A Point Prevalence Survey of Antimicrobial Use at Geita Regional Referral Hospital in North-Western Tanzania
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Duration, and Setting
2.2. Study Population and Selection Criteria and Participant Sample Size Considerations
2.3. Data Collection
2.4. Quality Control
2.5. Data Interpretation, Management and Analysis
3. Results
3.1. The Distribution of Patients Enrolled during the Point Prevalence Survey at Geita Regional Referral Hospital
3.2. Sociodemographic and Clinical Characteristics of Patients Admitted during Point Prevalence Survey at Geita Regional Referral Hospital
3.3. Prevalence of and Indications for Antibiotics Use among Patients Admitted to Geita Regional Referral Hospital
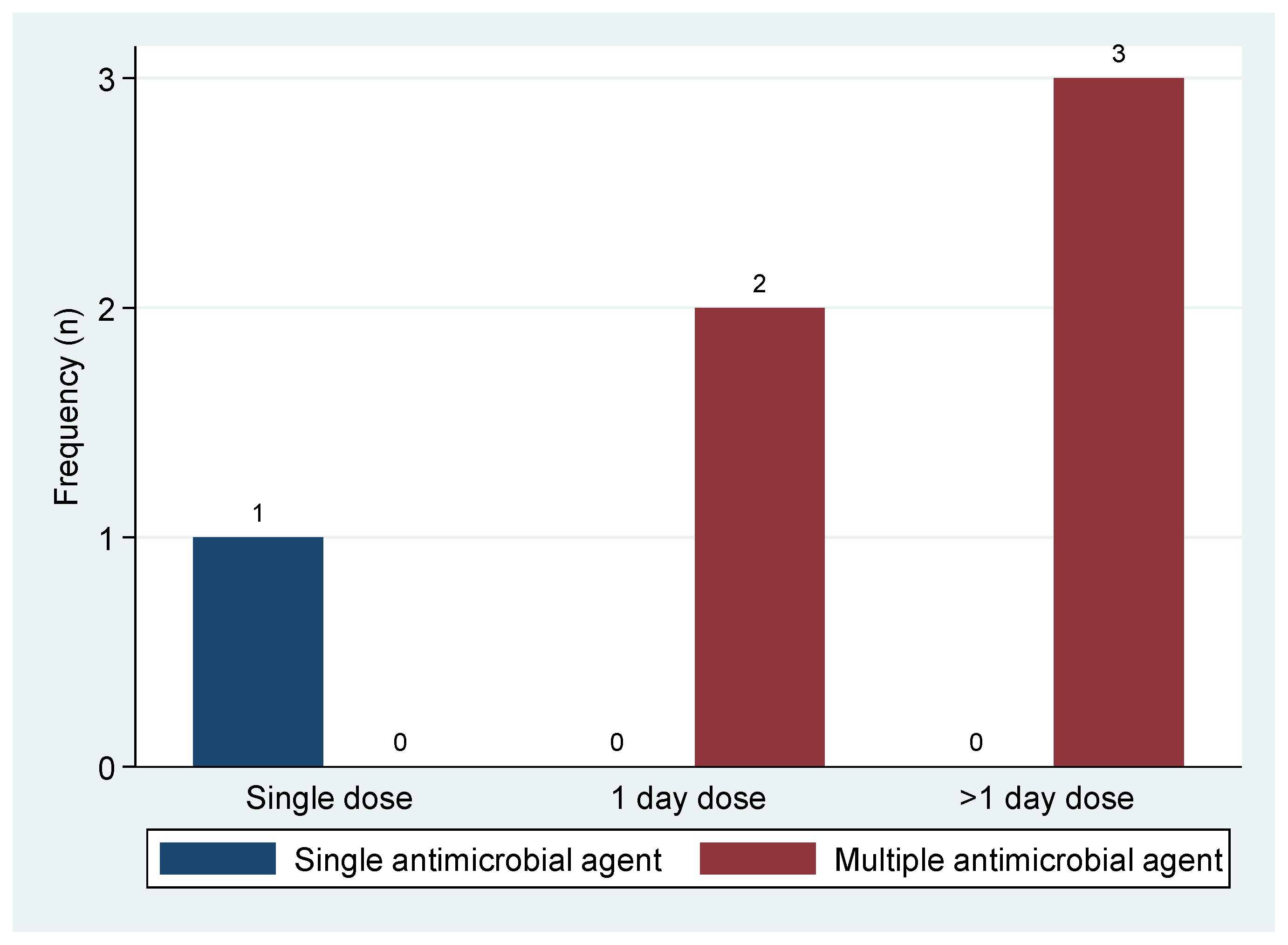
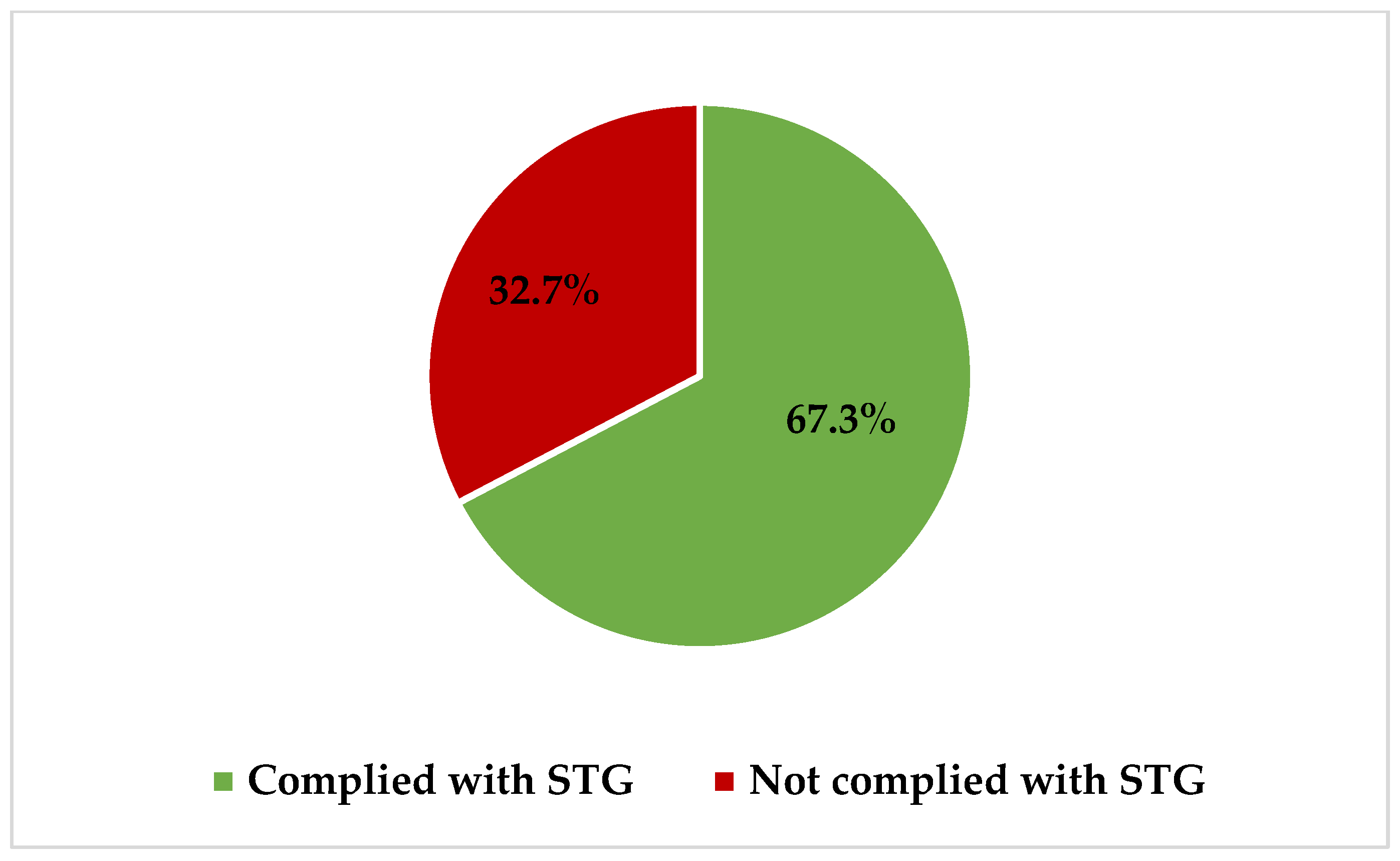
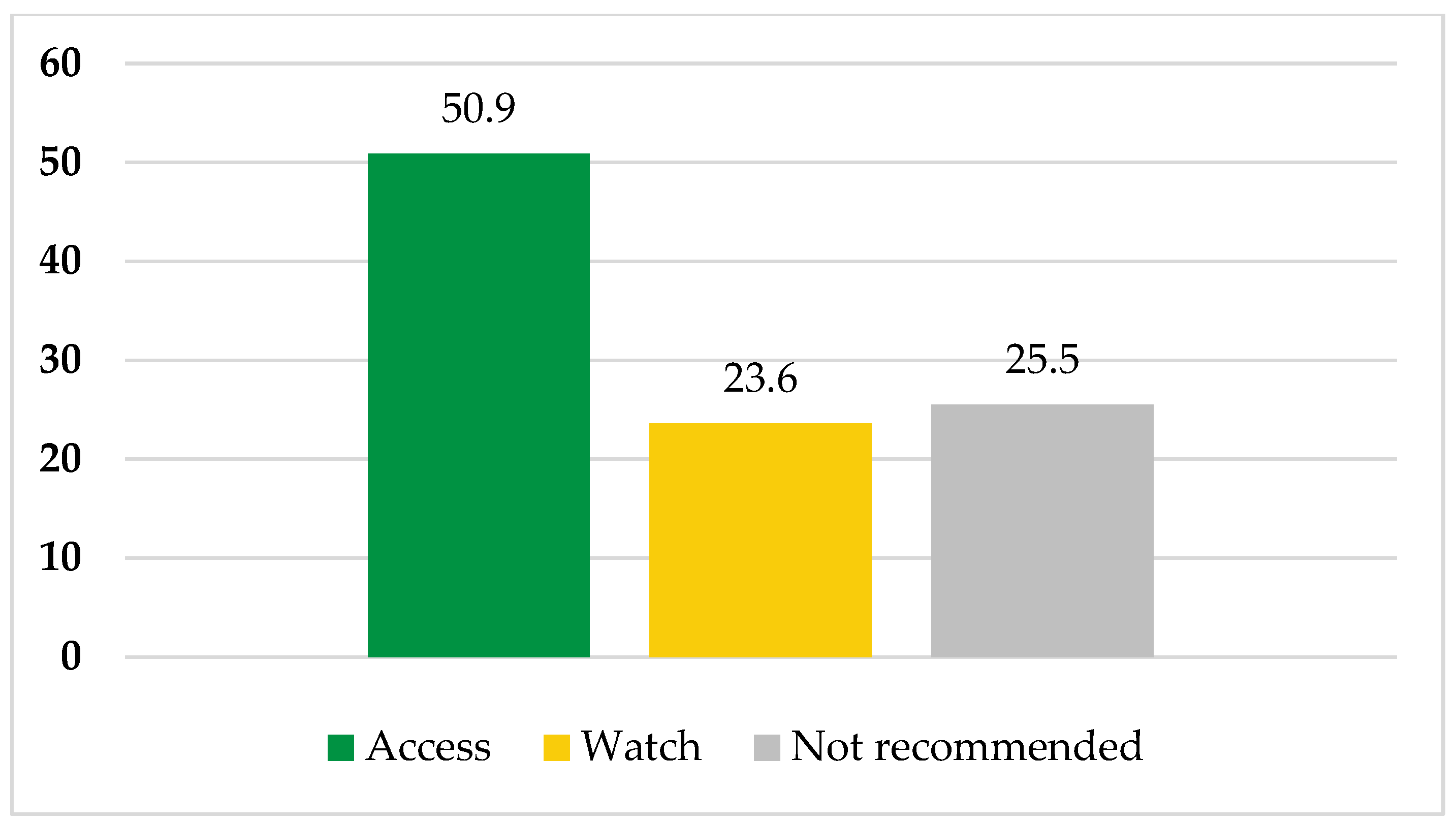
3.4. Compliance of Antibiotic Prescriptions with Standard Treatment Guidelines and National Essential Medicine List for Tanzania Mainland and WHO-AWaRe Classifications at Geita Regional Referral Hospital
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Coculescu, B.-I. Antimicrobial resistance induced by genetic changes. J. Med. Life 2009, 2, 114–123. [Google Scholar]
- WHO. Global Action Plan on Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- MoHT. The National Action Plan on Antimicrobial Resistance 2017–2022; Ministry of Health, Tanzania: Dar es Salaam, Tanzania, 2017. [Google Scholar]
- MoHT. The National Action Plan on Antimicrobial Resistance 2023–2028; Ministry of Health, Tanzania: Dar es Salaam, Tanzania, 2023. [Google Scholar]
- WHO. WHO Methodology for Point Prevalence Survey on Antibiotic Use in Hospitals; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Omulo, S.; Oluka, M.; Achieng, L.; Osoro, E.; Kinuthia, R.; Guantai, A.; Opanga, S.A.; Ongayo, M.; Ndegwa, L.; Verani, J.R.; et al. Point-prevalence survey of antibiotic use at three public referral hospitals in Kenya. PLoS ONE 2022, 17, e0270048. [Google Scholar] [CrossRef]
- Ayukekbong, J.A.; Ntemgwa, M.; Atabe, A.N. The threat of antimicrobial resistance in developing countries: Causes and control strategies. Antimicrob. Resist. Infect. Control 2017, 6, 47. [Google Scholar] [CrossRef]
- Tadesse, B.T.; Ashley, E.A.; Ongarello, S.; Havumaki, J.; Wijegoonewardena, M.; González, I.J.; Dittrich, S. Antimicrobial resistance in Africa: A systematic review. BMC Infect. Dis. 2017, 17, 616. [Google Scholar] [CrossRef]
- Vandael, E.; Latour, K.; Goossens, H.; Magerman, K.; Drapier, N.; Catry, B.; Versporten, A.; the Belgian Point Prevalence Survey Study Group. Point prevalence survey of antimicrobial use and healthcare-associated infections in Belgian acute care hospitals: Results of the Global-PPS and ECDC-PPS 2017. Antimicrob. Resist. Infect. Control 2020, 9, 13. [Google Scholar] [CrossRef]
- Horumpende, P.G.; Mshana, S.E.; Mouw, E.F.; Mmbaga, B.T.; Chilongola, J.O.; de Mast, Q. Point prevalence survey of antimicrobial use in three hospitals in North-Eastern Tanzania. Antimicrob. Resist. Infect. Control 2020, 9, 149. [Google Scholar] [CrossRef]
- Seni, J.; Mapunjo, S.G.; Wittenauer, R.; Valimba, R.; Stergachis, A.; Werth, B.J.; Saitoti, S.; Mhadu, N.H.; Lusaya, E.; Konduri, N. Antimicrobial use across six referral hospitals in Tanzania: A point prevalence survey. BMJ Open 2020, 10, e042819. [Google Scholar] [CrossRef]
- Nandi, A.; Pecetta, S.; Bloom, D.E. Global antibiotic use during the COVID-19 pandemic: Analysis of pharmaceutical sales data from 71 countries, 2020–2022. eClinicalMedicine 2023, 57, 101848. [Google Scholar] [CrossRef]
- Malik, S.S.; Mundra, S. Increasing consumption of antibiotics during the COVID-19 pandemic: Implications for patient health and emerging anti-microbial resistance. Antibiotics 2022, 12, 45. [Google Scholar] [CrossRef]
- Wang, T.; Shen, L.; Yin, J.; Zhou, L.; Sun, Q. Antibiotic use in township hospitals during the COVID-19 pandemic in Shandong, China. Antimicrob. Resist. Infect. Control 2022, 11, 164. [Google Scholar] [CrossRef]
- Ndaki, P.M.; Mushi, M.F.; Mwanga, J.R.; Konje, E.T.; Mugassa, S.; Manyiri, M.W.; Mwita, S.M.; Ntinginya, N.E.; Mmbaga, B.T.; Keenan, K.; et al. Non-prescribed antibiotic dispensing practices for symptoms of urinary tract infection in community pharmacies and accredited drug dispensing outlets in Tanzania: A simulated clients approach. BMC Prim. Care 2022, 23, 287. [Google Scholar] [CrossRef] [PubMed]
- Aanensen, D.M.; Huntley, D.M.; Feil, E.J.; al-Own, F.; Spratt, B.G. EpiCollect: Linking smartphones to web applications for epidemiology, ecology and community data collection. PLoS ONE 2009, 4, e6968. [Google Scholar] [CrossRef] [PubMed]
- StataCorp. Stata Statistical Software: Release 15; StataCorp LLC: College Station, TX, USA, 2017. [Google Scholar]
- MoHT. Standard Treatment Guidelines and National Essential Medicines List for Tanzania Mainland; Ministry of Health, Tanzania: Dar es Salaam, Tanzania, 2021. [Google Scholar]
- WHO. 2021 AWaRe Classification; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Marsh, N.; Webster, J.; Larsen, E.; Cooke, M.; Mihala, G.; Rickard, C.M. Observational study of peripheral intravenous catheter outcomes in adult hospitalized patients: A multivariable analysis of peripheral intravenous catheter failure. J. Hosp. Med. 2018, 13, 83–89. [Google Scholar] [CrossRef] [PubMed]
- Rickard, C.M.; Larsen, E.; Walker, R.M.; Mihala, G.; Byrnes, J.; Saiyed, M.; Cooke, M.; Finucane, J.; Carr, P.J.; Marsh, N. Integrated versus nonintegrated peripheral intravenous catheter in hospitalized adults (OPTIMUM): A randomized controlled trial. J. Hosp. Med. 2023, 18, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Pasalioglu, K.B.; Kaya, H. Catheter indwell time and phlebitis development during peripheral intravenous catheter administration. Pak. J. Med. Sci. 2014, 30, 725. [Google Scholar] [CrossRef]
- Keogh, S.; Shelverton, C.; Flynn, J.; Mihala, G.; Mathew, S.; Davies, K.M.; Marsh, N.; Rickard, C.M. Implementation and evaluation of short peripheral intravenous catheter flushing guidelines: A stepped wedge cluster randomised trial. BMC Med. 2020, 18, 252. [Google Scholar] [CrossRef]
- D’Arcy, N.; Ashiru-Oredope, D.; Olaoye, O.; Afriyie, D.; Akello, Z.; Ankrah, D.; Asima, D.M.; Banda, D.C.; Barrett, S.; Brandish, C.; et al. Antibiotic prescribing patterns in Ghana, Uganda, Zambia and Tanzania hospitals: Results from the global point prevalence survey (G-PPS) on antimicrobial use and stewardship interventions implemented. Antibiotics 2021, 10, 1122. [Google Scholar] [CrossRef]
- Amponsah, O.K.O.; Buabeng, K.O.; Owusu-Ofori, A.; Ayisi-Boateng, N.K.; Hämeen-Anttila, K.; Enlund, H. Point prevalence survey of antibiotic consumption across three hospitals in Ghana. JAC-Antimicrob. Resist. 2021, 3, dlab008. [Google Scholar] [CrossRef]
- Eliopoulos, G.M.; Paterson, D.L.; Rice, L.B. Empirical antibiotic choice for the seriously ill patient: Are minimization of selection of resistant organisms and maximization of individual outcome mutually exclusive? Clin. Infect. Dis. 2003, 36, 1006–1012. [Google Scholar]
- Knobler, S.L.; Lemon, S.M.; Najafi, M.; Burroughs, T. (Eds.) Factors contributing to the emergence of resistance. In The Resistance Phenomenon in Microbes and Infectious Disease Vectors: Implications for Human Health and Strategies for Containment: Workshop Summary; National Academies Press: Washington, DC, USA, 2003. [Google Scholar]
- Bratzler, D.W.; Dellinger, E.P.; Olsen, K.M.; Perl, T.M.; Auwaerter, P.G.; Bolon, M.K.; Fish, D.N.; Napolitano, L.M.; Sawyer, R.G.; Slain, D.; et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am. J. Health Syst. Pharm. 2013, 70, 195–283. [Google Scholar] [CrossRef]
- Kannan, A.; Ravichandran, M.; Sundaramurthi, S.; Win, M.; Tara, A.; Ruo, S.W.; Sultan, W.; Yanamala, V.L.; Mohammed, A.R.H.; Dominic, J.L. Is Single-Dose Antimicrobial Prophylaxis Sufficient to Control Infections in Gastrointestinal Oncological Surgeries? Cureus 2021, 13, e16939. [Google Scholar] [CrossRef] [PubMed]
- Hemantkumar, B.; Ameya, A. Study of Single Dose of Antibiotic Prophylaxis in Clean Surgeries at a Tertiary Care Centre. MVP J. Med. Sci. 2022, 8, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Sweileh, W.M. Global research publications on irrational use of antimicrobials: Call for more research to contain antimicrobial resistance. Glob. Health 2021, 17, 94. [Google Scholar] [CrossRef] [PubMed]
- Rice, L.B. Antimicrobial stewardship and antimicrobial resistance. Med. Clin. N. Am. 2018, 102, 805–818. [Google Scholar] [CrossRef]
- Al-Omari, A.; Al Mutair, A.; Alhumaid, S.; Salih, S.; Alanazi, A.; Albarsan, H.; Abourayan, M.; Al Subaie, M. The impact of antimicrobial stewardship program implementation at four tertiary private hospitals: Results of a five-years pre-post analysis. Antimicrob. Resist. Infect. Control 2020, 9, 95. [Google Scholar] [CrossRef]
- Kiggundu, R.; Wittenauer, R.; Waswa, J.; Nakambale, H.N.; Kitutu, F.E.; Murungi, M.; Okuna, N.; Morries, S.; Lawry, L.L.; Joshi, M.P.; et al. Point prevalence survey of antibiotic use across 13 hospitals in Uganda. Antibiotics 2022, 11, 199. [Google Scholar] [CrossRef]
- Karanja, P.W.; Kiunga, A. Point Prevalence Survey and Patterns of Antibiotic Use at Kirinyaga County Hospitals, Kenya. East Afr. Sci. 2023, 5, 67–72. [Google Scholar] [CrossRef]
| Ward | Survey Date | Total Patients | Eligible Patients | Enrolled Patients |
|---|---|---|---|---|
| Antenatal ward | 9 March 2023 | 7 | 3 | 3 |
| Pediatric 6 | 9 March 2023 | 10 | 10 | 10 |
| Medical male | 9 March 2023 | 5 | 4 | 4 |
| Tuberculosis | 9 March 2023 | 1 | 0 | 0 |
| Medical female | 9 March 2023 | 5 | 4 | 2 |
| Postnatal ward | 10 March 2023 | 7 | 5 | 5 |
| Neonatal | 10 March 2023 | 5 | 5 | 5 |
| Pediatric 1 | 10 March 2023 | 10 | 5 | 5 |
| Grade | 10 March 2023 | 7 | 4 | 4 |
| Surgical male | 10 March 2023 | 16 | 12 | 12 |
| Surgical female | 10 March 2023 | 13 | 8 | 8 |
| Total | 86 | 60 | 58 | |
| Characteristics | Category | Frequency (n) | Percentage (%) |
|---|---|---|---|
| Age in years | Median [IQR] | 25.5 [1.7–36] | - |
| Sex | Female | 28 | 48.3 |
| Male | 30 | 51.7 | |
| Referral | No | 51 | 87.9 |
| Yes | 7 | 12.1 | |
| Central vascular line | No | 57 | 98.3 |
| Yes | 1 | 1.7 | |
| Peripheral vascular catheter | No | 1 | 1.7 |
| Yes | 57 | 98.3 | |
| Urinary indwelling catheter | No | 49 | 84.5 |
| Yes | 9 | 15.5 | |
| Intubation | No | 58 | 100 |
| Yes | 0 | 0.0 | |
| Malaria infection | No | 21 | 36.2 |
| Yes | 11 | 18.9 | |
| Not diagnosed | 26 | 44.9 | |
| Status of TB infection | No | 11 | 18.9 |
| Unknown | 47 | 81.1 | |
| HIV status | Negative | 9 | 15.5 |
| Positive | 1 | 1.7 | |
| Unknown | 48 | 82.8 | |
| Surgical procedure | No | 49 | 84.5 |
| Yes | 9 | 15.5 |
| Characteristic | Category | Frequency (n) | Percentage (%) |
|---|---|---|---|
| Currently using antibiotics | No | 3 | 5.2 |
| Yes | 55 | 94.8 | |
| Antibiotic agents | Mean (±SD) | 2 (±0.5) | - |
| Reason/indication for antibiotic use (N = 55) | Medical prophylaxis | 26 | 47.3 |
| Surgical prophylaxis | 6 | 10.9 | |
| Empirical treatment | 23 | 41.8 | |
| Indications for empiric treatment (N = 23) | CAIs | 21 | 91.3 |
| HCAIs | 2 | 8.7 | |
| Number of prescriptions (N = 110) | Amoxicillin | 2 | 1.8 |
| Ampicillin | 6 | 5.5 | |
| Ampicillin–cloxacillin | 26 | 23.6 | |
| Ceftriaxone | 26 | 23.6 | |
| Ceftriaxone–sulbactam | 2 | 1.8 | |
| Gentamicin | 20 | 18.2 | |
| Metronidazole | 28 | 25.5 | |
| Route of administration of prescribed antibiotics (N = 110) | Oral | 9 | 8.2 |
| Parenteral | 101 | 91.8 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kihwili, L.; Silago, V.; Francis, E.N.; Idahya, V.A.; Saguda, Z.C.; Mapunjo, S.; Mushi, M.F.; Mshana, S.E. A Point Prevalence Survey of Antimicrobial Use at Geita Regional Referral Hospital in North-Western Tanzania. Pharmacy 2023, 11, 159. https://doi.org/10.3390/pharmacy11050159
Kihwili L, Silago V, Francis EN, Idahya VA, Saguda ZC, Mapunjo S, Mushi MF, Mshana SE. A Point Prevalence Survey of Antimicrobial Use at Geita Regional Referral Hospital in North-Western Tanzania. Pharmacy. 2023; 11(5):159. https://doi.org/10.3390/pharmacy11050159
Chicago/Turabian StyleKihwili, Lutugera, Vitus Silago, Emiliana N. Francis, Vicent A. Idahya, Zabron C. Saguda, Siana Mapunjo, Martha F. Mushi, and Stephen E. Mshana. 2023. "A Point Prevalence Survey of Antimicrobial Use at Geita Regional Referral Hospital in North-Western Tanzania" Pharmacy 11, no. 5: 159. https://doi.org/10.3390/pharmacy11050159
APA StyleKihwili, L., Silago, V., Francis, E. N., Idahya, V. A., Saguda, Z. C., Mapunjo, S., Mushi, M. F., & Mshana, S. E. (2023). A Point Prevalence Survey of Antimicrobial Use at Geita Regional Referral Hospital in North-Western Tanzania. Pharmacy, 11(5), 159. https://doi.org/10.3390/pharmacy11050159







