Exploring the Impact of an Innovative Peer Role-Play Simulation to Cultivate Student Pharmacists’ Motivational Interviewing Skills
Abstract
1. Introduction
1.1. Motivational Interviewing in Pharmacy
1.2. Simulations and Role-Play Teaching and Learning in Pharmacy Education
2. Method
2.1. Course Context and Preparatory Activities for Role-Playing
2.2. Description of Focal Learning Activity: An Innovative Approach to Peer Role-Play in MI
2.3. Learning Materials and Activities
2.3.1. Asthma and Medication Primer
2.3.2. Role-Play Scenario and Roles
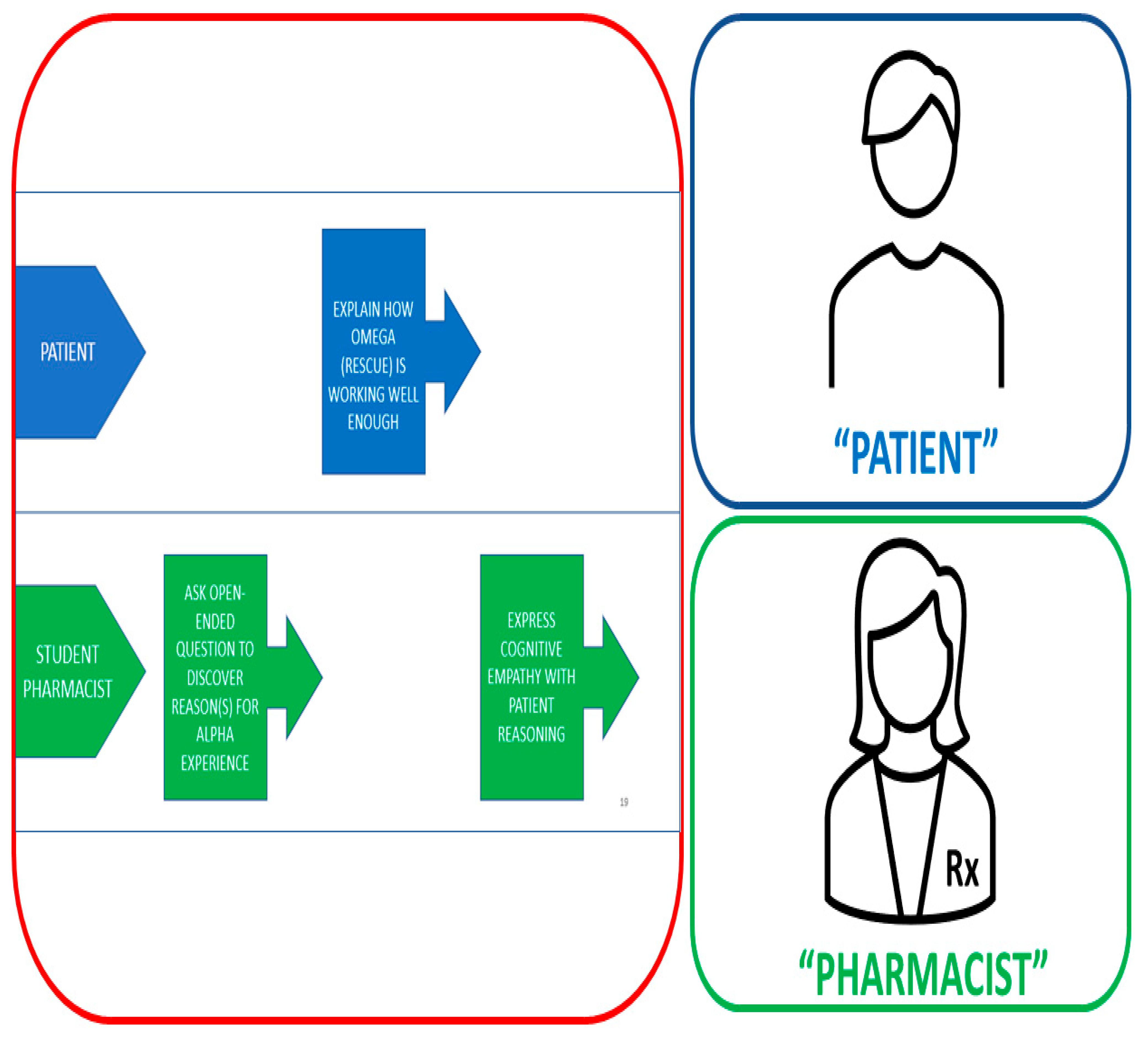
2.3.3. Turn-by-Turn Action Script
2.4. Assessing the Impact of the Role-Play Activity
2.4.1. Instructor-Graded Rubric
2.4.2. Written Student Reflections
3. Results
3.1. Instructor-Graded Rubrics
3.2. Written Student Reflections
4. Discussion
4.1. Unique Features of Our MI Approach That Improved Processes and Skills Assessment
4.2. Impact of Our MI Approach on Student Learning
4.3. The Benefits of Peer Engagement in Role-Play
4.4. Cultivating Communication Skills “On Camera”: Laying Foundations for a Telehealth Future
4.5. Limitations and Future Directions
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Joint Commission of Pharmacy Practitioners. The Pharmacists’ Patient Care Process. Available online: https://jcpp.net/patient-care-process/ (accessed on 23 May 2023).
- Accreditation Council for Pharmacy Education. Accreditation Standards and Key Elements for the Professional Degree Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Standards. 2016. Available online: https://www.acpe-accredit.org/pdf/Standards2016FINAL.pdf (accessed on 23 May 2023).
- Helling, D.K.; Johnson, S.G. Defining and advancing ambulatory care pharmacy practice: It is time to lengthen our stride. Am. J. Health-Syst. Pharm. 2014, 71, 1348–1356. [Google Scholar] [CrossRef] [PubMed]
- Beardsley, R.S.; Skrabal, M.Z.; Kimberlin, C.L. Communication Skills in Pharmacy Practice: A Practical Guide for Students and Practitioners, 7th ed.; Wolters Kluwer: Philadelphia, PA, USA, 2020; pp. 1–11+115–141. [Google Scholar]
- Wallman, A.; Vaudan, C.; Sporrong, S.K. Communications training in pharmacy education, 1995–2010. Am. J. Pharm. Educ. 2013, 77, 36. [Google Scholar] [CrossRef] [PubMed]
- Janke, K.K.; Bloom, T.J.; Boyce, E.G.; Johnson, J.L.; Kopacek, K.; O’Sullivan, T.A.; Petrelli, H.M.W.; Steeb, D.R.; Ross, L.J. A Pathway to Professional Identity Formation: Report of the 2020–2021 AACP Student Affairs Standing Committee. Am. J. Pharm. Educ. 2021, 85, 8714. [Google Scholar] [CrossRef] [PubMed]
- Davis, N.M.; Cohen, M.R. Counseling reduces dispensing accidents. Am. Pharm. 1992, 32, 22. [Google Scholar] [CrossRef]
- DeYoung, M. Research on the effects of pharmacist-patient communication in institutions and ambulatory care sites, 1969–1994. Am. J. Health-Syst. Pharm. 1996, 53, 1277–1291. [Google Scholar] [CrossRef] [PubMed]
- Zolnierek, K.B.H.; Dimatteo, M.R. Physician communication and patient adherence to treatment: A meta-analysis. Med. Care 2009, 8, 826–834. [Google Scholar] [CrossRef]
- Lupu, A.M.; Stewart, A.L.; O’Neil, C. Comparison of active-learning strategies for motivational interviewing skills, knowledge, and confidence in first-year pharmacy students. Am. J. Pharm. Educ. 2012, 76, 28. [Google Scholar] [CrossRef]
- Adrian, J.A.L.; Zeszotarski, P.; Ma, C. Developing Pharmacy Student Communication Skills through Role-playing and Active Learning. Am. J. Pharm. Educ. 2015, 79, 44. [Google Scholar] [CrossRef]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Helping People Change, 3rd ed.; Guilford Press: New York, NY, USA, 2013. [Google Scholar]
- Lundahl, B.; Burke, B.L. The Effectiveness and Applicability of Motivational Interviewing: A Practice-Friendly Review of Four Meta-Analyses. J. Clin. Psychol. 2009, 65, 1232–1245. [Google Scholar] [CrossRef]
- Berger, B.A.; Villaume, W.A. A New Conceptualization and Approach to Learning and Teaching Motivational Interviewing. Innov. Pharm. 2016, 7, 3. [Google Scholar] [CrossRef][Green Version]
- Buring, S.M.; Brown, B.; Kim, K.; Heaton, P.C. Implementation and evaluation of motivational interviewing in a Doctor of Pharmacy curriculum. Curr. Pharm. Teach. Learn. 2011, 3, 78–84. [Google Scholar] [CrossRef]
- Biddle, M.A.; Hoover, R.M. Teaching motivational interviewing in a blended learning environment. Curr. Pharm. Teach. Learn. 2020, 12, 728–734. [Google Scholar] [CrossRef] [PubMed]
- Ekong, G.; Kavookjian, J.; Hutchison, A. Predisposition for empathy, intercultural sensitivity, and intentions for using motivational interviewing in first year pharmacy students. Am. J. Pharm. Educ. 2017, 81, 5989. [Google Scholar] [CrossRef] [PubMed]
- Kane-Gill, S.L.; Smithburger, P.L. Transitioning knowledge gained from simulation to pharmacy practice. Am. J. Pharm. Educ. 2011, 75, 210. [Google Scholar] [CrossRef] [PubMed]
- Zerilli, T.; Fidler, B.D.; Tendhar, C. Assessing the impact of standardized patient encounters on students’ medical history-taking skills in practice. Am. J. Pharm. Educ. 2023, 87, 8989. [Google Scholar] [CrossRef]
- Robertson, A.D.; Moore, M.; McFadden, L.; Steere, E.L.; Barnes, J.; Shrader, S. Implementation and evaluation of simulations in a required course to improve empathy of pharmacy students. Curr. Pharm. Teach. Learn. 2022, 14, 1404–1410. [Google Scholar] [CrossRef]
- Gelis, A.; Cervello, S.; Rey, R.; Llorca, G.; Lambert, P.; Franck, N.; Dupeyron, A.; Delpont, M.; Rolland, B. Peer Role-Play for Training Communication Skills in Medical Students: A Systematic Review. Simul. Healthc. 2020, 15, 106–111. [Google Scholar] [CrossRef]
- Stokoe, E. Simulated Interaction and Communication Skills Training: The ‘Conversation-Analytic Role-Play Method’. In Applied Conversation Analysis; Antaki, C., Ed.; Palgrave Macmillan: London, UK, 2011; pp. 119–139. [Google Scholar] [CrossRef]
- Goggin, K.; Hawes, S.M.; Duval, E.R.; Spresser, C.D.; Martinez, D.A.; Lynam, I.; Barnes, A.; Hinton-Dampf, A.M.; Murphy, M.E.; Marken, P.A.; et al. A motivational interviewing course for pharmacy students. Am. J. Pharm. Educ. 2010, 74, 70. [Google Scholar] [CrossRef]
- Mounsey, A.L.; Bovbjerg, V.; White, L.; Gazewood, J. Do students develop better motivational interviewing skills through role-play with standardised patients or with student colleagues? Med. Educ. 2006, 40, 775–780. [Google Scholar] [CrossRef]
- McFarlane, R.; Spes-Skrbis, M.; Taub, A. Let’s Chat—A fresh take on the invaluable role of peer-to-peer conversation in student engagement, participation, and inclusion. Stud. Success 2017, 8, 107–111. [Google Scholar] [CrossRef]
- Curtis, E.; Ryan, C.; Roy, S.; Simes, T.; Lapkin, S.; O’Neill, B.; Faithfull-Byrne, A. Incorporating peer-to-peer facilitation with a mid-level fidelity student led simulation experience for undergraduate nurses. Nurse Ed. Pract. 2016, 20, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Goldsmith, M.; Stewart, L.; Ferguson, L. Peer learning partnership: An innovative strategy to enhance skill acquisition in nursing students. Nurse Ed. Today 2006, 26, 123–130. [Google Scholar] [CrossRef]
- Medina, M.S.; Plaza, C.M.; Stowe, C.D.; Robinson, E.T.; DeLander, G.; Beck, D.E.; Melchert, R.B.; Supernaw, R.B.; Roche, V.F.; Gleason, B.L.; et al. Center for the Advancement of Pharmacy Education (CAPE) 2013 educational outcomes. Am. J. Pharm. Educ. 2013, 77, 162. [Google Scholar] [CrossRef]
- 2023 GINA Main Report: Global Strategy for Asthma Management and Prevention. Available online: https://ginasthma.org/2023-gina-main-report/ (accessed on 1 June 2023).
- Ratka, A. Empathy and the Development of Affective Skills. Am. J. Pharm. Educ. 2018, 82, 7192. [Google Scholar] [CrossRef] [PubMed]
- Lofland, J.; Lofland, L.H. Analyzing Social Settings: A Guide to Qualitative Observation and Analysis; Wadsworth Publishing Co.: Belmont, CA, USA, 1995. [Google Scholar]
- Ford, J.; Reuber, M. Comparisons of Communication in Medical Face-To-Face and Teleconsultations: A Systematic Review and Narrative Synthesis. Health Commun. 2023, 1–15. [Google Scholar] [CrossRef] [PubMed]
- American Society of Health System Pharmacists Practice Advancement Initiative 2030 Recommendations. Available online: https://www.ashp.org/pharmacy-practice/pai/pai-recommendations (accessed on 1 June 2023).

| MI Learning Objectives after Completing MI Exercises, Students Should Be Able to: | CAPE Outcome |
|---|---|
| Affirm the importance of empathic communication between patients and pharmacists. | 3.6, 4.1 |
| Demonstrate reflective listening with peers who are role-playing as patients. | 3.6 |
| List the steps necessary to decrease issues or relational resistance during counselling. | 1.1 |
| Discuss the connections between rapport (relationship) building, reflective listening, and issue/relational resistance. | 1.1 |
| Demonstrate reflective listening as you paraphrase the patient’s sense making. | 3.2, 3.3, 3.6 |
| Collect the patient’s sense making as neutral, non-judged data. | 3.3, 3.6, 4.4 |
| Invite patients to reflect on their own motivations for change. | 3.2, 3.3, 3.6 |
| Close the deal with goal setting and conditional commitment with high rapport. | 2.3, 3.3, 3.6 |
| Through peer interactions, demonstrate the ability to verbally communicate clearly and professionally, working toward shared goals. | 3.4, 3.6, 4.2, 4.4 |
| Through engagement in innovative role-playing exercises with peers, gain experience in patient–provider communication and patient advocacy. | 3.2, 3.3, 3.6, 4.3 |
| Student Pharmacist Role | Patient Role |
|---|---|
| Your patient is currently relying only on Omega to manage their asthma symptoms when they become severe. You and your patient’s physician both agree that your patient would experience better health by taking Alpha every day. Your goal is to increase your patient’s intrinsic motivation and self-efficacy to adhere to an Alpha regimen. | You were recently seen in the emergency room for a severe asthma attack. Recent changes in your life have worsened your asthma and you have significant stress that has made it difficult for you to adhere to your physician’s recommended asthma action plan. Your goal is to resist taking Alpha (because you prefer Omega) for much of the encounter but to engage in reasonable change talk by the end if the student pharmacist communicates with you effectively. |
| Rubric Criteria: | # Students (out of 82) |
|---|---|
| Employs patient autonomy | 19 |
| Expresses empathy | 1 |
| Develops discrepancy | 23 |
| Enhances patient’s self-efficacy | 3 |
| Rolls with resistance | 6 |
| Patient role: well-prepared | 9 |
| Patient role: challenge presented | 10 |
| Role Played | MI Rubric Criteria | Context from Action Script | Illustrative Quote Demonstrating Need of Improvement to Meet Competency in MI Skill | Illustrative Quote Demonstrating Competency in MI Skill |
|---|---|---|---|---|
| Student Pharmacist | Employs patient autonomy: reassures patient that they are in control | Patient expresses that Omega (rescue) inhaler has been working well, so why take new medication (Alpha for daily maintenance)? | “But I want you to take the Alpha daily…” | “I want to show you that you have options, I want to educate you on the options you have. It is totally your choice…” |
| Student Pharmacist | Expresses empathy: summarizes ambivalence | Patient explains to the pharmacist why they do not take the Alpha as the MD recommended. | “I completely understand that it is very hard to remember taking medications. I take medications myself and I sometimes forget to take my medications.” | “I get that. On the one hand, you have to work and worry about the stresses at work. And on the other hand, you have to worry about, you know, taking another medication along with you every day.” |
| Student Pharmacist | Develops discrepancy: provides patient opportunity to talk about distance between current and goal state | Patient is explaining why they have not adhered to Alpha in the past. | “Is there any way you would be more willing to try the Alpha, or do you feel as though it is not necessary at all?” | “How would you feel if your asthma meds worked better, and you had an easier time breathing?” |
| Student Pharmacist | Enhances patient’s self-efficacy: helps patient build confidence through change-talk | Patient is trying to determine if they are up to the task of taking on a new maintenance medication (Alpha inhaler), given stresses in their life and possibly forgetting to take the med every day. | “I recommend you take it. It is the best course of action for you.” | “We are here to help you. Would you consider a medication alert using your phone to remind you to take the daily medication?” |
| Student Pharmacist | Rolls with resistance: non-confrontational, shifts topic, stresses patient autonomy | Pharmacist is asking the patient how they take the Alpha. Patients are responding that they do not take it at all or as prescribed. | “If you only take Alpha like once in a while, it won’t help you by preventing your symptoms.” | “I get that you don’t want people (family) nagging you (to take maintenance Alpha). Really, the entirety of this (counseling session) is centered on you, what you are willing to do (to improve your asthma treatment). That said, is there anything you would be willing to do with the Alpha medication at this time?” |
| Theme | N (%) * | Explanation | Sample Quotation |
|---|---|---|---|
| Relevance to current and future professional identity formation | 54 (46) | Students perceived that this experience would be beneficial in their short- and long-term futures, including upcoming IPPE rotations, pharmacy skills labs, APPE rotations, and professional practice. They also indicated the breadth of applicability beyond the clinical realm, including leadership, teamwork, community service, and interpersonal relationships. | “Communication is a huge part of my transformation into a practicing professional. I will utilize these skills and behaviors in all parts of my life such as interviews, peer-to-peer communication, relationships, parenting, managing, work, and public service. This class has provided endless utility to me and communicating in a way that is professional is just the tip of the iceberg.” |
| Communication skill awareness and development | 51 (44) | Students experienced “aha” moments regarding the importance of word choice. They described the challenges of using open-ended questions to guide patients, rather than expert recommendations. They appreciated the impact of subtle variations in empathic responses, such as the difference between “I understand” and “That’s understandable.” They also indicated that communicating through digital media added value to the experience. | “I work as a pharmacy technician, so I talk to many patients every shift I work, but while counseling I really had to think about how I was saying everything. I had never really thought about how I was saying things to patients, but it really does make a difference. The motivational interviewing assignment changed the process of what goes through my head while talking to patients and that will stick with me for many years, through school and long after I become a pharmacist.” |
| Learning MI principles and techniques | 36 (31) | Students indicated awareness of the four main MI techniques and underlying principles, with “expressing empathy” emerging as the most consistently mentioned. Many articulated difficult balances and trade-offs among the principles and techniques, such as respecting autonomy and avoiding confrontation while still guiding patients to make healthier choices. | “When I first tried to do the video without thinking about what I wanted to say, I realized how hard it is to have a conversation and motivate a patient that is challenging you because you still have to help direct them to make the best decision for their health, while also making them feel understood. Learning how to roll with resistance without being confrontational is very difficult, and I think that’s one of the main things that I learned from this assignment.” |
| Value of peer engagement | 31 (26) | Students indicated that working with peers helped build connection, trust, and confidence. The experience created a dynamic of interdependence and mutual accountability. Many indicated that discussing empathic responses with peers was instructive, as it helped them appreciate the different ways that others might interpret their empathic formulations, including unintended meanings. | “We began to record [my partner’s] part of the assignment, and once we finished recording, I immediately apologized to her because I thought that I messed up her part, but surprisingly she told me that it was perfect and that I did amazingly. We continued for my part of the assignment, and I started to mess up a lot and immediately became self-conscious of how badly I was doing, but my partner assured me that I was doing my best and to never give up. I don’t know why, but at that moment I felt more confident and remembered that it’s fine to mess up, so I gave it my all in my part of the video, and once we finished, my partner said how proud she was of me.” |
| Learning through role-play | 20 (17) | Students indicated that the action script helped to surface realistic challenges they would encounter in professional practice, in some cases exposing areas for improvement in their communication skills/approach. Many indicated that a “patient” role-player had helped draw attention to these deficits through their responses as the “patient.” Several students mentioned the pressure of improvising on the spot but nonetheless perceived the purpose and value of the pressure for their development. | “The [action script] included challenges such as patient reluctance and noncompliance, which I thought were extremely helpful in simulating a real pharmacist–patient interaction. Not having a full script made the scenarios more realistic and I had to think under pressure while the patient was waiting for a response. This “under pressure” feeling cannot be simulated without working with peers or in a group… I felt more comfortable in my abilities to overcome obstacles that may arise during pharmacist–patient counseling after this activity due to the realistic parameters of the assignment.” |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Denvir, P.; Briceland, L.L. Exploring the Impact of an Innovative Peer Role-Play Simulation to Cultivate Student Pharmacists’ Motivational Interviewing Skills. Pharmacy 2023, 11, 122. https://doi.org/10.3390/pharmacy11040122
Denvir P, Briceland LL. Exploring the Impact of an Innovative Peer Role-Play Simulation to Cultivate Student Pharmacists’ Motivational Interviewing Skills. Pharmacy. 2023; 11(4):122. https://doi.org/10.3390/pharmacy11040122
Chicago/Turabian StyleDenvir, Paul, and Laurie L. Briceland. 2023. "Exploring the Impact of an Innovative Peer Role-Play Simulation to Cultivate Student Pharmacists’ Motivational Interviewing Skills" Pharmacy 11, no. 4: 122. https://doi.org/10.3390/pharmacy11040122
APA StyleDenvir, P., & Briceland, L. L. (2023). Exploring the Impact of an Innovative Peer Role-Play Simulation to Cultivate Student Pharmacists’ Motivational Interviewing Skills. Pharmacy, 11(4), 122. https://doi.org/10.3390/pharmacy11040122






