Pharmacist-Led Interventions for Medication Adherence in Patients with Chronic Kidney Disease: A Scoping Review
Abstract
:1. Introduction
Aim
2. Method
2.1. Study Selection
2.1.1. Participants
2.1.2. Concept
2.1.3. Context
2.1.4. Types of sources
2.2. Search Strategy
2.3. Extraction of Results and Data Synthesis
3. Results
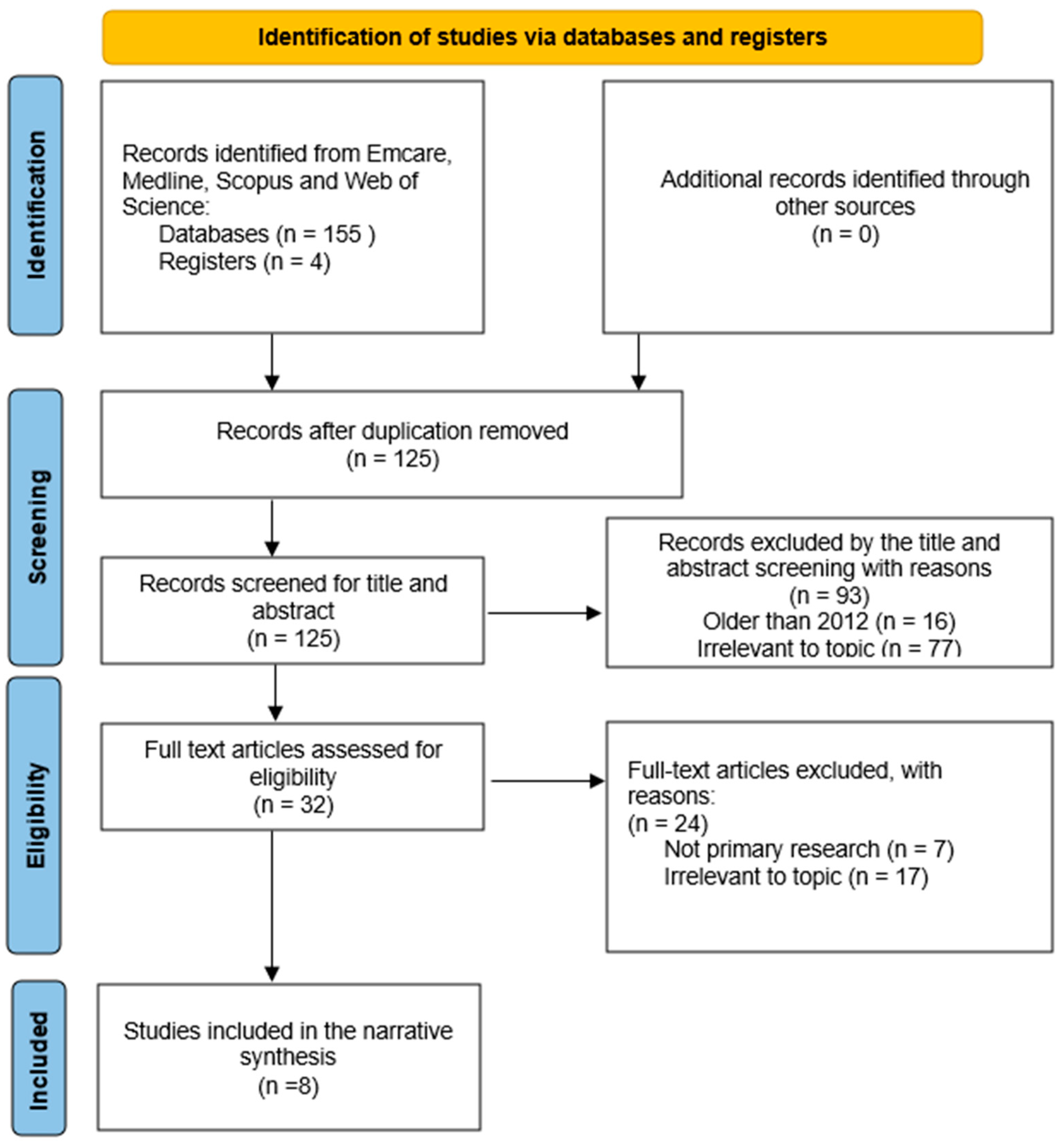
3.1. Study Selection
3.2. Characteristics of Included Studies
3.3. Barriers to Adherence
3.4. Interventions
3.5. Pharmacist and Patient Perceptions
3.6. Financial Implications
3.7. Overall Outcomes
| Author, Year, Country and Aim | Study Design: Participants: | Methodology (and Analysis) | Study Findings |
|---|---|---|---|
| Al-Abdelmuhsin et al., 2020, Saudi Arabia [20] To assess the satisfaction of patients undergoing hemodialysis regarding counselling services provided by pharmacists. | Study design: cross-sectional survey—self reporting questionnaire. Participants: n = 138 patients. Age: 51–75. On dialysis for 1–5 years with comorbidities. Setting: outpatient pharmacy service at hospital. | Methodology: 224 hemodialysis (HD) patients in the KAMC-Central Region (KAMC-CR) completed a satisfaction survey recording demographic data, HD duration, preferred counselling time, detailed medications list and preferred health professional for medication counselling. Analysis: descriptive data were summarized and analyzed using chi-square tests and Fisher’s exact tests (p < 0.05). | Barriers: ☒ Interventions: ☒ Perceptions: ☒ Financial Implications: ☒ Outcomes: ☒ pharmacists play an integral role in providing patients with knowledge regarding their treatment and thus improving their relationship with their often-extensive therapies. |
| Chandrasekhar et al., 2018, India [10] To evaluate the effect that various interventional methods have on medication adherence behaviors of patients with CKD. | Study design: prospective interventional study—modified Morisky eight item questionnaire and self-reporting questionnaire. Participants: n = 163 patients. Age (years): ≥76 (9%), 61–75 (40%), 46–60 (28%), 31–45 (16%), <30 (7%). 48% in stage 5 of CKD, 32% in stage 4 of CKD and remaining 20% were in stage 3 of CKD. None of the study subjects were in stage 1 or 2 of CKD. Setting: outpatient pharmacy service at hospital. | Methodology: the Modified Morisky 8 item Questionnaire (MMQS-8) was used to characterize patient adherence. Interventions including patient counselling, patient information leaflets and tele-health consults were provided to patients based on their adherence scores. Post-interventional patient adherence was recorded for comparison. Analysis: Chi square tests, independent t tests, ANOVA techniques and paired t tests were all used to analyze the statistical significance in adherence score changes and differences between participant groups. | Barriers: ☒ Interventions: ☒ Perceptions: ☒ Financial Implications: ☒ Outcomes: ☒ periodic counselling by clinical pharmacists of patients with CKD improves medication adherence through improving comprehension and removing misconceptions regarding the disease and therapy. Statistically significant association exist between medication adherence before and after intervention (p <0.001). |
| Cooney et al., 2015, USA [17] To evaluate the effect of a pharmacist-based quality improvement program on patient outcomes and adherence to CKD guidelines in a primary care setting. | Study design: pragmatic, randomized, controlled trial—direct measure of parathyroid hormone and blood pressure. Participants: n = 2199 patients. Age: mean—75.6 years. 76%—stage 1, 2, 3, 18%—stage 4, 6%—stage 4–5. Setting: outpatient pharmacy service at medical center. | Methodology: patients were selected from community based outpatient clinics (moderate to severe CKD). The intervention arm included pharmacist medicine reviews and counselling, pharmacist collaboration with physicians and the provision of information booklets to patients. Clinical outcomes indicated quality of life and all-cause mortality recorded as indicators. Analysis: for categorical outcomes, control and interventional arms were compared using Chi-squared tests. Impact of interventions evaluated using t tests. | Barriers: ☒ Interventions: ☒ Perceptions: ☒ Financial Implications: ☒ Outcomes: ☒ pharmacist-led medication reviews, counselling, collaboration with physicians and patient information resources improved medication adherence in patients with CKD. |
| Daifi et al., 2021, USA [15] To evaluate the impact of a clinical pharmacist in a single hemodialysis (HD) facility on patient medication outcomes and compliance. | Study design: retrospective observational descriptive study—clinician assessment of drug-related problems. Participants: n = 2000 patients. Age: mean 63 (26–92). All patients on hemodialysis. Setting: outpatient hemodialysis facility. | Methodology: HD patients clinical notes made by pharmacists during daily medication reconciliations and medication reviews were recorded in patient electronic medical records. Analysis: patterns in medication-related problems (MRP), drug classes associated with medication-related problems and overall outcomes were identified and considered. | Barriers: ☒ Interventions: ☒ Perceptions: ☒ Financial Implications: ☒ Outcomes: ☒ pharmacist interventions are an effective means of addressing medication-related programs for patients with CKD, resulting in improved medication adherence, patient outcomes and alleviating financial burden on the healthcare system. |
| Ghimire et al., 2018, Australia [9] To measure Australian renal-specialized pharmacists’ perceptions, current practices and barriers to assessing adherence in dialysis patients. | Study design: cross-sectional online survey—pharmacist survey. Participants: n = 41 renal-specialized pharmacists. Setting: Public and private dialysis units. | Methodology: survey questions (10 point Likert scale) demographics, medication adherence, contributors to nonadherence, perceived effectiveness of methods to identify adherence, barriers to assessing adherence and pharmacists’ confidence in assessing adherence. Analysis: descriptive analysis and analysis using Dunn–Bonferroni test to identify statistically significant differences between groups with a p-value threshold of <0.05. | Barriers: ☒ Interventions: ☒ Perceptions: ☒ Financial Implications: ☒ Outcomes: ☒ importance of a designated renal pharmacist in clinical settings for the assessment and counselling of dialysis patient medication adherence highlighted. |
| Qudah et al., 2016, Jordan [18] To evaluate the applicability of a physician and pharmacist collaborative model in the management of blood pressure in HD patients. | Study design: randomized controlled, block design clinical study—direct measure of blood pressure. Participants: n = 56 patients. Age: mean 52 years ± 18. Hemodialysis patients. Setting: inpatient hospital. | Methodology: in the interventional arm, pharmacists reviewed patient blood pressure (BP) readings and provided advise to physicians to optimize pharmacotherapy. Patients were also provided with educational materials and counselled by the pharmacist. Patient BP was used as the indicator for therapy efficacy. Analysis: continuous data were reported as mean ± standard deviation for normally distributed data and independent t-tests were used to detect differences. Categorical data were expressed as frequencies and percentages and compared using chi-squared tests. Significance was set to 0.05 and the confidence interval at 95%. | Barriers: ☒ Interventions: ☒ Perceptions: ☒ Financial Implications: ☒ Outcomes: ☒ implementation of collaborative pharmacist-physician interventions significantly improved medication adherence and patient outcomes. |
| Song et al., 2021, Korea [19] To analyze the effectiveness of clinical pharmacist services on drug-related problems and patient outcomes in in patients with chronic kidney disease (CKD). | Study design: prospective, randomized, parallel, controlled clinical trial—clinician assessment of drug related problems. Participants: n = 100 patients. Age: mean 51 years ± 17. Hemodialysis patients. Setting: inpatient hospital. | Methodology: The intervention group received pharmacist-led medication reconciliation, medication evaluation and management reviews and discharge pharmaceutical care transition (dPCT) services. Outcomes were measured using the number of drug-related problems (DRP) at discharge. Analysis: Categorical variables are presented as numbers and percentages; continuous parametric data is presented as mean values and standard deviations and nonparametric continuous data are represented as medians and interquartile ranges. | Barriers: ☒ Interventions: ☒ Perceptions: ☒ Financial Implications: ☒ Outcomes: ☒ hospital Pharmacist interventions resulted in a significant reduction in drug-related discrepancies (p < 0.001) in patients with CKD. |
| Yeung et al., 2017, USA [16] To design and investigate a pharmacist-run intervention using low health literacy flashcards and smartphone-activated quick response (QR) barcoded educational flashcard video to increase medication adherence and disease state understanding. | Study design: prospective, matched, quasi-experimental design—outcome measure—medication possession ratio. Participants: n = 34 participants. Age: mean 52 years ± 8. Patients with diabetes, heart failure and/or hypertension. Setting: community-oriented outpatient clinic. | Methodology: patients medication adherence was measured using the modified Pharmacy Quality Alliance Proportion of Days Covered (PDC) model. Interventional group patients were given targeted low health literacy educational resources. These included quick-response barcoded educational flashcards and videos regarding relevant medications. Post-interventional medication was then recorded for comparison. Analysis: descriptive statistics were used to describe demographic data and baseline patient characteristics. The Wilcoxon signed ranked test was used to compare the differences between the initial and post-interventional PDC results. | Barriers: ☒ Interventions: ☒ Perceptions: ☒ Financial Implications: ☒ Outcomes: ☒ pharmacist-led use of flashcards and QR-coded prescription bottles is an innovative and effective means of improving medication adherence and disease state understanding in low-health literacy patient populations. |
4. Discussion
4.1. Summary of Evidence
4.2. Condition- and Medication-Related Factors
4.3. Healthcare System and Healthcare Professional-Related Factors
4.4. Patient-Related Factors
4.5. Socioeconomic Factors
4.6. Strength and Limitations
4.7. Further Research and Knowledge Gaps
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kidney Health Australia. Chronic Kidney Disease (CKD) Management in Primary Care; Kidney Health Australia: Melbourne, VIC, Australia, 2020. [Google Scholar]
- Finkel, K.W.; Perazella, M.A.; Cohen, E.P. Onco-Nephrology, 1st ed.; Elsevier: Philadelphia, PA, USA, 2020. [Google Scholar]
- Australian Institute of Health and Welfare—Department of Health. Cardiovascular Disease, Diabetes and Chronic Kidney Disease: Australian Facts: Morbidity—Hospital Care 2014; Australian Institute of Health and Welfare: Canberra, ACT, Australia, 2014.
- Paneerselvam, G.S.; Aftab, R.; Sirisinghe, R.G.; Mei Lai, P.S.; Lim, S.K. Study protocol: Effectiveness of patient centered pharmacist care in improving medication adherence, clinical parameters and quality of life among hemodialysis patients. PloS ONE 2022, 17, e0263412. [Google Scholar] [CrossRef]
- Vrijens, B.; De Geest, S.; Hughes, D.A.; Przemyslaw, K.; Demonceau, J.; Ruppar, T.; Dobbels, F.; Fargher, E.; Morrison, V.; Lewek, P.; et al. A new taxonomy for describing and defining adherence to medications. Br. J. Clin. Pharmacol. 2012, 73, 691–705. [Google Scholar] [CrossRef]
- Peh, K.Q.E.; Kwan, Y.H.; Goh, H.; Ramchandani, H.; Phang, J.K.; Lim, Z.Y.; Loh, D.H.F.; Østbye, T.; Blalock, D.V.; Yoon, S.; et al. An Adaptable Framework for Factors Contributing to Medication Adherence: Results from a Systematic Review of 102 Conceptual Frameworks. J. Gen. Intern. Med. 2021, 36, 2784–2795. [Google Scholar] [CrossRef]
- Dinh, H.T.T.; Nguyen, N.T.; Bonner, A. Healthcare systems and professionals are key to improving health literacy in chronic kidney disease. J. Ren. Care 2022, 48, 4–13. [Google Scholar] [CrossRef] [PubMed]
- Kini, V.; Ho, P.M. Interventions to Improve Medication Adherence: A Review. JAMA 2018, 320, 2461–2473. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, S.; Banks, C.; Jose, M.D.; Castelino, R.L.; Zaidi, S.T.R. Renal pharmacists’ perceptions and current practices of assessing medication adherence in dialysis patients. Int. J. Clin. Pharm. 2018, 40, 26–35. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekhar, D.; Ganesan, G.V.; Sreekumar, S.; Pradeep, A.; Geoji, A.S.; George, A.E.; Vipinachadran, A. Impact of Intensified Pharmaceutical Interventions in Medication Adherence in Chronic Kidney Disease Patients. J. Young Pharm. 2018, 10, 208–212. [Google Scholar] [CrossRef]
- Bosworth, H.B. Enhancing medication adherence. In The Public Health Dilemma, 1st ed.; Springer Healthcare Ltd.: Tarporley, UK, 2012. [Google Scholar]
- Aromataris, E.; Munn, Z. (Eds.) JBI Manual for Evidence Synthesis; JBI, 2020. Available online: https://synthesismanual.jbi.global (accessed on 28 November 2023).
- Clarivate. Endnote Version X9; Clarivate: London, UK, 2013. [Google Scholar]
- Tugwell, P.; Tovey, D. PRISMA 2020. J. Clin. Epidemiol. 2021, 134, A5–A6. [Google Scholar] [CrossRef] [PubMed]
- Daifi, C.; Feldpausch, B.; Roa, P.; Yee, J. Implementation of a Clinical Pharmacist in a Hemodialysis Facility: A Quality Improvement Report. Kidney Med. 2021, 3, 241–247.e1. [Google Scholar] [CrossRef] [PubMed]
- Yeung, D.L.; Alvarez, K.S.; Quinones, M.E.; Clark, C.A.; Oliver, G.H.; Alvarez, C.A.; Jaiyeola, A.O. Low-health literacy flashcards & mobile video reinforcement to improve medication adherence in patients on oral diabetes, heart failure, and hypertension medications. J. Am. Pharm. Assoc. 2017, 57, 30–37. [Google Scholar]
- Cooney, D.; Moon, H.; Liu, Y.; Miller, R.T.; Perzynski, A.; Watts, B.; Drawz, P.E. A pharmacist based intervention to improve the care of patients with CKD: A pragmatic, randomized, controlled trial. BMC Nephrol. 2015, 16, 56. [Google Scholar] [CrossRef]
- Qudah, B.; Albsoul-Younes, A.; Alawa, E.; Mehyar, N. Role of clinical pharmacist in the management of blood pressure in dialysis patients. Int. J. Clin. Pharm. 2016, 38, 931–940. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.-K.; Jeong, S.; Han, N.; Na, H.; Jang, H.Y.; Sohn, M.; Kim, Y.S.; Joo, K.-W.; Oh, K.-H.; Kim, D.K.; et al. Effectiveness of Clinical Pharmacist Service on Drug-Related Problems and Patient Outcomes for Hospitalized Patients with Chronic Kidney Disease: A Randomized Controlled Trial. J. Clin. Med. 2021, 10, 1788. [Google Scholar] [CrossRef] [PubMed]
- Al-Abdelmuhsin, L.; Al-Ammari, M.; Babelghaith, S.D.; Wajid, S.; Asiri, Y.A.; Almetawazi, M.S.; Alghadeer, S.M.; Al-Arifi, M.N. Pharmacist-led Medication Counseling for Patients Undergoing Hemodialysis: A Path to Better Adherence. Int. J. Environ. Res. Public Health 2020, 17, 2399. [Google Scholar] [CrossRef]
- Sabaté, E. Adherence to Long-Term Therapies Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Ritter, J.M.; Flower, R.J.; Henderson, G.; Rang, H.P.; Loke, Y.K.; MacEwan, D. Rang & Dale’s Pharmacology, 8th ed.; Elsevier Churchill Livingstone: London, UK, 2016. [Google Scholar]
- McCahon, D.; Denholm, R.E.; Huntley, A.L.; Dawson, S.; Duncan, P.; Payne, R.A. Development of a model of medication review for use in clinical practice: Bristol medication review model. BMC Med. 2021, 19, 262. [Google Scholar] [CrossRef] [PubMed]
- Shea, S.C. The Medication Interest Model: How to Talk with Patients about Their Medications; Wolters Kluwer: Philadelphia, PA, USA, 2018. [Google Scholar]
- Cross, A.J.; Elliott, R.A.; Petrie, K.; Kuruvilla, L.; George, J. Interventions for improving medication-taking ability and adherence in older adults prescribed multiple medications. Cochrane Database Syst. Rev. 2020, 2020, CD012419. [Google Scholar] [CrossRef]
- Salgado, T.M.; Moles, R.; Benrimoj, S.I.; Fernandez-Llimos, F. Pharmacists’ interventions in the management of patients with chronic kidney disease: A systematic review. Nephrol. Dial. Transplant. 2012, 27, 276–292. [Google Scholar] [CrossRef]
- Al Raiisi, F.; Stewart, D.; Fernandez-Llimos, F.; Salgado, T.M.; Mohamed, M.F.; Cunningham, S. Clinical pharmacy practice in the care of Chronic Kidney Disease patients: A systematic review. Int. J. Clin. Pharm. 2019, 41, 630–666. [Google Scholar] [CrossRef]
- Jasińska-Stroschein, M. The Effectiveness of Pharmacist Interventions in the Management of Patient with Renal Failure: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 11170. [Google Scholar] [CrossRef]
- Marquez, L.L.; Ladd, D.L. Promoting Health Literacy: Finding Consumer Health Resources and Writing Health Materials for Patients. J. Hosp. Librariansh. 2019, 19, 156–164. [Google Scholar] [CrossRef]
- Schoen, D.; Balchin, D.; Thompson, S. Health promotion resources for Aboriginal people: Lessons learned from consultation and evaluation of diabetes foot care resources. Health Promot. J. Aust. 2010, 21, 64–69. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calleja, L.; Glass, B.D.; Cairns, A.; Taylor, S. Pharmacist-Led Interventions for Medication Adherence in Patients with Chronic Kidney Disease: A Scoping Review. Pharmacy 2023, 11, 185. https://doi.org/10.3390/pharmacy11060185
Calleja L, Glass BD, Cairns A, Taylor S. Pharmacist-Led Interventions for Medication Adherence in Patients with Chronic Kidney Disease: A Scoping Review. Pharmacy. 2023; 11(6):185. https://doi.org/10.3390/pharmacy11060185
Chicago/Turabian StyleCalleja, Luke, Beverley D. Glass, Alice Cairns, and Selina Taylor. 2023. "Pharmacist-Led Interventions for Medication Adherence in Patients with Chronic Kidney Disease: A Scoping Review" Pharmacy 11, no. 6: 185. https://doi.org/10.3390/pharmacy11060185
APA StyleCalleja, L., Glass, B. D., Cairns, A., & Taylor, S. (2023). Pharmacist-Led Interventions for Medication Adherence in Patients with Chronic Kidney Disease: A Scoping Review. Pharmacy, 11(6), 185. https://doi.org/10.3390/pharmacy11060185







