Pharmacist-Led Implementation of Brief Tobacco Cessation Interventions during Mobile Health Access Events
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Subjects
2.2. Study Measures and Tobacco Cessation Interventions
2.3. Data Collection and Analyses
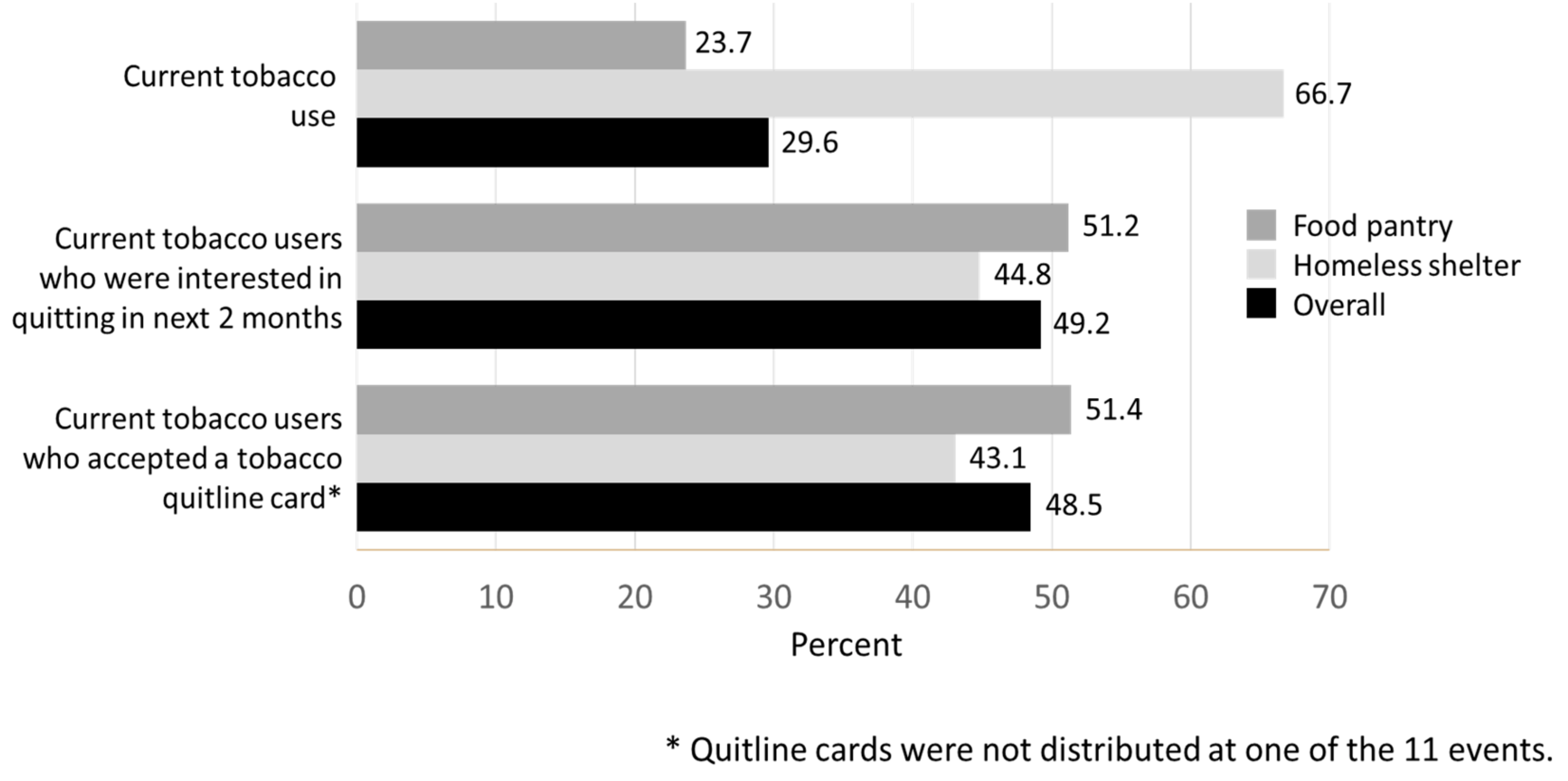
3. Results
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Centers for Disease Control and Prevention; National Center for Chronic Disease Prevention and Health Promotion. Tobacco Use. Available online: https://www.cdc.gov/chronicdisease/resources/publications/factsheets/tobacco.htm (accessed on 3 April 2023).
- Cornelius, M.E.; Loretan, C.G.; Wang, T.W.; Jamal, A.; Homa, D.M. Tobacco Product Use Among Adults—United States, 2020. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Baggett, T.P.; Lebrun-Harris, L.A.; Rigotti, N.A. Homelessness, Cigarette Smoking and Desire to Quit: Results from a US National Study. Addiction 2013, 108, 2009–2018. [Google Scholar] [CrossRef] [PubMed]
- Kim-Mozeleski, J.E.; Pandey, R. The Intersection of Food Insecurity and Tobacco Use: A Scoping Review. Health Promot. Pract. 2020, 21, 124S–138S. [Google Scholar] [CrossRef] [PubMed]
- Soar, K.; Dawkins, L.; Robson, D.; Cox, S. Smoking amongst Adults Experiencing Homelessness: A Systematic Review of Prevalence Rates, Interventions and the Barriers and Facilitators to Quitting and Staying Quit. J. Smok. Cessat. 2020, 15, 94–108. [Google Scholar] [CrossRef]
- Han, L.; Ran, J.; Mak, Y.-W.; Suen, L.K.-P.; Lee, P.H.; Peiris, J.S.M.; Yang, L. Smoking and Influenza-Associated Morbidity and Mortality: A Systematic Review and Meta-Analysis. Epidemiology 2019, 30, 405–417. [Google Scholar] [CrossRef] [PubMed]
- Benowitz, N.L.; Goniewicz, M.L.; Halpern-Felsher, B.; Krishnan-Sarin, S.; Ling, P.M.; O’Connor, R.J.; Pentz, M.A.; Robertson, R.M.; Bhatnagar, A. Tobacco Product Use and the Risks of SARS-CoV-2 Infection and COVID-19: Current Understanding and Recommendations for Future Research. Lancet Respir. Med. 2022, 10, 900–915. [Google Scholar] [CrossRef]
- Babb, S.; Malarcher, A.; Schauer, G.; Asman, K.; Jamal, A. Quitting Smoking Among Adults—United States, 2000–2015. MMWR Morb. Mortal. Wkly. Rep. 2017, 65, 1457–1464. [Google Scholar] [CrossRef]
- Merritt Hawkins Team. Survey of Physician Appointment Wait Times and Medicare and Medicaid Acceptance Rates. Available online: https://www.merritthawkins.com/uploadedFiles/MerrittHawkins/Content/News_and_Insights/Articles/mha-2022-wait-time-survey.pdf (accessed on 3 April 2023).
- Kamimura, A.; Panahi, S.; Ahmmad, Z.; Pye, M.; Ashby, J. Transportation and Other Nonfinancial Barriers Among Uninsured Primary Care Patients. Health Serv. Res. Manag. Epidemiol. 2018, 5, 2333392817749681. [Google Scholar] [CrossRef]
- Kilchenstein, D.; Banta, J.E.; Oh, J.; Grohar, A. Cost Barriers to Health Services in U.S. Adults Before and After the Implementation of the Affordable Care Act. Cureus 2022, 14, e21905. [Google Scholar] [CrossRef]
- Cheyne, K.; Smith, M.; Felter, E.M.; Orozco, M.; Steiner, E.A.; Park, Y.; Gary-Webb, T.L. Food Bank-Based Diabetes Prevention Intervention to Address Food Security, Dietary Intake, and Physical Activity in a Food-Insecure Cohort at High Risk for Diabetes. Prev. Chronic Dis. 2020, 17, E04. [Google Scholar] [CrossRef]
- Fuster, D.; Gelberg, L. Community Screening, Identification, and Referral to Primary Care, for Hepatitis C, B, and HIV Among Homeless Persons in Los Angeles. J. Community Health 2019, 44, 1044–1054. [Google Scholar] [CrossRef]
- Janssens, J.-P.; Wuillemin, T.; Adler, D.; Jackson, Y. Screening for Tuberculosis in an Urban Shelter for Homeless in Switzerland: A Prospective Study. BMC Infect. Dis. 2017, 17, 347. [Google Scholar] [CrossRef]
- Patterson, F.; Robson, S.; McGarry, C.; Taylor, D.; Halvorsen, S.; Rex, S.; Landgraf, R. Testing the Feasibility of a System-Based Approach to Deliver a Smoking Cessation and Food Nudging Intervention at Food Pantry Sites. Transl. Behav. Med. 2020, 10, 146–154. [Google Scholar] [CrossRef]
- Haake, E.R.; Krieger, K.J. Establishing a Pharmacist-Managed Outreach Clinic at a Day Shelter for Homeless Veterans. Ment. Health Clin. 2020, 10, 232–236. [Google Scholar] [CrossRef]
- McCosker, L.K.; El-Heneidy, A.; Seale, H.; Ware, R.S.; Downes, M.J. Strategies to Improve Vaccination Rates in People Who Are Homeless: A Systematic Review. Vaccine 2022, 40, 3109–3126. [Google Scholar] [CrossRef]
- Vijayaraghavan, M.; Elser, H.; Frazer, K.; Lindson, N.; Apollonio, D. Interventions to Reduce Tobacco Use in People Experiencing Homelessness. Cochrane Database Syst. Rev. 2020, 12, CD013413. [Google Scholar] [CrossRef]
- Hartman-Filson, M.; Chen, J.; Lee, P.; Phan, M.; Apollonio, D.E.; Kroon, L.; Donald, F.; Vijayaraghavan, M. A Community-Based Tobacco Cessation Program for Individuals Experiencing Homelessness. Addict. Behav. 2022, 129, 107282. [Google Scholar] [CrossRef]
- Hudmon, K.S.; Corelli, R.L.; de Moor, C.; Zillich, A.J.; Fenlon, C.; Miles, L.; Prokhorov, A.V.; Zbikowski, S.M. Outcomes of a Randomized Trial Evaluating Two Approaches for Promoting Pharmacy-Based Referrals to the Tobacco Quitline. J. Am. Pharm. Assoc. 2018, 58, 387–394. [Google Scholar] [CrossRef]
- Vidrine, J.I.; Shete, S.; Cao, Y.; Greisinger, A.; Harmonson, P.; Sharp, B.; Miles, L.; Zbikowski, S.M.; Wetter, D.W. Ask-Advise-Connect: A New Approach to Smoking Treatment Delivery in Health Care Settings. JAMA Intern. Med. 2013, 173, 458–464. [Google Scholar] [CrossRef]
- Bowen, D.J.; Kreuter, M.; Spring, B.; Cofta-Woerpel, L.; Linnan, L.; Weiner, D.; Bakken, S.; Kaplan, C.P.; Squiers, L.; Fabrizio, C.; et al. How We Design Feasibility Studies. Am. J. Prev. Med. 2009, 36, 452–457. [Google Scholar] [CrossRef]
- Gonzalvo, J.D.; Meredith, A.; Adeoye-Olatunde, O.; Kimiecik, C.; Pastakia, S.; Rodriguez, N.; Ruiz, Y.; Ott, C.; Schellhase, E.; Crawford, E.; et al. A Call to Action from the Purdue University Center for Health Equity and Innovation. J. Am. Coll. Clin. Pharm. 2022, 5, 865–874. [Google Scholar] [CrossRef]
- IBM Corp. IBM SPSS Statistics, Version 28.0.1; IBM: Armonk, NY, USA, 2019. [Google Scholar]
- Brown, T.J.; Todd, A.; O’Malley, C.; Moore, H.J.; Husband, A.K.; Bambra, C.; Kasim, A.; Sniehotta, F.F.; Steed, L.; Smith, S.; et al. Community Pharmacy-Delivered Interventions for Public Health Priorities: A Systematic Review of Interventions for Alcohol Reduction, Smoking Cessation and Weight Management, Including Meta-Analysis for Smoking Cessation. BMJ Open 2016, 6, e009828. [Google Scholar] [CrossRef] [PubMed]
- Liao, C.-Y.; Mott, D.A.; Ford, J.H., II; Look, K.A.; Hayney, M.S. Influenza Vaccination Rates and Location for Receiving the Influenza Vaccination among Older Adult Medicare Beneficiaries. J. Am. Pharm. Assoc. 2021, 61, 432–441.e2. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. COVID-19 Vaccination Federal Retail Pharmacy Partnership Program. Available online: https://www.cdc.gov/vaccines/covid-19/retail-pharmacy-program/index.html (accessed on 3 April 2023).
- Berenbrok, L.A.; Tang, S.; Gabriel, N.; Guo, J.; Sharareh, N.; Patel, N.; Dickson, S.; Hernandez, I. Access to Community Pharmacies: A Nationwide Geographic Information Systems Cross-Sectional Analysis. J. Am. Pharm. Assoc. 2022, 62, 1816–1822.e2. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Doucette, W.R.; Andreski, M.; Pudlo, A. Patient Experiences at Enhanced-Service Pharmacies in Iowa. Innov. Pharm. 2019, 10. [Google Scholar] [CrossRef]
- US Department of Health and Human Services. Treating Tobacco Use and Dependence: 2008 Update; US Department of Health and Human Services: Rockville, MD, USA, 2008. [Google Scholar]
- Hilts, K.E.; Corelli, R.L.; Vernon, V.P.; Hudmon, K.S. Update and Recommendations: Pharmacists’ Prescriptive Authority for Tobacco Cessation Medications in the United States. J. Am. Pharm. Assoc. 2022, 62, 1531–1537. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Best Practices User Guide: Cessation in Tobacco Prevention and Control; U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA, USA, 2020. [Google Scholar]
- Farrell, S.J.; Dunn, M.; Huff, J. Psychiatric Outreach Team; Royal Ottawa Health Care Group Examining Health Literacy Levels in Homeless Persons and Vulnerably Housed Persons with Mental Health Disorders. Community Ment. Health J. 2020, 56, 645–651. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hudmon, K.S.; Czarnik, J.S.; Lahey, A.M.; Crowe, S.J.; Conklin, M.; Corelli, R.L.; Gonzalvo, J.D.; Hilts, K.E. Pharmacist-Led Implementation of Brief Tobacco Cessation Interventions during Mobile Health Access Events. Pharmacy 2023, 11, 72. https://doi.org/10.3390/pharmacy11020072
Hudmon KS, Czarnik JS, Lahey AM, Crowe SJ, Conklin M, Corelli RL, Gonzalvo JD, Hilts KE. Pharmacist-Led Implementation of Brief Tobacco Cessation Interventions during Mobile Health Access Events. Pharmacy. 2023; 11(2):72. https://doi.org/10.3390/pharmacy11020072
Chicago/Turabian StyleHudmon, Karen Suchanek, Julia S. Czarnik, Alexa M. Lahey, Susie J. Crowe, Megan Conklin, Robin L. Corelli, Jasmine D. Gonzalvo, and Katy Ellis Hilts. 2023. "Pharmacist-Led Implementation of Brief Tobacco Cessation Interventions during Mobile Health Access Events" Pharmacy 11, no. 2: 72. https://doi.org/10.3390/pharmacy11020072
APA StyleHudmon, K. S., Czarnik, J. S., Lahey, A. M., Crowe, S. J., Conklin, M., Corelli, R. L., Gonzalvo, J. D., & Hilts, K. E. (2023). Pharmacist-Led Implementation of Brief Tobacco Cessation Interventions during Mobile Health Access Events. Pharmacy, 11(2), 72. https://doi.org/10.3390/pharmacy11020072






