Community-Centered Patient Journey Map in Opioid Use Disorder: A Tool to Address Compassion Fatigue among Community Pharmacists
Abstract
1. Introduction
2. Materials and Methods
2.1. Creation of the Patient Journey Map
2.2. Research Team
2.3. Participants and Data Collection
3. Results
3.1. Overview of Results
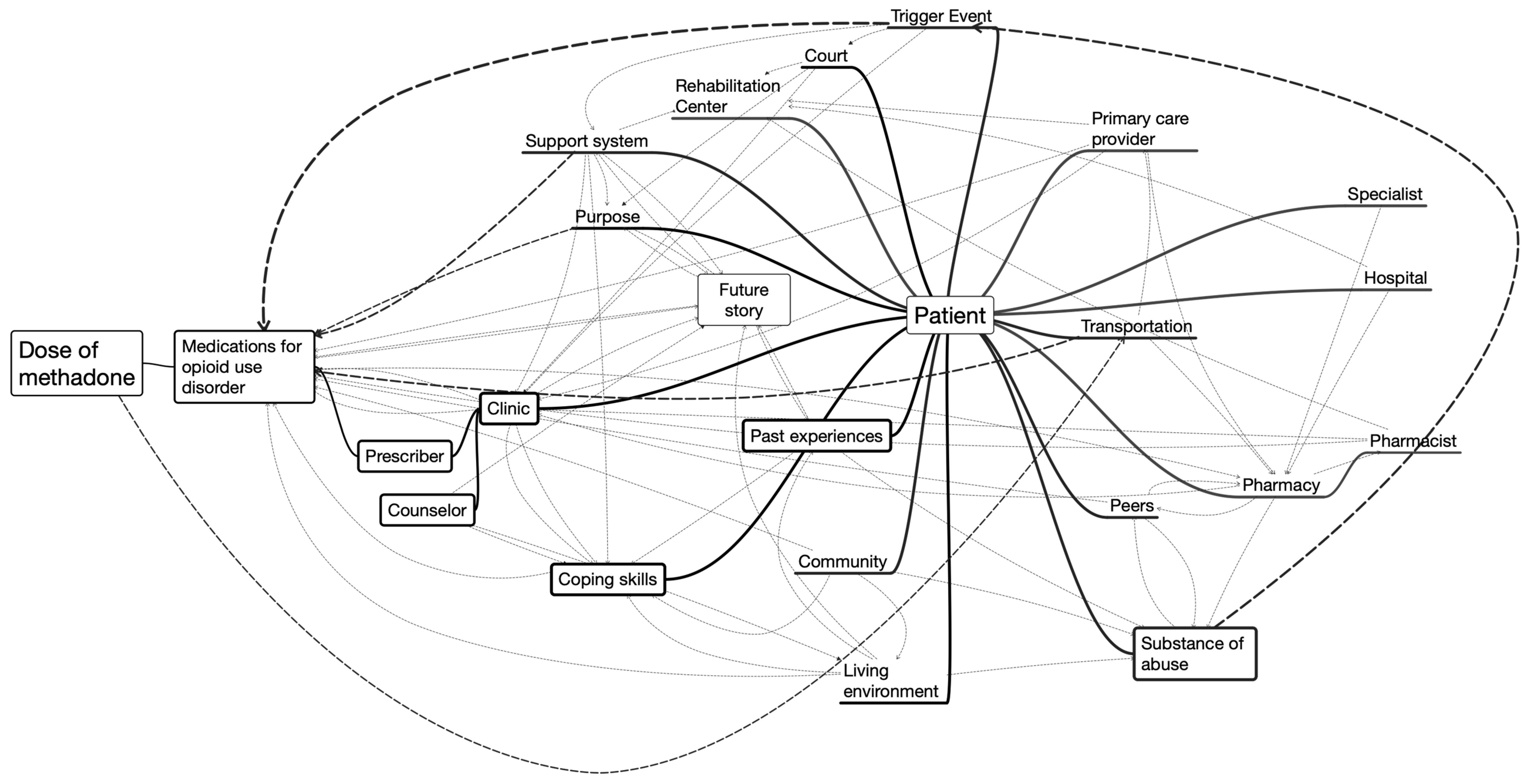
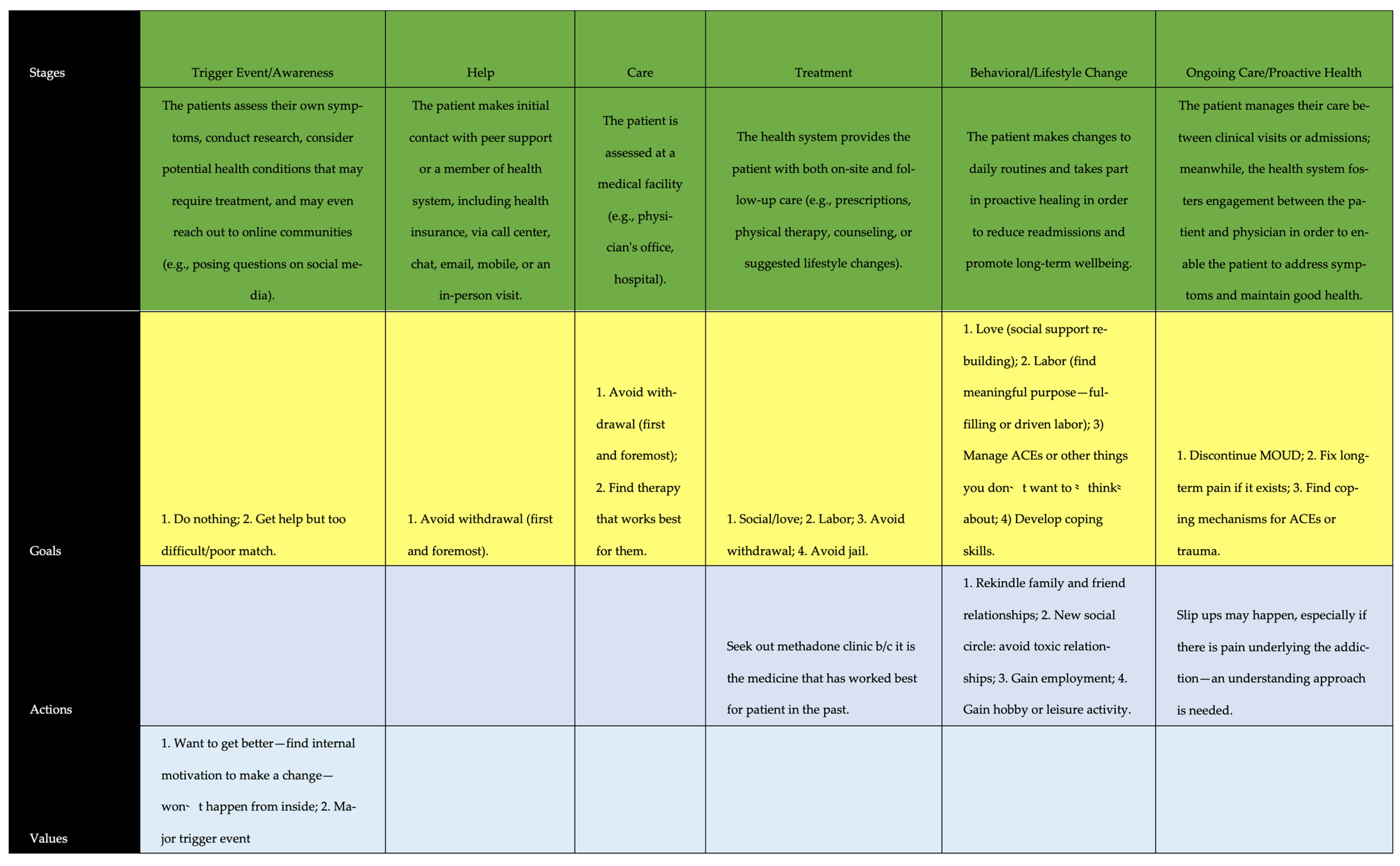
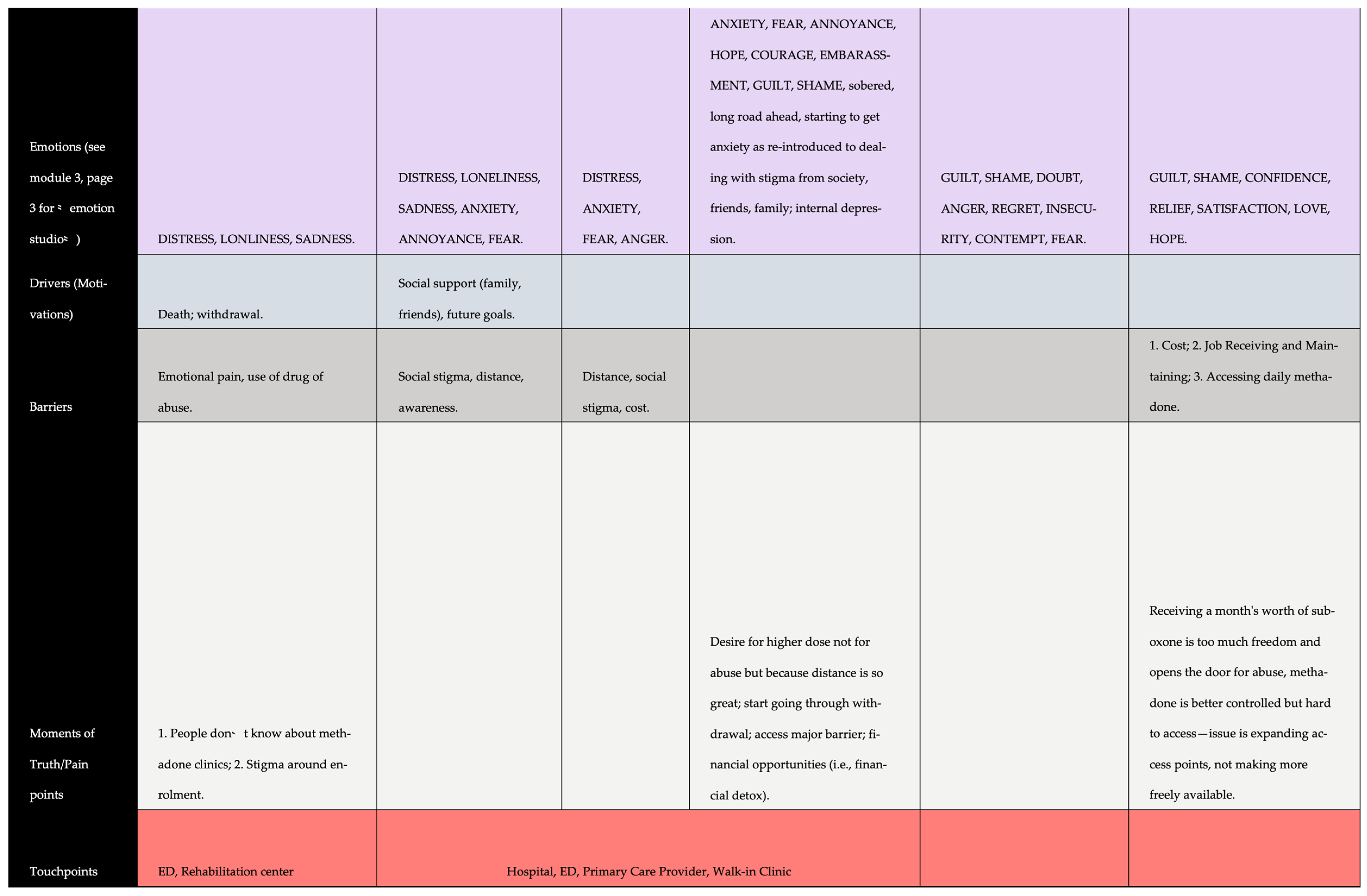
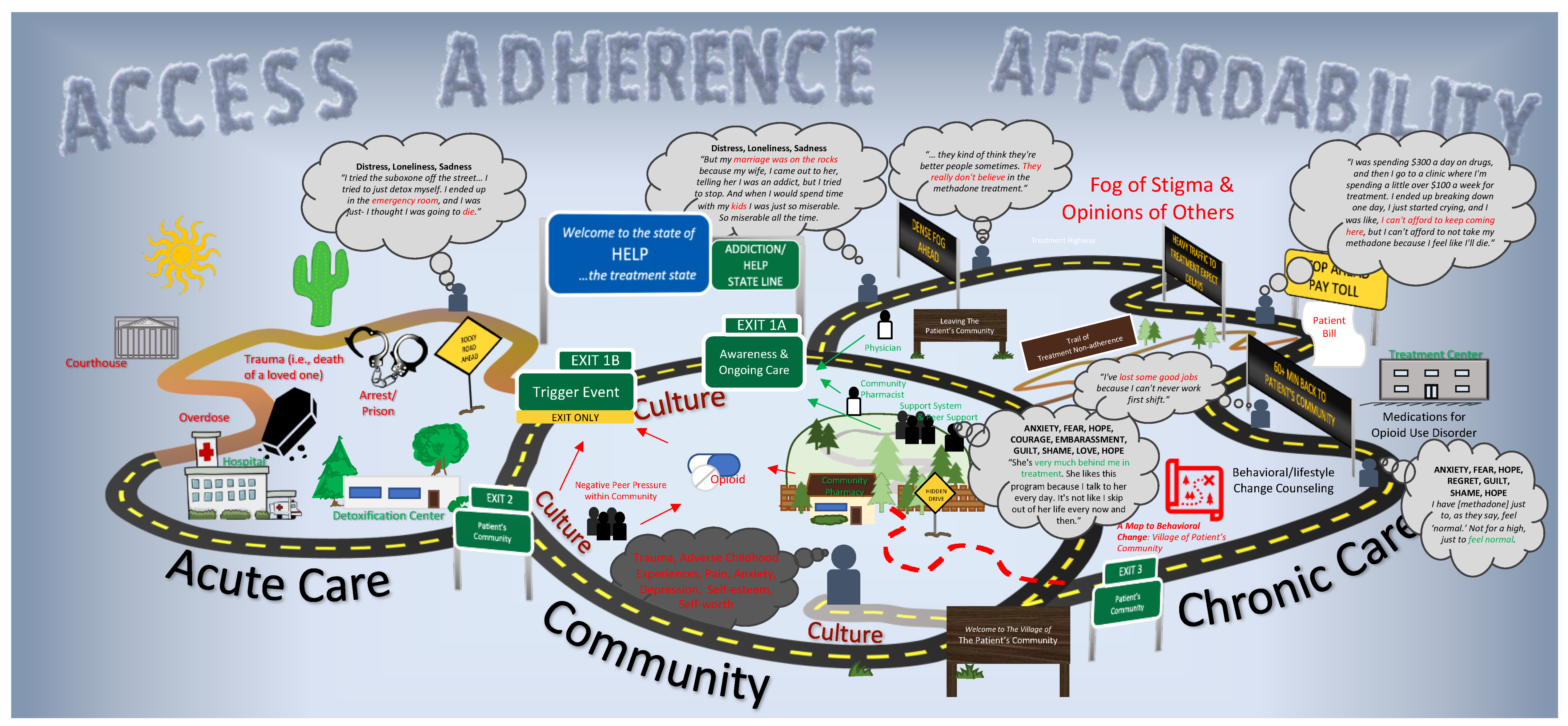
3.2. Community-Centered Patient Journey Map
3.3. Beginning the Patient Journey toward Treatment
3.4. Entering Treatment through ‘Trigger Events’
“Yeah, you got to want to be clean, you know what I’m saying? Then, I didn’t care, you know what I mean? I was just using it for a crutch. But now I’m- I don’t want to go to prison, you know what I’m saying? I just, I want to do right, and that’s the difference. And like, my Dad, because he died of drug use, you know what I mean? He just died this past year.”(P12)
3.5. Entering Treatment through Awareness
“Well, I needed somebody that would kind of, how do I put this, you know [help me]. Because, when I was going to the doctor to get the pain pills, I’d get 120, 90 to 120 [pills], and that’s a 30-day supply. Well, I would be out in two weeks. That’s a lot of pills. So I said, something has got to stop. I’m not going to survive doing this. And I was addicted. They would say, well, why don’t you just quit? Well, I wish it was easier said than done! I just, it’s a lot of stuff that plays into it besides just being an addict and addicted to pain pills. You’ve got all the peer pressure and you have to change your life. You can’t be around people that associate with you. You know, you lose friends. It’s just the way it is if you want to quit, you know, like that. But I got so many [painful] injuries- like, right now, I’m going to have to eventually have a whole hip replacement in my right hip now. And I just, you know, just keep holding on, I don’t want to have to go do it. But I’m eventually going to have to do it. It’s just I’m at that age that I’m falling apart.”(P9)
“I’m 39, and I’ve been- since I was 25, I’d been in and out of drugs, not hard drugs, it was mostly just pot, and then I started taking Lortabs, and then it went to OxyContin, which then led me here to methadone. So I guess my goal is to just get clean…”(P2)
“Once you get two days behind [in payment], you’re put on financial detox. They take you down ten milligrams every day until you’re down to zero, and then you’re done. They just kick you out.”(P2)
“That was frustrating because, when I was working a day job, there was a time or two that I had to not take my medicine because I had to be at work by 9:00. And, I mean, I would get there [to the clinic] at 6:30 or 6:45, and I would have to leave at like 8:30. I’m like, I can’t wait. I’m like, you know, you guys want me to stay clean, believe you me, I want to stay clean, too, but I got to have a job too.”(P11)
“And, at that time, they had like three to six months waiting list, and I thought, oh my God, I can’t wait that long.”(P15)
“…I have to drive an hour every day. I’ve lost like some good jobs because I can’t never work first shift.”(P8)
“Yes, you do [feel stigmatized]. You know, and it may be self-thought. You know, you may have got the wrong attitude from the pharmacist or the personnel there at the pharmacy or whatever. It just seems like sometimes, you know, if you’re picking up a medication, sometimes you’re treated differently than- I’m treated differently when I go in to pick up my heart medication, okay? If I go in and get my blood pressure medication or my blood thinners, I’ve had several heart attacks, so if I go in and get that medication, I’m smiled at and sent on my way. But sometimes when I went in to get the pain medication, [medication for OUD], you know, you could just feel a sense that you were treated a little differently. And I try not to think that about anyone, I really do, but sometimes it’s hard not to feel that. You know, you sense that you’re being treated differently, yeah.”
3.6. Returning to the Community and Ongoing Care
“You know, you may have got the wrong attitude from the pharmacist or the personnel there at the pharmacy or whatever. It just seems like sometimes, you know, if you’re picking up a narcotic medication, sometimes you’re treated differently than- I’m treated differently when I go in to pick up my heart medication, okay? If I go in and get my blood pressure medication or my blood thinners, I’ve had several heart attacks, so if I go in and get that medication, I’m smiled at and sent on my way. But sometimes when I went in to get the pain medication, narcotics, you know, you could just feel a sense that you were treated a little differently. And I try not to think that about anyone, I really do, but sometimes it’s hard not to feel that. You know, you sense that you’re being treated differently.”(P14)
“And, then the biggest difference was [the prescriber] gave me a written prescription and just told me to go to a pharmacy and get it filled. They don’t really know me, I’m just the person who shows up, but of course [the prescriber and community pharmacist] have talked. That’s how they do it, the [prescriber and community pharmacist] talk to each other and set it up between them, so they know you’re coming, right?”(P16)
“Oh, well, I was able to keep a job. My social life improved. I wasn’t always looking or trying to find, you know, my fix just so I could feel better and go sit in my room. Once I got the treatment, I was able to get back out there. And I’m a social butterfly, so I like being around people and talking and hanging out with friends and doing stuff. So once I got treatment, it kind of opened my life back up.”(P6)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mattick, R.P.; Breen, C.; Kimber, J.; Davoli, M. Buprenorphine maintenance versus placebo or methadonemaintenance for opioid dependence. Cochrane Database Syst. Rev. 2014, 2, CD002207. [Google Scholar] [CrossRef]
- Volkow, N.D.; Frieden, T.R.; Hyde, P.S.; Cha, S.S. Medication-assisted therapies–tackling the opioid-overdoseepidemic. N. Engl. J. Med. 2014, 370, 2063–2066. [Google Scholar] [CrossRef]
- Krawczyk, N.; Mojtabai, R.; Stuart, E.A.; Fingerhood, M.; Agus, D.; Lyons, B.C.; Weiner, J.P.; Saloner, B. Opioid agonist treatment and fatal overdose risk in a state-wide USpopulation receiving opioid use disorder services. Addiction 2020, 115, 1683–1694. [Google Scholar] [CrossRef] [PubMed]
- The Centers for Disease Control and Prevention. National Center for Health Statistics. Available online: https://www.cdc.gov/nchs/ (accessed on 7 October 2022).
- Manchikanti, L.; Fellows, S.H.B.; Janata, J.W.; Pampati, V.; Grider, J.S.; Boswell, M.V. Opioid epidemic in the United States. Pain Physician 2012, 15, ES9–ES38. [Google Scholar] [CrossRef] [PubMed]
- The Centers for Disease Control Prevention, U.S. Opioid Dispensing Rate Maps. Available online: https://www.cdc.gov/drugoverdose/rxrate-maps/index.html (accessed on 7 October 2022).
- Cochran, G.; Rubinstein, J.; Bacci, J.L.; Ylioja, T.; Tarter, R. Screening community pharmacy patients for risk of prescription opioid misuse. J. Addict. Med. 2015, 9, 411. [Google Scholar] [CrossRef] [PubMed]
- SAMHSA. Results from the 2020 National Survey on Drug Use and Health: Mental Health Detailed Tables; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2022. [Google Scholar]
- Sullivan, M.D.; Edlund, M.J.; Fan, M.-Y.; Devries, A.; Brennan Braden, J.; Martin, B.C. Risks for possible and probable opioid misuse among recipients of chronic opioid therapy in commercial and medicaid insurance plans: The TROUP Study. Pain 2010, 150, 332–339. [Google Scholar] [CrossRef]
- Muhuri, P.K.; Gfroerer, J.C.; Davies, M.C. Associations of Nonmedical Pain Reliever Use and Initiation of Heroin Use in the United States; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2013. Available online: https://www.samhsa.gov/data/sites/default/files/DR006/DR006/nonmedical-pain-reliever-use-2013.htm (accessed on 13 May 2016).
- Cicero, T.J.; Ellis, M.S.; Surratt, H.L.; Kurtz, S.P. The Changing Face of Heroin Use in the United States: A Retrospective Analysis of the Past 50 Years. JAMA Psychiatry 2014, 71, 821–826. [Google Scholar] [CrossRef]
- Carlson, R.G.; Nahhas, R.W.; Martins, S.S.; Daniulaityte, R. Predictors of transition to heroin use among non-opioid dependent illicit pharmaceutical opioid users: A natural history study. Drug Alcohol Depend. 2016, 160, 127–134. [Google Scholar] [CrossRef]
- National Institute on Drug Abuse. Heroin DrugFacts. December 2022. Available online: http://www.drugabuse.gov/publications/drugfacts/heroin (accessed on 16 February 2023).
- Hagemeier, N.E.; Murawski, M.M.; Lopez, N.C.; Alamian, A.; Pack, R.P. Theoretical exploration of Tennessee community pharmacists’ perceptions regarding opioid pain reliever abuse communication. Res. Soc. Adm. Pharm. 2014, 10, 562–575. [Google Scholar] [CrossRef]
- Eukel, H.N.; Skoy, E.; Werremeyer, A.; Burck, S.; Strand, M. Changes in pharmacists’ perceptions after a training in opioid misuse and accidental overdose prevention. J. Contin. Educ. Health Prof. 2019, 39, 7–12. [Google Scholar] [CrossRef]
- Berenbrok, L.A.; Tang, S.; Gabriel, N.; Guo, J.; Sharareh, N.; Patel, N.; Dickson, S.; Hernandez, I. Access to community pharmacies: A nationwide geographic information systems cross-sectional analysis. J. Am. Pharm. Assoc. 2022, 62, 1816–1822.e2. [Google Scholar] [CrossRef] [PubMed]
- Joudrey, P.J.; Chadi, N.; Roy, P.; Morford, K.L.; Bach, P.; Kimmel, S.; Wang, E.A.; Calcaterra, S.L. Pharmacy-based methadone dispensing and drive time to methadone treatment in five states within the United States: A cross-sectional study. Drug Alcohol Depend. 2020, 211, 107968. [Google Scholar] [CrossRef] [PubMed]
- Bach, P.; Hartung, D. Leveraging the role of community pharmacists in the prevention, surveillance, and treatment of opioid use disorders. Addict. Sci. Clin. Pract. 2019, 14, 30. [Google Scholar] [CrossRef]
- Wu, L.T.; John, W.S.; Ghitza, U.E.; Wahle, A.; Matthews, A.G.; Lewis, M.; Hart, B.; Hubbard, Z.; Bowlby, L.A.; Greenblatt, L.H.; et al. Pharm-OUD-Care Collaborative Investigators. Buprenorphine physician-pharmacist collaboration in the management of patients with opioid use disorder: Results from a multisite study of the National Drug Abuse Treatment Clinical Trials Network. Addiction 2021, 116, 1805–1816. [Google Scholar] [CrossRef] [PubMed]
- Cochran, G.; Hruschak, V.; DeFosse, B.; Hohmeier, K.C. Prescription opioid abuse: Pharmacists’ perspective and response. Integr. Pharm. Res. Pract. 2016, 5, 65. [Google Scholar] [CrossRef]
- Cernasev, A.; Desselle, S.; Hohmeier, K.C.; Canedo, J.; Tran, B.; Wheeler, J. Pharmacy technicians, stigma, and compassion fatigue: Front-line perspectives of pharmacy and the US opioid epidemic. Int. J. Environ. Res. Public Health 2021, 18, 6231. [Google Scholar] [CrossRef] [PubMed]
- Werremeyer, A.; Mosher, S.; Eukel, H.; Skoy, E.; Steig, J.; Frenzel, O.; Strand, M.A. Pharmacists’ stigma toward patients engaged in opioid misuse: When “social distance” does not mean disease prevention. Subst. Abus. 2021, 42, 919–926. [Google Scholar] [CrossRef]
- Dowdell, E.B.; Alderman, S.E.; Foushee, N.; Holland, E.; Reedy, E.A. Expressions of Compassion Fatigue by Emergency Department Nurses Caring for Patients With Opioid and Substance Use Disorders. J. Emerg. Nurs. 2022, 48, 688–697. [Google Scholar] [CrossRef]
- Fatani, S.; Bakke, D.; D’Eon, M.; El-Aneed, A. Qualitative assessment of patients’ perspectives and needs from community pharmacists in substance use disorder management. Subst. Abus. Treat. Prev. Policy 2021, 16, 38. [Google Scholar] [CrossRef]
- Heley, K.; Kennedy-Hendricks, A.; Niederdeppe, J.; Barry, C.L. Reducing Health-Related Stigma Through Narrative Messages. Health Commun. 2020, 35, 849–860. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, S.; O’Raghallaigh, P.; Woodworth, S.; Lim, Y.L.; Kenny, L.C.; Adam, F. An integrated patient journey mapping tool for embedding quality in healthcare service reform. J. Decis. Syst. 2016, 25 (Suppl. S1), 354–368. [Google Scholar] [CrossRef]
- Flood, M.; Ennis, M.; Ludlow, A.; Sweeney, F.F.; Holton, A.; Morgan, S.; Clarke, C.; Carroll, P.; Mellon, L.; Boland, F.; et al. Research methods from human-centered design: Potential applications in pharmacy and health services research. Res. Soc. Adm. Pharm. 2021, 17, 2036–2043. [Google Scholar] [CrossRef]
- Devi, R.; Kanitkar, K.; Narendhar, R.; Sehmi, K.; Subramaniam, K. A narrative review of the patient journey through the lens of non-communicable diseases in low-and middle-income countries. Adv. Ther. 2020, 37, 4808–4830. [Google Scholar] [CrossRef] [PubMed]
- Trebble, T.M.; Hansi, N.; Hydes, T.; Smith, M.A.; Baker, M. Process mapping the patient journey: An introduction. BMJ 2010, 341, c4078. [Google Scholar] [CrossRef] [PubMed]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic analysis: Striving to meet the trustworthiness criteria. Int. J. Qual. Methods 2017, 16, 1609406917733847. [Google Scholar] [CrossRef]
- Montiel Ishino, F.A.; McNab, P.R.; Gilreath, T.; Salmeron, B.; Williams, F. A comprehensive multivariate model of biopsychosocial factors associated with opioid misuse and use disorder in a 2017–2018 United States national survey. BMC Public Health 2020, 20, 1740. [Google Scholar] [CrossRef]
- Chisholm-Burns, M.A.; Spivey, C.A.; Sherwin, E.; Wheeler, J.; Hohmeier, K. The opioid crisis: Origins, trends, policies, and the roles of pharmacists. Am. J. Health Syst. Pharm. 2019, 76, 424–435. [Google Scholar] [CrossRef]
- Carroll, J.J.; Mital, S.; Wolff, J.; Noonan, R.K.; Martinez, P.; Podolsky, M.C.; Killorin, J.C.; Green, T.C. Knowledge, preparedness, and compassion fatigue among law enforcement officers who respond to opioid overdose. Drug Alcohol Depend. 2020, 217, 108257. [Google Scholar] [CrossRef]
- Winstanley, E.L. The bell tolls for thee & thine: Compassion fatigue & the overdose epidemic. Int. J. Drug Policy 2020, 85, 102796. [Google Scholar]
- Coetzee, S.K.; Laschinger, H.K. Toward a comprehensive, theoretical model of compassion fatigue: A n integrative literature review. Nurs. Health Sci. 2018, 20, 4–15. [Google Scholar] [CrossRef]
- Brown, A.R. Health professionals’ attitudes toward medications for opioid use disorder. Subst. Abus. 2022, 43, 598–614. [Google Scholar] [CrossRef] [PubMed]
- Avery, J.; Knoepflmacher, D.; Mauer, E.; Kast, K.A.; Greiner, M.; Avery, J.; Penzner, J.B. Improvement in residents’ attitudes toward individuals with substance use disorders following an online training module on stigma. HSS J. ® 2019, 15, 31–36. [Google Scholar] [CrossRef] [PubMed]
- Moses, T.E.; Chammaa, M.; Ramos, R.; Waineo, E.; Greenwald, M.K. Incoming medical students’ knowledge of and attitudes toward people with substance use disorders: Implications for curricular training. Subst. Abus. 2021, 42, 692–698. [Google Scholar] [CrossRef] [PubMed]
- Muzyk, A.; Smothers, Z.P.; Collins, K.; MacEachern, M.; Wu, L.T. Pharmacists’ attitudes toward dispensing naloxone and medications for opioid use disorder: A scoping review of the literature. Subst. Abus. 2019, 40, 476–483. [Google Scholar] [CrossRef]
- Raisch, D.W.; Fudala, P.J.; Saxon, A.J.; Walsh, R.; Casadonte, P.; Ling, W.; Johnson, B.A.; Malkerneker, U.; Ordorica, P.; Williford, W.O.; et al. Pharmacists’ and pharmacy technicians’ perceptions and attitudes toward dispensing buprenorphine and buprenorphine/naloxone to patients with opioid dependence. J. Am. Pharm. Assoc. 2005, 45, 23–32. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hohmeier, K.C.; Cernasev, A.; Leibold, C.; Moore, T.M.; Schlesinger, E.; Cochran, G.; Arce, I.; Geminn, W.; Chisholm-Burns, M. Community-Centered Patient Journey Map in Opioid Use Disorder: A Tool to Address Compassion Fatigue among Community Pharmacists. Pharmacy 2023, 11, 52. https://doi.org/10.3390/pharmacy11020052
Hohmeier KC, Cernasev A, Leibold C, Moore TM, Schlesinger E, Cochran G, Arce I, Geminn W, Chisholm-Burns M. Community-Centered Patient Journey Map in Opioid Use Disorder: A Tool to Address Compassion Fatigue among Community Pharmacists. Pharmacy. 2023; 11(2):52. https://doi.org/10.3390/pharmacy11020052
Chicago/Turabian StyleHohmeier, Kenneth Charles, Alina Cernasev, Christina Leibold, Todd M. Moore, Erica Schlesinger, Gerald Cochran, Ileana Arce, Wesley Geminn, and Marie Chisholm-Burns. 2023. "Community-Centered Patient Journey Map in Opioid Use Disorder: A Tool to Address Compassion Fatigue among Community Pharmacists" Pharmacy 11, no. 2: 52. https://doi.org/10.3390/pharmacy11020052
APA StyleHohmeier, K. C., Cernasev, A., Leibold, C., Moore, T. M., Schlesinger, E., Cochran, G., Arce, I., Geminn, W., & Chisholm-Burns, M. (2023). Community-Centered Patient Journey Map in Opioid Use Disorder: A Tool to Address Compassion Fatigue among Community Pharmacists. Pharmacy, 11(2), 52. https://doi.org/10.3390/pharmacy11020052









