Antimicrobial Resistance Following Prolonged Use of Hand Hygiene Products: A Systematic Review
Abstract
:1. Introduction
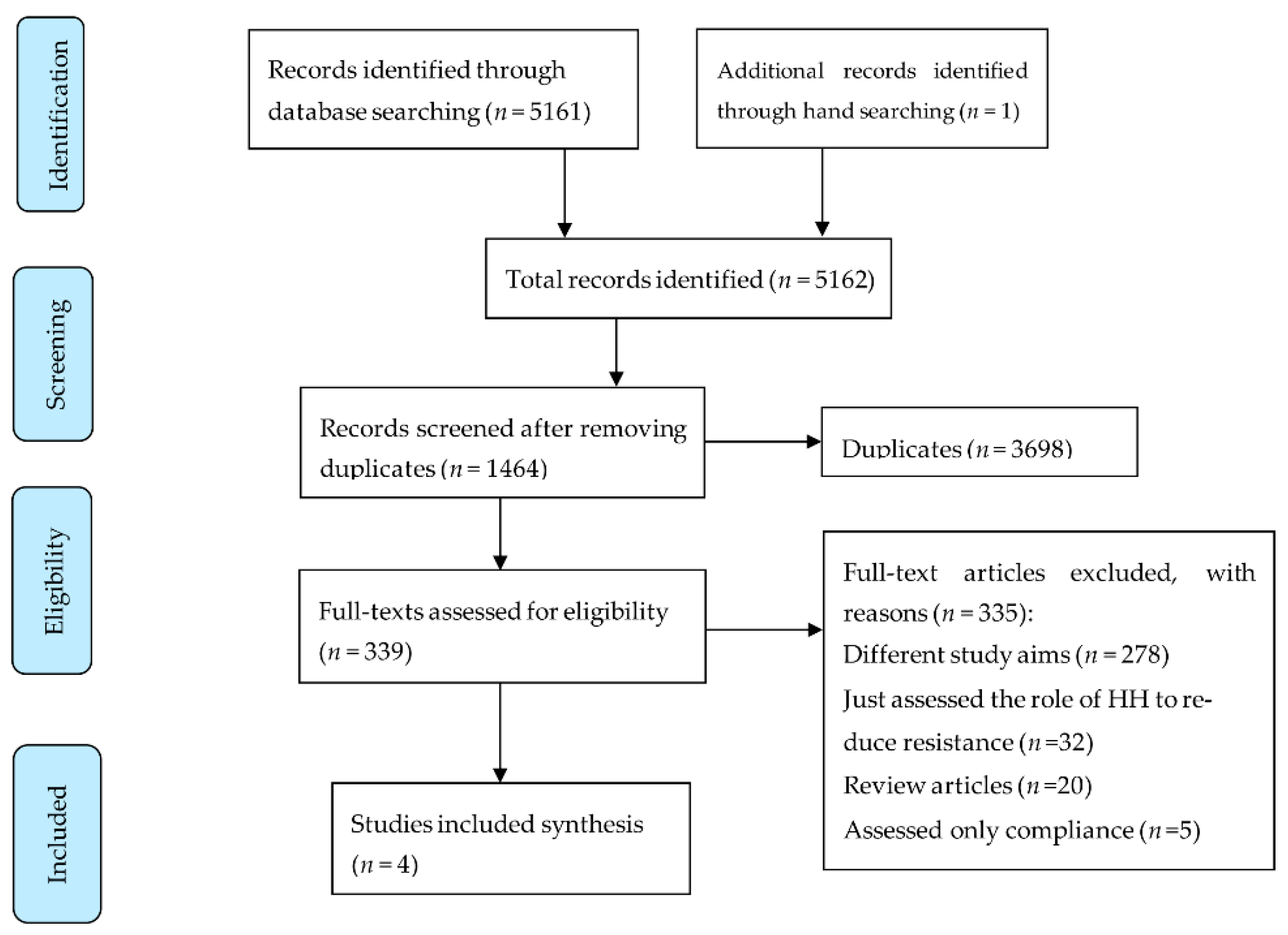
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Study Identification and Data Synthesis
2.3. Quality Assessment
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Prestinaci, F.; Pezzotti, P.; Pantosti, A. Antimicrobial resistance: A global multifaceted phenomenon. Pathog. Glob. Health 2015, 109, 309–318. [Google Scholar] [CrossRef] [Green Version]
- Schweizer, H.P. Efflux as a mechanism of resistance to antimicrobials in Pseudomonas aeruginosa and related bacteria: Unanswered questions. Genet. Mol. Res. 2003, 2, 48–62. [Google Scholar] [PubMed]
- Cohen, M.L. Epidemiology of Drug Resistance: Implications for a Post—Antimicrobial Era. Science 1992, 257, 1050–1055. [Google Scholar] [CrossRef]
- Jackson, N.; Czaplewski, L.; Piddock, L.J.V. Discovery and development of new antibacterial drugs: Learning from experience? J. Antimicrob. Chemother. 2018, 73, 1452–1459. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rochon-Edouard, S.; Pons, J.-L.; Veber, B.; Larkin, M.; Vassal, S.; Lemeland, J.-F. Comparative in vitro and in vivo study of nine alcohol-based handrubs. Am. J. Infect. Control. 2004, 32, 200–204. [Google Scholar] [CrossRef] [PubMed]
- Cheeseman, K.; Denyer, S.; Hosein, I.; Williams, G.; Maillard, J.-Y. Evaluation of the bactericidal efficacy of three different alcohol hand rubs against 57 clinical isolates of S. aureus. J. Hosp. Infect. 2009, 72, 319–325. [Google Scholar] [CrossRef]
- Campoccia, D.; Montanaro, L.; Arciola, C.R. The significance of infection related to orthopedic devices and issues of antibiotic resistance. Biomaterials 2006, 27, 2331–2339. [Google Scholar] [CrossRef]
- Mathur, P. Hand hygiene: Back to the basics of infection control. Indian J. Med. Res. 2011, 134, 611–620. [Google Scholar] [CrossRef]
- Jones, R.D.; Jampani, H.B.; Newman, J.L.; Lee, A.S. Triclosan: A review of effectiveness and safety in health care settings. Am. J. Infect. Control 2000, 28, 184–196. [Google Scholar] [CrossRef]
- Abbas, M.; Nunes, T.R.; Martischang, R.; Zingg, W.; Iten, A.; Pittet, D.; Harbarth, S. Nosocomial transmission and outbreaks of coronavirus disease 2019: The need to protect both patients and healthcare workers. Antimicrob. Resist. Infect. Control. 2021, 10, 7. [Google Scholar] [CrossRef]
- Kraemer, S.A.; Ramachandran, A.; Perron, G.G. Antibiotic Pollution in the Environment: From Microbial Ecology to Public Policy. Microorganisms 2019, 7, 180. [Google Scholar] [CrossRef] [Green Version]
- Cimiotti, J.P.; Wu, F.; Della-Latta, P.; Nesin, M.; Larson, E. Emergence of Resistant Staphylococci on the Hands of New Graduate Nurses. Infect. Control. Hosp. Epidemiol. 2004, 25, 431–435. [Google Scholar] [CrossRef]
- Kampf, G. Acquired resistance to chlorhexidine—Is it time to establish an ’antiseptic stewardship’ initiative? J. Hosp. Infect. 2016, 94, 213–227. [Google Scholar] [CrossRef] [PubMed]
- Aiello, A.E.; Larson, E.L.; Levy, S.B. Consumer antibacterial soaps: Effective or just risky? Clin. Infect. Dis. 2007, 45 (Suppl. S2), S137–S147. [Google Scholar] [CrossRef] [PubMed]
- Aiello, A.E.; Marshall, B.; Levy, S.B.; Della-Latta, P.; Lin, S.X.; Larson, E. Antibacterial Cleaning Products and Drug Resistance. Emerg. Infect. Dis. 2005, 11, 1565–1570. [Google Scholar] [CrossRef] [PubMed]
- Horner, C.; Mawer, D.; Wilcox, M. Reduced susceptibility to chlorhexidine in staphylococci: Is it increasing and does it matter? J. Antimicrob. Chemother. 2012, 67, 2547–2559. [Google Scholar] [CrossRef] [PubMed]
- Yazdankhah, S.P.; Scheie, A.A.; Høiby, E.A.; Lunestad, B.-T.; Heir, E.; Fotland, T.Ø.; Naterstad, K.; Kruse, H. Triclosan and Antimicrobial Resistance in Bacteria: An Overview. Microb. Drug Resist. 2006, 12, 83–90. [Google Scholar] [CrossRef]
- PROSPERO International Prospective Register of Systematic Reviews. Emergence of Antimicrobial Resistance Following Long-Term Use of Hand Washing Products: A Systematic Review. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42017070054 (accessed on 22 December 2021).
- Baym, M.; Lieberman, T.D.; Kelsic, E.D.; Chait, R.; Gross, R.; Yelin, I.; Kishony, R. Spatiotemporal microbial evolution on antibiotic landscapes. Science 2016, 353, 1147–1151. [Google Scholar] [CrossRef] [Green Version]
- Aiello, A.E.; Marshall, B.; Levy, S.B.; Della-Latta, P.; Larson, E. Relationship between Triclosan and Susceptibilities of Bacteria Isolated from Hands in the Community. Antimicrob. Agents Chemother. 2004, 48, 2973–2979. [Google Scholar] [CrossRef] [Green Version]
- Cook, H.A.; Cimiotti, J.P.; Della-Latta, P.; Saiman, L.; Larson, E.L. Antimicrobial resistance patterns of colonizing flora on nurses’ hands in the neonatal intensive care unit. Am. J. Infect. Control 2007, 35, 231–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Geraldo, I.M.; Gilman, A.; Shintre, M.S.; Modak, S.M. Rapid Antibacterial Activity of 2 Novel Hand Soaps: Evaluation of the Risk of Development of Bacterial Resistance to the Antibacterial Agents. Infect. Control. Hosp. Epidemiol. 2008, 29, 736–741. [Google Scholar] [CrossRef] [PubMed]
- Baraldi, M.M.; Gnatta, J.R.; Padoveze, M.C. Risks and benefits of using chlorhexidine gluconate in handwashing: A systematic literature review. Am. J. Infect. Control. 2019, 47, 704–714. [Google Scholar] [CrossRef] [PubMed]
- Copitch, J.L.; Whitehead, R.N.; Webber, M.A. Prevalence of decreased susceptibility to triclosan in Salmonella enterica isolates from animals and humans and association with multiple drug resistance. Int. J. Antimicrob. Agents 2010, 36, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Schweizer, H.P. Triclosan: A widely used biocide and its link to antibiotics. FEMS Microbiol. Lett. 2001, 202, 1–7. [Google Scholar] [CrossRef]
- Chuanchuen, R.; Beinlich, K.; Hoang, T.T.; Becher, A.; Karkhoff-Schweizer, R.R.; Schweizer, H.P. Cross-resistance between triclosan and antibiotics in Pseudomonas aeruginosa is mediated by multidrug efflux pumps: Exposure of a susceptible mutant strain to triclosan selects nfxB mutants overexpressing MexCD-OprJ. Antimicrob. Agents Chemother. 2001, 45, 428–432. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Advice for the Public: Coronavirus Disease (COVID-19). Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public (accessed on 7 November 2021).
- Daverey, A.; Dutta, K. COVID-19: Eco-friendly hand hygiene for human and environmental safety. J. Environ. Chem. Eng. 2021, 9, 104754. [Google Scholar] [CrossRef]
- Singer, A.C.; Shaw, H.; Rhodes, V.; Hart, A. Review of Antimicrobial Resistance in the Environment and Its Relevance to Environmental Regulators. Front. Microbiol. 2016, 7, 1728. [Google Scholar] [CrossRef] [Green Version]
- Pidot, S.J.; Gao, W.; Buultjens, A.H.; Monk, I.R.; Guerillot, R.; Carter, G.P.; Lee, J.Y.H.; Lam, M.M.C.; Grayson, M.L.; Ballard, S.A.; et al. Increasing tolerance of hospital Enterococcus faecium to handwash alcohols. Sci. Transl. Med. 2018, 10, eaar6115. [Google Scholar] [CrossRef] [Green Version]
- Atolani, O.; Baker, M.T.; Adeyemi, O.; Olanrewaju, I.R.; Hamid, A.A.; Ameen, O.M.; Oguntoye, S.O.; Usman, L.A. COVID-19: Critical discussion on the applications and implications of chemicals in sanitizers and disinfectants. EXCLI J. 2020, 19, 785–799. [Google Scholar]
- Mahmood, A.; Eqan, M.; Pervez, S.; Alghamdi, H.A.; Tabinda, A.B.; Yasar, A.; Brindhadevi, K.; Pugazhendhi, A. COVID-19 and frequent use of hand sanitizers; human health and environmental hazards by exposure pathways. Sci. Total Environ. 2020, 742, 140561. [Google Scholar] [CrossRef]
- Rusic, D.; Vilovic, M.; Bukic, J.; Leskur, D.; Perisin, A.S.; Kumric, M.; Martinovic, D.; Petric, A.; Modun, D.; Bozic, J. Implications of COVID-19 Pandemic on the Emergence of Antimicrobial Resistance: Adjusting the Response to Future Outbreaks. Life 2021, 11, 220. [Google Scholar] [CrossRef] [PubMed]
- Ciotti, C.; Ferrao, B.; Garrigues, I.; Nérome, S. Bacteria which are highly resistant to antibiotics are not resistant hydro-alcoholic products. Infect. Dis. Now 2021, 51, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Kamathewatta, K.; Bushell, R.; Rafa, F.; Browning, G.; Billman-Jacobe, H.; Marenda, M. Colonization of a hand washing sink in a veterinary hospital by an Enterobacter hormaechei strain carrying multiple resistances to high importance antimicrobials. Antimicrob. Resist. Infect. Control. 2020, 9, 163. [Google Scholar] [CrossRef] [PubMed]
| Authors, Year [Ref] | Country | Study Year | Age | Gender | Study Type | Setting | Participants | Sample Size | Key Finding | NOS Score |
|---|---|---|---|---|---|---|---|---|---|---|
| Aiello et al., 2004 [20] | USA | 2003 | NR | NR | Double-blinded randomised intervention trial | Household | Household, the primary caregiver | 224 (half received antibacterial products) | No statistically significant association between triclosan MICs and susceptibility to antibiotic was found. There was an increasing trend in the association of ORs for all species, compared at baseline (OR 0.65, CI95% 0.33–1.27) versus at the end of the year (OR 1.08, CI95% 0.62–1.97) and for GNB alone at baseline (OR 0.66, CI95% 0.29–1.51) versus the end of year (OR 2.69, CI95% 0.78 to 9.23) regardless of the hand-washing product used. There was a significantly higher proportion of Acinetobacter lwoffii for which the triclosan MICs were greater than the median at the end of the year compared to the baseline (p > 0.001). There were significantly higher proportions of Klebsiella pneumoniae and S. aureus for which the triclosan MICs were greater than the median at baseline compared to the end of the year (p ≥ 0.013 and p ≥ 0.001, respectively). There were no significant differences when we compared the proportion of triclosan MIC values greater than the median at baseline versus that at the end of the year for any of the other organisms (all p ≥ 0.05) | *** *** * |
| Aiello et al., 2005 [15] | USA | One full year, before 2005 | NR | NR | Double-masked randomised home intervention trial | Household | Household primary caregiver | 238 | Antibacterial products did not lead to a significant increase in AMR after one year (OR 1.33, CI95% 0.74–2.41) | *** *** ** |
| Cook et al., 2007 [21] | USA | March 2001–January 2003 | Averageage 41.1 years | 116 female, 3 male | Sub-study of a larger cross-over clinical trial | Hospital | NICU staff nurses | 119 | When antiseptic soap was used, there was a significant increase in Staphylococcus epidermidis isolates resistant to oxacillin (RR 1.92; CI95% 1.08–3.43) and gentamicin (RR, 1.50; CI95% 1.00–2.27) and a 7.22 times increased risk of rifampicin resistance among Staphylococcus warneri isolates (CI95% 2.97–17.56) | *** ** |
| Geraldo et al., 2008 [22] | USA | Not mentioned | NR | NR | In-vitro, a volunteer method and in-vivo method | Laboratory setting | Effectiveness of soaps evaluated using an in-vitro tube dilution method, a volunteer method, and 2 pig skin methods. No specifics about volunteers have been provided | NR | The MIC and minimum bactericidal concentrations of triclosan alone and triclosan-containing soaps against S. aureus increased 8- to 62.5-fold after passage (20 times), whereas those of TPB and FPB (both alone and in soap) were unchanged to 62.5-fold after passage (20 times) | ** |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Banik, G.R.; Durayb, B.; King, C.; Rashid, H. Antimicrobial Resistance Following Prolonged Use of Hand Hygiene Products: A Systematic Review. Pharmacy 2022, 10, 9. https://doi.org/10.3390/pharmacy10010009
Banik GR, Durayb B, King C, Rashid H. Antimicrobial Resistance Following Prolonged Use of Hand Hygiene Products: A Systematic Review. Pharmacy. 2022; 10(1):9. https://doi.org/10.3390/pharmacy10010009
Chicago/Turabian StyleBanik, Gouri Rani, Bandar Durayb, Catherine King, and Harunor Rashid. 2022. "Antimicrobial Resistance Following Prolonged Use of Hand Hygiene Products: A Systematic Review" Pharmacy 10, no. 1: 9. https://doi.org/10.3390/pharmacy10010009
APA StyleBanik, G. R., Durayb, B., King, C., & Rashid, H. (2022). Antimicrobial Resistance Following Prolonged Use of Hand Hygiene Products: A Systematic Review. Pharmacy, 10(1), 9. https://doi.org/10.3390/pharmacy10010009








