholle, C.; Ramanan, R. Evaluation and Perception of Clinical Pharmacist Participation in a Rapid Response Team During Cardiopulmonary Resuscitation. Qual. Manag. Health Care 2022, 31, 34–37. [Google Scholar] [CrossRef]
- Currey, E.M.; Falconer, N.; Isoardi, K.Z.; Barras, M. Impact of pharmacists during in-hospital resuscitation or medical emergency response events: A systematic review. Am. J. Emerg. Med. 2024, 75, 98–110. [Google Scholar] [CrossRef]
- Roman, C.; Dooley, M.; Fitzgerald, M.; Smit, V.; Cameron, P.; Mitra, B. Pharmacists in Trauma: A randomised controlled trial of emergency medicine pharmacists in trauma response teams. Emerg. Med. J. 2024, 41, 397–403. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Pollock, D.; Peters, M.D.J.; Khalil, H.; McInerney, P.; Alexander, L.; Tricco, A.C.; Evans, C.; de Moraes, É.B.; Godfrey, C.M.; Pieper, D.; et al. Recommendations for the extraction, analysis, and presentation of results in scoping reviews. JBI Evid. Synth. 2023, 21, 520–532. [Google Scholar] [CrossRef]
- Aromataris, E.; Lockwood, C.; Porritt, K.; Pilla, B.; Jordan, Z. (Eds.) JBI Manual for Evidence Synthesis; JBI: Adelaide, Australia, 2024; ISBN 978-0-6488488-2-0. Available online: https://synthesismanual.jbi.global (accessed on 5 June 2025).
- Amini, A.; Faucett, E.A.; Watt, J.M.; Amini, R.; Sakles, J.C.; Rhee, P.; Erstad, B.L.; Patanwala, A.E. Effect of a pharmacist on timing of postintubation sedative and analgesic use in trauma resuscitations. Am. J. Health Syst. Pharm. 2013, 70, 1513–1517. [Google Scholar] [CrossRef] [PubMed]
- Bond, C.A.; Raehl, C.L.; Pitterle, M.E. Staffing and the cost of clinical and hospital pharmacy services in United States hospitals. Pharmacotherapy 1999, 19, 767–781. [Google Scholar] [CrossRef] [PubMed]
- Cooper, B.E. Pharmacist involvement in a rapid-response team at a community hospital. Am. J. Health Syst. Pharm. 2007, 64, 694–698. [Google Scholar] [CrossRef]
- Ernst, A.A.; Weiss, S.J.; Sullivan, A., 4th; Sarangarm, D.; Rankin, S.; Fees, M.; Sarangarm, P. On-site pharmacists in the ED improve medical errors. Am. J. Emerg. Med. 2012, 30, 717–725. [Google Scholar] [CrossRef] [PubMed]
- Fairbanks, R.J. Results of the Emergency Pharmacist Outcomes Study. In Proceedings of the ASHP Mid-Year Meeting, Las Vegas, NV, USA, 5 December 2007. [Google Scholar]
- Feih, J.; Peppard, W.J.; Katz, M. Pharmacist involvement on a rapid response team. Am. J. Health Syst. Pharm. 2017, 74, S10–S16. [Google Scholar] [CrossRef] [PubMed]
- Groth, C.M.; Acquisto, N.M. Pharmacists as members of the rapid response team. J. Pharm. Pract. 2014, 29, 116–120. [Google Scholar] [CrossRef]
- Hashemipour, Z.; Delgado, G., Jr.; Dehoorne-Smith, M.; Edwin, S.B. Pharmacist integration into cardiac arrest response teams. Am. J. Health Syst. Pharm. 2013, 70, 662, 664, 666–667. [Google Scholar] [CrossRef] [PubMed]
- Heavner, M.S.; Rouse, G.E.; Lemieux, S.M.; Owusu, K.A.; IX, D.P.; Yazdi, M.; Lee, L.A. Experience with integrating pharmacist documenters on cardiac arrest teams to improve quality. J. Am. Pharm. Assoc. 2018, 58, 311–317. [Google Scholar] [CrossRef] [PubMed]
- Lada, P.; Delgado, G., Jr. Documentation of pharmacists’ interventions in an emergency department and associated cost avoidance. Am. J. Health Syst. Pharm. 2007, 64, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Lamkin, L.; Lindsey, S.; Weant, K.; Shoff, H.; Pinkston, C. Implications of the presence of an emergency medicine pharmacist during critical care trauma patient resuscitation. J. Am. Coll. Clin. Pharm. 2019, 2, 251–256. [Google Scholar] [CrossRef]
- McAllister, M.W.; Chestnutt, J.G. Improved outcomes and cost savings associated with pharmacist presence in the Emergency Department. Hosp. Pharm. 2017, 52, 433–437. [Google Scholar] [CrossRef]
- Ray, L.; Acquisto, N.M.; Coralic, Z.; Feldman, R.; Mercer, K.; Zimmerman, D.E.; Howington, G.T.; Slocum, G.W.; Faine, B.; Rech, M.A. A national survey of medication utilization for cardiac resuscitation in the emergency department: A survey of emergency medicine pharmacists. Am. J. Health Syst. Pharm. 2024, 81, 1313–1321. [Google Scholar] [CrossRef] [PubMed]
- Robb, C.M.; Douglas, N.; McKechnie, E.; Upton, D. An evaluation of the pharmacist’s role on a cardiac arrest team. Hosp. Pharm. 2003, 10, 22–24. [Google Scholar]
- Harbi, S.A.; Miller, D. Pharmacists’ attitudes toward ACLS provider training program. Am. J. Health Syst. Pharm. 2006, 63, 1000–1003. [Google Scholar] [CrossRef]
- Hale, L.S.; Nyberg, S.M.; Mohr, A.M.; Wegner-Busch, E.K. Preliminary national survey of pharmacist involvement in trauma resuscitation. Am. J. Health Syst. Pharm. 2009, 66, 797–798. [Google Scholar] [CrossRef] [PubMed]
- Machado, C.; Barlows, T.G., III; Marsh, W.A.; Coto-Depani, Y.; Dalin, G. Pharmacists on the emergency cardiopulmonary resuscitation team: Their responsibilities, training, and attitudes. Hosp. Pharm. 2003, 38, 40–49. [Google Scholar] [CrossRef]
- Marlowe, K.F.; Woods, D.D. Evaluating a Training Program for Pharmacist Code Blue Response. Hosp. Pharm. 2005, 40, 49–54. [Google Scholar] [CrossRef]
- Shimp, L.A.; Mason, N.A.; Toedter, N.M.; Atwater, C.B.; Gorenflo, D.W. Pharmacist participation in cardiopulmonary resuscitation. Am. J. Health Syst. Pharm. 1995, 52, 980–984. [Google Scholar] [CrossRef] [PubMed]
- Toma, M.B.; Winstead, P.S.; Smith, K.M.; Lewis, D.A.; Clifford, T.M. Pharmacy resident participation in cardiopulmonary resuscitation events. Am. J. Health Syst. Pharm. 2007, 64, 747–753. [Google Scholar] [CrossRef]
- Wanbon, R.; Lyder, C.; Villeneuve, E.; Shalansky, S.; Manuel, L.; Harding, M. Clinical pharmacy services in Canadian emergency departments: A national survey. Can. J. Hosp. Pharm. 2015, 68, 191–201. [Google Scholar] [CrossRef]
- Zanza, C.; Romenskaya, T.; Zuliani, M.; Piccolella, F.; Bottinelli, M.; Caputo, G.; Rocca, E.; Maconi, A.; Savioli, G.; Longhitano, Y. Acute traumatic pain in the Emergency Department. Diseases 2023, 11, 45. [Google Scholar] [CrossRef]
- Fabbri, A.; Voza, A.; Riccardi, A.; Serra, S.; Iaco, F.; Study and Research Center of the Italian Society of Emergency Medicine (SIMEU). The pain management of trauma patients in the Emergency Department. J. Clin. Med. 2023, 12, 3289. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Patel, H.; Wee, M.; Tejani, A.M.; Lau, A. Clinical Outcomes of Pharmacist Involvement in Cardiac Arrest and Trauma Resuscitations: A Scoping Review. Pharmacy 2025, 13, 89. https://doi.org/10.3390/pharmacy13040089
Patel H, Wee M, Tejani AM, Lau A. Clinical Outcomes of Pharmacist Involvement in Cardiac Arrest and Trauma Resuscitations: A Scoping Review. Pharmacy. 2025; 13(4):89. https://doi.org/10.3390/pharmacy13040089
Chicago/Turabian StylePatel, Harshita, Myles Wee, Aaron M. Tejani, and Anthony Lau. 2025. "Clinical Outcomes of Pharmacist Involvement in Cardiac Arrest and Trauma Resuscitations: A Scoping Review" Pharmacy 13, no. 4: 89. https://doi.org/10.3390/pharmacy13040089
APA StylePatel, H., Wee, M., Tejani, A. M., & Lau, A. (2025). Clinical Outcomes of Pharmacist Involvement in Cardiac Arrest and Trauma Resuscitations: A Scoping Review. Pharmacy, 13(4), 89. https://doi.org/10.3390/pharmacy13040089







