Promoting Cultural Humility by Integrating Health Equity Literature into the Pharmacy Curriculum
Abstract
:1. Introduction
2. Materials and Methods
2.1. Overview
2.2. Baseline and Concluding Survey
2.3. Reading Assignments
2.4. Post-Assignment Surveys
2.5. Statistical Analysis
3. Results
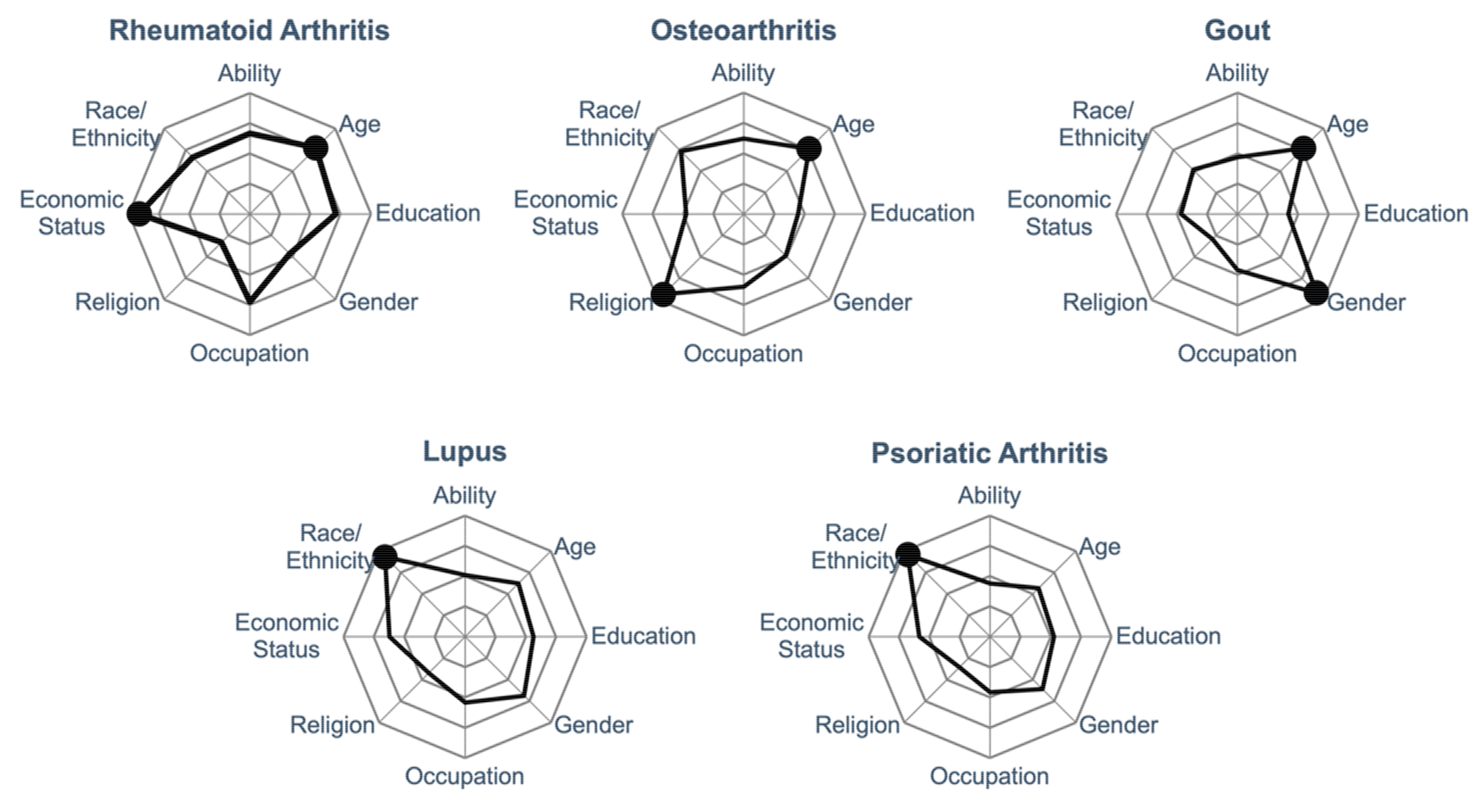
3.1. Students Have Different Baseline Perceptions of How Certain Characteristics Affect Rheumatology Care
3.2. Students Enjoyed Engaging with the Articles and Thought Critically about the Content
3.3. Student Perceptions of the Impact of Social Determinants of Health Evolved with Assigned Readings
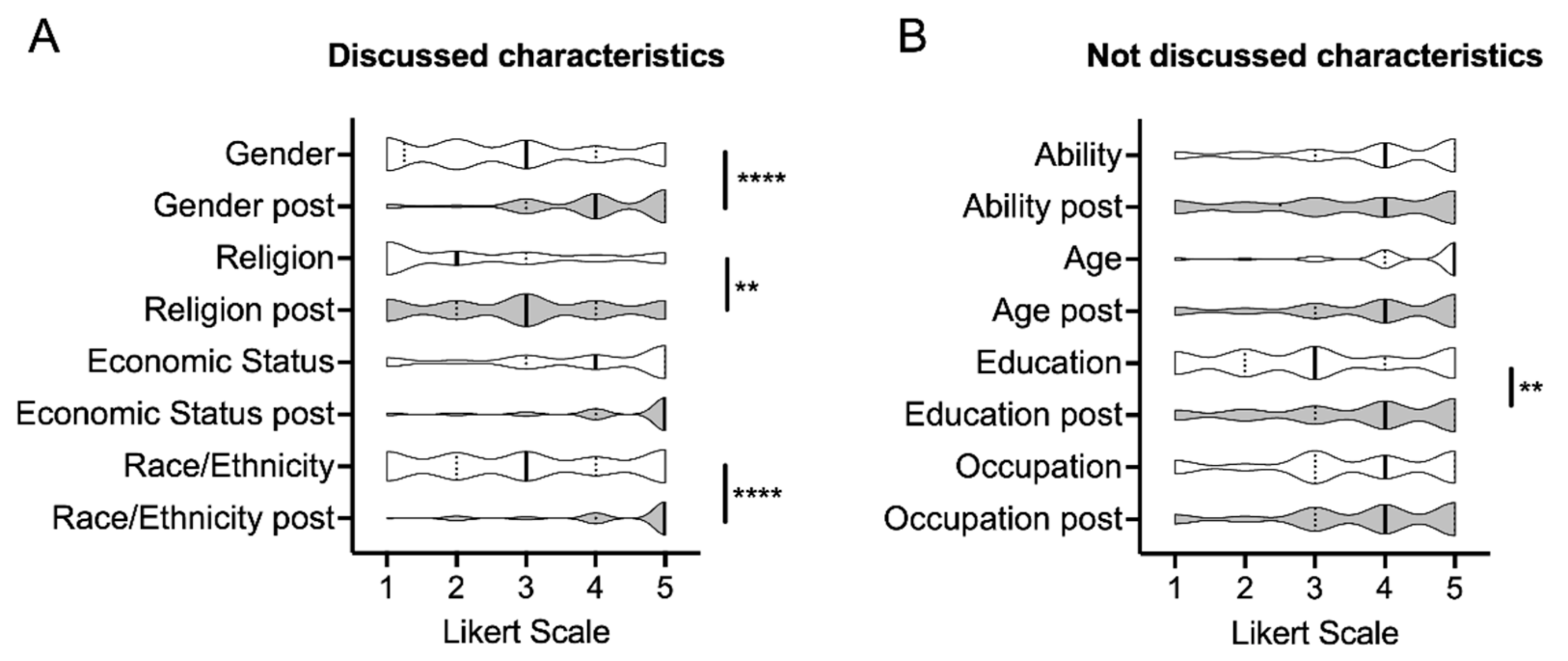
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Betancourt, J.R.; Green, A.R.; Carrillo, J.E.; Owusu, A.-F., II. Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Rep. 2003, 118, 293–302. [Google Scholar] [CrossRef]
- Avant, N.D.; Weed, E.; Connelly, C.; Hincapie, A.L.; Penm, J. Qualitative analysis of student pharmacists’ reflections of Harvard’s race Implicit Association Test. Curr. Pharm. Teach. Learn. 2018, 10, 611–617. [Google Scholar] [CrossRef] [PubMed]
- Hall, W.J.; Chapman, M.V.; Lee, K.M.; Merino, Y.M.; Thomas, T.W.; Payne, B.K.; Eng, E.; Day, S.H.; Coyne-Beasley, T. Implicit racial/rthnic bias among health care professionals and its influence on health care outcomes: A systematic review. Am. J. Public Health 2015, 105, e60–e76. [Google Scholar] [CrossRef] [PubMed]
- Marcelin, J.R.; Siraj, D.S.; Victor, R.; Kotadia, S.; Maldonado, Y.A. The impact of unconscious bias in healthcare: How to recognize and mitigate it. J. Infect. Dis. 2019, 220 (Suppl. S2), S62–S73. [Google Scholar] [CrossRef]
- Wallis, C.J.D.; Jerath, A.; Coburn, N.; Klaassen, Z.; Luckenbaugh, A.N.; Magee, D.E.; Hird, A.E.; Armstrong, K.; Ravi, B.; Esnaola, N.F.; et al. Association of surgeon-patient sex concordance with postoperative outcomes. J. Am. Med. Assoc. Surg. 2021, 157, 146–156. [Google Scholar] [CrossRef]
- Tervalon, M.; Murray-Garcia, J. Cultural humility versus cultural competence: A critical distinction in defining physician training outcomes in multicultural education. J. Health Care Poor Underserved 1998, 9, 117–125. [Google Scholar] [CrossRef]
- Goodman, X.Y.; Nugent, R.L. Teaching cultural competence and cultural humility in dental medicine. Med. Ref. Serv. Q. 2020, 39, 309–322. [Google Scholar] [CrossRef]
- Trinh, N.H.; Jahan, A.B.; Chen, J.A. Moving from cultural competence to cultural humility in psychiatric education. Psychiatr. Clin. N. Am. 2021, 44, 149–157. [Google Scholar] [CrossRef]
- Alsharif, N.Z. Cultural humility and interprofessional education and practice: A winning combination. Am. J. Pharm. Educ. 2012, 76, 120. [Google Scholar] [CrossRef]
- Chang, E.S.; Simon, M.; Dong, X. Integrating cultural humility into health care professional education and training. Adv. Health Sci. Educ. Theory Pract. 2012, 17, 269–278. [Google Scholar] [CrossRef]
- Rouse, M.J. Continuing professional development in pharmacy. J. Am. Pharm. Assoc. 2004, 44, 517–520. [Google Scholar] [CrossRef] [PubMed]
- Khamis, S.; Abdi, A.M.; Basgut, B. Preparing lifelong learners for delivering pharmaceutical care in an ever-changing world: A study of pharmacy students. BMC Med. Educ. 2020, 20, 502. [Google Scholar] [CrossRef] [PubMed]
- Cailor, S.M.; Chen, A.M.H.; Kiersma, M.E.; Keib, C.N. The impact of a research course on pharmacy students’ perceptions of research and evidence-based practice. Curr. Pharm. Teach. Learn. 2017, 9, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.B.; Turner, M.; Patel, M.; Markle, J.; Amend, C.; Absher, R.; Roh, J. Evaluation of an evidence-based medicine curriculum in a PGY1 pharmacy residency program using the Fresno Test. Am. J. Pharm. Educ. 2018, 82, 6294. [Google Scholar] [CrossRef] [PubMed]
- Kiles, T.M.; Patel, K.; Aghagoli, A.; Spivey, C.A.; Chisholm-Burns, M.; Hohmeier, K.C. A community-based partnership collaborative practice agreement project to disseminate and implement evidence-based practices in community pharmacy. Curr. Pharm. Teach. Learn. 2021, 13, 1522–1528. [Google Scholar] [CrossRef]
- Cifaldi, M.; Renaud, J.; Ganguli, A.; Halpern, M.T. Disparities in care by insurance status for individuals with rheumatoid arthritis: Analysis of the medical expenditure panel survey, 2006–2009. Curr. Med. Res. Opin. 2016, 32, 2029–2037. [Google Scholar] [CrossRef]
- Chokkhanchitchai, S.; Tangarunsanti, T.; Jaovisidha, S.; Nantiruj, K.; Janwityanujit, S. The effect of religious practice on the prevalence of knee osteoarthritis. Clin. Rheumatol. 2010, 29, 39–44. [Google Scholar] [CrossRef]
- Harrold, L.R.; Yood, R.A.; Mikuls, T.R.; Andrade, S.E.; Davis, J.; Fuller, J.; Chan, K.A.; Roblin, D.; Raebel, M.A.; Von Worley, A.; et al. Sex differences in gout epidemiology: Evaluation and treatment. Ann. Rheum. Dis. 2006, 65, 1368–1372. [Google Scholar] [CrossRef]
- Rodgers, W.; Williams, E.M.; Smalls, B.L.; Singleton, T.; Tennessee, A.; Kamen, D.; Gilkeson, G. Treating systemic lupus erythematosus (SLE): The impact of historical environmental context on healthcare perceptions and decision-making in Charleston, South Carolina. Int. J. Environ. Res. Public Health 2020, 17, 2285. [Google Scholar] [CrossRef]
- Alexis, A.F.; Blackcloud, P. Psoriasis in skin of color: Epidemiology, genetics, clinical presentation, and treatment nuances. J. Clin. Aesthet. Dermatol. 2014, 7, 16–24. [Google Scholar]
- Thomas, M.; Balbo, J.; Nottingham, K.; Forster, L.; Chavan, B. Student journal club to improve cultural humility with LGBTQ patients. J. Prim. Care Commun. Health 2020, 11, 2150132720963686. [Google Scholar] [CrossRef] [PubMed]
- Henson, B.; Drame, I. Introduction to a programmatic approach to health disparities and cultural competency training in pharmacy education. Am. J. Pharm. Educ. 2021, 86, 8658. [Google Scholar] [CrossRef]
- Drame, I.; Gibson, C.M.; Nonyel, N.P.; Addo-Atua, J.; Butler, L.; Riley, A.; Kebodeaux, C.; Henson, B.; Borja-Hart, N. Strategies for incorporating health disparities and cultural competency training into the pharmacy curriculum and co-curriculum. Am. J. Pharm. Educ. 2022, 86, 8631. [Google Scholar] [CrossRef] [PubMed]
- Assemi, M.; Cullander, C.; Hudmon, K.S. Implementation and evaluation of cultural competency training for pharmacy students. Ann. Pharm. 2004, 38, 781–786. [Google Scholar] [CrossRef] [PubMed]
- Haas-Gehres, A.; Portillo, E.; Kachlic, M.D.; Siu, A. An opportunity to integrate cultural sensitivity training into the doctor of pharmacy curriculum. Am. J. Pharm. Educ. 2021, 85, 8459. [Google Scholar] [CrossRef] [PubMed]
- Haack, S. Engaging pharmacy students with diverse patient populations to improve cultural competence. Am. J. Pharm. Educ. 2008, 72, 124. [Google Scholar] [CrossRef]
- Chen, A.M.H.; Cailor, S.M.; Wicker, E.; Harper, N.G.; Franz, T.T.; Pahl, B. Integrating health literacy and cultural competency concepts across the Doctor of Pharmacy curriculum. Am. J. Pharm. Educ. 2020, 84, ajpe7764. [Google Scholar] [CrossRef]
- Dawn, S.; Dominguez, K.D.; Troutman, W.G.; Bond, R.; Cone, C. Instructional scaffolding to improve students’ skills in evaluating clinical literature. Am. J. Pharm. Educ. 2011, 75, 62. [Google Scholar] [CrossRef]
- Mezgebe, M.; Chesson, M.M.; Thurston, M.M. Pharmacy student perceptions regarding understanding of and confidence in literature evaluation following a student-led journal club. Curr. Pharm. Teach. Learn. 2019, 11, 557–564. [Google Scholar] [CrossRef]
- Bookstaver, P.B.; Rudisill, C.N.; Bickley, A.R.; McAbee, C.; Miller, A.D.; Piro, C.C.; Schulz, R. An evidence-based medicine elective course to improve student performance in advanced pharmacy practice experiences. Am. J. Pharm. Educ. 2011, 75, 9. [Google Scholar] [CrossRef]
- Stark, J.E.; Cole, J.L.; Barnes, L.M.; Chapman, A.; Costner, M. Implementation of a novel learning experience in scientific writing, publishing, and peer review into a first year pharmacy practice residency. J. Am. Pharm. Assoc. 2021, 62, 840–844. [Google Scholar] [CrossRef] [PubMed]
- Johnson, A.; Thornby, K.A.; Ferrill, M. Critical appraisal of biomedical literature with a succinct journal club template: The ROOTs format. Hosp. Pharm. 2017, 52, 488–495. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Year 1 (Mean ± SEM) | Year 2 (Mean ± SEM) | p Value |
|---|---|---|---|
| n = 96 (70%) | n = 112 (84%) | ||
| Age | 3.9 ± 0.12 | 4.3 ± 0.09 | 0.15 |
| Ability | 3.1 ± 0.14 | 3.8 ± 0.12 | <0.01 |
| Economic Status | 3.0 ± 0.13 | 3.8 ± 0.13 | <0.0001 |
| Occupation | 3.5 ± 0.13 | 3.5 ± 0.12 | 0.95 |
| Education | 2.5 ± 0.12 | 3.0 ± 0.13 | 0.20 |
| Race/Ethnicity | 2.6 ± 0.14 | 3.0 ± 0.14 | 0.47 |
| Gender | 2.4 ± 0.13 | 2.8 ± 0.13 | 0.49 |
| Religion | 1.5 ± 0.10 | 2.3 ± 0.14 | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Venditto, V.J.; Colón, K. Promoting Cultural Humility by Integrating Health Equity Literature into the Pharmacy Curriculum. Pharmacy 2022, 10, 116. https://doi.org/10.3390/pharmacy10050116
Venditto VJ, Colón K. Promoting Cultural Humility by Integrating Health Equity Literature into the Pharmacy Curriculum. Pharmacy. 2022; 10(5):116. https://doi.org/10.3390/pharmacy10050116
Chicago/Turabian StyleVenditto, Vincent J., and Kristie Colón. 2022. "Promoting Cultural Humility by Integrating Health Equity Literature into the Pharmacy Curriculum" Pharmacy 10, no. 5: 116. https://doi.org/10.3390/pharmacy10050116
APA StyleVenditto, V. J., & Colón, K. (2022). Promoting Cultural Humility by Integrating Health Equity Literature into the Pharmacy Curriculum. Pharmacy, 10(5), 116. https://doi.org/10.3390/pharmacy10050116







