How Do Pharmacists Distribute Their Work Time during a Clinical Intervention Trial?—A Time and Motion Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. The Pharmacist Intervention
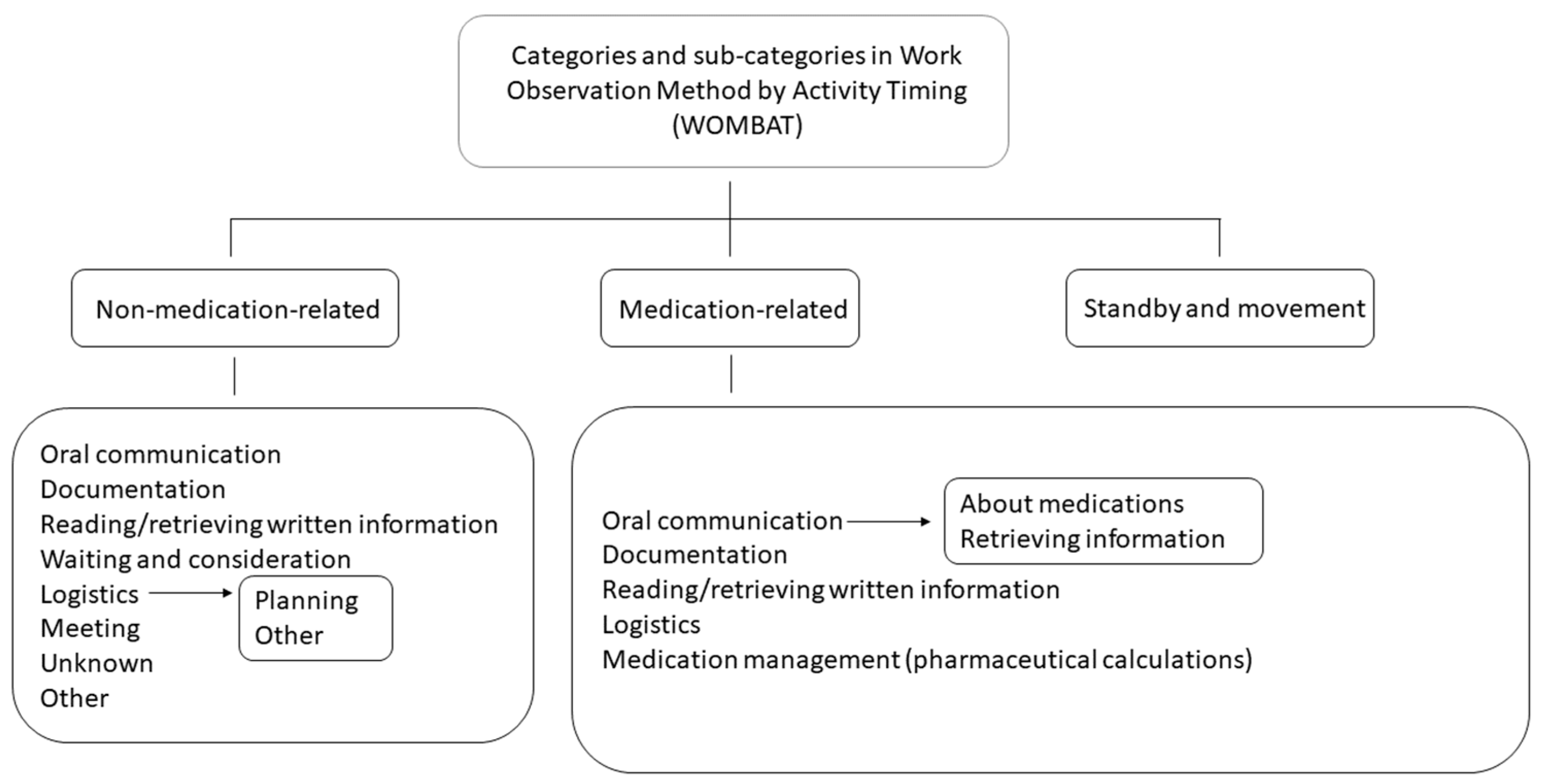
2.3. Data Collection Tool and Piloting
2.4. Data Collection
2.5. Data Analysis
2.6. Ethics
3. Results
3.1. Distributions of Pharmacists’ Work Time per Task
3.2. Where the Pharmacists Were
3.3. Face-to-Face Interactions
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morganti, K.G.; Bauhoff, S.; Blanchard, J.C.; Abir, M.; Iyer, N.; Smith, A.; Vesely, J.V.; Okeke, E.N.; Kellermann, A.L. The Evolving Role of Emergency Departments in the United States. Rand Health Q. 2013, 3, 3. [Google Scholar]
- Farmer, B.M.; Hayes, B.D.; Rao, R.; Farrell, N.; Nelson, L. The Role of Clinical Pharmacists in the Emergency Department. J. Med. Toxicol. 2018, 14, 114–116. [Google Scholar] [CrossRef]
- Chui, M.A.; Pohjanoksa-Mäntylä, M.; Snyder, M.E. Improving medication safety in varied health systems. Res. Social. Adm. Pharm. 2019, 15, 811–812. [Google Scholar] [CrossRef]
- Darraj, A.; Hudays, A.; Hazazi, A.; Hobani, A.; Alghamdi, A. The Association between Emergency Department Overcrowding and Delay in Treatment: A Systematic Review. Healthcare 2023, 11, 385. [Google Scholar] [CrossRef]
- Johnsgard, T.; Elenjord, R.; Lehnbom, E.C.; Risor, T.; Zahl-Holmstad, B.; Vesela Holis, R.; Hugaas Ofstad, E.; Garcia, B.H. Emergency department physicians’ experiences and perceptions with medication-related work tasks and the potential role of clinical pharmacists. Int. J. Qual. Stud. Health Well-Being 2023, 18, 2226941. [Google Scholar] [CrossRef]
- Nymoen, L.D.; Tran, T.; Walter, S.R.; Lehnbom, E.C.; Tunestveit, I.K.; Oie, E.; Viktil, K.K. Emergency department physicians’ distribution of time in the fast paced-workflow-a novel time-motion study of drug-related activities. Int. J. Clin. Pharm. 2022, 44, 448–458. [Google Scholar] [CrossRef]
- Johnsgård, T.; Elenjord, R.; Holis, R.V.; Waaseth, M.; Zahl-Holmstad, B.; Fagerli, M.; Svendsen, K.; Lehnbom, E.C.; Ofstad, E.H.; Risør, T.; et al. How much time do emergency department physicians spend on medication-related tasks? A time- and-motion study. BMC Emerg. Med. 2024, 24, 56. [Google Scholar] [CrossRef]
- Holis, R.V.; Garcia, B.H.; Lehnbom, E.C.; Fagerli, M.; Majeed, A.; Johnsgard, T.; Zahl-Holmstad, B.; Svendsen, K.; Waaseth, M.; Skjold, F.; et al. How much time do nurses in Norwegian emergency departments spend on different work tasks with and without a clinical pharmacist present—A time and motion study. submitted.
- Kukielka, E.; Jones, R. Medication Safety in the Emergency Department: A Study of Serious Medication Errors Reported by 101 Hospitals from 2011 to 2020. Patient Saf. 2022, 4, 49–59. [Google Scholar] [CrossRef]
- Nymoen, L.D.; Björk, M.; Flatebø, T.E.; Nilsen, M.; Godø, A.; Øie, E.; Viktil, K.K. Drug-related emergency department visits: Prevalence and risk factors. Intern. Emerg. Med. 2022, 17, 1453–1462. [Google Scholar] [CrossRef]
- Khalil, H.; Kynoch, K.; Hines, S. Interventions to ensure medication safety in acute care: An umbrella review. Int. J. Evid. Based Healthc. 2020, 18, 188–211. [Google Scholar] [CrossRef]
- Kooda, K.; Canterbury, E.; Bellolio, F. Impact of Pharmacist-Led Antimicrobial Stewardship on Appropriate Antibiotic Prescribing in the Emergency Department: A Systematic Review and Meta-Analysis. Ann. Emerg. Med. 2022, 79, 374–387. [Google Scholar] [CrossRef]
- Nguyen, P.M.; Nguyen, K.T.; Pham, S.T.; Thanh Le, V.T.; Thi Le, T.C.; Diep, H.G.; Minh Le, N.N.; Vinh Ly, H.H.; Nhu Nguyen, T.T.; Lam, A.N.; et al. Pharmacist-Led Interventions to Reduce Drug-Related Problems in Prescribing for Pediatric Outpatients in a Developing Country: A Randomized Controlled Trial. J. Pediatr. Pharmacol. Ther. 2023, 28, 212–221. [Google Scholar] [CrossRef]
- Dietrich, S.K.; Bushong, B.T.; Schneider-Smith, E.A.; Mixon, M.A. Emergency medicine pharmacist interventions reducing exposure to costs (EMPIRE-C). Am. J. Emerg. Med. 2022, 54, 178–183. [Google Scholar] [CrossRef]
- Dager, W.E.; Branch, J.M.; King, J.H.; White, R.H.; Quan, R.S.; Musallam, N.A.; Albertson, T.E. Optimization of inpatient warfarin therapy: Impact of daily consultation by a pharmacist-managed anticoagulation service. Ann. Pharmacother. 2000, 34, 567–572. [Google Scholar] [CrossRef]
- Rahman, R.N.; Nikolik, B.; de Ridder, M.A.J.; Hoek, A.E.; Janssen, M.J.A.; Schuit, S.C.E.; Karapinar-Çarkit, F.; van den Bemt, P.M.L.A. The effect of emergency department pharmacists on drug overuse and drug underuse in patients with an ADE-related hospitalisation: A controlled intervention study. BMC Health Serv. Res. 2022, 22, 1363. [Google Scholar] [CrossRef]
- Atey, T.M.; Peterson, G.M.; Salahudeen, M.S.; Bereznicki, L.R.; Wimmer, B.C. Impact of pharmacist interventions provided in the emergency department on quality use of medicines: A systematic review and meta-analysis. Emerg. Med. J. 2023, 40, 120–127. [Google Scholar] [CrossRef]
- Grill, J.; Bryant, C.; Markel, K.; Wisniewski, S.J. A study of time saved by emergency medicine physicians through working with clinical pharmacists in the emergency department. Am. J. Emerg. Med. 2019, 37, 1720–1722. [Google Scholar] [CrossRef]
- Yeung, E.Y.; Mohammed, R.S. What tasks can physicians delegate to pharmacists? Br. J. Gen. Pract. 2018, 68, 519. [Google Scholar] [CrossRef]
- Garcia, B.H.; Halvorsen, K.H. Klinisk Praksis—En Veletablert Undervisningsform i Tromsø. Norsk Farmaceutisk Tidsskrift [Internet]. 2020. Available online: https://www.farmatid.no/artikler/klinisk-praksis-en-veletablert-undervisningsform-tromso (accessed on 7 January 2021).
- Vesela, R.; Elenjord, R.; Lehnbom, E.C.; Ofstad, E.H.; Johnsgard, T.; Zahl-Holmstad, B.; Risor, T.; Wisloff, T.; Roslie, L.; Filseth, O.M.; et al. Integrating the clinical pharmacist into the emergency department interdisciplinary team: A study protocol for a multicentre trial applying a non-randomised stepped-wedge study design. BMJ Open 2021, 11, e049645. [Google Scholar] [CrossRef]
- Ballermann, M.A.; Shaw, N.T.; Mayes, D.C.; Gibney, R.T.; Westbrook, J.I. Validation of the Work Observation Method By Activity Timing (WOMBAT) method of conducting time-motion observations in critical care settings: An observational study. BMC Med. Inform. Decis. Mak. 2011, 11, 32. [Google Scholar] [CrossRef]
- Westbrook, J.I.; Li, L.; Georgiou, A.; Paoloni, R.; Cullen, J. Impact of an electronic medication management system on hospital doctors’ and nurses’ work: A controlled pre-post, time and motion study. J. Am. Med. Inform. Assoc. 2013, 20, 1150–1158. [Google Scholar] [CrossRef]
- Glantz, A.; Ormon, K.; Sandstrom, B. “How do we use the time?”—An observational study measuring the task time distribution of nurses in psychiatric care. BMC Nurs. 2019, 18, 67. [Google Scholar] [CrossRef]
- Lehnbom, E.C.; Li, L.; Prgomet, M.; Lam, W.Y.; Westbrook, J.I. Little Things Matter: A Time and Motion Study of Pharmacists’ Activities in a Paediatric Hospital. Stud. Health Technol. Inform. 2016, 227, 80–86. [Google Scholar]
- Walter, S.R.; Dunsmuir, W.T.M.; Raban, M.Z.; Westbrook, J.I. Understanding Clinical Workflow Through Direct Continuous Observation: Addressing the Unique Statistical Challenges. In Cognitive Informatics: Reengineering Clinical Workflow for Safer and More Efficient Care; Zheng, K., Westbrook, J., Kannampallil, T.G., Patel, V.L., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 191–210. [Google Scholar] [CrossRef]
- Gleason, K.M.; McDaniel, M.R.; Feinglass, J.; Baker, D.W.; Lindquist, L.; Liss, D.; Noskin, G.A. Results of the Medications at Transitions and Clinical Handoffs (MATCH) study: An analysis of medication reconciliation errors and risk factors at hospital admission. J. Gen. Intern. Med. 2010, 25, 441–447. [Google Scholar] [CrossRef]
- Vira, T.; Colquhoun, M.; Etchells, E. Reconcilable differences: Correcting medication errors at hospital admission and discharge. Qual. Saf. Health Care 2006, 15, 122–126. [Google Scholar] [CrossRef]
- Curatolo, N.; Gutermann, L.; Devaquet, N.; Roy, S.; Rieutord, A. Reducing medication errors at admission: 3 cycles to implement, improve and sustain medication reconciliation. Int. J. Clin. Pharm. 2015, 37, 113–120. [Google Scholar] [CrossRef]
- American College of Clinical, P.; Hume, A.L.; Kirwin, J.; Bieber, H.L.; Couchenour, R.L.; Hall, D.L.; Kennedy, A.K.; LaPointe, N.M.; Burkhardt, C.D.; Schilli, K.; et al. Improving care transitions: Current practice and future opportunities for pharmacists. Pharmacotherapy 2012, 32, e326–e337. [Google Scholar] [CrossRef]
- Khalil, V.; deClifford, J.M.; Lam, S.; Subramaniam, A. Implementation and evaluation of a collaborative clinical pharmacist’s medications reconciliation and charting service for admitted medical inpatients in a metropolitan hospital. J. Clin. Pharm. Ther. 2016, 41, 662–666. [Google Scholar] [CrossRef]
- Jordan, J.N.; Wadsworth, T.G.; Robinson, R.; Hruza, H.; Paul, A.; O’Connor, S.K. Patient Satisfaction with Pharmacist-Provided Health-Related Services in a Primary Care Clinic. Pharmacy 2021, 9, 187. [Google Scholar] [CrossRef]
- Dreischulte, T.; van den Bemt, B.; Steurbaut, S.; the European Society of Clinical, P. European Society of Clinical Pharmacy definition of the term clinical pharmacy and its relationship to pharmaceutical care: A position paper. Int. J. Clin. Pharm. 2022, 44, 837–842. [Google Scholar] [CrossRef]
- Hughes, E.; Terry, D.; Huynh, C.; Petridis, K.; Aiello, M.; Mazard, L.; Ubhi, H.; Terry, A.; Wilson, K.; Sinclair, A. Future enhanced clinical role of pharmacists in Emergency Departments in England: Multi-site observational evaluation. Int. J. Clin. Pharm. 2017, 39, 960–968. [Google Scholar] [CrossRef]
- Crafford, L.; Kusurkar, R.A.; Bronkhorst, E.; Gous, A.G.S.; Wouters, A. Understanding of healthcare professionals towards the roles and competencies of clinical pharmacists in South Africa. BMC Health Serv. Res. 2023, 23, 290. [Google Scholar] [CrossRef]
- Nancarrow, S.A.; Booth, A.; Ariss, S.; Smith, T.; Enderby, P.; Roots, A. Ten principles of good interdisciplinary team work. Hum. Resour. Health 2013, 11, 19. [Google Scholar] [CrossRef]
- Kotter, J.P. Accelerate! Harv. Bus. Rev. 2012, 90, 44–52, 54–58, 149. [Google Scholar]
- Chen, E.Y.H.; Bell, J.S.; Ilomaki, J.; Corlis, M.; Hogan, M.E.; Caporale, T.; Van Emden, J.; Westbrook, J.I.; Hilmer, S.N.; Sluggett, J.K. Medication administration in Australian residential aged care: A time-and-motion study. J. Eval. Clin. Pract. 2021, 27, 103–110. [Google Scholar] [CrossRef]
- Bingham, G.; Tong, E.; Poole, S.; Ross, P.; Dooley, M. A longitudinal time and motion study quantifying how implementation of an electronic medical record influences hospital nurses’ care delivery. Int. J. Med. Inform. 2021, 153, 104537. [Google Scholar] [CrossRef]
- Richardson, L.C.; Lehnbom, E.C.; Baysari, M.T.; Walter, S.R.; Day, R.O.; Westbrook, J.I. A time and motion study of junior doctor work patterns on the weekend: A potential contributor to the weekend effect? Intern. Med. J. 2016, 46, 819–825. [Google Scholar] [CrossRef]
- Adair, J.G. The Hawthorne effect: A reconsideration of the methodological artifact. J. Appl. Psychol. 1984, 69, 334–345. [Google Scholar] [CrossRef]
- World Medical, A. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Bull. World Health Organ. 2001, 79, 373–374. [Google Scholar]
| EDs Total | ED1 | ED2 | |
|---|---|---|---|
| Total observed time, hh:mm:ss | 196:55:33 | 100:38:12 | 96:17:21 |
| Number of pharmacists observed | 10 | 4 | 6 |
| Number of sessions observed | 100 | 51 | 49 |
| Mean number of patients per session (min–max) | 5.83 (0–13) | 5.90 (0–13) | 5.76 (1–11) |
| Mean time per patient per session in hh:mm:ss (min–max) | 00:14:39 (00:00:37–01:54:54) | 00:13:58 (00:01:51–00:51:20) | 00:15:20 (00:00:37–01:54:54) |
| EDs Total | ED1 | ED2 | |||||
|---|---|---|---|---|---|---|---|
| Total observed time, hh:mm:ss | 196:55:33 | 100:38:12 | 96:17:21 | ||||
| % | (95% CI) | % | (95% CI) | % | (95% CI) | ||
| Medication-related | 41.8 | 42.8 | 40.8 | ||||
| Documentation | 16.2 | (14.6–17.7) | 15.2 | (13.3–17.5) | 17.2 | (15.1–19.6) | |
| Oral communication | 16.3 | (14.9–17.8) | 16.7 | (14.3–18.7) | 15.9 | (13.9–18.3) | |
| Retrieve information about medication use | 9.5 | (8.2–10.9) | 10.7 | (9.1–12.6) | 8.3 | (6.5–10.5) | |
| About medications | 6.8 | (6.0–7.6) | 6.0 | (4.9–7.1) | 7.7 | (6.7–8.8) | |
| Reading/retrieving written information | 9.6 | (8.8–10.4) | 9.1 | (8.2–10.3) | 10.0 | (8.9–11.4) | |
| Logistics | 0.1 | (0.0–0.3) | 0.2 | (0.0–0.5) | 0.0 | - | |
| Pharmaceutical calculations | 0.1 | (0.0–0.1) | 0.1 | (0.0–0.1) | 0.1 | (0.0–0.1) | |
| Non-medication-related | 41.8 | 47.0 | 36.3 | ||||
| Reading/retrieving written information | 17.9 | (16.6–19.1) | 19.7 | (17.9–21.5) | 16.0 | (14.5–17.9) | |
| Oral communication | 8.3 | (7.6–9.1) | 9.3 | (8.1–10.7) | 7.3 | (6.6–8.1) | |
| Logistics | 4.5 | (4.1–4.9) | 5.2 | (4.7–5.9) | 3.8 | (3.3–4.2) | |
| Planning | 4.4 | (4.1–4.8) | 5.1 | (4.6–5.6) | 3.8 | (3.3–4.2) | |
| Other logistics | 0.1 | (0.1–0.2) | 0.1 | (0.1–0.2) | 0.1 | (0.1–0.2) | |
| Meeting | 3.3 | (2.0–5.1) | 4.2 | (1.9–7.3) | 2.4 | (1.2–4.3) | |
| Other | 3.1 | (1.9–4.9) | 3.6 | (1.4–7.0) | 2.6 | (1.5–4.2) | |
| Waiting/consideration | 2.2 | (1.9–2.5) | 1.8 | (1.5–2.3) | 2.5 | (2.1–3.0) | |
| Documentation | 1.7 | (1.3–2.2) | 2.6 | (1.7–3.6) | 0.8 | (0.5–1.2) | |
| Confidential | 1.2 | (0.5–2.2) | 1.2 | (0.2–2.7) | 1.2 | (0.3–2.6) | |
| Standby and movement | 17.4 | 11.0 | 24.1 | ||||
| Standby | 13.6 | (11.5–15.5) | 6.9 | (4.9–9.4) | 20.5 | (17.4–23.9) | |
| Movement | 3.8 | (3.5–4.1) | 4.1 | (3.7–4.6) | 3.5 | (3.2–4.0) | |
| EDs Total | ED1 | ED2 | ||||
|---|---|---|---|---|---|---|
| Total observed time, hh:mm:ss | 196:55:33 | 100:38:12 | 96:17:21 | |||
| % | (95% CI) | % | (95% CI) | % | (95% CI) | |
| In the ED | 88.0 | (85.2–91.2) | 79.2 | (75.8–82.7) | 97.2 | (92.9–102.5) |
| Outside the ED | 11.4 | (9.2–14.1) | 20.1 | (15.4–24.8) | 2.3 | (1.5–3.4) |
| In the COVID-19 room | 0.4 | (0.2–1.0) | 0.5 | (0.3–0.9) | 0.4 | (0.0–0.8) |
| In the medicine room | 0.1 | (0.0–0.3) | 0.2 | (0.0–0.6) | 0.0 | (0.0–0.1) |
| EDs Total | ED1 | ED2 | |||||
|---|---|---|---|---|---|---|---|
| Total observed time, hh:mm:ss | 196:55:33 | 100:38:12 | 96:17:21 | ||||
| % | (95% CI) | % | (95% CI) | % | (95% CI) | ||
| In total | 22.0 | (21.2–22.9) | 22.7 | (21.4–23.9) | 21.4 | (20.2–22.6) | |
| With patients/relatives | 7.8 | (7.2–8.4) | 7.8 | (7.1–8.7) | 7.7 | (7.0–8.6) | |
| With physicians | 7.4 | (6.9–8.0) | 6.5 | (5.7–7.3) | 8.4 | (7.6–9.3) | |
| With pharmacists | 6.5 | (6.0–7.0) | 9.1 | (8.3–10.0) | 3.6 | (3.1–4.2) | |
| With nurses | 3.6 | (3.2–4.0) | 4.4 | (3.8–5.0) | 2.8 | (2.3–3.3) | |
| With others | 2.6 | (2.3–2.9) | 2.9 | (2.4–3.4) | 2.3 | (1.8–2.7) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holis, R.V.; Elenjord, R.; Lehnbom, E.C.; Andersen, S.; Fagerli, M.; Johnsgård, T.; Zahl-Holmstad, B.; Svendsen, K.; Waaseth, M.; Skjold, F.; et al. How Do Pharmacists Distribute Their Work Time during a Clinical Intervention Trial?—A Time and Motion Study. Pharmacy 2024, 12, 106. https://doi.org/10.3390/pharmacy12040106
Holis RV, Elenjord R, Lehnbom EC, Andersen S, Fagerli M, Johnsgård T, Zahl-Holmstad B, Svendsen K, Waaseth M, Skjold F, et al. How Do Pharmacists Distribute Their Work Time during a Clinical Intervention Trial?—A Time and Motion Study. Pharmacy. 2024; 12(4):106. https://doi.org/10.3390/pharmacy12040106
Chicago/Turabian StyleHolis, Renata Vesela, Renate Elenjord, Elin Christina Lehnbom, Sigrid Andersen, Marie Fagerli, Tine Johnsgård, Birgitte Zahl-Holmstad, Kristian Svendsen, Marit Waaseth, Frode Skjold, and et al. 2024. "How Do Pharmacists Distribute Their Work Time during a Clinical Intervention Trial?—A Time and Motion Study" Pharmacy 12, no. 4: 106. https://doi.org/10.3390/pharmacy12040106
APA StyleHolis, R. V., Elenjord, R., Lehnbom, E. C., Andersen, S., Fagerli, M., Johnsgård, T., Zahl-Holmstad, B., Svendsen, K., Waaseth, M., Skjold, F., & Garcia, B. H. (2024). How Do Pharmacists Distribute Their Work Time during a Clinical Intervention Trial?—A Time and Motion Study. Pharmacy, 12(4), 106. https://doi.org/10.3390/pharmacy12040106






